Abstract
Background
Taxus baccata, also known as English yew, is a poison that causes cardiac arrhythmias and can result in death from cardiogenic shock.
Case summary
A 49-year-old gentleman was admitted following yew ingestion with suicidal intent. He was bradycardic at 30 b.p.m. and hypotensive on arrival. Electrocardiography revealed complete heart block with broad complex ventricular escape rate of 30 b.p.m. Bedside echocardiography revealed severe global impairment of right and left ventricular systolic function. Urgent temporary transvenous pacing was instituted, and the patient was considered for veno-arterial extracorporeal membrane oxygenation. Unfortunately, he deteriorated rapidly and cardiorespiratory arrest ensued, and despite prolonged in-hospital resuscitation, the patient died. Post-mortem examination revealed small needle-shaped plant leaves together with seeds found in the stomach. Ante mortem serum sample analysis sent to the Royal Botanical Gardens and revealed the presence of taxine Type B alkaloids in the patient’s blood.
Discussion
Yew poisoning is a rare occurrence, and there is currently no effective antidote. Treatment involves supportive management, comprising prolonged effective cardiopulmonary resuscitation, pacing, and mechanical cardiac support. This case illustrates the importance of prompt recognition of yew poisoning, alongside early consideration of pacing and mechanical cardiac support. Due to the rarity of this cause of heart block, and since patients may not always volunteer a history of yew ingestion, yew poisoning is something that physicians should be aware of and this should be considered in the differential diagnosis in patients with unexpected heart block. Serum analysis for taxine alkaloids can be used to confirm the diagnosis.
Keywords: Yew, Taxus baccata, Taxine alkaloids, Poisoning, Complete heart block, Case report
Learning points
Yew poisoning is a rare cause of complete heart block, which can lead to cardiogenic shock and death, with no effective antidote.
Treatment is supportive and includes temporary pacing and mechanical support.
We advocate early transfer to tertiary centres with extracorporeal membrane oxygenation facilities, given the low success rate of pacing in cases of yew poisoning.
Introduction
Taxus baccata, also known as English yew, is an evergreen conifer that is traditionally used in ornamental sculpture and woodwork. It is inexpensive and widely available in Europe and Asia. Throughout history, yew tree species have been implicated in human and animal poisoning.1 All parts of the yew tree, except for the red aril, contain taxine alkaloids.1 Taxine B is the most potent alkaloid with respect to toxicity.1 Taxines cause dose-dependent blockade of calcium and sodium channels, resulting in pronounced QRS prolongation, decreased myocardial contractility, and prolonged atrioventricular conduction time. Minimum lethal doses are reported to range from 0.6 to 1.3 g yew leaves/kg body weight, and intoxication is known to be resistant to standard treatments with no effective antidote.1
We present the case of a fatal intentional ingestion of various yew tree constituents and the experience gained from a cardiology perspective.
Timeline
| 6 h prior to admission | Deliberate ingestion of approximately 50 g of yew leaves and seeds. |
| 30 min prior to admission |
|
| Admission to hospital | Profoundly bradycardic with complete heart block and hypotension. |
| 35 min post-admission |
|
| 1 h 20 min post-admission | Failing to capture with temporary pacing wire despite good lead position. Cardiac arrest in the cardiac catheterization laboratory. Cardiopulmonary resuscitation commenced, patient intubated, and ventilated. |
| 1 h 35 min post-admission | Venoarterial-extracorporeal membrane oxygenation discussed with tertiary centre, but patient too unstable to be transported and deteriorating rapidly. |
| 2 h 30 min post-admission |
|
| 3 days post-admission | Post-mortem revealed stomach contents of needle-shaped leaves and seeds. Ante mortem serum analysis revealed presence of taxine Type B alkaloids. |
Case presentation
A well-built 49-year-old gentleman with a history of depression was brought in by the ambulance following intentional ingestion of yew tree leaves and seeds (∼50 g) as a suicide attempt. The patient also reported consuming yew tree oil the previous day with no effect. On assessment by the ambulance crew, he was found to be profoundly bradycardic, with a heart rate of 38 b.p.m. and hypotensive with blood pressure (BP) of 79/47 mmHg. Prior to arrival at the hospital, he was treated with bolus intravenous saline challenges and intravenous boluses of 600 μg of atropine, totalling 1800 μg.
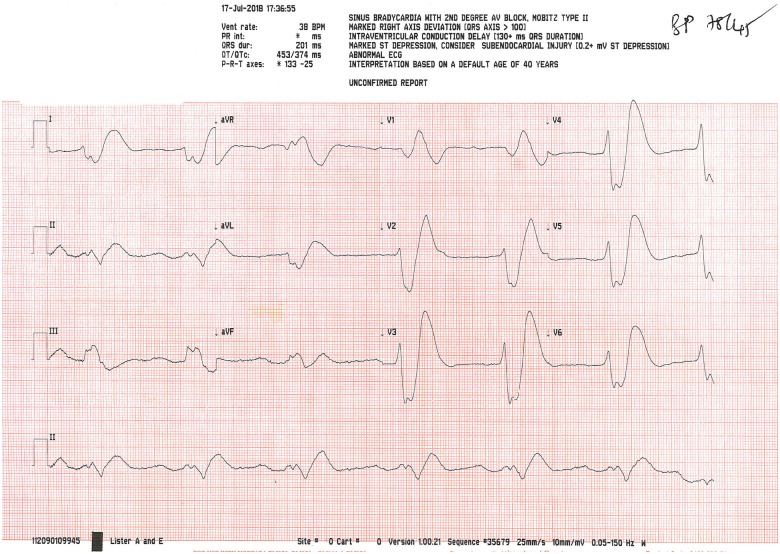
On admission, the patient was drowsy but coherent and responsive to questions. He admitted to taking yew tree oil and seeds with suicidal intent at 09.30 that morning. He was on sertraline for depression, which was first diagnosed 20 years ago. On examination, he was profoundly bradycardic with a heart rate of 30 b.p.m. and hypotensive with BP of 70/50 mm Hg. His cardiorespiratory, abdominal, and neurological examinations were otherwise unremarkable. The electrocardiogram (ECG) (Figure 1) revealed complete heart block with very broad QRS complex. The patient’s clinical presentation was quickly recognized to be due to yew poisoning after consulting the UK National Poisoning Information Service’s (NPIS) online database, TOXBASE®. He was then transferred as an emergency to the cardiac catheterization laboratory for temporary pacing wire insertion. The patient was paced at 100 b.p.m. with increasing output due to difficulty in capture, but even with adequate pacing capture, the VP did not respond. Eventually, there was failure of electrical capture. Bedside echocardiography revealed severe global biventricular impairment of right and left ventricular systolic function. The systolic BP continued to fall to 50 mmHg, and asystole ensued. Cardiopulmonary resuscitation (CPR) was commenced in accordance with the UK Resuscitation Council’s Advance Life Support guidelines and the patient was intubated and ventilated.
Figure 1.
Electrocardiogram on admission revealing complete heart block with broadened, bizarre, and sinusoidal QRS appearance.
Treatment with 50 mL sodium bicarbonate 8.4%, 10 mL 10% calcium gluconate, and 1 mg of adrenaline was administered within the first cycle of CPR. The local extracorporeal membrane oxygenation (ECMO) life support team was contacted and the patient provisionally accepted for transfer. Continuous CPR with the LUCAS® chest compression system was initiated an hour into the arrest, in preparation for transfer to the ECMO unit. The patient’s rhythm hitherto had predominantly shown pulseless electrical activity (PEA) and asystole on rhythm checks. There were three documented ventricular tachycardia episodes requiring defibrillation. There were intermittent episodes of return of spontaneous circulation, with a BP of 140/90 mmHg, but each time this was followed by PEA or asystole. Despite prolonged resuscitation period of 1 h and 50 min, serial arterial blood gases continued to deteriorate, with progressive mixed metabolic and respiratory acidosis, Type 2 respiratory failure, a rising lactate and hyperglycaemia (Table 1). This reflects the patient’s critical condition owing to inadequate cardiac output despite persistent resuscitation efforts. After prolonged resuscitation, the patient died 3 h and 12 min post-admission.
Table 1.
Serial arterial blood gas results during the admission reflecting biochemical deterioration
| Time post-admission | 20 min | 1 h 30 min | 2 h 5 min | 2 h 30 min | Normal ranges |
|---|---|---|---|---|---|
| pH | 7.280 | 7.287 | 7.023 | 6.897 | 7.350–7.450 |
| pCO2 (kPa) | 6.11 | 6.41 | 8.16 | 9.68 | 4.70–6.00 |
| pO2 (kPa) | 2.98 | 1.98 | 8.35 | 8.26 | 10.70–14.60 |
| HCO3 (mmol/L) | 21.0 | 22.5 | 15.6 | 13.8 | 23.0–30.0 |
| BE (mmol/L) | −5.7 | −4.5 | −16.0 | −20.3 | −1 to +1 |
| Na (mmol/L) | 140.6 | 141.4 | 142 | 138.8 | 133.0–146.0 |
| K (mmol/L) | 3.96 | 4.05 | 4.22 | 3.35 | 3.50–5.30 |
| Ca (mmol/L) | 1.19 | 1.33 | 1.25 | 1.31 | 1.15–1.33 |
| Cl (mmol/L) | 105 | 106 | 101 | 107 | 95–108 |
| Glu (mmol/L) | 9.4 | 8.9 | 20.7 | 22.3 | 3.5–6.0 |
| Lac (mmol/L) | 4.30 | 4.17 | 11.76 | 11.37 | 1.00–1.80 |
| FiO2 (%) | 60.0 | 20.0 | 100.0 | 100.0 | 21.0 |
Bold values represent values outside the normal range.
Post-mortem examination revealed small needle-shaped plant leaves together with seeds found in the stomach. Ante mortem serum sample analysis sent to the Royal Botanical Gardens and revealed the presence of taxine Type B alkaloids in the patient’s blood. Given the history, serum analysis and post-mortem findings, the cause of death was deemed to be due to yew (leaves, oil, and seed) poisoning.
Discussion
Taxine alkaloids are the active constituents in yew plants that cause cardiotoxicity.1 These alkaloids are present in all parts of the plant, apart from the fleshy red part of the plant, the aril.2 Our patient ingested an equivalent of around 0.7–0.8 g/kg of yew tree leaves, seed, and oil. According to Wilson et al.,1 the lethal oral dose of yew leaves in humans range from 0.6 to 1.3 g yew leaves/kg body weight. Yew tree poisoning has a high mortality rate, but remains a rare occurrence, with only a handful of case reports in the literature.3–14
Cardiotoxicity occurs via the blockade of sodium and calcium channels in cardiac myocytes, leading to atrioventricular block, evidenced by prolonged PR and QRS intervals on the ECG.1 The clinical severity is dependent on quantity, type and route of exposure, and whether the seed was chewed or only swallowed.2 Clinical signs and symptoms usually occur within 3–4 h following ingestion, and include dizziness, pupillary dilation, nausea and vomiting, abdominal pain, muscle weakness, and seizures.1,2 Patients may present with an initial tachycardia, however, can progress rapidly to bradycardia, cardiac standstill, and death secondary to cardiogenic shock. Presently, there is no effective antidote, and management of yew poisoning is largely supportive, including activated charcoal, fluid resuscitation, electrolyte replacement, inotropic support, and prolonged CPR in light of the long duration of cardiotoxicity of taxines.2,14
Temporary transvenous pacemaker insertion or external pacing should be considered, although electrical capture may be challenging, and was unsuccessful in the majority of the yew tree poisoning cases.2,5 The UK NPIS do not advocate gastric decontamination as the benefit is unclear.2 Although not licensed for this purpose, digoxin-specific fragment antigen-binding (Fab) has been shown to be beneficial if administered early.2,5 Other adjuncts include the use of lidocaine and lipid emulsion.2 Mechanical cardiac support, including venoarterial-ECMO or an intra-aortic balloon pump may be considered if other measures have failed, and if there is life-threatening haemodynamic instability.2,14
Given the prevalence of yew trees in Europe and publicized content on the internet as a method of suicide,15 yew poisoning is easily accessible. As such, this highlights the importance of early recognition of yew poisoning, anticipation of cardiac arrhythmias, and prompt management with supportive treatment, prolonged CPR and consideration of electrical and mechanical cardiac support. On hindsight, we advocate early transfer to tertiary centres with ECMO facilities, given the low success rate of pacing in cases of yew poisoning. Although it is reassuring that these cases remain a rarity, such cases should be recorded nationally, to improve the understanding and management through pooled data.
Lead author biography
Dr Natasha G. is an academic foundation doctor at Cambridge University Hospitals NHS trust. She graduated from University College London medical school and received a 1st class honours and Dean’s List nomination for her intercalated BSc in medical science with surgical sciences.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Wilson CR, Sauer J, Hooser SB.. Taxines: a review of the mechanism and toxicity of yew (Taxus spp.) alkaloids. Toxicon 2001;39:175–185. [DOI] [PubMed] [Google Scholar]
- 2.National Poisons Information Service [Internet]. https://www.toxbase.org/ (13 December 2019).
- 3. Baum C, Bohnen S, Sill B, Philipp S, Damerow H, Kluge S, Reichenspurner H, Blankenberg S, Soffker G, Barten MJ, Sydow K.. Prolonged resuscitation and cardiogenic shock after intoxication with European yew (Taxus baccata): Complete recovery after intermittent mechanical circulatory support. Int J Cardiol 2015;181:176–178. [DOI] [PubMed] [Google Scholar]
- 4. Cummins RO, Haulman J, Quan L, Graves JR, Peterson D, Horan S.. Near-fatal yew berry intoxication treated with external cardiac pacing and digoxin-specific FAB antibody fragments. Ann Emerg Med 1990;19:38–43. [DOI] [PubMed] [Google Scholar]
- 5. Farag M, Badowski D, Koschny R, Skopp G, Brcic A, Szabo GB.. Extracorporeal life support and digoxin-specific Fab fragments for successful management of Taxus baccata intoxication with low output and ventricular arrhythmia. Am J Emerg Med 2017;35:1987.e3–1987.e7. [DOI] [PubMed] [Google Scholar]
- 6. Lassnig E, Heibl C, Punzengruber C, Eber B.. ECG of a “dying heart” in a young woman—a case of yew poisoning. Int J Cardiol 2013;167:e71–e73. [DOI] [PubMed] [Google Scholar]
- 7. Panzeri C, Bacis G, Ferri F, Rinaldi G, Persico A, Uberti F, Restani P.. Extracorporeal life support in a severe Taxus baccata poisoning. Clin Toxicol (Phila) 2010;48:463–465. [DOI] [PubMed] [Google Scholar]
- 8. Pierog J, Kane B, Kane K, Donovan JW.. Management of isolated yew berry toxicity with sodium bicarbonate: a case report in treatment efficacy. J Med Toxicol 2009;5:84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Soumagne N, Chauvet S, Chatellier D, Robert R, Charriere JM, Menu P.. Treatment of yew leaf intoxication with extracorporeal circulation. Am J Emerg Med 2011;29:354 e5–e6. [DOI] [PubMed] [Google Scholar]
- 10. Thooft A, Goubella A, Fagnoul D, Taccone FS, Brimioulle S, Vincent JL, De Backer D.. Combination of veno-arterial extracorporeal membrane oxygenation and hypothermia for out-of-hospital cardiac arrest due to Taxus intoxication. CJEM 2014;16:504–507. [DOI] [PubMed] [Google Scholar]
- 11. Vališ M, Kočí J, Tuček D, Lutonský T, Kopová J, Bartoń P, Vyšata O, Krajíčková D, Korábečný J, Masopust J, Klzo L.. Common yew intoxication: a case report. J Med Case Rep 2014;8:4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Van Ingen G, Visser R, Peltenburg H, Van Der Ark AM, Voortman M.. Sudden unexpected death due to Taxus poisoning. A report of five cases, with review of the literature. Forensic Sci Int 1992;56:81–87. [DOI] [PubMed] [Google Scholar]
- 13. Willaert W, Claessens P, Vankelecom B, Vanderheyden M.. Intoxication with Taxus baccata: cardiac arrhythmias following yew leaves ingestion. Pacing Clin Electrophysiol 2002;25(4 Pt 1):511–512. [DOI] [PubMed] [Google Scholar]
- 14. Zutter A, Hauri K, Evers KS, Uhde S, Fassl J, Reuthebuch OT, Berset A, Kuhne M, Donner BC.. “Chaotic arrhythmia” during successful resuscitation after ingestion of yew (Taxus baccata) needles. Pediatr Emerg Care 2017;35:e223–e225. [DOI] [PubMed] [Google Scholar]
- 15.BBC. Ben Hines Died After Ingesting Yew Tree Poison 2014. https://www.bbc.co.uk/news/uk-england-norfolk-26089688 (13 December 2019).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.