Abstract
Objectives
To explore physicians’ and nurses’ knowledge, attitudes and experiences of shared decision making (SDM) in rheumatology, to identify barriers and facilitators to SDM, and to examine whether physicians’ and nurses’ perspectives of SDM differ.
Methods
A cross-sectional, exploratory, online survey was used. Besides demographic characteristics, healthcare professionals’ knowledge, attitudes and experiences of SDM in rheumatology were assessed. Barriers and facilitators to SDM were identified from healthcare professionals’ answers. Descriptive statistics were computed and differences between physicians’ and nurses’ perspectives of SDM were examined with a t-test or Fisher’s exact test, as appropriate.
Results
Between April and June 2019, 77 physicians and 70 nurses completed the survey. Although most healthcare professionals lacked a full conceptual understanding of SDM, almost all physicians (92%) and all nurses had a (very) positive attitude toward SDM, which was most frequently motivated by the belief that SDM improves patients’ treatment adherence. The majority (>50%) of healthcare professionals experienced problems with the application of SDM in clinical practice, mostly related to time constraints. Other important barriers were the incompatibility of SDM with clinical practice guidelines and beliefs that patients do not prefer to be involved in decision making or are not able to take an active role. Modest differences between physicians’ and nurses’ perspectives of SDM were found.
Conclusions
There is a clear need for education and training that equips and empowers healthcare professionals to apply SDM. Furthermore, the commitment of time, resources and financial support for national, regional and organisational initiatives is needed to make SDM in rheumatology a practical reality.
Keywords: nursing, qualitative research, treatment
Key messages.
What is already known about this subject?
Shared decision making (SDM) is applied in clinical practice only to a limited extent.
Studies in rheumatology on healthcare professionals’ perspectives of SDM are lacking.
What does this study add?
Results of a cross-sectional, exploratory, online survey, completed by 147 healthcare professionals, showed that healthcare professionals lacked a full conceptual understanding of SDM.
Overall, healthcare professionals had a (very) positive attitude toward SDM. However, the majority of them experienced problems with the application of SDM in clinical practice (eg, time constraints, the incompatibility of SDM with clinical practice guidelines and beliefs that patients do not prefer to be involved in decision making or are not able to take an active role).
How might this impact on clinical practice?
There is a clear need for education and training that equips and empowers healthcare professionals to apply SDM.
Introduction
Shared decision making (SDM) is widely recognised as a key component of patient centred care. At its core, SDM is an approach in which healthcare professionals and patients work together to make decisions based on the best available evidence, while accounting for patients’ treatment preferences.1 2 SDM is thought to improve patients’ treatment adherence and, ultimately, health outcomes.3 SDM is most appropriate for preference-sensitive decisions. That is, decisions where two or more equivalent treatment options exist and the best decision depends on how individual patients value the risks and benefits of each treatment option.4 5 International rheumatology guidelines explicitly recommend SDM.6 7
However, SDM is applied in clinical practice only to a limited extent.8 9 Its low uptake may be attributed to a range of factors affecting successful implementation (eg, a lack of awareness, time constraints and the power imbalance in the healthcare professional–patient relationship).10 11 Since SDM represents a shift in the way most clinical rheumatology care is implemented, the health system change model proposed by Grol and Wensing provides a useful framework for identifying factors that inhibit or drive change.12 According to this model, barriers and facilitators may be identified on six levels of the healthcare system: (1) the innovation itself; (2) the individual professional; (3) the patient; (4) the social context; (5) the organisational context; and (6) the economic and political context.12 Considering factors on each of these levels increases the likelihood of implementing SDM successfully.12–14 As a first step, insight into healthcare professionals’ perspectives of SDM is essential for the development of tailored implementation strategies to overcome barriers and to facilitate SDM.10 15
A systematic review of 38 studies in various clinical specialisations (eg, oncology, paediatrics and general practice) identified barriers and facilitators to SDM related to the level of the individual professional (ie, knowledge, attitudes and experiences) and external levels (eg, the organisational context).10 These factors may also apply to rheumatology. However, there may be other factors unique to the practice of rheumatology that play out as barriers and facilitators. To date, studies in rheumatology on healthcare professionals’ perspectives of SDM are lacking. Both physicians and nurses play a prominent role in the treatment of patients with a rheumatic disease and are professionally well-suited to apply SDM.6 7 16 17 Therefore, the aim of this study was to explore physicians’ and nurses’ knowledge, attitudes and experiences of SDM in rheumatology, to identify barriers and facilitators to SDM, and to examine whether physicians’ and nurses’ perspectives of SDM differ.
Methods
Design and setting
This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology statement and using the Checklist for Reporting Results of Internet E-Surveys.18 19 A cross-sectional, exploratory, online survey was used to collect data from healthcare professionals. Healthcare professionals were eligible to participate if they worked as a rheumatologist, physician assistant, nurse specialist or rheumatology nurse in the Netherlands. Healthcare professionals in training were also eligible to participate. No other eligibility criteria were applied. In this study, rheumatologists and physician assistants were categorised as physicians. Nurse specialists and rheumatology nurses were categorised as nurses. The categorisation was based on healthcare professionals’ common tasks and responsibilities in the treatment of patients with a rheumatic disease.6 7 17 Convenience sampling was used to recruit participants. Recruitment took place through the Dutch rheumatology association (439 members, rheumatologists), rheumatology unit of the Dutch association for physician assistants (18 members, physician assistants) and rheumatology unit of the Dutch nurses association (251 members, nurse specialists and rheumatology nurses).20–22 The Dutch rheumatology association placed a call for participation in their email newsletter and the other two professional associations sent an email directly to their members requesting them to participate. In addition, the personal networks of the researchers were used to recruit additional participants via snowball sampling and to send follow-up emails to those who did not respond to the initial survey request.
Survey
Another survey, exploring Dutch trauma surgeons’ perspectives of SDM, was adapted for this study.23 The survey included both open-ended questions, asking participants to answer in their own words, and close-ended questions, providing multiple answer options. SurveyMonkey was used to distribute the survey online. Prior to fielding, the usability and technical functionality of the survey were pretested by a researcher, rheumatologist and rheumatology nurse. The survey was refined based on their feedback. The survey consisted of 18 questions, presented over 11 screens. Participants were required to answer each question in order to continue through the survey. They were not allowed to go back to previous questions. The survey took about 10–15 min to complete and was open between April and June 2019. Online supplementary appendix 1 presents the survey.
rmdopen-2019-001121supp001.pdf (89.2KB, pdf)
Demographic questions
The survey started with five demographic questions: (1) age; (2) sex; (3) profession; (4) years of work experience; and (5) work setting. The other 13 questions assessed participants’ knowledge, attitudes and experiences of SDM in rheumatology.
Knowledge
Participants’ knowledge was assessed with three questions. The first question asked participants to score their presumed knowledge of SDM on a 11-point scale (0=no knowledge, 10=comprehensive knowledge). Subsequently, participants were asked to answer an open-ended question: ‘How do you define SDM?’. Participants’ definitions were rated as concordant, discordant or inconclusive, depending on the extent they were in line with current consensus in the literature on the definition of SDM. Two researchers (EGEM and JEV) independently rated participants’ definitions. Disagreements between the researchers were resolved through discussion until consensus was reached. To be rated as concordant, participants’ definitions had to refer to at least two communicative behaviours predefined as essential for SDM (eg, asking the patient about his/her personal values and preferences). Participants’ definitions were rated as discordant if they did not refer to any communicative behaviour predefined as essential for SDM or referred to communicative behaviour(s) predefined as conflicting with SDM (eg, letting the patient decide after giving thorough information). Participants’ definitions were rated as inconclusive if they were too short or too ambiguous to reliably interpret what was meant. Online supplementary appendix 2 presents an overview of 13 communicative behaviours predefined as essential for SDM (seven out of 13), not essential for SDM (four out of 13) and conflicting with SDM (two out of 13).23 With the third question, participants were asked to rate the 13 different communicative behaviours as essential for SDM or not.
Attitudes
Six questions assessed participants’ attitudes. The first question, ‘How do you feel about applying SDM in clinical practice?’, was assessed on a 5-point scale (0=very positive, 4=very negative). Participants could provide an explanation of their answer in free text. With the third and fourth question, participants were asked to indicate which types of rheumatic diseases (eg, rheumatoid arthritis, gout and osteoarthritis) and decisions (eg, diagnostic testing, adjusting medication doses and making lifestyle changes) they considered appropriate for SDM. Subsequently, they could provide an explanation of their answer in free text. The sixth question asked participants about their usual decision making style.24 Answer options were: ‘I make decisions alone’, ‘I make decisions after seriously considering my patient’s opinion’, ‘My patient and I share responsibility for making decisions’, ‘My patient makes decisions after seriously considering my opinion’ and ‘My patient makes decisions alone’.
Experiences
Participants’ experiences were assessed with four questions. The first question, ‘In what percentage of the situations appropriate for SDM do you apply SDM?’, was assessed on a 5-point scale (0=0%, 5=100%). Subsequently, participants could tick up to three reasons for not applying SDM. With the third question, participants were asked about problems with the application of SDM, if any. The final question was open-ended: ‘What do you need to improve the application of SDM in clinical practice?’.
Barriers and facilitators
A priori, a list of barriers and facilitators to SDM was generated from a review of relevant literature and used for a thematic analysis.10 11 25 26 Participants’ answers to both close- and open-ended questions were read and coded using the list. While reading participants’ answers, the research team also explored whether any barriers and facilitators surfaced that had not been identified in previous studies. Eventually, all identified barriers and facilitators were grouped according to six levels of the healthcare system.12
Statistical analysis
Only participants who completed the survey were included in the analyses. Participants’ knowledge, attitudes and experiences were analysed descriptively. Continuous variables, following a normal distribution, were reported as means and SD and categorical variables as absolute numbers and percentages. Differences between physicians’ and nurses’ perspectives of SDM were examined with a t-test (continuous variables) or Fisher’s exact test (categorical variables). P values <0.05 were considered statistically significant. The statistical analysis was performed using Stata V.13.
Ethical considerations
A minimum of personal information was collected that did not identify or could not be used, either alone or in combination, to identify participants. To ensure anonymity, the internet protocol (IP) address tracking option in SurveyMonkey was disabled.
Results
Participants
One hundred and forty-seven healthcare professionals (77 physicians and 70 nurses) completed the survey. Assuming that all members of the Dutch rheumatology association, rheumatology unit of the Dutch association for physician assistants and rheumatology unit of the Dutch nurses association received the survey request, response rates were respectively 15%, 56% and 28%. Participants’ demographic characteristics are presented in table 1.
Table 1.
Participants’ demographic characteristics
| Characteristics | Physicians (n=77) | Nurses (n=70) | P value |
| Age (in years), mean (SD) | 45.7 (9.5) | 50.7 (9.0) | <0.01 |
| Sex, n (%) | |||
| Male | 26 (34) | 1 (1) | <0.01 |
| Female | 51 (66) | 69 (99) | |
| Profession, n (%) | |||
| Rheumatologist | 67 (87) | – | – |
| Physician assistant | 10 (13) | – | |
| Nurse specialist | – | 11 (16) | |
| Rheumatology nurse | – | 59 (84) | |
| Years of work experience, mean (SD) | 11.1 (9.5) | 11.8 (7.0) | 0.63 |
| Work setting†, n (%) | |||
| Academic hospital | 18 (23) | 12 (17) | 0.12 |
| Teaching hospital | 33 (43) | 19 (27) | |
| General hospital | 25 (32) | 36 (51) | |
| Other‡ | 6 (8) | 5 (7) |
†The sum of percentages exceeds 100 since some participants worked in multiple settings.
‡Other work settings included independent treatment centres and primary care practices.
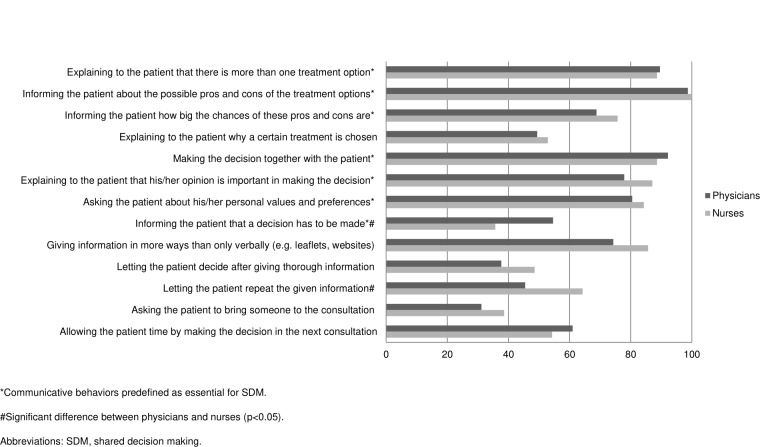
Knowledge
The mean scores of physicians’ and nurses’ presumed knowledge of SDM were, respectively 7.2 (SD=1.0) and 7.0 (SD=1.7) (p=0.22) on a scale from 0 (=no knowledge) to 10 (=comprehensive knowledge). Participants reported various definitions of SDM. Less than half of them reported a definition that was rated as concordant (physicians: 47%, nurses: 33%). Furthermore, 21% of physicians and 32% of nurses reported a definition that was rated as discordant and 33% of physicians and 36% of nurses reported a definition that was rated as inconclusive. There was no significant difference between physicians and nurses (p=0.18). Examples of participants’ definitions of SDM that were rated as concordant, discordant and inconclusive are presented in online supplementary appendix 3. Figure 1 presents the percentages of participants who rated 13 different communicative behaviours as essential for SDM. All seven communicative behaviours predefined as essential for SDM were rated as such by the majority of physicians (>50%). The majority of nurses (>50%) also rated these behaviours as essential for SDM, except for ‘Informing the patient that a decision has to be made’, which was rated as essential for SDM by 36% of nurses. Communicative behaviours predefined as conflicting with SDM (ie, ‘Explaining to the patient why a certain treatment is chosen’ and ‘Letting the patient decide after giving thorough information’) were rated as essential for SDM by respectively 49% and 38% of physicians and 53% and 49% of nurses. Significantly more physicians than nurses rated ‘Informing the patient that a decision has to be made’ as essential for SDM (physicians: 55%, nurses: 36%, p=0.03), whereas significantly more nurses than physicians rated ‘Letting the patient repeat the given information’ as essential for SDM (physicians: 45%, nurses: 64%, p=0.03).
Figure 1.
The percentages of participants who rated 13 different communicative behaviours as essential for SDM.
Attitudes
Almost all physicians (92%) and all nurses reported a positive or very positive attitude toward SDM. There was a significant difference between physicians and nurses (p=0.04) (online supplementary appendix 4). The most frequently reported motivation for participants’ (very) positive attitude was the belief that SDM improves patients’ treatment adherence. Furthermore, physicians also frequently reported that they believe SDM benefits the professional relationship with patients. SDM was considered appropriate for all types of rheumatic diseases by 56% of physicians and 57% of nurses (p=1.00). Forty-nine per cent of physicians and 40% of nurses considered all types of decisions appropriate for SDM (p=0.32). Pharmacological decisions (ie, starting and/or stopping medication, adjusting medication doses and administering single medication doses) were considered most appropriate, whereas decisions for diagnostic testing were considered least appropriate. Significantly more physicians than nurses considered decisions for diagnostic testing appropriate for SDM (physicians: 68%, nurses: 50%, p=0.04), whereas significantly more nurses than physicians considered decisions for paramedical treatment (eg, physical therapy, occupational therapy and dietetics) appropriate for SDM (physicians: 77%, nurses: 91%, p=0.02). Participants reasoned that, basically, the appropriateness of SDM does not depend on the type of rheumatic disease or decision. Most participants (physicians: 78%, nurses: 73%, p=0.05) reported that they usually share responsibility for making decisions with their patient (online supplementary appendix 4).
Experiences
Eighty-one per cent of physicians and 87% of nurses reported applying SDM in 75% or more of the situations appropriate for SDM (p=0.37) (online supplementary appendix 4). Table 2 presents an overview of participant-reported reasons for not applying SDM. The three most frequently reported reasons of physicians for not applying SDM were: ‘SDM is often too complex for patients’ (47%), ‘Patients want me to make the decision’ (26%) and ‘I do not have enough time to apply SDM’ (26%). Nurses most frequently reported that: ‘SDM is often too complex for patients’ (30%), ‘Patients want me to make the decision’ (49%) and ‘SDM is incompatible with clinical practice guidelines’ (31%). Sixty-five per cent of physicians and 56% of nurses reported problems with the application of SDM in clinical practice, mostly related to time constraints (p=1.00). Accordingly, participants frequently reported a need for longer consultation times to improve the application of SDM in clinical practice.
Table 2.
Overview of participant-reported reasons for not applying SDM
| Reasons | Physicians (n=77) | Nurses (n=70) | P value |
| SDM is often too complex for patients, n (%) | 36 (47) | 21 (30) | 0.04 |
| Patients want me to make the decision, n (%) | 20 (26) | 34 (49) | 0.01 |
| I do not have enough time to apply SDM, n (%) | 20 (26) | 10 (14) | 0.10 |
| SDM is incompatible with clinical practice guidelines, n (%) | 12 (16) | 22 (31) | 0.03 |
| Not applicable (ie, I always apply SDM)*, n (%) | 11 (14) | 22 (31) | 0.02 |
| I forget to apply SDM, n (%) | 5 (6) | 3 (4) | 0.72 |
| Other, n (%) | 4 (5) | 1 (1) | 0.96 |
| I often know better than patients what the best decision is, n (%) | 2 (3) | 3 (4) | 0.67 |
| I do not know exactly how to apply SDM, n (%) | 1 (1) | 2 (3) | 0.61 |
| My colleagues do not have a positive attitude toward SDM, n (%) | 0 (0) | 1 (1) | 0.48 |
| Shared decision making is not professional, n (%) | – | – | – |
| My employer does not support shared decision making, n (%) | – | – | – |
SDM, shared decision making.
Barriers and facilitators
All identified barriers and facilitators to SDM, grouped according to six levels of the healthcare system, are presented in table 3.12
Table 3.
All identified barriers and facilitators to SDM*, grouped according to six levels of the healthcare system12
| Levels | Barriers | Facilitators |
| The innovation itself | SDM takes too much time There are not always two or more equivalent treatment options available Sometimes decisions are urgent and have to be made right away SDM causes patients to question the expertise of healthcare professionals (nurses only) SDM causes patients distress or discomfort |
SDM saves time in the long run (physicians only) SDM fulfils the ethical imperative of respecting patient autonomy SDM is appropriate regardless of the type of rheumatic disease or decision SDM benefits the professional relationship with patients (physicians only) SDM improves patients’ treatment adherence Ultimately, SDM improves health outcomes |
| The individual professional | Healthcare professionals lack knowledge of what SDM entails Healthcare professionals do not exactly know how to apply SDM Healthcare professionals fall back into routines (ie, they forget to apply SDM) There is a lack of motivation among healthcare professionals to change routines Healthcare professionals lack knowledge of treatment options Healthcare professionals lack communication skills Healthcare professionals do not want to stray away from what they believe is the best decision There are many other things demanding the attention of healthcare professionals |
Healthcare professionals have a (very) positive attitude toward SDM Healthcare professionals feel confident to apply SDM Healthcare professionals have hands-on experience with SDM Healthcare professionals try to imagine themselves in their patients’ shoes There are education programme on SDM available There are communication skills training programme available |
| The patient | Patients do not prefer to be involved in decision making SDM is often too complex for patients (ie, patients are not able to take an active role) Patients lack knowledge of treatment options Patients’ treatment preferences are at odds with those of healthcare professionals Sometimes there are communication issues (eg, language barriers) |
Patients are well-prepared for consultations There is patient information on treatment options available (eg, leaflets, booklets and websites) |
| The social context | The inter-professional collaboration is inadequate (eg, poor communication between physicians and nurses) (nurses only) Colleagues are not supportive (nurses only) |
Physicians and nurses collaborate successfully with each other There is a supportive team culture |
| The organisational context | SDM is incompatible with clinical practice guidelines There is not enough time to apply SDM (ie, consultation times are too short) The workflow does not allow SDM to be easily implemented (eg, poor logistics) (nurses only) There is a lack of tools that support the application of SDM (eg, decision aids) |
Consultation times are long enough to apply SDM |
| The economic and political context | There is a lack of reimbursement for SDM (physicians only) Some treatment options are expensive (physicians only) |
SDM is an important topic in the Dutch healthcare system |
*Barriers and facilitators were experienbed by both physicians and nurses, unless indicated otherwise.
SDM, shared decision making.
Discussion
This is the first study in rheumatology on healthcare professionals’ perspectives of SDM. We explored physicians’ and nurses’ knowledge, attitudes and experiences of SDM in rheumatology and identified barriers and facilitators to SDM. Our results showed that healthcare professionals lacked a full conceptual understanding of SDM. Overall, healthcare professionals had a (very) positive attitude toward SDM. However, the majority of them experienced problems with the application of SDM in clinical practice, mostly related to time constraints. Other important barriers were the incompatibility of SDM with clinical practice guidelines and beliefs that patients do not prefer to be involved in decision making or are not able to take an active role.
Although healthcare professionals reported having decent knowledge of SDM, most of them failed to report a definition of SDM concordant with current consensus in the literature on its definition. Furthermore, communicative behaviours predefined as conflicting with SDM (ie, ‘Explaining to the patient why a certain treatment is chosen’ and ‘Letting the patient decide after giving thorough information’) were rated as essential for SDM by a substantial proportion of healthcare professionals. These results are consistent with those of studies in other clinical specialisations, indicating that healthcare professionals do not fully grasp the concept of SDM.23 27 28 Consequently, healthcare professionals may mistakenly believe that they apply SDM.29 Particularly, they may confuse SDM with informed consent (ie, the patient agrees with a treatment option after being fully informed about the potential risks and benefits and alternatives) or informed decision making. The latter refers to an approach in which, ultimately, the patient independently decides on a treatment option.1 Therefore, increasing healthcare professionals’ conceptual understanding of SDM is an important first step to improve its application in clinical practice.
In this study, we identified a range of barriers and facilitators to SDM corresponding with the literature.10 For example, time constraints and patients’ inability to apply SDM were important barriers also reported in previous studies. Healthcare professionals’ (very) positive attitude toward SDM was an important facilitator also reported previously. The incompatibility of SDM with clinical practice guidelines was an important barrier not frequently reported in previous studies. Indeed, SDM may seem problematic if patients’ treatment preferences are at odds with recommendations of clinical practice guidelines. This result suggests that, in some clinical practices more than others, healthcare professionals feel pressured to strictly follow these guidelines.30 Since clinical practice guidelines do not encompass recommendations for individual patients, deviations may be necessary to ensure that patients are treated as individuals.30–33 Moreover, the American College of Rheumatology and European League Against Rheumatism state that their guidelines are not meant to be prescriptive and warrant SDM.6 7
This study is complementary to a study of Nota and colleagues on patients’ perspectives of SDM in rheumatology.34 Together, our studies cover the perspectives of the most important stakeholders in SDM (ie, healthcare professionals and patients). We found many similarities, suggesting that barriers and facilitators to SDM are largely the same for healthcare professionals and patients. However, an important barrier only reported by Nota and colleagues was patients’ lack of awareness about their ability to make a choice.34 Hence, healthcare professionals have a facilitating role in raising awareness of SDM among patients. Furthermore, it is equally important for healthcare professionals to know whether and to what extent patients prefer to be involved in decision making. In this study, healthcare professionals frequently reported that patients do not prefer to be involved in decision making or are not able to take an active role. However, previous studies have consistently shown that the majority of patients with a rheumatic disease opt for SDM, regardless of their characteristics (eg, age, sex and educational level).34–37 This result suggests that healthcare professionals’ reasons for not applying SDM are partly based on misconceptions, thus stressing the importance of exploring patients’ preferred role in decision making.38
Modest differences between physicians’ and nurses’ perspectives of SDM were found. These differences may be attributed to their specific roles in clinical rheumatology care. For example, significantly more physicians than nurses considered diagnostic testing appropriate for SDM. This seems logical since diagnostic testing is not part of nurses’ common tasks and responsibilities in the treatment of patients with a rheumatic disease. Although physicians’ and nurses’ knowledge, attitudes and experiences of SDM in rheumatology were more or less the same, inadequate inter-professional collaboration was an important barrier. Consequently, patients may receive conflicting information from different healthcare professionals. This result was also found in a study from Hofstede and colleagues on barriers and facilitators to SDM in multidisciplinary sciatica care.39 Therefore, we emphasise the need for better collaboration and communication between healthcare professionals and structured information provision to patients.
There are several strengths and limitations of this study that need consideration. A strength was the inclusion of both physicians and nurses. Most previous studies only covered physicians’ perspectives, leaving the perspectives of other healthcare professionals underexposed. Another strength was that we systematically grouped all identified barriers and facilitators according to six levels of the healthcare system, thus considering a comprehensive spectrum of factors that may affect implementation success.12 A limitation was the low response rate. However, previous studies showed that there is trend towards declining response rates of surveys for healthcare professionals.40 Even a response rate below 10% is nowadays not uncommon.41 Furthermore, it is important to note that healthcare professionals’ answers to questions about their attitudes and experiences of SDM (eg, ‘In what percentage of the situations appropriate for SDM do you apply SDM?’) could be influenced by their own definition of SDM. We can also not exclude the possibility of selection bias since healthcare professionals with a (very) positive attitude toward SDM might have been more inclined to participate. Yet, our sample corresponds with the total population in terms of participants’ demographic characteristics (ie, age, sex, profession, years of work experience and work setting). Finally, replication of this study in other countries is desirable to examine the robustness and generalisability of our results.
In light of our results, there are important practice implications to address the low uptake of SDM in clinical practice. Since we found that healthcare professionals lacked a full conceptual understanding of SDM despite having a (very) positive attitude, there is a clear need for education and training that equips and empowers them to apply SDM. For example, professional organisations may want to consider initiating accredited education and training programmes for their members.42 43 We also advocate for making SDM part of healthcare education curricula. This ensures that all healthcare professionals are reached rather than only those who are interested in the approach. A key message for healthcare professionals, arising from our results, is to ask patients directly about their decision making preferences and to do everything possible to maximise patients’ decisional capacity. Indeed, a patient’s preferred role in decision making cannot be assumed to be similar to that of other patients and may evolve over time.44 Furthermore, our results call for the commitment of time, resources and financial support for national, regional and organisational initiatives to enable healthcare professionals to apply SDM.45 In conclusion, tailored implementation strategies targeting factors related to all levels of the healthcare system are needed to make SDM in rheumatology a practical reality.
Footnotes
Contributors: EGEM: study conception and design, collection of data, analysis and interpretation of data, drafting and critical revision of the manuscript, and approval of the final version of the manuscript. BvdB: study conception and design, critical revision of the manuscript, and approval of the final version of the manuscript. SW: study conception and design, critical revision of the manuscript, and approval of the final version of the manuscript. FvdH: study conception and design, critical revision of the manuscript, and approval of the final version of the manuscript. JEV: study conception and design, analysis and interpretation of data, critical revision of the manuscript, and approval of the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not applicable.
Ethics approval: The Dutch medical research ethical committee of Arnhem-Nijmegen waived ethical approval since this study was not subject to the medical research involving human subjects act (file number 2019–5315).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997;44:681–92. 10.1016/S0277-9536(96)00221-3 [DOI] [PubMed] [Google Scholar]
- 2. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012;27:1361–7. 10.1007/s11606-012-2077-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stacey D, Légaré F, Col NF, et al. Decision AIDS for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2014;1. [DOI] [PubMed] [Google Scholar]
- 4. Elwyn G, Edwards A, Kinnersley P, et al. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract 2000;50:892–9. [PMC free article] [PubMed] [Google Scholar]
- 5. Elwyn G, Frosch D, Rollnick S. Dual equipoise shared decision making: definitions for decision and behaviour support interventions. Implementation Sci 2009;4 10.1186/1748-5908-4-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Singh JA, Saag KG, Bridges SL, et al. 2015 American College of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol 2016;68:1–26. 10.1002/art.39480 [DOI] [PubMed] [Google Scholar]
- 7. Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 2017;76:960–77. 10.1136/annrheumdis-2016-210715 [DOI] [PubMed] [Google Scholar]
- 8. Nota I, Drossaert CHC, Taal E, et al. Patient participation in decisions about disease modifying anti-rheumatic drugs: a cross-sectional survey. BMC Musculoskelet Disord 2014;15:33 10.1186/1471-2474-15-333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mathijssen EGE, Vriezekolk JE, Popa CD, et al. Shared decision making in routine clinical care of patients with rheumatoid arthritis: an assessment of audio-recorded consultations. Ann Rheum Dis 2019:annrheumdis-2019-216137 10.1136/annrheumdis-2019-216137 [DOI] [PubMed] [Google Scholar]
- 10. Légaré F, Ratté S, Gravel K, et al. Barriers and facilitators to implementing shared decision-making in clinical practice: Update of a systematic review of health professionals’ perceptions. Patient Educ Couns 2008;73:526–35. 10.1016/j.pec.2008.07.018 [DOI] [PubMed] [Google Scholar]
- 11. Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns 2014;94:291–309. 10.1016/j.pec.2013.10.031 [DOI] [PubMed] [Google Scholar]
- 12. Grol R, Wensing M. What drives change? barriers to and incentives for achieving evidence‐based practice. Med J Aust 2004;180:S57–60. 10.5694/j.1326-5377.2004.tb05948.x [DOI] [PubMed] [Google Scholar]
- 13. Chaudoir SR, Dugan AG, Barr CHI. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implementation Sci 2013;8 10.1186/1748-5908-8-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Scholl I, LaRussa A, Hahlweg P, et al. Organizational- and system-level characteristics that influence implementation of shared decision-making and strategies to address them — a scoping review. Implementation Sci 2018;13 10.1186/s13012-018-0731-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Baker R, Camosso-Stefinovic JF, Gillies CF, et al. Tailored interventions to address determinants of practice. Cochrane Database Syst Rev 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clark NM, Nelson BW, Valerio MA, et al. Consideration of Shared Decision Making in Nursing: A Review of Clinicians’ Perceptions and Interventions. Open Nurs J 2009;3:65–75. 10.2174/1874434600903010065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bech B, Primdahl J, van Tubergen A, et al. Update of the EULAR recommendations for the role of the nurse in the management of chronic inflammatory arthritis. Ann Rheum Dis 2018;2019. [DOI] [PubMed] [Google Scholar]
- 18. Elm Evon, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet E-Surveys (cherries). J Med Internet Res 2004;6:e34 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nederlandse Vereniging voor Reumatologie Dutch rheumatology association, 2019. Available: https://www.nvr.nl [Accessed 4 Sep 2019].
- 21. Rheumatology unit of the Dutch association for physician assistants, 2019. Available: https://www.napa.nl [Accessed 4 Sep 2019].
- 22. Rheumatology unit of the Dutch nurses association, 2019. Available: https://www.venvn.reumatologie.nl [Accessed 4 Sep 2019].
- 23. Woltz S, Krijnen P, Pieterse AH, et al. Surgeons’ perspective on shared decision making in trauma surgery. A national survey. Patient Educ Couns 2018;101:1748–52. 10.1016/j.pec.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 24. Degner LF, Sloan JA, Venkatesh P. The control preferences scale. Can J Nurs Res 1997;29:21–43. [PubMed] [Google Scholar]
- 25. Covvey JR, Kamal KM, Gorse EE, et al. Barriers and facilitators to shared decision-making in oncology: a systematic review of the literature. Support Care Cancer 2019;27:1613–37. 10.1007/s00520-019-04675-7 [DOI] [PubMed] [Google Scholar]
- 26. Boland L, Graham ID, Légaré F, et al. Barriers and facilitators of pediatric shared decision-making: a systematic review. Implement Sci 2019;14 10.1186/s13012-018-0851-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Forcino RC, Yen RW, Aboumrad M, et al. US-based cross-sectional survey of clinicians’ knowledge and attitudes about shared decision-making across healthcare professions and specialties. BMJ Open 2018;8:e022730 10.1136/bmjopen-2018-022730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Topp J, Westenhöfer J, Scholl I, et al. Shared decision-making in physical therapy: A cross-sectional study on physiotherapists’ knowledge, attitudes and self-reported use. Patient Educ Couns 2018;101:346–51. 10.1016/j.pec.2017.07.031 [DOI] [PubMed] [Google Scholar]
- 29. Pollard S, Bansback N, Bryan S. Physician attitudes toward shared decision making: a systematic review. Patient Educ Couns 2015;98:1046–57. 10.1016/j.pec.2015.05.004 [DOI] [PubMed] [Google Scholar]
- 30. van der Weijden T, Pieterse AH, Koelewijn-van Loon MS, et al. How can clinical practice guidelines be adapted to facilitate shared decision making? A qualitative key-informant study. BMJ Qual Saf 2013;22:855–63. 10.1136/bmjqs-2012-001502 [DOI] [PubMed] [Google Scholar]
- 31. Guerrier M, Légaré F, Turcotte S, et al. Shared decision making does not influence physicians against clinical practice guidelines. PLoS One 2013;8:e62537 10.1371/journal.pone.0062537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ansmann L, Pfaff H. Providers and Patients Caught Between Standardization and Individualization: Individualized Standardization as a Solution Comment on "(Re) Making the Procrustean Bed? Standardization and Customization as Competing Logics in Healthcare". Int J Health Policy Manag 2017;7:349–52. 10.15171/ijhpm.2017.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mannion R, Exworthy M. (Re) making the procrustean bed? standardization and Customization as competing logics in healthcare. Int J Health Policy Manag 2017;6:301–4. 10.15171/ijhpm.2017.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nota I, Drossaert CHC, Taal E, et al. Arthritis patients’ motives for (not) wanting to be involved in medical decision-making and the factors that hinder or promote patient involvement. Clin Rheumatol 2016;35:1225–35. 10.1007/s10067-014-2820-y [DOI] [PubMed] [Google Scholar]
- 35. Chilton F, Collett RA. Treatment choices, preferences and decision-making by patients with rheumatoid arthritis. Musculoskeletal Care 2008;6:1–14. 10.1002/msc.110 [DOI] [PubMed] [Google Scholar]
- 36. Mahlich J, Sruamsiri R. Preference for shared decision-making in Japanese patients with rheumatoid arthritis. Cogent Medicine 2017;4 10.1080/2331205X.2017.1353262 [DOI] [Google Scholar]
- 37. Fraenkel L, Nowell WB, Michel G, et al. Preference phenotypes to facilitate shared decision-making in rheumatoid arthritis. Ann Rheum Dis 2018;77:678–83. 10.1136/annrheumdis-2017-212407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Stiggelbout AM, Weijden TVd, Wit MPTD, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ 2012;344:e256 10.1136/bmj.e256 [DOI] [PubMed] [Google Scholar]
- 39. Hofstede SN, Marang-van de Mheen PJ, Wentink MM, et al. Barriers and facilitators to implement shared decision making in multidisciplinary sciatica care: a qualitative study. Implementation Sci 2013;8 10.1186/1748-5908-8-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: an observational study. BMC Health Serv Res 2009;9:160 10.1186/1472-6963-9-160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Van Mol C. Improving web survey efficiency: the impact of an extra reminder and reminder content on web survey response. Int J Soc Res Methodol 2017;20:317–27. 10.1080/13645579.2016.1185255 [DOI] [Google Scholar]
- 42. Légaré F, Witteman HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Aff 2013;32:276–84. 10.1377/hlthaff.2012.1078 [DOI] [PubMed] [Google Scholar]
- 43. Légaré F, Stacey D, Turcotte S, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev 2014;9. [DOI] [PubMed] [Google Scholar]
- 44. Chewning B, Bylund CL, Shah B, et al. Patient preferences for shared decisions: a systematic review. Patient Educ Couns 2012;86:9–18. 10.1016/j.pec.2011.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. van der Weijden T, Post H, Brand PLP, et al. Shared decision making, a buzz-word in the Netherlands, the PACE quickens towards nationwide implementation. Z Evid Fortbild Qual Gesundhwes 2017;123:69–74. 10.1016/j.zefq.2017.05.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2019-001121supp001.pdf (89.2KB, pdf)