Abstract
Objectives
In 2014–2015, over 400 social housing units were constructed in selected communities in Nunavik and Nunavut, two Inuit regions in northern Canada where housing shortages and poor quality housing are endemic and undermine population health. This paper presents results from a before-and-after study examining the effects of rehousing, i.e., relocating to a newly constructed or pre-existing social housing unit, on psychosocial health and asthma-related symptoms for Inuit adults.
Methods
Baseline data were collected 1–6 months before, and follow-up data 15–18 months after rehousing. Of the 289 participants at baseline, 186 were rehoused. Of the 169 participants eligible at follow-up, 102 completed the study. Self-reported health measures included psychological distress, perceived stress in daily life, perceived control over one’s life, and asthma-related symptoms. Data are analyzed using multilevel models for longitudinal data.
Results
After adjusting for age, sex, and region of residence, participants reported significantly lower levels of psychological distress and perceived stress in daily life, and improved sense of control over their lives 15 to 18 months after rehousing. Participants were also significantly less likely to report asthma-related symptoms at follow-up.
Conclusion
Significant positive health impacts are observed for adults who relocated to newly constructed or pre-existing social housing units. Increasing investments to redress the housing situation across Inuit Nunangat is required, not only to improve living conditions but also to improve the health and well-being of the population.
Keywords: Housing, Intervention, Indigenous Peoples, Inuit
Résumé
Objectifs
En 2014-2015, plus de 400 logements sociaux ont été construits dans certaines communautés au Nunavik et au Nunavut, deux des quatre régions Inuit du nord du Canada où la pénurie de logements, et des conditions inadéquates des logements, sont endémiques et nuisent à la santé de la population. Cet article présente les résultats d’une étude pré-post qui évalue l’impact de déménager dans un logement social nouvellement construit, ou préexistant, sur la santé psychosociale et les symptômes liés à l’asthme chez des adultes Inuit.
Méthodes
Les données ont été recueillies entre 1 et 6 mois avant le déménagement (temps 0; t0), puis au suivi entre 15 à 18 mois après le déménagement. Sur les 289 participants recrutés à t0, 186 ont déménagé. Sur les 169 participants éligibles au suivi, 102 ont complété l’étude. Les mesures de santé autorapportées comprennent la détresse psychologique, le stress perçu dans la vie quotidienne, le contrôle sur la vie, et les symptômes liés à l’asthme. Les données ont été analysées à l'aide de modèles multiniveaux pour données longitudinales.
Résultats
De 15 à 18 mois suivant le déménagement, on observe une diminution significative de la détresse psychologique, du stress perçu dans la vie quotidienne, et des symptômes liés à l’asthme. On note aussi une augmentation significative de la perception du contrôle sur sa vie.
Conclusion
Déménager dans un logement social nouvellement construit, ou préexistant, a un effet positif et significatif sur la santé des Inuit. Augmenter les investissements pour remédier aux conditions inadéquates de logement est nécessaire, non seulement pour améliorer les conditions de vie, mais aussi pour améliorer la santé et le bien-être de la population.
Mots-clés: Logement, Intervention, Populations autochtones, Inuit
Introduction
In Canada, 13% of households are in “core housing need”, meaning their houses require major repairs, are inappropriate in size, and/or are unaffordable (Statistics Canada 2017a). In Nunavut, one of the four Inuit land claims regions, 37% of the population is in core housing need (Government of Canada 2017), a situation that is undermining population health (Knotsch and Kinnon 2011).
The association between poor housing and poor health is well known, with effects across the lifespan (Oswald and Wahl 2004; Weitzman et al. 2013). Evidence linking housing conditions to Indigenous Peoples’ health is mostly focused on the association between overcrowding, poor indoor air quality, higher rates of tuberculosis infections (Clark et al. 2002; Khan et al. 2016), and respiratory health outcomes and hospitalizations, especially among children (Banerji et al. 2009; Kovesi et al. 2007; Bailie et al. 2010; Karron et al. 1999; Koch et al. 2002). Recent cross-sectional studies indicate that living in crowded conditions is associated with elevated physiological stress among Inuit adults, especially among women (Riva et al. 2014b), and with lower mental wellness among Inuit youth aged 15–30 (Gray et al. 2016). In Greenland, feeling depressed is more likely to be reported by Inuit adults living in crowded households, with the association being more important for women than for men (Riva et al. 2014a). Among adolescents in Nunavik, however, a prospective study did not report significant association between household crowding in childhood and psychological distress in adolescence (Pepin et al. 2018).
In general populations, interventions aiming to improve housing conditions show positive health effects, but these do not always reach statistical significance (Thomson et al. 2013). A Cochrane review of housing interventions identified studies (with a range of designs) examining the health impacts of rehousing interventions–defined as relocating to a different dwelling–or improvement in indoor housing conditions due to improved structure or housing fabric (Thomson et al. 2013). Studies reported improvements in self-rated general health (Barnes 2003), whereas associations with respiratory health were mixed; one study reported significant reduction in asthma and bronchial symptoms in adults (Ambrose 2000). In a housing relocation program for low-income women, improvement in housing quality, and especially reduction in crowding, predicted improvement in post-move psychological distress (Wells and Harris 2007). After moving to a new dwelling, gains in space and privacy (proxy measures of crowding) were significantly associated with improvements in health for families with dependent children (Kearns et al. 2011).
There are few studies assessing the impacts of rehousing interventions on the health of Indigenous Peoples. One exception is the Housing Infrastructure and Child Health (HICH) study examining the association between improvement in housing infrastructure and reduction in common childhood illnesses in 10 Indigenous communities in Australia (Bailie et al. 2012). Although results show an improvement in infrastructure in the house, there was only a marginal reduction in household crowding, and no effect on childhood illness. The authors concluded that housing improvement programs that do not reduce crowding and that are not supported by social, behavioural, and community-wide programs have limited potential to improve health in communities facing very high levels of overcrowding (as was the case for the 10 communities in the HICH study; Bailie et al. 2012; Bailie et al. 2011). Longitudinal and experimental evidence of the rehousing–health association in Indigenous contexts is lacking.
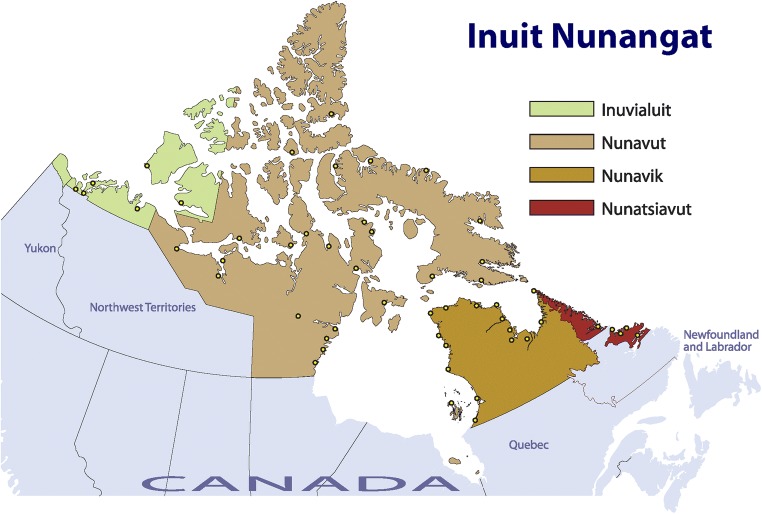
In 2014–2015, over 400 social housing units were constructed in selected communities in Nunavik and Nunavut, two of the four regions in Inuit Nunangat (Fig. 1). The impending shift in housing conditions of a relatively large number of people presented an opportunity to assess the health impacts of social housing construction. In this paper, we examine the effect of rehousing on asthma-related symptoms and psychosocial health for Inuit adults. A secondary objective is to examine differential effects by sex.
Fig. 1.
Map of Inuit Nunangat. Source: Inuit Tapiriit Kanatami. Available at: https://www.itk.ca/wp-content/uploads/2016/07/InuitNunaat_Basic_0.pdf
Methods
The context of the intervention
Nunavik is the Inuit territory in the northern part of the province of Quebec in Canada. The Nunavik population of 13,000 live in 14 coastal communities ranging in size from 209 to 2754 inhabitants. Nunavut is the Inuit territory in northern Canada, where 35,944 people live in 25 communities ranging from 129 to 7740 inhabitants. In Nunavik and Nunavut, there are no roads connecting the communities among themselves, or with southern population centres.
The housing market is largely subsidized, with over 80% of the population in Nunavut and Nunavik living in social (subsidized) housing at the 2016 Census (Statistics Canada 2017b). Recent housing needs surveys estimate a housing shortfall of about 900 units in Nunavik (Société d’habitation du Québec 2014) and 3600 units in Nunavut (Nunavut Housing Corporation 2012). Between 2011 and 2016, Nunavik and Nunavut saw their population increase by about 10% compared with 5% for Canada; one third of the population is under 15 years of age, compared with 17% for Canada (Statistics Canada 2017b). The young and rapidly growing population creates ongoing pressure for the construction of new housing, further compounded by the short construction season (May to December) and high cost of construction (materials shipped by sealift; fly-in labour).
In 2014 and 2015, 216 social housing units were constructed in eight communities in Nunavik, and 210 units in 12 communities in Nunavut. Construction included a mix of one-, two-, and four-bedroom houses and apartments in multiplexes (5 to 10 apartments units) accommodating single-person, small, and large family households. The number of new units constructed in the communities ranged from 5 to 30. The intervention studied is the “rehousing” of adult tenants who are on the waitlist for social housing. Tenants can be rehoused to a newly constructed house or apartment (unit) or to a pre-existing unit that became available for new tenants to move in.
In both regions, new housing units are allocated first to communities where the housing shortage is most acute. Then, the local housing committee allocates units to applicants most in need, where need is defined by a point-based system set according to specific criteria such as low income, number of dependent children, living in overcrowded dwellings, and social problems at home. When tenants are informed they have been allocated a house, they usually only have a few days (sometimes a few weeks) to move. New houses come equipped with a refrigerator and cooking range, but tenants have to acquire other appliances and furniture. In Nunavut, tenants pay monthly rent on a geared-to-income basis. In Nunavik, rent is calculated according to a formula that considers dwelling size and income.
Study design
In this prospective observational (uncontrolled) study, baseline data were collected one to 6 months before rehousing, and follow-up data were collected 15 to 18 months after rehousing. This time to follow-up is longer than most rehousing intervention studies (Thomson et al. 2013) and is likely to provide enough time to observe changes in health (Petticrew et al. 2009). The time between baseline data collection, rehousing, and follow-up data collection varied because of the high cost of data collection which required that travel to communities happened at the same time, and because of climatic events delaying housing construction in some communities.
Baseline data were collected in the Fall 2014 in Nunavik and in the Spring 2015 in Nunavut. In Nunavik, households were recruited in the six communities where new social housing units were being constructed in 2014. In Nunavut, households were recruited in six communities where a larger number of housing units were slated for construction in 2015. In each community, households ranked at the top of the waitlist for social housing, i.e., those who were most likely to move, were recruited by local housing officers. Households were oversampled by 25% to account for the possibility that not everyone met at baseline would be moving (for example, in communities where 30 new units were constructed, we recruited 38 households to the study). At recruitment, participants did not know if they would be moving to a new house. From the 357 eligible households at baseline, 241 households were recruited. Within households, all adults aged ≥ 18 years were invited to participate. A total of 289 adults were recruited, for a participation rate of 68%.
Of the 289 participants, 186 (64.4%) were rehoused. Of these, 82 (44%) were rehoused to a newly constructed unit, and 98 (53%) to a unit that was already built but became available (information on the type of house was missing for six participants). Fifteen participants were not eligible for post-moving assessments because they had moved houses once or more following the initial move, or had moved to another community; two participants were deceased. During follow-up data collection (Nunavik: Spring 2016; Nunavut: Fall 2016 and Spring 2017), every attempt was made to contact participants. A refusal was deemed as such after three contacts. The high cost of data collection prevented the research team from returning to the communities where participants were out of town when follow-up data collection was underway (n = 16 eligible participants were lost at follow-up for this reason). Of the 169 participants eligible at follow-up, 102 completed the study.
The same questionnaires were administered face to face at baseline and follow-up. In each community, local Inuit research assistants were recruited to contact participants, schedule interviews, and provide interpretation when needed. Data collection took place in a neutral environment (e.g., rented rooms at the municipality office). The Household Questionnaire was administered to the main household respondent only, normally the person whose name was on the waitlist; it collected information on structural and material housing conditions. All participants answered the Individual Questionnaire, which collected health, demographic, and socio-economic information. Questionnaires were pilot-tested with Inuit living in Nunavik, Nunavut, and in Quebec City. Questionnaires were mostly administered in English, but were also administered in Inuktitut or Inuinnaqtun (hereafter Inuktut, a global term referring to the Indigenous language spoken by Inuit in Canada). As compensation, participants received a $20 voucher from the local store and the chance to win one of two iPads.
Measures
Five health measures were selected based on their plausible associations with housing conditions. Asthma-related outcomes were assessed using the Asthma Score, an index with five questions denoting the presence or absence of symptoms in the past year (Sunyer et al. 2007). The index was dichotomized to contrast participants with ≥ 1 symptom(s) to those without asthma symptoms.
Self-rated health is a predictor of morbidity and mortality in general populations (Idler and Benyamini 1997), and is associated with risk factors for chronic disease among Inuit (Saudny et al. 2012). Self-rated health was dichotomized to contrast participants reporting their health as excellent, very good, or good, vs. participants reporting their health as fair or poor.
Psychological distress was measured using the six-item Kessler psychological distress scale (Kessler et al. 2002), previously used in Inuit health surveys (Rochette and Blanchet 2007). Questions assessed the frequency of symptoms of mental illness or nonspecific psychological distress in the past month with answers scored on a 5-point scale. The overall score ranges from 0 to 24, with higher scores denoting higher levels of distress. In general populations, a score of 13 points or higher indicates serious psychological distress.
Stress in daily life was measured using the 10-item Perceived Stress Scale (PSS) (Cohen et al. 1983), which correlates with cortisol levels, a biological marker of stress in general populations (Pruessner et al. 1999). Questions assess frequency of feelings and thoughts during the last month, with answers rated on a 5-point scale. PSS scores range from 0 to 40; higher scores indicate higher stress.
Finally, we considered perceived control over one’s life, or mastery, as a potential outcome of rehousing. Mastery is defined as “the extent to which an individual regards their life chances as being under their personal control rather than fatalistically ruled” (Pearlin and Schooler 1978). Mastery was assessed using the Pearlin Mastery scale (Pearlin and Schooler 1978), with modified response options (five rather than four categories). Responses to each of the seven items are scored on a 5-point scale, with scores ranging from 7 to 35; higher scores indicate higher mastery.
Statistical analyses
Data were analyzed with multilevel models for longitudinal data (Singer and Willett 2003) using Stata v14 software (StataCorp 2010). Multilevel models account for the hierarchical structure of the database, i.e., repeated measures clustered in individuals clustered in households and communities. They also consider the non-independence of observations and are robust to unbalanced datasets, e.g., single-participant households and households with multiple participants (Singer and Willett 2003). Age, sex, and region of residence were considered as covariates in all statistical models. Smoking status (people reporting being a current cigarette smoker vs. not) was considered in models for asthma-related symptoms. Adjusting for household financial situation or for moving into a newly built vs. a pre-existing unit did not influence the results; these variables were therefore not included in the final models.
Ethical implications
This project was developed and conducted in collaboration with territorial, regional, and provincial organizations responsible for housing, public health, and preserving Inuit values and practices. The project was approved and supported by the mayors of all communities involved, the Nunavik Nutrition and Health Committee, and the Nunavut Research Institute. It received ethical approval from the Comité d’éthique de la recherche du CHU de Québec and from McGill University Internal Review Board. At recruitment, potential participants were informed that their participation in the project (or refusal to participate) would not affect their rank on the waitlist, their current housing situation, or whether or not they would get to move. All participants provided informed written consent.
Results
More women than men participated in the study, the average age of participants was 31 years, and more than half reported being in a relationship (Table 1). Mostly speaking Inuktut at home was reported by 57% of participants. At baseline, most lived in social housing, and one third had been on the waitlist for social housing for four years or more. On average, there were 6.5 people per house. Almost 80% of participants were smokers. One in four participants reported having completed their secondary schooling or partial technical training, and 16% reported having some post-secondary education. Despite 60% of participants being employed, almost 60% reported an annual personal income below $20,000. These statistics speak to the difficult socio-economic conditions prevailing in the Canadian Arctic.
Table 1.
Socio-demographic characteristics and housing conditions of the 289 participants at baseline
| Socio-demographic characteristics | n (%) | |
|---|---|---|
| Age | 18–25 years | 110 (38.1) |
| 26–35 years | 103 (35.6) | |
| 36–45 years | 34 (11.8) | |
| ≥ 46 years | 42 (14.5) | |
| Sex | Women | 163 (56.4) |
| Region of residence | Nunavik | 134 (46.4) |
| Nunavut | 155 (53.6) | |
| Language mostly used at homea | Mostly Inuktut | 138 (57.3) |
| Mix of Inuktut and English or French | 52 (21.7) | |
| Mostly English or French | 49 (20.3) | |
| Marital status | Single | 128 (44.3) |
| In a relationship | 159 (55.0) | |
| Current smoker | 229 (79.2) | |
| Personal income | < $20,000 | 170 (58.8) |
| $20,000–$40,000 | 58 (20.1) | |
| > $40,000 | 39 (13.5) | |
| In employment | 174 (60.2) | |
| Highest education level | Less than secondary school | 158 (54.7) |
| Secondary school completed or technical training | 73 (25.3) | |
| Post-secondary education (with or without diploma) | 47 (16.3) | |
| Housing conditionsa | ||
| Lives in social housing | 188 (78.0) | |
| Time on waitlist | < 1 year | 32 (13.3) |
| 1 to < 2 years | 40 (16.6) | |
| 2 to < 4 years | 84 (34.9) | |
| ≥ 4 years | 79 (32.8) | |
| Average number of people in the house (mean (se)) | 6.5 (0.2) | |
aData are from the household questionnaire, n = 241 households; other data are from the individual questionnaire
There were few differences in baseline socio-demographic and health measures between those who did not move and those who were rehoused and completed the study (Table 2). Among participants who were rehoused, the only difference was for perceived stress in daily life, which was significantly higher at baseline for those who did not complete the study vs. those who did. Selection bias appears to be limited in our study.
Table 2.
Comparison of socio-demographic characteristics and health measures at baseline between (a) participants who did not move vs. those who were rehoused and completed the study and (b) participants who were rehoused and did not complete the study vs. those who completed the study
| (a) Comparing baseline values between participants who: | (b) Comparing baseline values between participants who were rehoused and: | |||||
|---|---|---|---|---|---|---|
| Were not rehoused (n = 103) | Were rehoused and completed the study (n = 102) | p valuea | Did not complete the study (n = 82) | Completed the study (n = 102) | p value | |
| Age (mean (se)) | 32.9 (1.3) | 31.4 (1.0) | 0.354 | 29 (1.0) | 31.4 (1.0) | 0.091 |
| Women (n (%)) | 57 (55.3) | 58 (56.9) | 0.826 | 48 (58.5) | 58 (56.9) | 0.819 |
| Income (n (%)) | 0.325 | 0.710 | ||||
| < $20,000 | 65 (63.1) | 59 (57.8) | 44 (53.7) | 59 (57.8) | ||
| $20,000–$40,000 | 16 (15.5) | 22 (21.6) | 20 (24.4) | 22 (21.6) | ||
| > $40,000 | 12 (11.7) | 16 (15.7) | 11 (13.4) | 16 (15.7) | ||
| Missing | 10 (9.7) | 5 (4.9) | 7 (8.5) | 5 (4.9) | ||
| Presence of ≥ 1 asthma-related symptom(s) (n (%)) | 36 (35.3) | 47 (46.1) | 0.221 | 35 (42.7) | 47 (46.1) | 0.825 |
| Self-rated health (n (%)) | 0.891 | 0.424 | ||||
| Poor or fair | 27 (26.2) | 29 (28.4) | 19 (23.2) | 29 (28.4) | ||
| Good, very good, or excellent | 70 (68.0) | 72 (70.6) | 62 (75.6) | 72 (70.6) | ||
| Psychological distress (mean (se)) | 8.2 (0.6) | 8.3 (0.5) | 0.881 | 8.5 (0.7) | 8.3 (0.5) | 0.819 |
| Serious psychological distress (n (%)) | 27 (26.2) | 25 (24.5) | 0.528 | 16 (19.5) | 25 (24.5) | 0.481 |
| Perceived stress (mean (se)) | 17.9 (0.6) | 16.9 (0.6) | 0.240 | 18.9 (0.6) | 16.9 (0.6) | 0.031 |
| Mastery (mean (se)) | 23.0 (0.5) | 23.4 (0.5) | 0.536 | 22.5 (0.4) | 23.4 (0.5) | 0.154 |
ap values generated using Student’s t tests for continuous variables and chi-square tests for categorical variables
Values for asthma-related symptoms and psychosocial health for the 289 participants at baseline, and crude change in these measures between baseline and follow-up for the 102 participants who completed the study, are shown in Table 3. While significantly fewer participants reported asthma-related symptoms at follow-up, there was no change in self-rated health. The overall mean score of psychological distress and the proportion of participants showing serious psychological distress were significantly lower among participants at follow-up. Perceived stress in daily life was also significantly lower at follow-up. The mean score for mastery was significantly higher at follow-up.
Table 3.
Health measurements among the 289 participants at baseline and for the 102 participants who completed the study
| 289 participants at baseline | 102 participants who completed the study* | |||
|---|---|---|---|---|
| Baseline | Follow-up | p value for change | ||
| Presence of following symptoms in past year (n (%)) | ||||
| Wheezing or whistling in chest | 67 (23.2) | 28 (27.5) | 16 (15.7) | 0.011 |
| Waking up with a feeling of tightness in chest first thing in the morning | 54 (18.7) | 23 (22.5) | 15 (14.7) | 0.185 |
| Attack of shortness of breath that came on during the day when not doing anything demanding physically | 43 (14.9) | 18 (17.6) | 12 (11.8) | 0.210 |
| Attack of shortness of breath that came on after stopped exercising | 57 (19.7) | 22 (21.6) | 15 (14.7) | 0.210 |
| Waking up at night by an attack of shortness of breath | 26 (9.0) | 13 (12.7) | 9 (8.8) | 0.424 |
| Presence of ≥ 1 asthma symptom(s) (n (%)) | 120 (41.5) | 47 (46.1) | 33 (32.4) | 0.013 |
| Self-rated health (n (%)) | ||||
| Poor or fair | 77 (26.6) | 29 (28.4) | 21 (20.6) | 0.144 |
| Good, very good, or excellent | 204 (70.6) | 72 (70.6) | 80 (78.4) | |
| Psychological distress (mean (se)) | 8.3 (0.3) | 8.3 (0.5) | 5.9 (0.5) | < 0.001 |
| Serious psychological distress (n (%)) | 69 (23.9) | 25 (24.5) | 11 (10.8) | 0.009 |
| Perceived stress in daily life (mean (se)) | 17.9 (0.4) | 16.9 (0.6) | 15.5 (0.6) | 0.023 |
| Mastery (mean (se)) | 23.1 (0.3) | 23.4 (0.5) | 24.9 (0.5) | 0.003 |
*p values generated from marginal homogeneity tests for categorical variables, and paired t tests for continuous variables
Table 4 presents results of unadjusted and adjusted multilevel models of change between baseline and follow-up for the selected health measures. In models adjusted for age, sex, and region, the odds of reporting asthma-related symptoms were significantly lower after the move. Mean scores of psychological distress and perceived stress in daily life were significantly lower by, respectively, 2.5 and 1.4 points, 15–18 months after rehousing. Perceived mastery significantly improved from baseline to follow-up by 1.5 points. There was no significant effect on self-rated health nor effect modification by sex (results not presented).
Table 4.
Unadjusted and adjusted linear and logistic multilevel regression models of change in psychosocial health and asthma-related symptoms for the 102 participants who completed the study
| Unadjusted model | Adjusted modela | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Presence of asthma-related symptomsb | 0.4 (0.2–0.8)* | 0.4 (0.2–0.8)* |
| Coeff (se) | Coeff (se) | |
| Psychological distress | − 2.4 (0.6)*** | − 2.5 (0.6)*** |
| Perceived stress | − 1.5 (0.7)* | − 1.4 (0.7)* |
| Mastery | 1.5 (0.5)** | 1.5 (0.5)** |
aModels adjusted for age, sex, and region; bModel further adjusted for smoking status. *p < 0.05; **p < 0.01; ***p < 0.001
Discussion
Results of this study show that, 15–18 months after rehousing, participants presented with significantly reduced scores of psychological distress and perceived stress in daily life, and improved sense of control over their lives. They were also less likely to report asthma-related symptoms. These results, similar for men and women, support those of other studies conducted in general populations showing improved mental health (Wells and Harris 2007; Kearns et al. 2011) and respiratory health (Ambrose 2000) for people moving to a new house.
Our results, however, differ from those of the Housing Infrastructure and Child Health (HICH) study in Australia, where there was an average of 11 people per dwelling. The number of houses built in the communities increased the local housing stock only by about 10%; the overall reduction in crowding in HICH was therefore relatively small. As most families were still living in crowded conditions at follow-up, this could explain why no effect on childhood illness was observed (Bailie et al. 2012, 2011). For the 102 participants who completed the study, there was an average of 6.9 persons per household at baseline, which is considerably lower than the average in the HICH study. At follow-up, the average number of people per household was reduced to 3.3 (Riva et al. 2019). This significant reduction in crowding could explain the health improvements observed in our study.
Other possible pathways explaining the observed improvements in health measures could be through changes in thermal comfort and psychosocial benefits of the house. The Housing, Insulation and Health study is a cluster-randomized trial of insulating existing houses in low-income communities in New Zealand (Howden-Chapman et al. 2007). Insulation was significantly associated with warmer and drier houses, which resulted in improved self-rated health and decreased wheezing, days off school and work, and visits to general practitioners. In our study, we observed significant improvements in thermal comfort (e.g., relative humidity and protection from outside climate) after rehousing (Riva et al. 2019) which may be associated with improvement in asthma-related symptoms and possibly with mental health (Howden-Chapman et al. 2007). In the Housing And Regeneration Project (SHARP) study in Scotland, Kearns et al. reported that, after rehousing, gains in house-related psychosocial benefits (e.g., feelings of autonomy, control, security, privacy, and status) were significantly associated with improvements in mental health, notably for families with dependent children (Kearns et al. 2011). Considering psychosocial factors associated with the house, such as mastery, might be especially relevant pathways to consider in Indigenous contexts given colonial housing policy.
Findings of this study indicate that rehousing, made possible by social housing construction in Inuit Nunangat, can have multiple implications for health and well-being for those who move. This evidence provides important information to guide future research exploring whether health improvements observed are associated with reduction in crowding, improvements in thermal comfort, and/or in psychosocial benefits associated with the house.
Strengths and limitations
Whereas the prospective design is a strength, evidence for the causal relationship between housing conditions and health would have been strengthened with a control group. In natural experiment studies, such as this rehousing study, having comparable control and intervention groups is feasible (Howden-Chapman et al. 2007), but is complex, difficult, and costly to operationalize (Petticrew et al. 2016). In the geographically remote context of this study, budgetary considerations limited the possibility of having a control group. Ethical considerations were also given careful attention. The substantial housing backlog and the high demand for housing in Nunavik and Nunavut means that the right to an adequate shelter (United Nations Human Rights Office of the High Commissioner 1976) is not enjoyed by many. The intervention, hypothesized to improve living conditions and health outcomes, could not be attributed to all participants at baseline nor at different levels of intensity. Having a control group for whom “treatment as usual” is waiting several more months before rehousing (if rehousing at all) was unethical. Other limitations include potential measurement, response, recall and repeated testing biases, and regression towards the mean. Participants recruited to the study were not randomly selected to be representative of the population in Nunavik and Nunavut. However, the inclusion of multiple communities in two regions with different housing governance structures enhances the potential generalizability of our findings to other regions in Inuit Nunangat.
Conclusion
Results of this project indicate that social housing construction in Inuit Nunangat has significant and positive health impacts for those who relocate to a new or already existing dwelling. This evidence is timely. In its recent National Housing Strategy (Government of Canada 2017), Canada has committed to large-scale investments in housing for Indigenous communities across the country. Increasing investments is needed to improve not only living conditions but also the health of the whole population and to reduce the health gap with the rest of the Canadian population.
Assessing the impacts of housing interventions in remote, isolated, and/or sparsely populated Indigenous communities in Canada is possible providing involvement and support of Indigenous organizations and local communities, and sufficient budget. In the coming years, some Indigenous communities in Canada will see investments in housing as per the federal government commitment through the National Housing Strategy (Government of Canada 2017). Not all investments will be for the construction of social housing. Different modes of tenure (private, rent-to-own) might be explored as well as retrofitting of dwellings to improve structural integrity and energy efficiency. Whether or not these will have an impact on Indigenous Peoples’ health and well-being remains to be established. Evaluation studies of these housing initiatives are required to strengthen the evidence base to support Indigenous organizations and governments in making their own decisions with regard to housing in their communities (Inuit Tapiriit Kanatami 2019).
Acknowledgements
This study was conducted in collaboration with the following organizations which reviewed the article prior to submission: Kativik Municipal Housing Bureau, Kativik Regional Government, Nunavik Regional Board of Health and Social Services, Société d’habitation du Québec, Nunavut Housing Corporation, Government of Nunavut Department of Health, Nunavut Tunngavik Incorporated. We acknowledge the collaboration of Inuit research assistants, local housing committees and managers, and mayors, without whom this study would not have been possible. We thank participants who generously gave their time to participate in the project. We acknowledge the contribution of other co-researchers on this project, the statistical advice of Jose Correa at McGill, and the contribution of graduate students who assisted with data collection.
Funding
This study is funded by the Institute of Indigenous Peoples Health of the Canadian Institutes of Health Research (Grant No. GIR134230) and by ArcticNet, a Network of Centres of Excellence of Canada. This research was undertaken, in part, thanks to funding from the Canada Research Chairs program. Karine Perreault is supported by a Doctoral Research Award from the Canadian Institutes of Health Research.
Compliance with ethical standards
The project was approved and supported by mayors of all communities involved, the Nunavik Nutrition and Health Committee, and the Nunavut Research Institute. It received ethical approval from the Comité d’éthique de la recherche du CHU de Québec and from McGill University Internal Review Board.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ambrose, P. (2000). A drop in the ocean: the health gain from the Central Stepney SRB in the context of national health inequalities. University of Brighton: Brighton: The Health and Social Policy Research Centre.
- Bailie, R., Stevens, M., McDonald, E., Brewster, D., & Guthridge, S. (2010). Exploring cross-sectional associations between common childhood illness, housing and social conditions in remote Australian Aboriginal communities. BMC Public Health, 10, 147. [DOI] [PMC free article] [PubMed]
- Bailie R, McDonald EL, Stevens M, Guthridge S, Brewster DR. Evaluation of an Australian indigenous housing programme: community level impact on crowding, infrastructure function and hygiene. J Epidemiol Community Health. 2011;65:432–437. doi: 10.1136/jech.2009.091637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailie R, Stevens M, McDonald E. The impact of housing improvement and socio-environmental factors on common childhood illnesses: a cohort study in Indigenous Australian communities. J Epidemiol Community Health. 2012;66:821–831. doi: 10.1136/jech.2011.134874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerji A, Greenberg D, White L, Macdonald W, Saxton A, Thomas E, et al. Risk factors and viruses associated with hospitalization due to lower respiratory tract infections in Canadian Inuit children: a case-control study. Pediatr Infect Dis J. 2009;28:1–5. doi: 10.1097/INF.0b013e318184ef02. [DOI] [PubMed] [Google Scholar]
- Barnes, R. (2003). Housing and health uncovered. London: Shepherd’s Bush Housing Association 2003. Available at: https://www.housinglin.org.uk/_assets/Resources/Housing/Housing_advice/Housing__Health_Uncovered.pdf. Accessed 19 Sept 2019.
- Clark M, Riben P, Nowgesic E. The association of housing density, isolation and tuberculosis in Canadian First Nations communities. Int J Epidemiol. 2002;31:940–943. doi: 10.1093/ije/31.5.940. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Government of Canada. (2017). Canada’s National Housing Strategy. A place to call home. Available at: http://publications.gc.ca/collections/collection_2018/edsc-esdc/Em12-54-2018-eng.pdf. Accessed 19 Sept 2019.
- Gray AP, Richer F, Harper S. Individual- and community-level determinants of Inuit youth mental wellness. Can J Public Health. 2016;107:e251–e257. doi: 10.17269/CJPH.107.5342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden-Chapman Philippa, Matheson Anna, Crane Julian, Viggers Helen, Cunningham Malcolm, Blakely Tony, Cunningham Chris, Woodward Alistair, Saville-Smith Kay, O'Dea Des, Kennedy Martin, Baker Michael, Waipara Nick, Chapman Ralph, Davie Gabrielle. Effect of insulating existing houses on health inequality: cluster randomised study in the community. BMJ. 2007;334(7591):460. doi: 10.1136/bmj.39070.573032.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Inuit Tapiriit Kanatami (2019). Inuit Nunangat Housing Strategy. Available at: https://www.itk.ca/wp-content/uploads/2019/04/2019-Inuit-Nunangat-Housing-Strategy-English.pdf. Accessed 19 Sept 2019.
- Karron RA, Singleton RJ, Bulkow L, Parkinson A, Kruse D, DeSmet I, et al. Severe respiratory syncytial virus disease in Alaska native children. J Infect Dis. 1999;180:41–49. doi: 10.1086/314841. [DOI] [PubMed] [Google Scholar]
- Kearns, A., Whitley, E., Mason, P., Petticrew, M., & Hoy, C. (2011). Material and meaningful homes: mental health impacts and psychosocial benefits of rehousing to new dwellings. Int J Public Health, 56(6), 597–607. [DOI] [PubMed]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-LT, et al. Short screening scales to monitor population prevalences and trends in nonspecific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Khan FA, Fox GJ, Lee RS, Riva M, Benedetti A, Proulx J-F, et al. Housing and tuberculosis in an Inuit village in northern Quebec: a case–control study. CMAJ Open. 2016;4:E496–E506. doi: 10.9778/cmajo.20160049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knotsch, C., & Kinnon, D. (2011). If not now … when? Addressing the ongoing Inuit housing crisis in Canada. Ottawa: National Aboriginal Health Organization. Available at: https://ruor.uottawa.ca/bitstream/10393/30246/1/2011_Inuit-Housing-Crisis-Canada-FullReport.pdf. Accessed 19 Sept 2019.
- Koch A, Sorensen P, Homoe P, Mølbak K, Pedersen FK, Mortensen T, et al. Population-based study of acute respiratory infections in children, Greenland. Emerg Infect Dis. 2002;8:586–593. doi: 10.3201/eid0806.010321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovesi T, Gilbert N, Stocco C, Fugler D, Dales R, Guay M, et al. Indoor air quality and the risk of lower respiratory tract infections in young Canadian Inuit children. Can Med Assoc J. 2007;177:155–160. doi: 10.1503/cmaj.061574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunavut Housing Corporation. (2012). Igluliuqatigiilauqta “Let’s Build a Home Together”. Framework for the GN Long-Term Comprehensive Housing and Homelessness Strategy. Available at: http://blueprintforaction.ca/docs/other/nhc-homelessness-en.pdf. Accessed 19 Sept 2019.
- Oswald F, Wahl H. Housing and health in later life. Rev Environ Health. 2004;19:223–252. [PubMed] [Google Scholar]
- Pearlin L, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. doi: 10.2307/2136319. [DOI] [PubMed] [Google Scholar]
- Pepin, C., Muckle, G., Moisan, C., Forget-Dubois, N., & Riva, M. (2018). Household overcrowding and psychological distress among Nunavik Inuit adolescents: a longitudinal study. Int J Circumpolar Health, 77, 1. [DOI] [PMC free article] [PubMed]
- Petticrew M, Kearns A, Mason P, Hoy C. The SHARP study: a quantitative and qualitative evaluation of the short-term outcomes of housing and neighbourhood renewal. BMC Public Health. 2009;9:415. doi: 10.1186/1471-2458-9-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petticrew M, Viehbeck S, Cummins S, Lang T. [Same words, different meanings: how epidemiological terminology struggles with population health intervention research]. Alternate title: À mêmes mots, sens différents--les difficultés de la terminologie épidémiologique avec la recherche en interventions en santé des populations. Rev Epidemiol Sante Publique. 2016;64:S43–S54. doi: 10.1016/j.respe.2016.02.004. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Hellhammer DH, Kirschbaum C. Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 1999;61:197–204. doi: 10.1097/00006842-199903000-00012. [DOI] [PubMed] [Google Scholar]
- Riva M, Lytken Larsen CV, Bjerregaard P. Household crowding and psychosocial health among Inuit in Greenland. Int J Public Health. 2014;59:739–748. doi: 10.1007/s00038-014-0599-x. [DOI] [PubMed] [Google Scholar]
- Riva M, Plusquellec P, Juster R-P, Laouan-Sidi EA, Abdous B, Lucas M, et al. Household crowding is associated with higher allostatic load among Inuit. J Epidemiol Community Health. 2014;68:363–369. doi: 10.1136/jech-2013-203270. [DOI] [PubMed] [Google Scholar]
- Riva, M., Perreault, K., Dufresne, P., Fletcher, C., Muckle, M., Potvin, L., et al. (2019). Social housing construction and improvements in housing conditions for Inuit in Northern Canada. In press.
- Rochette, L., & Blanchet, C. (2007). Qanuippitaa? How are we? Methodological report. Available at: http://www.inspq.qc.ca/pdf/publications/692_esi_methodological_report.pdf. Accessed 19 Sept 2019.
- Saudny, H., Cao, Z., & Egeland, G. M. (2012). Poor self-reported health and its association with biomarkers among Canadian Inuit. Int J Circumpolar Health, 71, 1. [DOI] [PMC free article] [PubMed]
- Singer JD, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. Oxford: Oxford University Press; 2003. [Google Scholar]
- Société d’habitation du Québec (2014). Housing in Nunavik. Available at: http://www.habitation.gouv.qc.ca/fileadmin/internet/documents/English/logement__nunavik_2014.pdf. Accessed 19 Sept 2019.
- StataCorp. (2010). Stata/SE 11.0 for Windows. College Station, TX, USA.
- Statistics Canada. (2017a). Core housing need, 2016 Census. Available at: http://www12.statcan.gc.ca/census-recensement/2016/dp-pd/chn-biml/index-eng.cfm. Accessed 19 Sept 2019.
- Statistics Canada. (2017b). Nunavik and Nunavut Census Profile, 2016 Census. For Nunavik, available at: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=HR&Code1=2417&Geo2=PR&Code2=24&Data=Count&SearchText=Region%20du%20Nunavik&SearchType=Begins&SearchPR=01&B1=All&GeoLevel=PR&GeoCode=2417&TABID=1. For Nunavut, available at: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=HR&Code1=6201&Geo2=PR&Code2=24&Data=Count&SearchText=Nunavut&SearchType=Begins&SearchPR=01&B1=All&GeoLevel=PR&GeoCode=6201&TABID=1. Accessed 19 Sept 2019.
- Sunyer J, Pekkanen J, Garcia-Esteban R, Svanes C, Künzli N, Janson C, et al. Asthma score: predictive ability and risk factors. Allergy. 2007;62:142–148. doi: 10.1111/j.1398-9995.2006.01184.x. [DOI] [PubMed] [Google Scholar]
- Thomson H, Thomas S, Sellstrom E, Petticrew M. Housing improvements for health and associated socioeconomic outcomes (review). The Cochrane Collaboration. Hoboken: Wiley; 2013. [DOI] [PubMed] [Google Scholar]
- United Nations Human Rights Office of the High Commissioner. (1976). International Covenant on Economic, Social and Cultural Rights. Article 11. Available at: http://www.ohchr.org/EN/ProfessionalInterest/Pages/CESCR.aspx. Accessed 19 Sept 2019.
- Weitzman M, Baten A, Rosenthal DG, Hoshino R, Tohn E, Jacobs DE. Housing and child health. Curr Probl Pediatr Adolesc Health Care. 2013;43:187–224. doi: 10.1016/j.cppeds.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Wells NM, Harris JD. Housing quality, psychological distress, and the mediating role of social withdrawal: a longitudinal study of low-income women. J Environ Psychol. 2007;27:69–78. doi: 10.1016/j.jenvp.2006.11.002. [DOI] [Google Scholar]