Abstract
Background
Non-bacterial thrombotic endocarditis (NBTE) is a rare condition, usually observed in association with malignancy, lupus erythematosus, or antiphospholipid syndrome. Diagnosis of NBTE remains a challenge as patients are often asymptomatic up to their first thromboembolic event. While there is no randomized data available for the guidance of treatment in NBTE, effective anticoagulation remains the main focus in the management of affected patients.
Case summary
A 44-year-old female patient without a significant medical history presented to the emergency department with a new numbness of her right hand. Magnetic resonance imaging scans facilitated the diagnosis of supratentorial stroke. Within the next 3 months, the patient had multiple thromboembolic events, including multiple strokes, pulmonary embolism, and renal/splenic infarction. Echocardiographic examination revealed large, transient vegetations of the aortic valve with concomitant aortic regurgitation. In addition, an incidental, pulmonary non-small-cell adenocarcinoma was found during the diagnostic work-up. Infective endocarditis was excluded by several negative blood cultures and missing signs of infection. Hence, the diagnosis of NBTE secondary to malignancy was made.
Discussion
We present a rare case of NBTE in the context of pulmonary adenocarcinoma. The adequate treatment of malignancy and effective anticoagulation are the main treatment options.
Keywords: Non-bacterial thrombotic endocarditis, Thromboembolism, Anticoagulation, Malignancy, Case report
Learning points
Non-bacterial thrombotic endocarditis (NBTE) is a rare condition, which should be considered in patients with recurrent thromboembolic events, especially in context of active malignancy.
While there is no randomized trial data guiding treatment of NBTE, adequate anticoagulation and short-term follow-up are essential in the management of patients with NBTE.
Introduction
Non-bacterial thrombotic endocarditis (NBTE) is a rare condition that is commonly observed in the context of malignancy. It is also associated with antiphospholipid syndrome and systemic lupus erythematosus. The diagnosis is often made post-mortem, as patients remain asymptomatic up to their first thromboembolic episode. Prevalence rates of up to 4% have been reported in patients with end-stage cancer. Typical presentation includes the deposition of thrombi on normal appearing heart valves and an increased rate of thromboembolic events without typical signs of an infectious disease.
Timeline
| Timeline | Events |
|---|---|
| Day 1 |
|
| Week 3 |
|
| Week 6 |
|
| Week 8 |
|
| Week 12 |
|
| Month 10 |
|
Case presentation
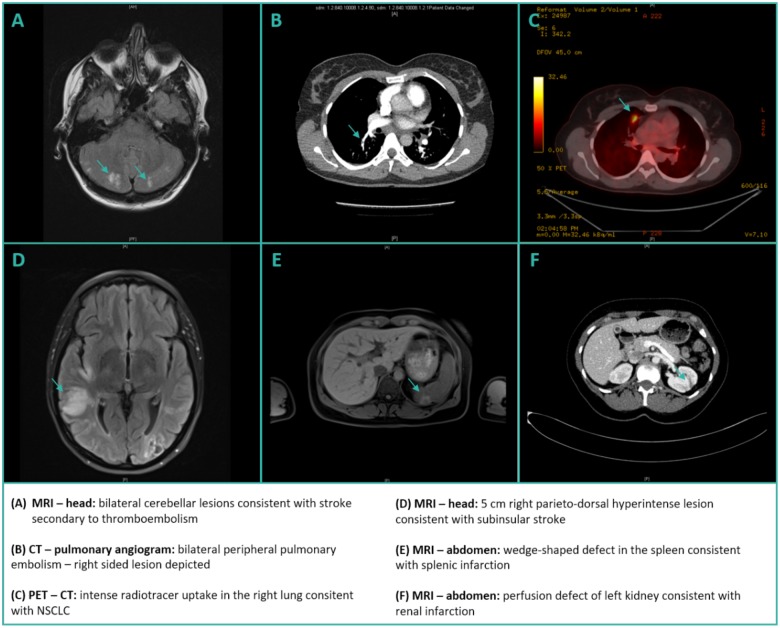
A 44-year-old female patient presented to the emergency department with the chief complaint of new-onset of numbness of her right hand. Except for a history of latent hypothyroidism, not requiring thyroid hormone replacement (<5 μU/mL), the patient was previously fit and well without a history of smoking or alcohol abuse. On examination, a neurologically suspect numbness of the fingers I–III of the right hand was confirmed. The rest of the physical examination was unremarkable and vital signs were stable. The patient underwent immediate magnetic resonance imaging (MRI) of the head, which showed significant bilateral supratentorial hyperintensity facilitating the diagnosis of stroke. In addition, bilateral peripheral pulmonary embolism was observed on pulmonary computed tomography (CT)-angiogram issued secondary to new-onset dyspnoea (Figure 2). Therapeutic anticoagulation with enoxaparin twice daily was initiated and an initial tentative diagnosis of a thromboembolic stroke was made. Transthoracic echocardiogram (TTE) in the emergency department showed normal left ventricular function without clear evidence of vegetations. However, a mild- to moderate tricuspid regurgitation was found, which was no longer visible on short-term follow-up TTE.
Figure 2.
Imaging of thromboembolic events/pulmonary carcinoma. (A) Magnetic resonance imaging—head: bilateral cerebellar lesions consistent with stroke secondary to thromboemblosim. (B) Computed tomography-pulmonary angiogram: bilateral peripheral pulmonary embolism—right-sided lesion depicted. (C) Positron emission tomography–computed tomography: intense radiotracer uptake in the right lung consistent with non-small-cell lung cancer. (D) Magnetic resonance imaging—head: 5 cm right parieto-dorsal hyperintense lesion consistent with subinsular stroke. (E) Magnetic resonance imaging—abdomen: wedge-shaped defect in the spleen consistent with splenic infarction. (F) Magnetic resonance imaging—abdomen: perfusion defect of left kidney consistent with renal infarction.
To further evaluate an incidental, suspect pulmonary lesion on chest X-ray and CT scan (large, ill-defined nodule), the decision to perform bronchoscopy was made to obtain material for histological preparation and mutation analysis. Once work up of diagnostic material was finished, an interdisciplinary expert tumour board, made the diagnosis of a non-small-cell adenocarcinoma of the right upper pulmonary lobe [TTF 1 positive, ALK negative, PD-L1 90% positive, and epidermal growth factor receptor (EGFR) positive with exon 19 deletion] with osseous metastases and a singular, hepatic metastasis. Following the promising results of the FLAURA study (Osimertinib in Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer)1 treatment with osimertinib, an EGFR tyrosine kinase inhibitor, was initiated and the patient was discharged home in a stable physical condition.
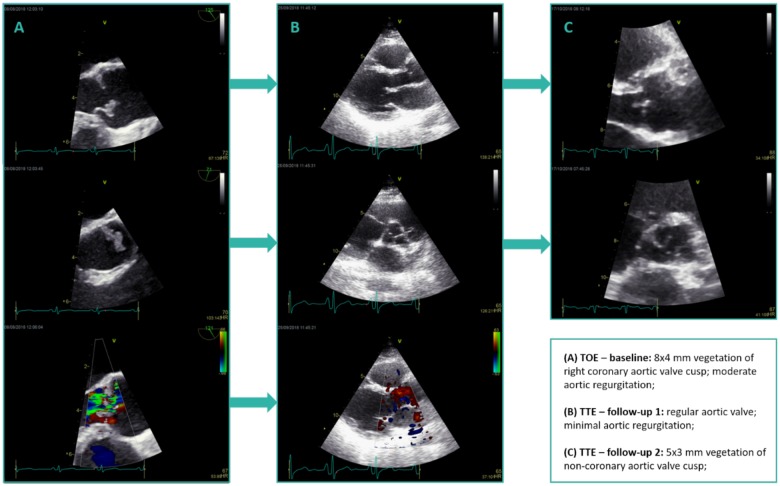
Unfortunately, the patient returned to the emergency department within 2 weeks of discharge with a new numbness of her left forearm, visual impairments, and headaches. Urgent MRI was issued, which revealed bilateral supratentorial and infratentorial strokes, significantly progressive from the previously performed MRI scans. At this point, the patient was referred to our cardiological department for the conduction of a transoesophageal echocardiography (TOE). Performance of a TOE earlier in the disease course was not possible due to a pronounced pharyngeal reflex. Transoesophageal echocardiography revealed an 8 × 4 mm vegetation of the right coronary cusp of the aortic valve with concomitant moderate aortic regurgitation (concentric jet with a vena contracta width of 4 mm and a pressure half time of 364 ms with a deceleration time of 1254 ms; Figure 1, Supplementary material). While the echocardiographic findings suggested aortic valve endocarditis, several consecutive blood cultures remained negative and the patient showed no signs of infectious disease (no fever, only minimal, clinically non-relevant C-reactive protein elevation; Table 1). There was also no microbiological growth of bacteria from the HACEK group, which are Gram-negative bacteria and a rare cause of infective endocarditis. Regardless, empiric antibiotic treatment with amoxicillin and clavulanic acid was initiated and therapeutic anticoagulation with enoxaparin continued. Sixty milligrams of enoxaparin were given twice daily as the patient had a weight of 62 kg and normal renal function. Upon abdominal MRI scans, renal and splenic infarction were observed (Figure 2). Extensive testing for an autoimmune disease (no evidence of antiphospholipid syndrome or lupus erythematosus) or coagulopathy remained negative.
Figure 1.
Echocardiographic findings. (A) Transoesophageal echocardiography—baseline: 8 × 4 mm vegetation of right coronary aortic valve cusp; moderate aortic regurgitation; (B) transthoracic echocardiography—follow-up 1: regular aortic valve; minimal aortic regurgitation; and (C) transthoracic echocardiography—follow-up 2: 5 × 3 mm vegetation of non-coronary aortic valve cusp.
Table 1.
Laboratory values of interest
| Laboratory values | Reference range | Patient—max level |
|---|---|---|
| White blood cells | 4–10 G/L | 9.4 G/L |
| Neutrophile granulocytes | 1.9–8 G/L | 6.8 G/L |
| CRP | <5 mg/dL | 26.5 mg/dL |
| Creatinine | 0.6–1.0 mg/dL | 1.1 mg/dL |
| eGFR | >60 mL/min/1.73 m² | >60 mL/min/1.73 m² |
| NT-proBNP | 0–125 ng/L | 710 ng/L |
| HbA1c | 4–5.6% | 5.1% |
| TSH | 0.3–3.0 µU/mL | 3.6 µU/mL |
| CYFRA 21-1 | 0–3.3 μg | 5.5 μg |
CRP, C-reactive protein; eGFR, estimated glomerular filtration rate (MDRD-formula); HbA1c, haemoglobin A1c; NT-proBNP, N-terminal prohormone of brain natriuretic peptide; TSH, thyroid-stimulating hormone.
Aside from continued cervical and thoracic spine pain, secondary to osseous metastases, the patient was feeling well and was subsequently discharged from the hospital with close follow-up scheduled. Two weeks later, TOE revealed a complete resolution of the aortic valve vegetation and a significant decline in the severity of aortic regurgitation.
After 4 weeks, the patient was readmitted to the hospital due to a new onset of aphasia, which was confirmed as a recurrence of right-sided subinsular stroke by cerebral MRI. Transthoracic echocardiography (TTE) at admission showed no progression of the mild aortic regurgitation. Transthoracic echocardiogram prior to discharge, however, revealed a new 5 × 3 mm vegetation of the left coronary cusp of the aortic valve (Figure 1, Supplementary material). The recurring aortic valve vegetations combined with multiple thromboembolic events at different sites in the context of malignancy and the missing signs of infectious disease facilitated the diagnosis of NBTE. Taking the preference of the patient into account, she was discharged home on long-term anticoagulation with rivaroxaban 15 mg once daily combined with antithrombotic treatment with clopidogrel 75 mg once daily. However, one may note that the chosen antithrombotic treatment regimen is off-label in the setting of NBTE.
Follow-up at 10 months revealed marked clinical improvement without evidence of thromboembolic recurrences.
Discussion
Non-bacterial thrombotic endocarditis is a rare condition characterized by the deposition of sterile thrombi on mainly left-sided heart valves and recurrent thromboembolic events. While data on the incidence of NBTE is limited, there appears to be a significant association with malignancy secondary to the state of hypercoagulability in cancer. Other conditions such as systemic lupus erythematosus, which leads to typical Libman–Sacks vegetations, and antiphospholipid syndrome have been observed in association with NBTE as well.2,3
Transthoracic echocardiography and TOE are important diagnostic modalities in the work-up of patients with suspected NBTE. Paradoxically, the disease usually effects valvular leaflets in high flow areas, such as the aortic or mitral valve.2 Contrary to infectious endocarditis, the vegetations in NBTE are not of inflammatory nature and can be classified as fibrin rich ‘white thrombi’. They are often only loosely connected to the heart valves as there is no inflammatory reaction at the site of attachment, which in turn precipitates dislodgement with following embolization. Additional important diagnostic procedures include a complete laboratory assessment with full blood count and chemistry, as well as several sets of blood cultures obtained at different sites.4–6
As there are no randomized controlled trials guiding the treatment of patients with NBTE, evidence is based on small observational studies. The 2015 European Society of Cardiology (ESC) guidelines for endocarditis7 underline the importance of anticoagulation as the mainstay of treatment in patients with NBTE secondary to the risk of recurrent embolization and the fragile nature of the thrombi. Currently, subcutaneous low molecular weight heparin is the anticoagulant of choice. However, an off-label switch to warfarin or a direct thrombin/factor Xa inhibitor may be a reasonable choice in young patients to avoid lifelong heparin treatment. In our case, dual antithrombotic therapy (DAT) with rivaroxaban and clopidogrel was chosen. The dosage was based on the results of the PIONEER AF-PCI study, which evaluated the efficacy of DAT in patients with atrial fibrillation after percutaneous coronary intervention.8 Following the initiation of anticoagulation haemorrhagic conversion of embolic events may occur. Another treatment option in NBTE includes surgical intervention in case of persistent, haemodynamically significant valvular disease. Indication for surgery should be based on the guidelines for conventional infective endocarditis. Naturally, treatment of the underlying cause for NBTE is necessary, if one can be identified.3,9
Lead author biography

Dr Christoph C. Kaufmann has finished his medical doctorate in 2016 and is currently employed as a cardiology fellow at the Wilhelminenhospital in Vienna. In addition, he is studying on his PhD degree at the medical university of Vienna.
Funding
The research was supported by the Ludwig Boltzmann Cluster for Cardiovascular Research, Vienna, and the Association for the Promotion of Research in Arteriosclerosis, Thrombosis and Vascular Biology (ATVB), Vienna.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Soria J-C, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, Dechaphunkul A, Imamura F, Nogami N, Kurata T, Okamoto I, Zhou C, Cho BC, Cheng Y, Cho EK, Voon PJ, Planchard D, Su W-C, Gray JE, Lee S-M, Hodge R, Marotti M, Rukazenkov Y, Ramalingam SS; FLAURA Investigators. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med 2018;378:113–125. [DOI] [PubMed] [Google Scholar]
- 2. Steiner I. Nonbacterial thrombotic endocarditis—a study of 171 case reports. Cesk Patol 1993;29:58–60. [PubMed] [Google Scholar]
- 3. Liu J, Frishman WH.. Nonbacterial thrombotic endocarditis: pathogenesis, diagnosis, and management. Cardiol Rev 2016;24:244–247. [DOI] [PubMed] [Google Scholar]
- 4. Allen AC, Sirota JH.. The morphogenesis and significance of degenerative verrucal endocardiosis (terminal endocarditis, endocarditis simplex, nonbacterial thrombotic endocarditis). Am J Pathol 1944;20:1025–1055. [PMC free article] [PubMed] [Google Scholar]
- 5. Asopa S, Patel A, Khan OA, Sharma R, Ohri SK.. Non-bacterial thrombotic endocarditis. Eur J Cardiothorac Surg 2007;32:696–701. [DOI] [PubMed] [Google Scholar]
- 6. Roldan CA, Sibbitt WL, Qualls CR, Jung RE, Greene ER, Gasparovic CM, Hayek RA, Charlton GA, Crookston K.. Libman-Sacks endocarditis and embolic cerebrovascular disease. JACC Cardiovasc Imaging 2013;6:973–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta J-P, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL; ESC Scientific Document Group. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015;36:3075–3128. [DOI] [PubMed] [Google Scholar]
- 8. Gibson CM, Mehran R, Bode C, Halperin J, Verheugt F, Wildgoose P, van Eickels M, Lip GY, Cohen M, Husted S, Peterson E, Fox K.. An open-label, randomized, controlled, multicenter study exploring two treatment strategies of rivaroxaban and a dose-adjusted oral vitamin K antagonist treatment strategy in subjects with atrial fibrillation who undergo percutaneous coronary intervention (PIONEER AF-PCI). Am Heart J 2015;169:472–478.e5. [DOI] [PubMed] [Google Scholar]
- 9. Rogers LR, Cho ES, Kempin S, Posner JB.. Cerebral infarction from non-bacterial thrombotic endocarditis. Clinical and pathological study including the effects of anticoagulation. Am J Med 1987;83:746–756. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.