Abstract
Background
Spontaneous coronary artery dissection (SCAD) is an uncommon cause of acute coronary syndrome in younger females with no pre-existing history of coronary artery disease. Recurrent SCAD is common after a first episode and can involve the same coronary artery or present as a new dissection unrelated to the initial lesion. Current recommendations advise for a conservative approach in the absence of haemodynamic compromise and flow limitations. Conversely, there are no clear guidelines for the management of early recurrent SCAD.
Case summary
A 52-year-old woman with history of obesity, asthma, and prediabetes presented with chest pain and electrocardiogram (ECG) showing inferior wall ST-elevation myocardial infarction (STEMI). Coronary angiography revealed proximal right coronary artery (RCA) dissection and distal left anterior descending artery (LAD) dissection, while left ventriculogram showed Takotsubo cardiomyopathy (TC). Angiography revealed no flow limitations so conservative management was pursued. She returned within a couple of days with recurrent chest pain and ECG showing similar findings of inferior STEMI. Repeat angiography confirmed progression of the proximal RCA SCAD with resolution of distal LAD SCAD. Since flow through the distal RCA was still preserved, conservative medical management was continued. She presented a third time for palpitations only and another repeat coronary angiogram showed healing RCA SCAD.
Discussion
Management of early recurrent SCAD continues to be a clinical dilemma. In addition, our patient had features of TC which shares a similar clinical risk factor profile with SCAD thus it may be prudent to further investigate for TC in patients presenting with SCAD and have suggestive features of TC on history and echocardiography.
Keywords: Spontaneous coronary artery dissection, Acute coronary syndrome, Takotsubo cardiomyopathy, Recurrence, Case report
Learning points
Spontaneous coronary artery dissection (SCAD) is an uncommon presentation of acute coronary syndrome in younger females and is usually managed conservatively.
Management of early recurrent SCAD is challenging since there are no clear guidelines.
Spontaneous coronary artery dissection and Takotsubo cardiomyopathy (TC) share a similar risk profile and it may be prudent to consider screening all newly diagnosed SCAD patients for TC with suggestive clinical and echocardiographic features.
Introduction
Spontaneous coronary artery dissection (SCAD) is an uncommon clinical entity seen typically in younger females with no known history of underlying coronary artery disease.1 It is defined as non-iatrogenic epicardial coronary artery dissection not associated with atherosclerosis or trauma. Myocardial injury in SCAD results from coronary artery obstruction secondary to intimal disruption or intramural haematoma formation. The aetiology is hypothesized to be multifactorial from a combination of underlying and acquired arteriopathies, genetic factors, hormonal effects, and systemic inflammatory diseases in combination with underlying stressors and environmental precipitants.2 The presentation can be variable with associated acute coronary syndrome (ACS), ventricular arrhythmias, or sudden cardiac death with high mortality in the acute stages.3 Recurrent SCAD is relatively common and described as either an extension of the primary dissection in the acute phase or a new dissection unrelated to the primary lesion. Incidence of recurrent SCAD has been reported up to 30% at 4–10 years of follow-up.1,2,4
Takotsubo syndrome or cardiomyopathy (TC) can present with chest pain or dyspnoea along with ST elevation and rise in cardiac biomarkers mimicking ACS.5 Spontaneous coronary artery dissection and TC are two distinct and mostly unrelated non-atherosclerotic causes of myocardial infarction. One of the proposed mechanisms for SCAD common to TC are hormonal effects and sympathetic stimulation associated with a stressful event.6 There are case reports and case series where coexistence of SCAD and TC were reported.7,8
We present a unique case of SCAD with features of TC who later developed recurrent SCAD. At present, there is expert consensus but no guidelines for the management of SCAD.9 The management of recurrent SCAD is controversial and posed a bigger dilemma for our patient with recent TC.
Timeline
| 3 days before hospitalization | Motder passes away. |
| Initial presentation | Chest pain during her mother’s funeral. Electrocardiogram showing inferior ST elevation and increased cardiac biomarkers. Angiogram shows spontaneous coronary artery dissection (SCAD) of the right coronary artery (RCA) and distal left anterior descending artery (LAD). Left ventriculogram showed Takotsubo cardiomyopathy. Thrombolysis in myocardial infarction 3 flow in vessels so managed conservatively. |
| Day 3 | Patient discharged home on medical therapy. |
| Day 5 | Recurrence of chest pain with elevated biomarkers and repeat ST elevation in inferior leads. Repeat angiogram showing progression of RCA and resolution of distal LAD SCAD. Thrombolysis in myocardial infarction 3 flow still present. |
| Day 7 | Patient discharged home on medical therapy. |
| Day 14 | Palpitations as an outpatient. Holter monitoring reveals occasional ectopic ventricular beats. |
| Day 15 | Patient hospitalized for ongoing palpitations. Repeat angiogram shows a well healing RCA SCAD. |
Case presentation
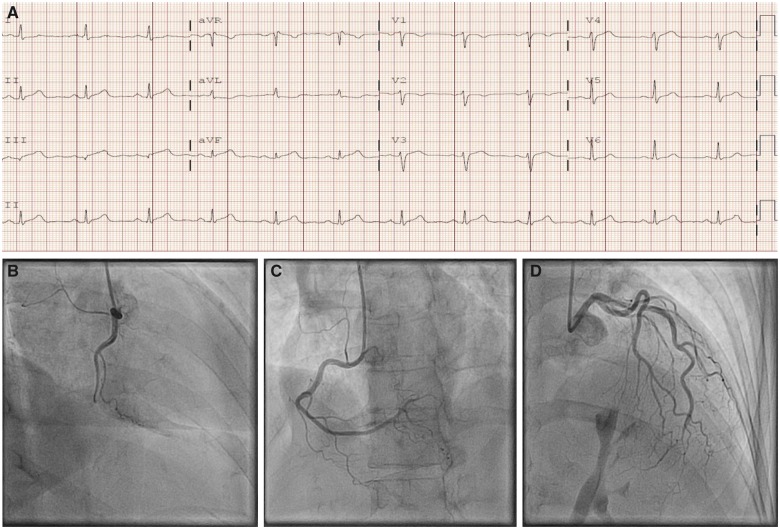
A 52-year-old woman, gravida 2, para 2, with history of obesity, asthma, and prediabetes presented to the emergency department with complaints of chest pain. Her mother passed away 3 days prior to her presentation. During the funeral, she reported left-sided chest pain which spontaneously resolved but reappeared later in the evening. It was described as substernal chest tightness, 6/10, non-radiating with no aggravating or relieving factors. Her vital signs included blood pressure 151/83, heart rate 73, respiratory rate 18/min, and she had normal physical examination. An electrocardiogram (ECG) on presentation showed ST-segment elevation in inferior leads with reciprocal changes in lateral leads (Figure 1A). Troponin T and CPK were elevated and peaked to 3.90 ng/mL (<0.03 ng/mL) and 1938 U/L (24–173 U/L), respectively during hospitalization. Emergency coronary angiography (CA) revealed Type 1 SCAD of the proximal right coronary artery (RCA) and long segment narrowing consistent with Type 2b distal left anterior descending artery (LAD) SCAD (Figure 1B–D). Given the presence of thrombolysis in myocardial infarction (TIMI) 3 flow through the RCA, conservative medical management was pursued. Left ventriculogram (LVgram) (Figure 2) revealed evidence of TC with apical akinesis, anterolateral hypokinesis, and inferobasal hyperkinesis, and a transthoracic echocardiogram (TTE) confirmed the same. Transthoracic echocardiogram showed ejection fraction 50–55% and no mitral regurgitation or left ventricular outflow tract obstruction. Repeat ECG’s the following day showed resolution of ST elevation. She remained chest pain free and was discharged on maximal medical therapy with dual antiplatelet agents, beta-blocker (BB), and high-dose statin.
Figure 1.
(A) Initial electrocardiogram on presentation to the emergency department. (B) Spontaneous right coronary artery dissection in left anterior oblique view. (C) Spontaneous right coronary artery dissection in right anterior oblique view. (D) Distal left anterior descending coronary dissection on left anterior oblique view.
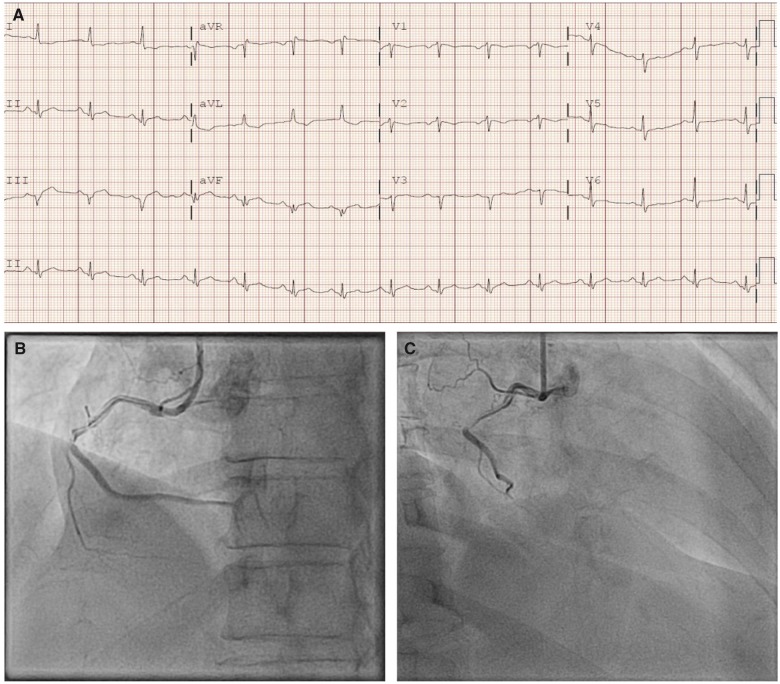
Figure 2.
Takotsubo’s cardiomyopathy on left ventriculography in (A) diastole and (B) systole during first coronary angiogram.
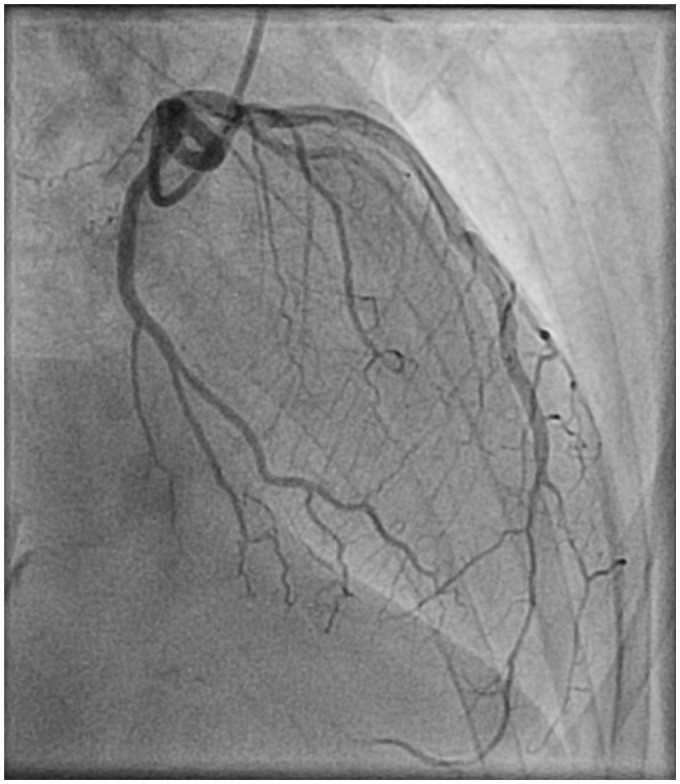
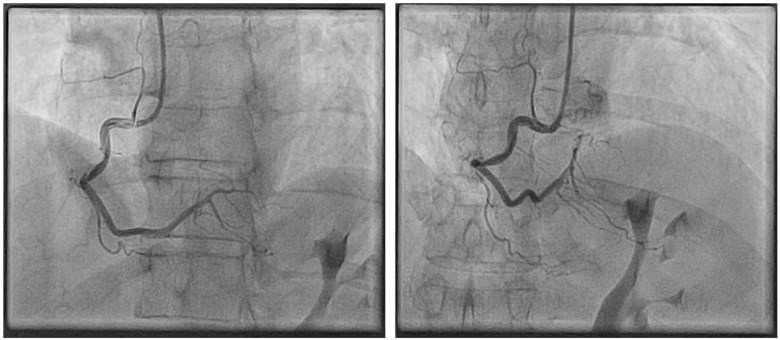
The patient returned to the hospital 2 days post-discharge with a similar presentation of persistent chest pain with ST elevation in inferior leads (Figure 3A) and elevated troponin of 0.958. Repeat CA revealed progression of proximal RCA dissection (Type 1 Saw, Figure 3B and C), while the distal LAD dissection showed near complete resolution (Type 2b, Figure 4). Since TIMI 3 flow was still present in the distal RCA it was decided to continue medical management. Repeat TTE suggested improvement in inferobasal and resolution of apical hypokinesis. Given her ongoing medical stability, she was discharged home. After 1 week, she complained of palpitations and a 24-h Holter monitor was ordered in the outpatient setting, revealing occasional ectopic ventricular beats but there was no ventricular arrhythmia. Since her palpitations worsened, she was readmitted to the hospital. She underwent another CA which showed evidence of a well healing RCA SCAD (Type 1 Saw, Figure 5). Patient continues to be asymptomatic during her last 1 month of follow-up.
Figure 3.
(A) Repeat electrocardiogram on her second presentation to emergency department. (B) Progression of right coronary dissection on second coronary angiography in left anterior oblique view. (C) Progression of right coronary dissection on second coronary angiography in right anterior oblique view.
Figure 4.
Healed distal left anterior descending dissection on second coronary angiogram in left anterior oblique view.
Figure 5.
Healing dissection of right coronary artery on third angiogram in two views.
Discussion
Spontaneous coronary artery dissection is an uncommon presentation for ACS seen mostly in younger women. There are a few reported cases in medical literature of SCAD presenting with TC. We present a unique case of recurrent SCAD associated with prior TC, posing a significant management dilemma.
Based on angiographic characteristics, the Saw classification for SCAD has now been commonly adapted (Table 1).10 Conservative medical management is the mainstay of therapy in treating stable patients with SCAD.3 A review of the existing literature suggests that healing of SCAD is time dependent.10 For our patient, the mild Type 2b distal LAD dissection had near complete resolution with conservative management but the Type I proximal RCA lesion progressed with extension of the dissection. Intracoronary imaging including intrasvascular ultrasound or optical coherence tomography was not performed to avoid further propagation of the dissection. However, blood flow was preserved, prompting us to continue medical management. A third CA on her final hospitalization confirmed the RCA SCAD was healing well. The timeline for resolution of the RCA SCAD was as expected adding credence to our decision to pursue conservative management in the absence of flow limitations.
Table 1.
Saw classification of spontaneous coronary artery dissection
| Type | Angiographic characteristics |
|---|---|
| Type 1 | Multiple lumen and contrast staining of the arterial wall |
| Type 2a | Stenosis of artery with abrupt change in vessel caliber, typically >20 mm not involving angiographic tip of vessel |
| Type 2b | Stenosis of artery with abrupt change in vessel caliber, extending to angiographic tip of vessel |
| Type 3 | Mimics atherosclerosis |
A recent single-centre study by Saw et al.11 noted that BB use was associated with lower risk of recurrent SCAD. Unfortunately, our patient developed recurrent SCAD despite being on BB therapy. She didn’t have any family history of SCAD, neither was she on oral contraception or hormone replacement therapy. In addition, the use of implantable bioresorbable vascular scaffold (BVS) has been reported in SCAD but is no longer available.12 A dual approach has been proposed for the management of SCAD involving BVS implantation with conservative management based on vessel diameter and haemodynamic features.12 Some authors have suggested percutaneous coronary intervention (PCI) as a first-line treatment in the presence of ongoing ischaemia and haemodynamic instability.12 Nonetheless, PCI was found to be associated with high rates of complications including propagation of the dissection flap, intramural haematoma formation, and technical challenges limiting placement of the wire into the true lumen.1 There have been instances where coronary artery bypass surgery was done for the treatment of SCAD.13,14 In lieu of the challenges involved, Buccheri et al.15 proposed a scoring system to diagnose and treat SCAD.
Conclusion
Management of recurrent SCAD continues to be a challenging given the absence of specific guidelines or even expert consensus. Although conservative management is the standard of care for a first presentation, management of early recurrent SCAD is not clearly defined. This is likely in part due to the limited clinical experience. Further case series or registries to evaluate outcomes in early recurrent SCAD are necessary to formulate guidelines for management.
In addition to SCAD, our patient had features suggestive of TC based on the LVgram and echocardiographic findings though subsequent imaging showed resolution of TC. Furthermore, SCAD and TC share a similar risk profile presenting in healthy young females with concomitant significant stressors. Thereby, in conclusion, it may be prudent to consider screening all newly diagnosed SCAD patients for TC with suggestive clinical and echocardiographic features.
Lead author biography

Hafiz U. Ghafoor currently a second year fellow in the cardiovascular disease fellowship programme at St. Vincent Hospital in Worcester, MA, USA. I consider myself fortunate as I found my specialty of choice early in my medical career. I have always tried to ensure that I keep myself productive in research along with the vigorous clinical training and have published both basic science and clinical research articles. My goal is to become an interventional cardiologist and apply the knowledge and training I have acquired to become an outstanding physician.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Tweet MS, Hayes SN, Pitta SR, Simari RD, Lerman A, Lennon RJ, Gersh BJ, Khambatta S, Best PJ, Rihal CS, Gulati R.. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012;126:579–588. [DOI] [PubMed] [Google Scholar]
- 2. Saw J, Aymong E, Sedlak T, Buller CE, Starovoytov A, Ricci D, Robinson S, Vuurmans T, Gao M, Humphries K, Mancini GB.. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014;7:645–655. [DOI] [PubMed] [Google Scholar]
- 3. Vrints CJ. Spontaneous coronary artery dissection. Heart 2010;96:801–808. [DOI] [PubMed] [Google Scholar]
- 4. Tweet MS, Eleid MF, Best PJ, Lennon RJ, Lerman A, Rihal CS, Holmes DR Jr, Hayes SN, Gulati R.. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv 2014;7:777–786. [DOI] [PubMed] [Google Scholar]
- 5. Prasad A, Lerman A, Rihal CS.. Apical ballooning syndrome (tako-tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008;155:408–417. [DOI] [PubMed] [Google Scholar]
- 6. Buccheri D, Zambelli G.. The link between spontaneous coronary artery dissection and takotsubo cardiomyopathy: analysis of the published cases. J Thorac Dis 2017;9:5489–5492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chou AY, Sedlak T, Aymong E, Sheth T, Starovoytov A, Humphries KH, Mancini GB, Saw J.. Spontaneous coronary artery dissection misdiagnosed as takotsubo cardiomyopathy: a case series. Can J Carrdiol 2015;31:1073.e5–8. [DOI] [PubMed] [Google Scholar]
- 8. Y-Hassan S. Spontaneous coronary artery dissection and takotsubo syndrome: an often overlooked association; review. Cardiovasc Revasc Med 2018;19:717–723. [DOI] [PubMed] [Google Scholar]
- 9. Hayes SN, Kim ESH, Saw J, Adlam D, Arslanian-Engoren C, Economy KE, Ganesh SK, Gulati R, Lindsay ME, Mieres JH, Naderi S, Shah S, Thaler DE, Tweet MS, Wood MJ.. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American Heart Association. Circulation 2018;137:e523–e557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saw J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter Cardiovasc Interv 2014;84:1115–1122. [DOI] [PubMed] [Google Scholar]
- 11. Saw J, Humphries K, Aymong E, Sedlak T, Prakash R, Starovoytov A, Mancini G.. Spontaneous coronary artery dissection: clinical outcomes and risk of recurrence. J Am Coll Cardiol 2017;70:1148–1158. [DOI] [PubMed] [Google Scholar]
- 12. Ruggiero A, Cuculo A, Centola A, Campanale G, Russo D, Gaglione A, Di Biase M, Brunetti ND, Alfonso F, Garcia-Guimaraes M, Cuesta J, Navarrete G, Bastante T, Saw J.. How should I treat an extended spontaneous coronary artery dissection in a young woman without cardiovascular risk factors mimicking takotsubo cardiomyopathy? EuroIntervention 2016;12:e1073–e1076. [DOI] [PubMed] [Google Scholar]
- 13. Patel KP, Sotolongo RP, Myrick TW.. Off-pump coronary artery bypass grafting for spontaneous coronary dissection in a 26-year-old patient two weeks post-partum: a case report and review. J Extra Corpor Technol 2008;40:127–129. [PMC free article] [PubMed] [Google Scholar]
- 14. Cetin E, Ozyuksel A.. Beating heart myocardial revascularisation of a sudden cardiac death survivor with spontaneous coronary artery dissection: Pitfalls from diagnosis to surgery. BMJ Case Rep 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Buccheri D, Piraino D, Andolina G.. Score system approach to diagnose and manage spontaneous coronary artery dissection. Rev Esp Cardiol (Engl Ed) 2016;69:878–879. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.