Abstract
Background
In patients with hypoplastic left heart syndrome (HLHS) premature closure or restriction of the interatrial communication causes severe cyanosis directly after birth with rapid deterioration in clinical state. An ex-utero intrapartum treatment (EXIT) procedure, extracorporal membrane oxygenation (ECMO), and emergency interventional cardiac catheterization or cardiac surgery has to be anticipated and prepared. We report the first case performing foetal atrial septum stenting in such a patient directly before birth to enable uncomplicated interatrial shunting postnatally.
Case summary
A 31-year-old pregnant woman was referred to our centre for further evaluation of the foetus due to HLHS. In the follow-up study before birth severe restriction of the foramen ovale with increased retrograde flow in the pulmonary veins [0.33 ratio antegrade/retrograde time velocity integral (TVI)] was detected. After careful consideration foetal atrial septum stenting was performed at 38 + 3 weeks of gestation. At 39 + 2 weeks of gestation the baby was born by caesarean section followed by an uncomplicated postnatal adaption. On the 7th day of life a Norwood procedure was performed and the baby was discharged on the 63rd postoperative day.
Discussion
Evaluation of the interatrial communication in foetuses with HLHS should be done carefully just before birth. In the case of severe restriction or closure of the foramen ovale atrial septum stenting just before birth can be considered as an alternative treatment to an EXIT procedure, ECMO, or emergency atrioseptectomy on bypass. However, a very experienced team of paediatric cardiologists and perinatologists with expertise in foetal cardiac interventions is needed to perform this technical difficult procedure.
Keywords: Congenital heart disease, Foetal cardiac intervention, Hypoplastic left heart syndrome, Case report
Learning points
This is the first report describing stenting of the atrial septum in a foetus with hypoplastic left heart syndrome (HLHS) and restrictive foramen ovale just before birth.
This technical challenging procedure should be limited only to patients with HLHS and severe restriction or closure of the foramen ovale.
Introduction
In neonates with hypoplastic left heart syndrome (HLHS) and mitral and/or aortic atresia oxygenated blood from the pulmonary veins can only leave the left atrium through the foramen ovale. Restriction across the interatrial communication can cause severe cyanosis directly after birth in these patients with rapid deterioration in clinical state.1 In expectation of this emergency situation an EXIT procedure, immediate ECMO installation, and/or urgent interventional cardiac catheterization or surgical atrioseptectomy has to be prepared. Ensuring unrestricted atrial shunting before birth might avoid emergency interventions right after birth.2 We report the first case in which foetal atrial septum stenting was performed directly before birth to enable unrestrictive interatrial shunting postnatally.
Timeline
| 38 + 3 weeks of gestation | Stenting of the atrial septum with an 18 G needle and 3 mm stent (9 mm length dilatation up to 3.4 mm at 16 bar). Mean pressure gradient was reduced from 1.12 to 0.34 mmHg and good left to right shunting was established |
| Birth at 39 + 2 weeks | Birth of a baby boy at 39 + 2 weeks of gestation by caesarean section. Uncomplicated postnatal adaptation without the need of urgent procedures. After admission to the PICU prostaglandin E1 administration was started |
| 6 days | Norwood procedure with Sano shunt to the right pulmonary artery and uncomplicated removal of the interatrial stent; secondary closure of the chest on the 4th postoperative day; starting of antiarrhythmic therapy (amiodarone) due to recurrent supraventricular tachycardia |
| 3.5 months | Bidirectional Glenn surgery with preceding diagnostic catheterization and discharge after uncomplicated postoperative course on the 9th postoperative day |
Case presentation
A 31-year-old pregnant woman was referred to our centre for further evaluation of the foetus due to HLHS. On foetal echocardiography at 25 + 6 weeks gestation a small left ventricle with severe endocardial fibroelastosis, aortic atresia, and mitral stenosis could be seen. The pulmonary veins presented enlarged with reduced antegrade flow and significant reverse flow on Doppler sonography (0.47 pulmonary vein TVI ratio; Figure 1). The foramen ovale seemed to be small and restrictive (Figure 2) but of sufficient size for postnatal interatrial shunting. The mother was then given an appointment for caesarean section in our centre at 39 + 0 weeks of gestation. In the foetal echocardiography follow-up study 1 week before admission the flow across the foramen ovale further reduced and there was still a pathological pulmonary vein TVI ratio of 0.33. After careful consideration and informed consent was given by the mother the decision to perform foetal atrial septum stenting was made. The procedure was then performed at 38 + 3 weeks of gestation under ultrasound guidance. All foetal intracardiac procedures are performed with an interdisciplinary team consisting of two paediatric cardiologists with one cardiac catheter laboratory nurse, one perinatologist with experience in intrauterine therapy, and one anaesthesiologist. General anaesthesia was used for the mother without separate analgesia of the foetus. The right atrium was punctured with an 18 G needle. Then the atrial septum was perforated and a 0.014 wire was placed into a left pulmonary vein. A 3 mm × 9 mm coronary artery stent (ProKineticEnergy®, Biotronik) was then placed into the atrial septum (Figure 3) and dilatation was performed up to 16 bars correlating with a 3.4 mm stent diameter. Then the needle was removed without signs of tamponade or other complications. In the follow-up echo the day after the procedure the stent was in place with improved left to right shunting (Figure 4). There was furthermore increased antegrade and decreased retrograde flow in the pulmonary veins measured by TVI in Doppler sonography (0.24 pulmonary vein TVI ratio). The mother was then again admitted for caesarean section at 39 + 2 weeks of gestation. There was completely uncomplicated postnatal adaption with Apgars 9 and 9 at 1 and 5 min and saturations of 86%. The newborn was then admitted to our pediatric intensive care unit (PICU) to start prostaglandin E1 infusions. On postnatal echocardiography, the stent was still in place with a mean velocity of 1.5 m/s measured by PW Doppler (Figure 5). On the 7th day of life the boy then underwent a Norwood procedure. The stent was removed and an atrioseptectomy performed. There was an uncomplicated secondary closure of the chest on the 4th postoperative day. Due to recurrent supraventricular tachycardia an antiarrhythmic therapy with amiodarone was started. There were no signs of severe pulmonary vascular disease during the entire stay in hospital and the patient was ultimately discharged on aspirin on the 63rd postoperative day with adequate saturations and sinus-rhythm. The postoperative course after discharge was uncomplicated without further episodes of supraventricular tachycardias. Bidirectional Glenn surgery was then performed at 3.5 months of age and the boy was discharged on the 9th postoperative day. After 5 months the antiarrhythmic therapy with amiodarone was stopped. The last check-up at our centre was done at the age of 10 months and the boy did not show any symptoms or abnormal findings with saturations of 84%.
Figure 1.
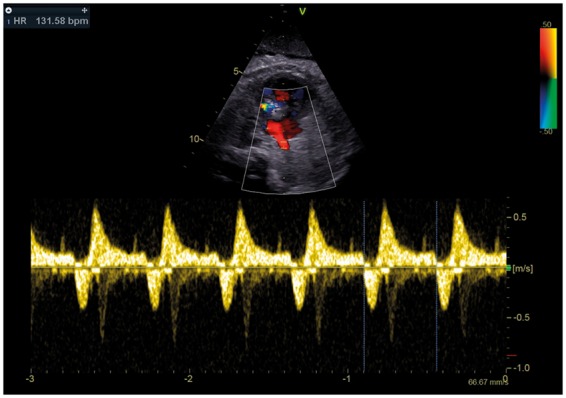
Dilated pulmonary vein with pathological antegrade/retrograde TVI ratio.
Figure 2.
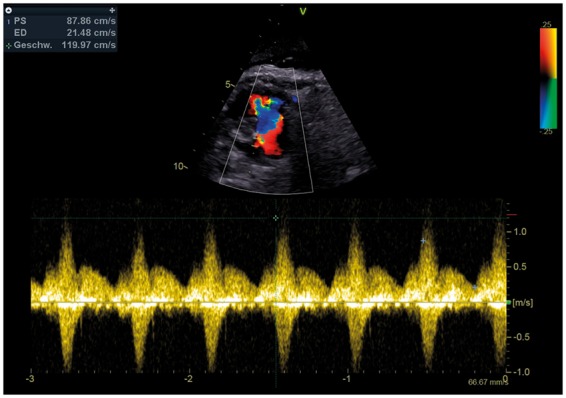
Restrictive flow across the foramen ovale.
Figure 3.
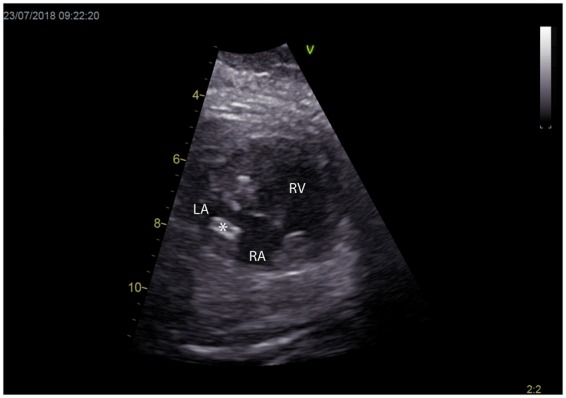
Coronary artery stent placed into the interatrial septum; *, stent, LA, left atrium; RA, right atrium.
Figure 4.
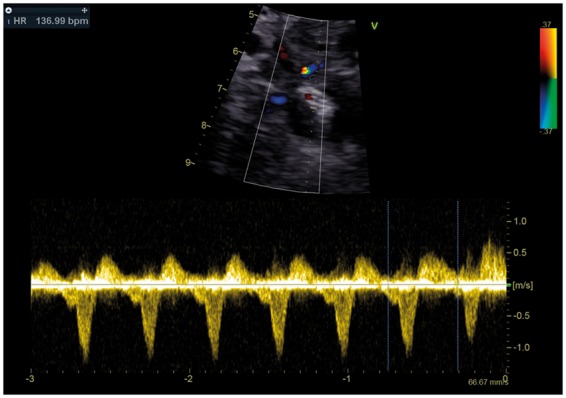
Improved flow across the interatrial septum.
Figure 5.
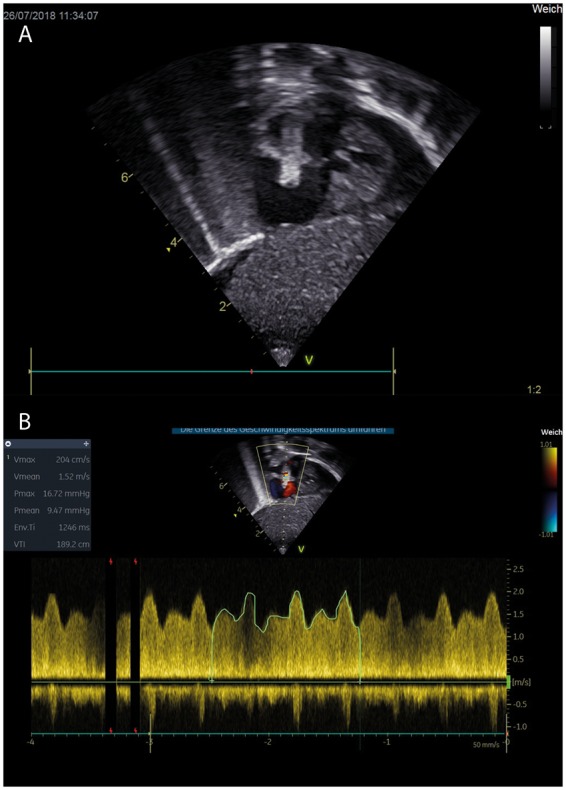
(A) Postnatal subcostal long axis view of the atrial septum stent in place, (B) left to right shunting across the atrial septum stent with a mean velocity of 1.5 m/s.
Discussion
This is the first report of a foetus with HLHS to receive an interatrial septum stent due to a highly restrictive foramen ovale just before birth. Stenting or septostomy of the interatrial septum in foetuses with HLHS in the late second or third trimester was already described earlier by other groups.1,3–5 The rationale during this stage of pregnancy is that restrictive interatrial shunting with increased reverse flow in the pulmonary veins causes alterations to the pulmonary vascular bed with a consequently severely increased morbidity and mortality in these patients.3 Performing foetal atrial septum stenting in late pregnancy will not improve these morphological alterations in the pulmonary vascular bed. However, premature closure or severe restriction of the foramen ovale will lead to rapid deterioration in clinical state with significant morbidity and mortality.1,2 Immediate ECMO installation, EXIT procedure, and/or urgent interventional catheterization or surgical atrioseptectomy have to be prepared in this situation. By stenting the interatrial septum just before birth unrestricted atrial shunting can be established and therefore emergency interventions might be avoided right after birth. In our case we had to balance the risks of prenatal stent placement vs. the risks of very invasive postnatal procedures. Having performed more than 140 intracardiac foetal interventions at that time, our team felt confident enough to perform this procedure with an acceptable risk.
Even though this can be considered as an alternative treatment, a very experienced team of paediatric cardiologists and perinatologists with expertise in foetal cardiac interventions is needed to perform this technical difficult procedure.
Conclusion
Evaluation of the interatrial communication in foetuses with HLHS should be done carefully just before birth. In cases with premature closure or restriction of the foramen ovale prenatal interatrial septum stenting can be considered as an alternative to postnatal emergency procedures to reduce the risk of additional morbidity in these patients.
Lead author biography
Andreas Tulzer is a fellow in paediatric cardiology at Children’s Heart Center in Linz, which is part of the Kepler University Hospital in Linz, Austria. He is part of the foetal cardiac interventions team for several years and also a PhD candidate. Furthermore, he is a member of the Fetal Cardiology working group of the AEPC.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Marshall AC, van der Velde ME, Tworetzky W, Gomez CA, Wilkins-Haug L, Benson CB, Jennings RW, Lock JE.. Creation of an atrial septal defect in utero for fetuses with hypoplastic left heart syndrome and intact or highly restrictive atrial septum. Circulation 2004;110:253–258. [DOI] [PubMed] [Google Scholar]
- 2. Jantzen DW, Moon-Grady AJ, Morris SA, Armstrong AK, Berg C, Dangel J, Fifer CG, Frommelt M, Gembruch U, Herberg U, Jaeggi E, Kontopoulos EV, Marshall AC, Miller O, Oberhoffer R, Oepkes D, Pedra CA, Pedra SR, Peralta F, Quintero RA, Ryan G, Gelehrter SK.. Hypoplastic left heart syndrome with intact or restrictive atrial septum: a report from the International Fetal Cardiac Intervention Registry. Circulation 2017;136:1346–1349. [DOI] [PubMed] [Google Scholar]
- 3. Chaturvedi RR, Ryan G, Seed M, van Arsdell G, Jaeggi ET.. Fetal stenting of the atrial septum: technique and initial results in cardiac lesions with left atrial hypertension. Int J Cardiol 2013;168:2029–2036. [DOI] [PubMed] [Google Scholar]
- 4. Kalish BT, Tworetzky W, Benson CB, Wilkins-Haug L, Mizrahi-Arnaud A, McElhinney DB, Lock JE, Marshall AC.. Technical challenges of atrial septal stent placement in fetuses with hypoplastic left heart syndrome and intact atrial septum. Catheter Cardiovasc Interv 2014;84:77–85. [DOI] [PubMed] [Google Scholar]
- 5. Marshall AC, Levine J, Morash D, Silva V, Lock JE, Benson CB, Wilkins-Haug LE, McElhinney DB, Tworetzky W.. Results of in utero atrial septoplasty in fetuses with hypoplastic left heart syndrome. Prenat Diagn 2008;28:1023–1028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


