Abstract
Objective
Wildfire smoke is an important source of air pollution associated with a range of cardiopulmonary health conditions. The Air Quality Health Index (AQHI) is the most widely used tool in Canada to communicate with the public about air pollution, but it may not adequately reflect health risks from wildfire smoke. The objective of this study was to evaluate the ability of the AQHI and four alternate AQHI-Plus amendments to predict adverse population health effects from wildfire smoke.
Methods
The maximum 1-h values of the AQHI and the four amendments were calculated for each 48-h period of the wildfire seasons from 2010 to 2017 for 32 health units in British Columbia. Generalized Poisson models were used to estimate the association between these values and daily counts of five health outcomes: all-cause mortality; physician visits for all circulatory causes; visits for all respiratory causes, including asthma; asthma-specific visits; and dispensations of salbutamol sulfate (i.e., Ventolin®). Model fit was evaluated with the Akaike information criterion.
Results
The AQHI and the four amendments were all associated with all five health outcomes. The AQHI exhibited best fit to the all-cause mortality and circulatory physician visits during all wildfire seasons, while the 1-h PM2.5Only AQHI-Plus exhibited best fit to the asthma-related outcomes during all wildfire seasons.
Conclusion
Individuals with common respiratory conditions such as asthma and chronic obstructive pulmonary disease are particularly susceptible to wildfire smoke. As such, the 1-h PM2.5Only AQHI-Plus amendment was recommended for communicating about potential health effects of air quality during wildfire seasons in BC.
Electronic supplementary material
The online version of this article (10.17269/s41997-019-00237-w) contains supplementary material, which is available to authorized users.
Keywords: Wildfire smoke, Air quality, Asthma, Air Quality Health Index (AQHI)
Résumé
Objectif
La fumée des incendies de forêts est une importante source de pollution atmosphérique associée à un éventail d’états pathologiques cardiopulmonaires. La cote air santé (CAS) est l’outil le plus communément utilisé au Canada pour aviser le public des niveaux de pollution atmosphérique, mais elle pourrait ne pas bien tenir compte des risques pour la santé de la fumée des incendies de forêts. Notre étude visait à évaluer les capacités de la CAS et de quatre indicateurs modifiés (AQUI-Plus, ou « CAS-Plus ») de prédire les effets néfastes de la fumée des incendies de forêts sur la santé des populations.
Méthode
Les valeurs maximales en 1 heure de la CAS et de ses quatre modifications ont été calculées pour chaque période de 48 heures durant les saisons des feux de forêt 2010 à 2017 pour 32 bureaux de santé de la Colombie-Britannique. Des modèles de Poisson généralisés ont servi à estimer les associations entre ces valeurs et le dénombrement quotidien de cinq résultats sanitaires : les décès toutes causes confondues; les visites chez le médecin attribuables à l’ensemble des problèmes circulatoires; les visites attribuables à l’ensemble des problèmes respiratoires, dont l’asthme; les visites spécifiquement attribuables à l’asthme; et la distribution de sulfate de salbutamol (Ventolin®). La qualité du modèle a été évaluée à l’aide du critère d’information d’Akaike.
Résultats
La CAS et ses quatre modifications ont toutes été associées aux cinq résultats sanitaires. La CAS présentait le meilleur ajustement avec les décès toutes causes confondues et les visites chez le médecin attribuables aux problèmes circulatoires durant toutes les saisons de feux de forêt, tandis que l’AQHI-Plus (1-h PM2.5only) présentait le meilleur ajustement avec les résultats liés à l’asthme durant toutes les saisons de feux de forêt.
Conclusion
Les personnes ayant des états pathologiques respiratoires courants comme l’asthme et la maladie pulmonaire obstructive chronique sont particulièrement sensibles à la fumée des incendies de forêts. C’est pourquoi la modification AQHI-Plus 1-h PM2.5Only est recommandée pour communiquer les informations relatives aux effets possibles de la qualité de l’air sur la santé durant la saison des feux de forêt en Colombie-Britannique.
Mots-clés: Fumée d’incendies de forêts, Qualité de l’air, Asthme, Cote air santé (CAS)
Introduction
Wildfire smoke is an important source of transient air pollution in the province of British Columbia (BC) and elsewhere in Canada, especially in more forested rural areas (Dods and Copes 2005). Its impacts on air quality are expected to increase as the climate changes and extreme fire weather becomes more common (Wotton et al. 2010). Wildfire smoke is a complex mixture of air pollutants, among which fine particulate matter (PM2.5) is the commonly measured pollutant of primary concern due to its high emission rates and consistently elevated ambient concentrations during smoke episodes (Naeher et al. 2007). Smoke-related PM2.5 has been associated with the exacerbation of cardiopulmonary conditions, leading to a range of acute health outcomes, from increased medication dispensations to increased risk of all-cause mortality, in BC and elsewhere (Reid et al. 2016; Henderson et al. 2011; Moore et al. 2006; Elliott et al. 2013; Yao et al. 2013; Yao et al. 2016; Liu et al. 2015). These increases have been observed even when the duration of exposure was measured in hours (Ghio 2008; Burgan et al. 2010; Brook et al. 2010). In BC, approximately 12% of the population has asthma and more than 22% has high blood pressure (Provincial Health Services Authority 2019), both of which can make individuals more vulnerable to wildfire smoke exposure. Wildfire smoke events are usually episodic, with concentrations changing rapidly in both time and space. Thus, timely and effective tools are needed to communicate the health risks to the public and to vulnerable populations so they can take protective actions.
The Air Quality Health Index (AQHI) is the most widely used tool in Canada to communicate with the public about the acute health risks posed by air pollution. It is expressed on a scale from 1 to 10+ and associated with four categories of health risk: low; moderate; high; and very high (Table 1). In each category, there are specific health messages for vulnerable populations and for the general public about how to reduce personal exposure and potential health effects (Government of Canada 2016). The AQHI is calculated based on a formula that includes the concentrations of three common air pollutants known to affect human health: ground-level ozone (O3); nitrogen dioxide (NO2); and PM2.5. The formula is constructed from the concentration-response relationship between daily all-cause mortality and these pollutants in Canadian urban centres, and is more weighted towards the NO2 (coefficient = 8.71*10e−4) and O3 (coefficient = 5.37*10e−4) components than the PM2.5 (coefficient = 4.87*10e−4) component (Eq. 1) (Stieb et al. 2008). Under conditions when PM2.5 concentrations are relatively high compared with O3 and NO2 concentrations, the elevated PM2.5 concentrations may not push the AQHI into the moderate or high risk category. In addition, the AQHI may not capture rapid increases in PM2.5 due to wildfire smoke because the value reported each hour is based on the 3-h trailing average of each pollutant. As such, the AQHI may not accurately reflect the impacts of wildfire smoke on air quality, public perception of risk, and population health in British Columbia (Elliott et al. 2013; Henderson et al. 2011; Yao et al. 2016).
Table 1.
Categories of the Air Quality Health Index (AQHI) and their associated health messages
| Health risk | AQHI | Health messages | |
|---|---|---|---|
| At-risk population | General population | ||
| Low | 1–3 | Enjoy your usual outdoor activities. | Ideal air quality for outdoor activities. |
| Moderate | 4–6 | Consider reducing or rescheduling strenuous activities outdoors if you are experiencing symptoms. | No need to modify your usual outdoor activities unless you experience symptoms such as coughing and throat irritation. |
| High | 7–10 | Reduce or reschedule strenuous activities outdoors. Children and the elderly should also take it easy. | Consider reducing or rescheduling strenuous activities outdoors if you experience symptoms such as coughing and throat irritation. |
| Very high | Above 10 | Avoid strenuous activities outdoors. Children and the elderly should also avoid outdoor physical exertion. | Reduce or reschedule strenuous activities outdoors, especially if you experience symptoms such as coughing and throat irritation. |
To address the possibility that the AQHI does not accurately reflect risks related to PM2.5 from wildfire smoke and other sources such as residential wood burning, BC implemented an AQHI-Plus amendment in late 2016. This amendment overrode the 3-pollutant AQHI whenever the 1-h PM2.5 concentrations reached 60 μg/m3 or higher (as described in greater detail in the Methods section). This Trump & Hold AQHI-Plus was designed to indicate 1-h air quality conditions that had a high probability of leading to an Air Quality Advisory being issued based on PM2.5 concentrations. These are typically issued when the 24-h average PM2.5 concentration approaches 25 μg/m3, which is the air quality objective in BC. This threshold has also been associated with increased respiratory health outcomes within the BC population during wildfire smoke events (McLean et al. 2015). Although stakeholders and the general public were supportive of the AQHI-Plus concept, feedback after implementation of the Trump & Hold amendment indicated that further improvement was necessary to resolve ongoing concerns about risk communication, such as the sudden jump to high risk triggered by concentrations over the 60 μg/m3 threshold (Breathe Clean Air Comox Valley 2017).
The objective of this project was to address the following two questions: (1) Is the AQHI indicative of smoke-related respiratory morbidity, cardiovascular morbidity, and all-cause mortality health outcomes during wildfire season? and (2) Would an alternate AQHI-Plus amendment be more indicative of these outcomes than the Trump & Hold AQHI-Plus? By answering these questions, the province of BC can make an evidence-based decision about the optimal AQHI-Plus amendment, if any, to use during wildfire seasons.
Methods
Study area and period
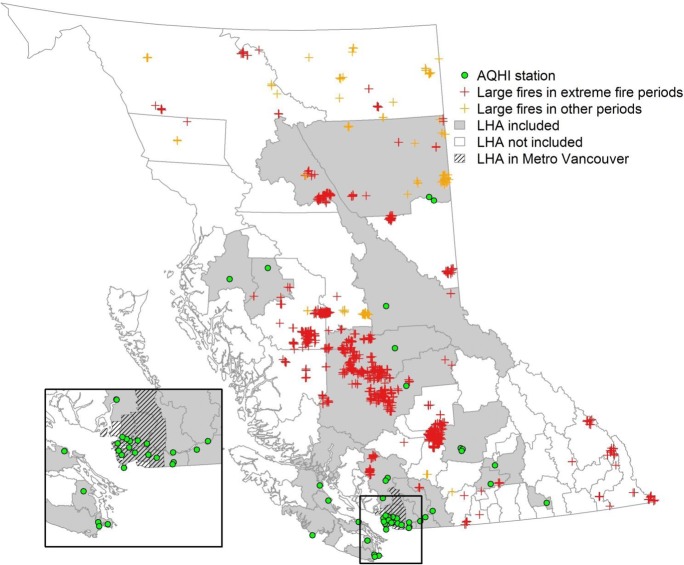
The study covered eight wildfire seasons (01 April to 30 September) from 2010 to 2017, where the early part of each wildfire season may also have impacts from localized prescribed burning. The province is divided into 89 local health areas (LHAs), which are the smallest geographical units to which administrative health data are aggregated. An LHA was included in the analyses if it had measurements for all three pollutants in the AQHI on at least 20% of the days during the study period. Across the province, 32 of the 89 LHAs met these criteria, representing more than 70% of the total population (Fig. 1). To better evaluate the utility of the AQHI and alternate AQHI-Plus amendments for wildfire smoke, we conducted analyses with all days in the study period and restricted to periods when wildfire activity was high. This restriction was based on estimated area burned (Sheldon and Sankaran 2017) and included July to September in the high-intensity seasons of 2010, 2014, 2015, and 2017. We also repeated the analyses for LHAs outside of Metro Vancouver, where wildfire smoke can have more frequent and intense impacts on air quality (Fig. 1).
Fig. 1.
Map of local health areas (LHAs) in British Columbia. Green dots indicate air quality monitors with data available for Air Quality Health Index (AQHI) calculations over the study period. Red and orange crosses indicate large fires observed by satellite during the high-intensity fire periods (July to September in 2010, 2014, 2015, and 2017) and the other periods in the study period, respectively. LHAs included in the study are in grey and LHAs within the Metro Vancouver area are cross-hatched
Air quality data and the AQHI
Measurements of 1-h averaged PM2.5, O3, and NO2 concentrations from 2010 to 2017 were obtained from the repository maintained by the BC Ministry of Environment and Climate Change Strategy. The AQHI was calculated using the following formula, where NO2a, O3a, and PM2.5a are the trailing 3-h average measurements of the NO2, O3, and PM2.5 concentrations:
| 1 |
The alternate AQHI-Plus amendments
Details of the four alternate AQHI-Plus amendments are described below (Table 2). For the Trump & Hold and 1-h PM2.5Only amendments, the AQHI and AQHI-Plus were calculated simultaneously for each hour, and the larger of the two values was assigned to that hour. Taking the larger of the two values ensured a conservative approach that reflected air quality impacts of PM2.5 alone or the impacts of all three pollutants. For the AQHI with 1.4*PM2.5 and AQHI with 2*PM2.5 amendments, the AQHI-Plus value was always larger than the AQHI value.
Table 2.
Calculation of the Air Quality Health Index (AQHI) and alternate amendments
| Calculation | Scenario* | |||
| H−2 |
PM2.5 = 10 μg/m3 O3 = 11 ppb NO2 = 4 ppb |
PM2.5 = 25 μg/m3 O3 = 11 ppb NO2 = 4 ppb |
||
| H−1 |
PM2.5 = 15 μg/m3 O3 = 9 ppb NO2 = 6 ppb |
PM2.5 = 60 μg/m3 O3 = 9 ppb NO2 = 6 ppb |
||
| H0 |
PM2.5 = 51 μg/m3 O3 = 10 ppb NO2 = 5 ppb |
PM2.5 = 100 μg/m3 O3 = 10 ppb NO2 = 5 ppb |
||
| AQHI | 2 | 4 | ||
| Trump & Hold | When the 1-h concentration of PM2.5 exceeds 60 μg/m3, the AQHI-Plus will be boosted to 7. In addition, if the following 1-h concentration exceeds 25 μg/m3, the AQHI-Plus will be reported as 7 for that hour and the next 4 h (total of 6 h). | 2 | 7 | |
| 1-h PM2.5Only | Take the ceiling values (the closest integer greater than or equal to a given value) of the 1-h PM2.5 concentration divided by 10. | 6 | 10 | |
| AQHI with 1.4*PM2.5 | 3 | 5 | ||
| AQHI with 2*PM2.5 | 3 | 7 | ||
*AQHI/AQHI alternate amendment values for the current hour (H0) based on pollutant concentrations in the current hour (H0), the previous hour (H−1), and the hour before that (H−2)
Trump & Hold
While the AQHI is calculated using 3-h trailing averages of the three pollutants, the Trump & Hold AQHI-Plus is based solely on measured 1-h concentrations of PM2.5. It is implemented as follows: if the PM2.5 concentration for the current hour (H0) exceeds 60 μg/m3, the AQHI-Plus value for that hour (H0) will be reported as 7 (the high risk category), even if the AQHI value is less than 7. If the PM2.5 concentration for the following hour (H+1) exceeds 25 μg/m3, the AQHI-Plus value will be maintained as 7 for H+1 and the next four hours (H+2 to H+5), even if the AQHI forecast for these hours is less than 7. The underlying rationale is that 1-h PM2.5 concentrations are predictive of air quality over the next few hours, and two consecutive 1-h concentrations can further improve the reliability of the prediction. The Trump & Hold AQHI-Plus amendment was proposed based on consensus from stakeholders in BC and implemented in late 2016.
The Trump & Hold thresholds were determined based on previous analyses to achieve a good balance between two objectives: the thresholds had to be low enough to capture as many air pollution events as possible, while also being high enough to omit events without lasting impact. Indeed, when the current 1-h PM2.5 concentration exceeds 60 μg/m3, the trailing 24-h average PM2.5 concentrations exceed 25 μg/m3 in almost 80% of cases (Fig. S1). This 25 μg/m3 threshold is important for two reasons: (1) because it is the provincial 24-h PM2.5 objective, and the concentration at which air quality advisories are typically issued in BC, and (2) because our previous work on wildfire smoke reported an observable population increase in asthma-related outcomes at this concentration (McLean et al. 2015).
1-h PM2.5Only
Public feedback about the Trump & Hold AQHI-Plus made it clear that users found the sudden jump to 7 at 60 μg/m3 difficult to interpret, because it did not reflect the gradual increase of PM2.5 before reaching this threshold (Breathe Clean Air Comox Valley 2017). The 1-h PM2.5Only AQHI-Plus amendment was developed to address this concern. It is calculated as the ceiling value (the closest integer greater than or equal to a given value) of the 1-h PM2.5 concentration divided by 10, with a maximum value of 10+. This algorithm is a linear extrapolation based on two anchor points: (1) the AQHI-Plus value should reach 7 (high risk category), when 1-h PM2.5 concentrations are over 60 μg/m3. This is consistent with the Trump & Hold AQHI-Plus and the analyses of the likelihood of exceeding the 25 μg/m3 24-h threshold value; and (2) the AQHI-Plus value should reach 4 (moderate risk category) when the 1-h PM2.5 concentrations are over 30 μg/m3, which is the threshold for odour perception of burning softwood (Kistler et al. 2012), the major type of forest species in BC. This anchor point was constructed to reflect public perception of the health risk related to smoke exposure, which usually starts to aggravate sensitive populations when they begin to smell the smoke.
AQHI with 1.4*PM2.5
Increasing the weight of PM2.5 in the 3-pollutant AQHI formula was another possible AQHI-Plus amendment to improve the sensitivity of the index to PM2.5. To inform the magnitude of this increase, a meta-analysis of studies on wildfire smoke exposure and mortality was conducted (Table S1). The pooled relative risk from these smoke-related studies was approximately 1.4 times higher than the relative risk used to derive the coefficient for PM2.5 in the AQHI (Fig. S2). As a result, the AQHI with 1.4*PM2.5 AQHI-Plus was calculated using the AQHI formula (Eq. 1) with 1.4 times of the original coefficient for PM2.5, based on 3-h trailing averages.
AQHI with 2*PM2.5
This amendment was calculated using 2.0 times the coefficient for PM2.5 in the AQHI formula (Eq. 1). This weight was derived based on two studies (Faustini et al. 2015; Linares et al. 2015) in 2015 that found the mortality risk associated with PM2.5 on smoke-impacted days was approximately double the risk on days without smoke impact (Fig. S3).
Assigning AQHI and AQHI-Plus values to LHAs
The AQHI values reported on websites and smartphone applications are updated hourly, and we assume that most users check the AQHI to assess current risk. As such, we conducted the analyses using the hourly values (rather than the daily mean values) that would have been reported to users under five different scenarios: the AQHI without amendment and the AQHI running with the four AQHI-Plus amendments. To associate AQHI and AQHI-Plus values with daily counts of health data, the maximum value in the 48-h period spanning the current and previous day was taken from the reported hourly values. We chose to use the 48-h time span to ensure that relevant exposures from the previous day were considered, because associations between air pollution and health outcomes are consistently observed within this time window (Elliott et al. 2013; Yao et al. 2016). Values for the analysis were set to missing (NA) if more than 25% of the hourly values in the 48-h period were missing. The highest AQHI or AQHI-Plus value measured from monitors within the boundary of a single LHA was assigned to that LHA for the day. All values in the 10+ range were set to 11, again to be consistent with information available to the public on different media reporting the AQHI.
Administrative health data
The BC Centre for Disease Control (BCCDC) has a mandate to conduct routine environmental health surveillance and evaluation using data feeds made available for these purposes. Daily counts of all-cause mortality for each LHA were retrieved from BC Vital Statistics data feed. Outpatient physician visits coded according to the International Classification of Diseases, 9th Revision (ICD-9) were retrieved from the BC Medical Services Plan data feed for respiratory causes (ICD-9 codes 460–519), circulatory causes (ICD-9 codes 390–459), and asthma (ICD-9 code 493). Pharmaceutical dispensations of salbutamol sulfate (trade name Ventolin® and generics) were retrieved from the BC PharmaNet data feed. Salbutamol sulfate (referred to as simply salbutamol henceforth) is commonly used to relieve acute exacerbations of asthma, chronic obstructive pulmonary disease (COPD), and other obstructive lung diseases.
Statistical analysis
To assess the ability of the AQHI or alternate AQHI-Plus amendments to predict the five health outcomes, we fitted the data using a generalized linear mixed-effects model with a Poisson distribution and logit link, accounting for the random effects of LHAs. All models were adjusted for temperature using a natural cubic spline of daily maximum apparent temperature with three degrees of freedom. Apparent temperature combines the effects of air temperature, relative humidity, and wind speed to calculate the temperature as perceived by humans (Steadman 1984). A binary variable indicating weekdays and weekends/holidays was also included. Model fit was measured using the Akaike information criterion (AIC). Simply put, the AIC indicates how much information is lost when a given model is fitted to a given dataset, so the model with the smallest AIC fits the data best. While the AIC provides information on the quality of a model relative to other models, it does not provide information on the absolute quality of the model. Each of the five models (AQHI and four AQHI-Plus amendments) for each of the five health outcomes were ranked by AIC.
Results
Description of AQHI and pollutant concentrations
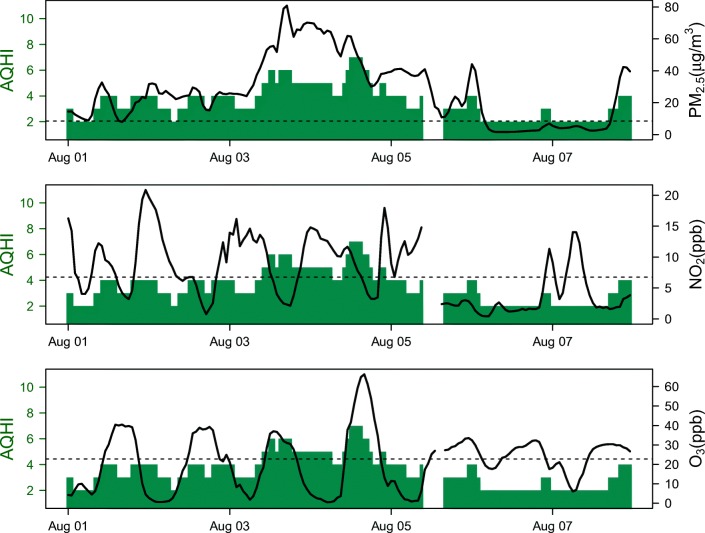
The Pearson’s correlation between PM2.5 and NO2 during the study period ranged from − 0.02 to 0.61 across 55 air-quality monitors, with a median of 0.35. The correlation between PM2.5 and O3 across the same monitors ranged from − 0.56 to 0.29, with a median of − 0.07. In one example, data from a 2014 wildfire smoke episode in Prince George show that PM2.5 concentrations were markedly elevated above baseline while the NO2 and O3 were much less elevated in comparison (Fig. 2). In this example, the highest AQHI values are observed during an O3 peak on 04 August, which was 3-fold higher than the baseline concentration. However, lower AQHI was observed during the PM2.5 peak on 03 August, which was 10-fold higher than the baseline concentration. Overall, the LHAs outside of Metro Vancouver had slightly higher PM2.5 and O3 concentrations than those within Metro Vancouver, while NO2 concentrations were lower (Table 3).
Fig. 2.
Illustration of the relationship between the 3-h trailing averages of PM2.5, NO2, and O3 concentrations (black lines) and the Air Quality and Health Index (AQHI, blue bars) at Prince George, British Columbia, from 01 to 08 August 2014. The black horizontal dashed lines indicate the average pollutant concentrations (baseline) over the entire study period
Table 3.
Summary of air pollutant concentrations and health outcomes during all fire seasons included in the study. Values are shown for all 32 local health areas (LHAs) in the analyses, and the 23 LHAs outside of Metro Vancouver
| All 32 LHAs | 23 LHAs outside Metro Vancouver | |
|---|---|---|
| Mean (25%ile, 75%ile) daily concentrations of three pollutants | ||
| PM2.5 (μg/m3) | 6.6 (5.2, 7.6) | 6.8 (4.8, 7.8) |
| O3 (ppb) | 22.1 (20.4, 23.5) | 22.7 (20.8, 24.0) |
| NO2 (ppb) | 6.5 (4.3, 8.0) | 5.1 (3.6, 6.7) |
| Overall (25%ile, 75%ile) LHA daily rates of five health outcomes per 100,000 population | ||
| All-cause mortality | 1.9 (1.6, 2.4) | 2.2 (2.0, 2.6) |
| Physician visits for circulatory causes | 98.9 (56.3, 105.3) | 100.2 (45.6, 106.3) |
| Physician visits for respiratory causes | 85.1 (44.6, 85.0) | 77.8 (35.9, 79.4) |
| Physician visits for asthma | 9.7 (5.3, 9.8) | 9.7 (3.8, 9.6) |
| Salbutamol dispensations | 30.5 (19.9, 33.6) | 33.9 (17.7, 34.8) |
Description of the 2-day maximum AQHI and alternate AQHI-Plus values
A total of 28,402 daily observations were included in the analyses for the entire study period, with a range of 270 to 1279 days included for each of the 32 LHAs. Out of the 28,402 observations, 7539 (27%) were in the 10 Metro Vancouver LHAs and 20,863 (73%) were outside. Further, 8718 (31%) were included in the analyses restricted to periods with intense fire activity across all LHAs, of which 6424 (74%) were outside of Metro Vancouver. The distributions of the AQHI and AQHI-Plus values were similar, with a 48-h maximum value of 2 to 5 in the majority of observations (Fig. 3). There were 44% to 113% more values above 7 for the four AQHI-Plus amendments compared with the AQHI (Fig. 3).
Fig. 3.
Frequency distribution of the Air Quality and Health Index (AQHI) and AQHI-Plus values for all observations included in the study period. Cells are colour coded by the percent change in frequency compared with the AQHI. For example, the frequency of 10+ values using the AQHI with 1.4*PM2.5 algorithm (n = 283) was 87% higher than the frequency of 10+ values using the AQHI (n = 151)
Health analyses
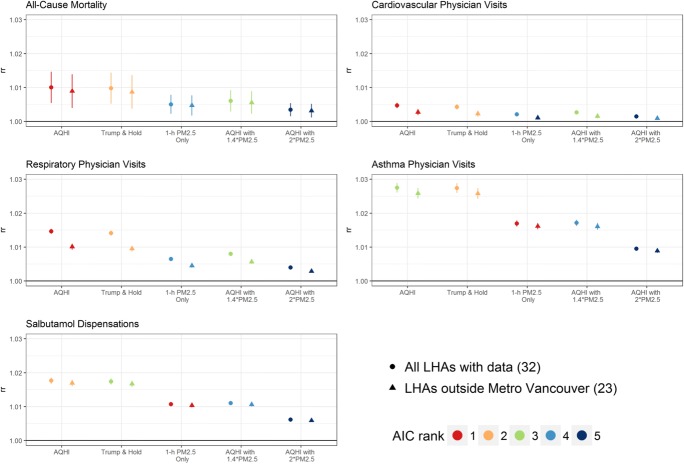
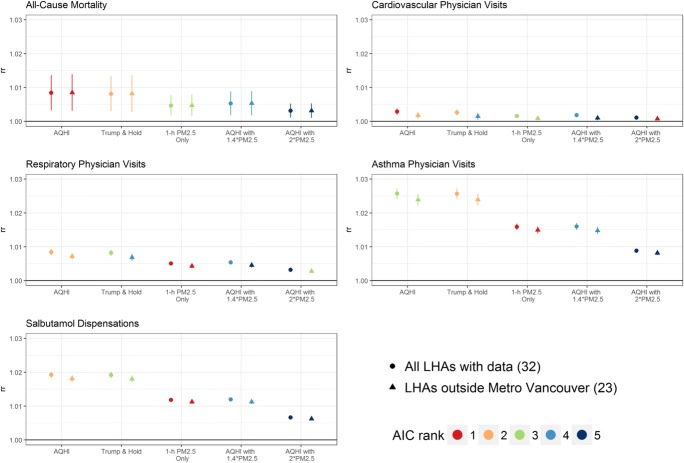
The LHAs outside of Metro Vancouver had lower rates of physician visits for respiratory causes compared with all LHAs, but higher rates of all-cause mortality and salbutamol dispensations. Physician visits for all circulatory causes and asthma were similar. These differences may be due to the demographic composition of the populations, regional variability in disease rates, or ease of access to health care. Increases in the AQHI and all four AQHI-Plus amendments were significantly (p = 0.05) associated with increased risk of all health outcomes tested in the analyses. Throughout the entire study period in all 32 LHAs, an AQHI increase of 1.0 was associated with a 1.0% (95% CI 0.5–1.5) increase in all-cause mortality; a 0.5% (0.4–0.5) increase in physician visits for cardiovascular conditions; a 1.5% (1.4–1.5) increase in physician visits for respiratory conditions; a 2.8% (2.6–2.9) increase in physician visits for asthma; and a 1.8% (1.7–1.9) increase in salbutamol dispensations (Fig. 4). Overall, the AQHI and Trump & Hold AQHI-Plus had the largest effect estimates, due to smaller numbers of large values compared with other AQHI-Plus algorithms. During all summers, the AQHI was best fitted to the mortality and physician visits for all cardiovascular and all respiratory conditions, while the 1-h PM2.5Only AQHI-Plus was best fitted to physician visits for asthma and salbutamol dispensations (Fig. 4). In the analysis restricted to periods with intense wildfire activity (Fig. 5), the AQHI was best fitted to mortality and physician visits for all cardiovascular conditions, while the 1-h PM2.5Only AQHI-Plus was best fitted to all of the respiratory outcomes.
Fig. 4.
Relative rates for a 1.0 index increase the maximum hourly Air Quality Health Index (AQHI) or alternate AQHI-Plus amendments in all wildfire seasons (April through September) for 2010–2017. Results are colour coded by the rank of model fit, where red indicates the model with the lowest Akaike information criterion (AIC). Dots indicate results from analysis with all available 32 local health areas (LHAs), and triangles indicate results from the 23 LHAs outside of Metro Vancouver
Fig. 5.
Relative rates for a 1.0 index increase the maximum hourly Air Quality Health Index (AQHI) or alternate AQHI-Plus amendments during high-intensity fire periods (July through September of 2010, 2014, 2015, and 2017). Results are colour coded by the rank of model fit, where red indicates the model with the lowest Akaike information criterion (AIC). Dots indicate results from analysis with all available 32 local health areas (LHAs), and triangles indicate results from the 23 LHAs outside of Metro Vancouver
Discussion
To evaluate which of the AQHI or AQHI-Plus amendments was most appropriate for BC during wildfire season, we assessed the association between five health outcomes and the maximum hourly AQHI or alternate AQHI-Plus values experienced during a 48-h window, and then compared models using the AIC. The results (Figs. 4 and 5) led to five important conclusions:
The AQHI and all four AQHI-Plus amendments were significantly associated with all-cause mortality, circulatory physician visits, and all respiratory health outcomes.
The AQHI had the best fit for all-cause mortality and circulatory physician visits during all wildfire seasons and during the high-intensity fire periods.
The 1-h PM2.5Only AQHI-Plus had the best fit for the asthma-related outcomes during all wildfire seasons and during the high-intensity fire periods.
The AQHI had the best fit for all respiratory physician visits during all wildfire seasons, but the 1-h PM2.5Only AQHI-Plus had the best fit during the high-intensity fire periods.
When the AQHI had the best fit, the 1-h PM2.5Only was typically ranked 2nd or 3rd among the four AQHI-Plus amendments. When the 1-h PM2.5Only had the best fit, the AQHI was typically ranked 1st or 2nd among the four other options.
These conclusions suggest that the AQHI is most indicative of the mortality and circulatory risks during periods affected by wildfire smoke. However, the 1-h PM2.5Only AQHI-Plus is most indicative of the respiratory risks during high-intensity fire periods, particularly for people with asthma. This is consistent with the rationale behind the AQHI formulation and with existing health evidence related to the effects of wildfire smoke.
The AQHI was developed based on the relationships between the three contributing pollutants and daily mortality in large Canadian cities (Stieb et al. 2008). Further work has been done to confirm that the AQHI is proportionally associated with measures of morbidity, such as physician visits, emergency room presentations, and hospital admissions (Martin et al. 2013; Chen et al. 2014; Szyszkowicz and Kousha 2014). The AQHI is associated with physiological measures such as heart rate variability, including in studies conducted outside of large urban areas (Cakmak et al. 2014; Stieb et al. 2017; Stieb et al. 2018). One concern about the AQHI with respect to wildfire smoke is the marked and disproportionate increase in respiratory morbidity during smoke episodes compared with mortality and other types of morbidity within the population. Where mortality and non-respiratory morbidity may be increased by 1–2% per 10 μg/m3 of PM2.5 during smoky periods (Liu et al. 2015), measures of respiratory morbidity and asthma-specific outcomes have been increased by 5–8% in multiple BC studies (Elliott et al. 2013; Yao et al. 2016; Henderson et al. 2011). This particular effect of wildfire smoke on respiratory health may be due to PM2.5 exposure alone, or it may be related to other unmeasured co-pollutants in the complex smoke mixture, such as volatile organic compounds.
Regardless of the mechanism, there is sufficient evidence in BC that PM2.5 from wildfire smoke has a larger impact on population respiratory health than PM2.5 in the typical background mixture, especially asthma exacerbation among the sensitive population. Studies have found that asthma-related outcomes were associated with PM2.5 in smoke-impacted regions, but not in other regions (Elliott et al. 2013), and the effect of PM2.5 is larger on extreme fire days compared with the entire fire season (Elliott et al. 2013; Yao et al. 2016). Because people with asthma are particularly sensitive to wildfire smoke, the existing health surveillance systems at the BCCDC are based on asthma-related outcomes, including physician visits and salbutamol dispensations. These systems have allowed us to observe same sensitivity across multiple different populations and wildfire seasons in BC (McLean et al. 2015). Meanwhile, evidence on mortality and cardiovascular health related to wildfire smoke has been less conclusive in BC and elsewhere. This may be due to inadequate statistical power to detect the reduced magnitude of the effects, suggesting that larger and better-designed studies will continue to improve the quality of the evidence (Liu et al. 2015; Reid et al. 2016).
There are some limitations in this study. First, only 32 out of the 89 LHAs were included due to the limited number of monitoring stations that measure all three AQHI pollutants in the province. While the 32 LHAs covered more than 70% of the population, they do omit many rural communities regularly impacted by wildfire smoke (Fig. 1). Second, the health data were only available as daily counts and therefore could not be used to fully evaluate the AQHI and AQHI-Plus amendments at the hourly time-scale. We chose to use the 48-h maximum of hourly values to increase the probability that the relevant exposure preceded the outcome of interest, and to account for the fact that the Trump & Hold AQHI-Plus was often activated by smoke inversions late at night, meaning that the value of 7 was carried into the following day. However, the true temporal nature of the relationship between smoke exposure and its acute population health effects is not accurately reflected in the study results. Third, we used measurements from a single air quality monitor to represent the exposure for population in the entire LHA, which introduces exposures misclassification likely to bias the results towards the null. This bias may be greater for the larger LHAs outside of Metro Vancouver, which may partially explain their smaller effect estimates. Fourth, we could not include data on aeroallergens such as tree, weed, and grass pollens, which can be concurrent with wildfire smoke and which also have acute impacts on respiratory health outcomes. Such data are not widely measured in Canada, and are not publicly available for research purposes. Finally, we have not included data from other Canadian jurisdictions and therefore cannot assess how the amendments would perform in other provinces and territories that are similarly affected by wildfire smoke.
Conclusion
The objective of these analyses was to compare the AQHI with four AQHI-Plus amendments that increased the influence of PM2.5 on the reported values during wildfire season, based on their ability to predict five different population health outcomes in BC. The need for this assessment was based on public perception that the AQHI was not adequately responsive to smoke impacts in BC communities (Breathe Clean Air Comox Valley 2017; Kelly 2017). Overall, we found that the AQHI was significantly associated with all five health outcomes during all wildfire seasons and during the high-intensity fire periods. However, we also found that the 1-h PM2.5Only AQHI-Plus amendment was a stronger indicator of the asthma-related outcomes during all wildfire seasons, and of all respiratory outcomes during high-intensity fire periods.
Based on these analyses, the BC Ministry of Environment and Climate Change Strategy decided that the previously implemented Trump & Hold AQHI-Plus should be replaced by the 1-h PM2.5Only AQHI-Plus. It has worked with Environment and Climate Change Canada to implement the 1-h PM2.5Only amendment across BC as a pilot project from 01 May through 30 September 2018, with user feedback solicited in future. As described here, the AQHI and 1-h PM2.5Only AQHI-Plus will both be calculated at every site for every hour, and the higher of the two values will be reported on all available media. When the wildfire season is low intensity, we expect that the AQHI-Plus will override the AQHI in less than 0.4% of all hours from July through September, ranging from 0.02% to 2.8% between stations (based on the lowest-intensity 2011 season). When the wildfire season is high intensity, we expect that the AQHI-Plus will override the AQHI in approximately 3.8% of all hours, ranging from 0.1% to 18% between stations (based on the highest-intensity 2017 season). In either case, the 1-h PM2.5Only AQHI-Plus amendment is a small change with the potential to improve risk communication and public trust in the AQHI across BC.
Electronic supplementary material
(DOCX 258 kb)
Funding information
This study was funded by the British Columbia Ministry of Environment and Climate Change Strategy.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Breathe Clean Air Comox Valley (2017). Air quality health index concerns http://breathecleanair.ca/wp-content/uploads/2017/09/BCACV-letter-re-AQHI-Concerns.pdf. Accessed 2018-08-14.
- Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Burgan O, Smargiassi A, Perron S, Kosatsky T. Cardiovascular effects of sub-daily levels of ambient fine particles: a systematic review. Environ Health. 2010;9(1):1. doi: 10.1186/1476-069X-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cakmak S, Kauri L, Shutt R, Liu L, Green MS, Mulholland M, et al. The association between ambient air quality and cardiac rate and rhythm in ambulatory subjects. Environ Int. 2014;73:365–371. doi: 10.1016/j.envint.2014.08.015. [DOI] [PubMed] [Google Scholar]
- Chen L, Villeneuve PJ, Rowe BH, Liu L, Stieb DM. The Air Quality Health Index as a predictor of emergency department visits for ischemic stroke in Edmonton, Canada. Journal of Exposure Science and Environmental Epidemiology. 2014;24(4):358. doi: 10.1038/jes.2013.82. [DOI] [PubMed] [Google Scholar]
- Dods P, Copes R. Wood smoke, forest fires and PM2.5 in British Columbia. BC Medical Journal. 2005;47(5):132–133. [Google Scholar]
- Elliott CT, Henderson SB, Wan V. Time series analysis of fine particulate matter and asthma reliever dispensations in populations affected by forest fires. Environ Health. 2013;12:11. doi: 10.1186/1476-069x-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faustini A, Alessandrini ER, Pey J, Perez N, Samoli E, Querol X, et al. Short-term effects of particulate matter on mortality during forest fires in southern Europe: results of the MED-PARTICLES Project. Occup Environ Med. 2015;72(5):323–329. doi: 10.1136/oemed-2014-102459. [DOI] [PubMed] [Google Scholar]
- Ghio AJ. Mechanism of asthmatic exacerbation by ambient air pollution particles. Expert review of respiratory medicine. 2008;2(1):109–118. doi: 10.1586/17476348.2.1.109. [DOI] [PubMed] [Google Scholar]
- Government of Canada (2016). Air quality health index. http://www.ec.gc.ca/cas-aqhi/default.asp?Lang=En. Accessed August 23 2016.
- Henderson SB, Brauer M, Macnab YC, Kennedy SM. Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ Health Perspect. 2011;119(9):1266–1271. doi: 10.1289/ehp.1002288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, A. (2017). Interior B.C. needs better air quality monitoring during wildfires: Kamloops doctors. http://www.cbc.ca/news/canada/british-columbia/interior-b-c-needs-better-air-quality-monitoring-during-wildfires-kamloops-doctors-1.4365457. Accessed 2018-08-15.
- Kistler M, Schmidl C, Padouvas E, Giebl H, Lohninger J, Ellinger R, et al. Odor, gaseous and PM10 emissions from small scale combustion of wood types indigenous to Central Europe. Atmos Environ. 2012;51:86–93. doi: 10.1016/j.atmosenv.2012.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linares C, Carmona R, Tobias A, Miron IJ, Diaz J. Influence of advections of particulate matter from biomass combustion on specific-cause mortality in Madrid in the period 2004-2009. Environ Sci Pollut Res Int. 2015;22(9):7012–7019. doi: 10.1007/s11356-014-3916-2. [DOI] [PubMed] [Google Scholar]
- Liu JC, Pereira G, Uhl SA, Bravo MA, Bell ML. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ Res. 2015;136:120–132. doi: 10.1016/j.envres.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin KL, Hanigan IC, Morgan GG, Henderson SB, Johnston FH. Air pollution from bushfires and their association with hospital admissions in Sydney, Newcastle and Wollongong, Australia 1994-2007. Aust N Z J Public Health. 2013;37(3):238–243. doi: 10.1111/1753-6405.12065. [DOI] [PubMed] [Google Scholar]
- McLean KE, Yao J, Henderson SB. An evaluation of the British Columbia Asthma Monitoring System (BCAMS) and PM2.5 exposure metrics during the 2014 forest fire season. Int J Environ Res Public Health. 2015;12(6):6710–6724. doi: 10.3390/ijerph120606710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore D, Copes R, Fisk R, Joy R, Chan K, Brauer M. Population health effects of air quality changes due to forest fires in British Columbia in 2003: estimates from physician-visit billing data. Can J Public Health. 2006;97(2):105–108. doi: 10.1007/BF03405325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naeher LP, Brauer M, Lipsett M, Zelikoff JT, Simpson CD, Koenig JQ, et al. Woodsmoke health effects: a review. Inhal Toxicol. 2007;19(1):67–106. doi: 10.1080/08958370600985875. [DOI] [PubMed] [Google Scholar]
- Provincial Health Services Authority (2019). Comparison to BC: the summary below highlights how your community is doing compared to the provincial average. http://communityhealth.phsa.ca/HealthProfiles/HealthReportComparisonToBC/Trail. Accessed 2019-04-17.
- Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016;124(9):1334. doi: 10.1289/ehp.1409277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldon TL, Sankaran C. The impact of Indonesian forest fires on Singaporean pollution and health. Am Econ Rev. 2017;107(5):526–529. doi: 10.1257/aer.p20171134. [DOI] [PubMed] [Google Scholar]
- Steadman RG. A universal scale of apparent temperature. J Clim Appl Meteorol. 1984;23(12):1674–1687. doi: 10.1175/1520-0450(1984)023<1674:AUSOAT>2.0.CO;2. [DOI] [Google Scholar]
- Stieb DM, Burnett RT, Smith-Doiron M, Brion O, Shin HH, Economou V. A new multipollutant, no-threshold air quality health index based on short-term associations observed in daily time-series analyses. J Air Waste Manage Assoc. 2008;58(3):435–450. doi: 10.3155/1047-3289.58.3.435. [DOI] [PubMed] [Google Scholar]
- Stieb DM, Shutt R, Kauri L, Mason S, Chen L, Szyszkowicz M, et al. Cardio-respiratory effects of air pollution in a panel study of outdoor physical activity and health in rural older adults. J Occup Environ Med. 2017;59(4):356. doi: 10.1097/JOM.0000000000000954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stieb DM, Shutt R, Kauri LM, Roth G, Szyszkowicz M, Dobbin NA, et al. Cardiorespiratory effects of air pollution in a panel study of winter outdoor physical activity in older adults. J Occup Environ Med. 2018;60(8):673–682. doi: 10.1097/JOM.0000000000001334. [DOI] [PubMed] [Google Scholar]
- Szyszkowicz M, Kousha T. Emergency department visits for asthma in relation to the air quality health index: a case-crossover study in Windsor, Canada. Canadian Journal of Public Health. 2014;105(5):e336–e341. doi: 10.17269/cjph.105.4539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wotton BM, Nock CA, Flannigan MD. Forest fire occurrence and climate change in Canada. Int J Wildland Fire. 2010;19(3):253–271. doi: 10.1071/WF09002. [DOI] [Google Scholar]
- Yao J, Brauer M, Henderson SB. Evaluation of a wildfire smoke forecasting system as a tool for public health protection. Environ Health Perspect. 2013;121(10):1142. doi: 10.1289/ehp.1306768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao J, Eyamie J, Henderson SB. Evaluation of a spatially resolved forest fire smoke model for population-based epidemiologic exposure assessment. Journal of Exposure Science and Environmental Epidemiology. 2016;26(3):233. doi: 10.1038/jes.2014.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 258 kb)