Abstract
Post-Epstein-Barr virus (EBV) cerebellitis is very rare complication of infectious mononucleosis and only a few adult cases are reported in literature. We present a 23-year-old patient who was admitted to the neurology service with worsening ataxia, nystagmus and dysarthria, 1 week after infectious mononucleosis. Imaging and cerebrospinal fluid studies were normal, serum studies revealed acute transaminitis and positive EBV viral capsid IgM and IgG. The patient underwent a 5-day course of intravenous immunoglobulins with rapid resolution of all his symptoms and was safely discharged home. The pathophysiology of post-EBV cerebellitis involves autoreactive antibodies, rather than a direct viral insult. Antineuronal antibodies might be the result of a mimicry between EBV proteins and neuronal antigens or they can be secreted by the EBV-transformed lymphocytes themselves. Many reports stress the benign, self-limiting nature of this syndrome; however, immunotherapy might de facto decrease the severity and duration of illness.
Keywords: neurology, Brain stem/cerebellum, infection (neurology)
Background
Post-Epstein-Barr virus (EBV) cerebellitis has been reported in children <6 years of age, but it is very rare in young immunocompetent adults. We present the case of post-EBV cerebellitis in a young adult treated with intravenous immunoglobulins.
Case presentation
A 23-year-old right-handed Caucasian man presented to the emergency department in September with worsening ataxia. A week prior to that he had developed fever up to 103°F (39.4°C), diaphoresis, headache and bilateral retro-orbital pain. The symptoms were partially relieved by scheduled nonsteroidal anti-inflammatory drugs (NSAIDs). A few days later, he developed gait ataxia and slurred speech which prompted him to visit the emergency department. He denied any history of drugs, alcohol use or recent travels. He had a coworker sick with cold, but no other sick contacts.
Investigations
His initial physical examination revealed scanned speech, impaired Holmes rebound sign on the left outstretched arm and unsteady gait without clear signs of gait ataxia. Liver, spleen and lymph nodes were not palpable and no rashes were noted. Labs revealed positive EBV viral capsid IgM and IgG (at >160 and 114. respectively), but his Epstein-Barr nuclear antigen IgG was negative (<18.00), consistent with a recent infection. IgM antibodies directed against the viral capsid antigen of EBV are useful in confirming the diagnosis of recent EBV infection along with clinical presentation and liver function tests. EBV IgM viral capsid antigen (VCA) titers decrease in most patients after 3–6 months but may persist in low titer for up to 1 year. EBV IgG VCA antibodies rise later than the IgM VCA antibodies but remain elevated with variable titers for life. Liver function tests showed alanine aminotransferase of 169, aspartate aminotransferase of 65, alkaline phosphatase of 189. Alcohol levels were normal; Lyme antibodies were negative. He underwent a brain MRI, which was, as expected in a case of postinfectious cerebellitis, completely normal (figures 1 and 2).
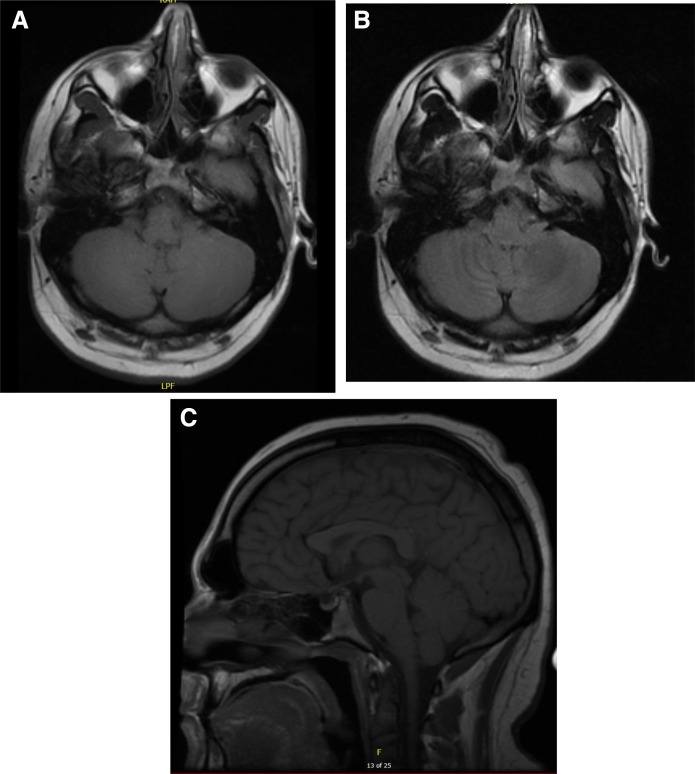
Figure 1.
Brain MRI. (A) Axial precontrast T1, (B) axial T2/FLAIR, (C) sagittal precontrast T1.
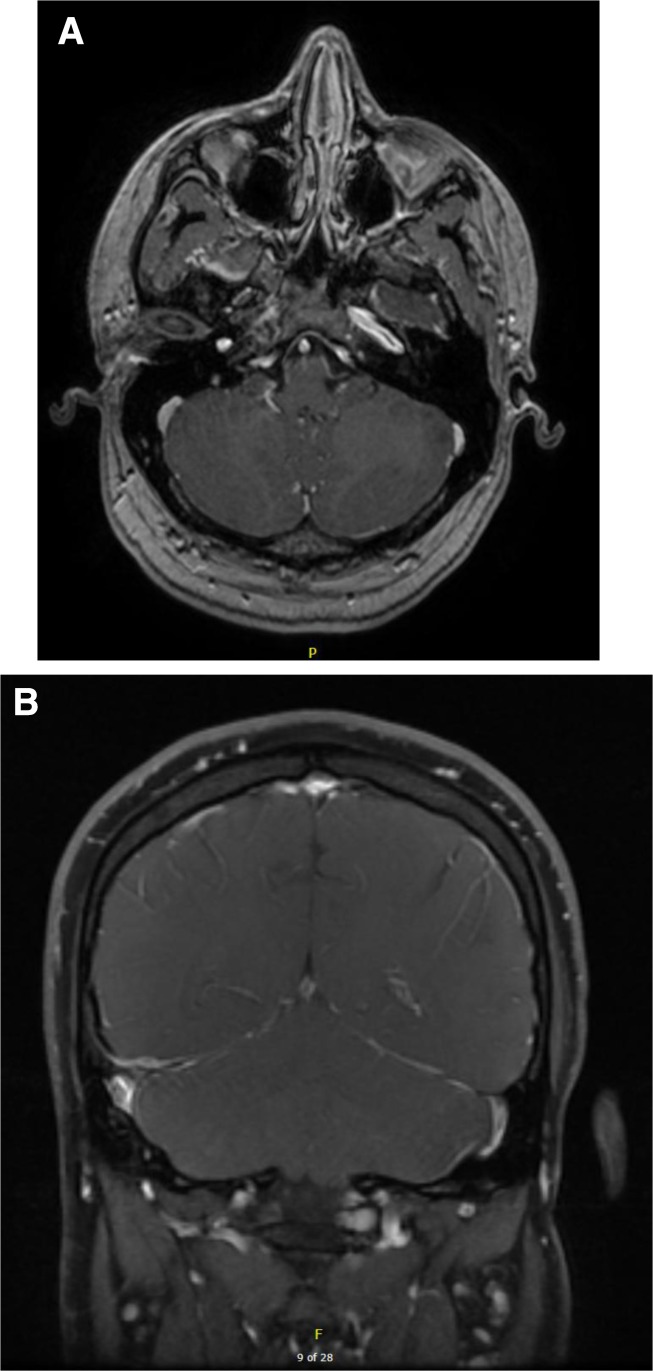
Figure 2.
Brain MRI. (A) Axial postcontrast T1, (B) coronal postcontrast T1.
They are characterised by signs of acute or subacute cerebellar dysfunction and by normal cerebrospinal fluid (CSF) studies, with elevated serum EBV antibodies.1 2 The role of MRI in patients with postinfectious cerebellitis is limited, as the MRI demonstrates no abnormalities in the majority of patients.3 4 Brain single-photon emission computed tomography (SPECT), on the other hand, may be useful in some cases as it might reveal regional perfusion abnormalities. In particular, regional hyperperfusion, which is related to tissue acidosis and necrosis, has been reported, .5–7 Our patient was not evaluated via SPECT, as this test is not routinely administered in these cases at our institution.
Despite his symptoms, he opted to be discharged home with a close neurology follow-up. A few days later, however, he was admitted to the neurology service again with worsening symptoms. A repeat physical examination revealed significant dysarthria, bilateral nystagmus, dysdiadochokinesia—worse on the left—and clear gait ataxia. A lumbar puncture was performed and the results were grossly normal, except for a slightly increased protein count at 55. EBV PCR within the CSF was, as expected, negative.
Treatment
The patient underwent a 5-day course of intravenous immunoglobulins.
Outcome and follow-up
After the initiation of treatment with intravenous immunoglobulins, the patient showed a rapid improvement in all his symptoms and was safely discharged home without the need for additional assistance or physical therapy.
Discussion
Cerebellitis is defined as inflammatory encephalitis limited to the cerebellum.8 9 It is characterised by symptoms of ataxia, nystagmus and dysarthria. Both the acute (infectious) and the subacute (postinfectious) forms of cerebellitis have been reported in children <6 years of age,10 11 but they are rare occurrences in young adults.12 In particular, postinfectious cerebellitis has been observed following many infectious diseases,13 but only a few cases of cerebellitis after EBV mononucleosis appear in literature.14–16 EBV mononucleosis is a viral illness that presents in young adults as a triad of fatigue, pharyngitis and lymphadenopathy. It is generally considered a self-limiting condition; however, neurological manifestations occur in 1% of the cases and include meningitis, encephalitis, transverse myelitis, Guillain-Barre syndrome and ataxia.17–19 In particular, EBV-associated cerebellar ataxias are preceded by infectious mononucleosis by 1–3 weeks. They are characterised by signs of acute or subacute cerebellar dysfunction and by normal CSF studies, with elevated serum EBV antibodies.1 2 The pathophysiology of this syndrome involves antiviral and autoreactive antibodies, rather than a direct viral insult,20 and the autoantibody titers can be increased even before the appearance of cerebellar symptoms. Among others, antineuronal and antitriosephosphate isomerase antibodies have been studied.21 22 The mechanisms underlying the production of such antibodies is still partly unknown but might involve antineuronal antibodies secreted by EBV-transformed B-cells or a mimicry between EBV proteins and neuronal antigens. These observations suggest that therapies directed at the immune response might be effective in treating post-EBV cerebellitis. Corticosteroids, plasmapheresis and intravenous immunoglobulins have been used in acute and subacute (postinfectious) cerebellar ataxias, especially in the paediatric population;3 9 23 24 however, no consensus guidelines have been published for the treatment of these entities. Many reports stress the benign, self-limiting nature of postinfectious cerebellar ataxias;10 13 14 however, residual cognitive and motor deficits can affect patient for months and cases of persistent cerebellar ataxias in adults have been described as well.25 Early intervention with immunotherapy might de facto decrease the severity and duration of illness and improve the patients’ quality of life.26 27 The case presented here, of post-EBV cerebellitis in a young male, reinforces the importance of early recognition and treatment of such patients to prevent adverse outcomes. Ours is one of the few examples of the efficacy of intravenous immunoglobulins for treating this condition.28 The patient presented to the hospital with progressively worsening signs of cerebellitis and demonstrated a dramatic improvement in his symptoms after the first dose of intravenous immunoglobulins. He completed a 5-day treatment course with complete resolution of the initial symptoms and was safely discharged home without additional need for physical or occupational therapy.
Learning points.
Post-Epstein-Barr virus (EBV) cerebellitis is a rare occurrence in adults.
Post-EBV cerebellitis is characterised by ataxia, nystagmus and dysarthria.
Post-EBV cerebellitis is associated with the presence of autoreactive antibodies, in particular, antineuronal antibodies.
Post-EBV cerebellitis is usually a self-limiting condition; however, treatment with intravenous immunoglobulin decreases the severity and duration of the syndrome.
Footnotes
Contributors: ED'A presented the case report. Both authors, ED'A and FK contributed to the final version of the manuscript. CI supervised the project.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Erzurum S, Kalavsky SM, Watanakunakorn C. Acute cerebellar ataxia and hearing loss as initial symptoms of infectious mononucleosis. Arch Neurol 1983;40:760–2. 10.1001/archneur.1983.04050110078016 [DOI] [PubMed] [Google Scholar]
- 2. Ito H, Sayama S, Irie S, et al. . Antineuronal antibodies in acute cerebellar ataxia following Epstein-Barr virus infection. Neurology 1994;44:1506–7. 10.1212/WNL.44.8.1506 [DOI] [PubMed] [Google Scholar]
- 3. Klockgether T, Döller G, Wüllner U, et al. . Cerebellar encephalitis in adults. J Neurol 1993;240:17–20. 10.1007/BF00838440 [DOI] [PubMed] [Google Scholar]
- 4. Hung KL, Liao HT, Tsai ML. Epstein-Barr virus encephalitis in children. Acta Paediatr Taiwan 2000;41. [PubMed] [Google Scholar]
- 5. Park JW, Choi YB, Lee KS. Detection of acute Epstein Barr virus cerebellitis using sequential brain HMPAO-SPECT imaging. Clin Neurol Neurosurg 2004;106:118–21. 10.1016/j.clineuro.2003.10.009 [DOI] [PubMed] [Google Scholar]
- 6. Nara T, Nozaki H, Nishimoto H. Brain perfusion in acute encephalitis: relationship to prognosis studied using SPECT. Pediatr Neurol 1990;6:422–4. 10.1016/0887-8994(90)90013-Q [DOI] [PubMed] [Google Scholar]
- 7. Kao CH, Wang SJ, Mak SC, et al. . Viral encephalitis in children: detection with technetium-99m HMPAO brain single-photon emission CT and its value in prediction of outcome. AJNR Am J Neuroradiol 1994;15:1369–73. [PMC free article] [PubMed] [Google Scholar]
- 8. Ş G, Kurugol Z, Aslan A. A rare cause of childhood Cerebellitis-Influenza infection: a case report and systematic review of literature.. Case Rep Pediatr 2018;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lancella L, Esposito S, Galli ML, et al. . Acute cerebellitis in children: an eleven year retrospective multicentric study in Italy. Ital J Pediatr 2017;43:54 10.1186/s13052-017-0370-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Connolly AM, Dodson WE, Prensky AL, et al. . Course and outcome of acute cerebellar ataxia. Ann Neurol 1994;35:673–9. 10.1002/ana.410350607 [DOI] [PubMed] [Google Scholar]
- 11. Robinson TJ, Glenn MS, Temple RW, et al. . Encephalitis and cerebellar ataxia associated with Epstein-Barr virus infections. Ulster Med J 1980;49:158–64. [PMC free article] [PubMed] [Google Scholar]
- 12. Nussinovitch M, Prais D, Volovitz B, et al. . Post-Infectious acute cerebellar ataxia in children. Clin Pediatr 2003;42:581–4. 10.1177/000992280304200702 [DOI] [PubMed] [Google Scholar]
- 13. Muscat K, Galea R, Vella M. An adult case of acute EBV cerebellitis. Eur J Case Rep Intern Med 2017;4:000519 10.12890/2016_000519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ashraf M. Post-EBV cerebellitis: a very rare complication of infectious mononucleosis. J Med Cases 2014;5 10.14740/jmc1779w [DOI] [Google Scholar]
- 15. Hussain RS, Hussain NA. Ataxia and encephalitis in a young adult with EBV mononucleosis: a case report. Case Rep Neurol Med 2013;2013:1–3. 10.1155/2013/516325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wadhwa NK, Ghose RR. Acute cerebellar ataxia and infectious mononucleosis. Postgrad Med J 1983;59:457–8. 10.1136/pgmj.59.693.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cho TA, Schmahmann JD, Cunnane ME. Case 30-2013 — a 19-year-old man with otalgia, slurred speech, and ataxia. N Engl J Med 2013;369:1253–61. [DOI] [PubMed] [Google Scholar]
- 18. Sawaishi Y, Takada G. Acute cerebellitis. Cerebellum 2002;1:223–8. 10.1080/14734220260418457 [DOI] [PubMed] [Google Scholar]
- 19. Jenson HB. Epstein-Barr virus. Pediatrics in Review 2011;32:375–84. 10.1542/pir.32-9-375 [DOI] [PubMed] [Google Scholar]
- 20. Uchibori A, Sakuta M, Kusunoki S, et al. . Autoantibodies in postinfectious acute cerebellar ataxia. Neurology 2005;65:1114–6. 10.1212/01.wnl.0000178802.38268.1e [DOI] [PubMed] [Google Scholar]
- 21. Go T. Intravenous immunoglobulin therapy for acute cerebellar ataxia. Acta Paediatr 2003;92:504–6. 10.1111/j.1651-2227.2003.tb00587.x [DOI] [PubMed] [Google Scholar]
- 22. Göhlich-Ratmann G, Wallot M, Baethmann M, et al. . Acute cerebellitis with near-fatal cerebellar swelling and benign outcome under conservative treatment with high dose steroids. Eur J Paediatr Neurol 1998;2:157–62. 10.1016/S1090-3798(98)80032-9 [DOI] [PubMed] [Google Scholar]
- 23. Schmahmann JD. Plasmapheresis improves outcome in postinfectious cerebellitis induced by Epstein-Barr virus. Neurology 2004;62:1443 10.1212/01.WNL.0000120752.24980.B3 [DOI] [PubMed] [Google Scholar]
- 24. Van Samkar A, Poulsen MNF, Bienfait HP, et al. . Acute cerebellitis in adults: a case report and review of the literature. BMC Res Notes 2017;10:610 10.1186/s13104-017-2935-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Karunarathne S, Udayakumara Y, Fernando H. Epstein-Barr virus co-infection in a patient with dengue fever presenting with post-infectious cerebellitis: a case report. J Med Case Rep 2012;6:43 10.1186/1752-1947-6-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ariño H, Gresa-Arribas N, Blanco Y, et al. . Cerebellar ataxia and glutamic acid decarboxylase antibodies: immunologic profile and long-term effect of immunotherapy. JAMA Neurol 2014;71:1009–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nanri K, Okita M, Takeguchi M, et al. . Intravenous immunoglobulin therapy for autoantibody-positive cerebellar ataxia. Intern Med Tokyo Jpn 2009;48:783–90. 10.2169/internalmedicine.48.1802 [DOI] [PubMed] [Google Scholar]
- 28. Sener U, Eidelman B. A case of Post-EBV cerebellitis treated with IVIg. Neurology 2017;88:322.27927932 [Google Scholar]