Abstract
Vascular bypass graft infection with Mycobacterium bovis following Bacillus Calmette–Guérin (BCG) immunotherapy for bladder cancer is an incredibly rare complication. We present the case of an 85-year-old man with a history of femorofemoral bypass who developed this complication over a year after BCG treatment. He was successfully treated with explantation of the polytetrafluoroethylene (PTFE) graft, redo bypass with vein graft, and antituberculous medical therapy.
Keywords: Mycobacterium bovis, Bladder cancer, Bacillus Calmette–Guérin, Pembrolizumab, Prosthetic bypass graft infection
1. Introduction
Bladder cancer is the ninth most commonly diagnosed malignancy in the world [1]. In the United States, it is the sixth most common, with approximately 80,470 new cases diagnosed in 2019 [2]. The authors’ state comprised 2580 of those cases. Bladder cancer is more common in men than in women, and major risk factors include smoking and occupational exposure to aromatic amines and polycyclic aromatic hydrocarbons [3].
BCG immunotherapy is a commonly used treatment for early stage bladder cancer. Intracavitary BCG instillation for superficial bladder tumors was first described in 1976 in a small series of nine patients [4]. To this day, BCG remains part of both the American and European guidelines for adjuvant therapy in superficial bladder cancer [5]. The treatment entails intravesical instillation of this live attenuated strain of Mycobacterium bovis.
In rare instances, patients have developed BCG infections after their therapy. The majority of BCG infections are either disseminated (34.4%) or local genitourinary (23.4%) in nature, with osteomuscular infections contributing another 19.9% and vascular 6.7% [6]. Within the vascular infection group, the most commonly seen manifestation is the mycotic aortic aneurysm, first described in 1988 [7]. Less commonly, there have been cases complicated by aortoenteric fistula development [8,9]. As well, BCG infection of aortic aneurysm endografts has been described [10]. Similarly, there have been rare instances of vascular bypass graft BCG infection, first described in 1999 [11]. We present an extremely uncommon case of vascular graft infection with Mycobacterium bovis following treatment with BCG. The patient provided consent for the publication of his case detail and images.
2. Case report
An 85-year-old man with a history of femorofemoral bypass performed seven years ago for right lower extremity rest pain presented to the emergency room with a right groin wound. His medical history includes bladder cancer diagnosed one year prior to presentation. His initial cancer treatment included intravesical BCG immunotherapy. His current treatment is with an immune checkpoint inhibitor, pembrolizumab, a monoclonal antibody against the programmed cell death protein 1 (PD-1) receptor found on T-cells, known to be exploited by certain cancer cells that express the ligand PD-L1, allowing them to avoid immune-mediated destruction [12]. This therapy was started eight months ago. He is otherwise a former smoker with chronic obstructive pulmonary disease (COPD), coronary artery disease, hypertension, and spinal stenosis. A left groin wound with purulent drainage was first noted by the patient's oncologist four months prior to presenting to the emergency room. This was managed with a 10-day course of doxycycline, 100 mg orally twice daily, while holding the pembrolizumab. Following the course of antibiotics, the wound was found by his oncologist to no longer have purulent drainage, so the immunotherapy was resumed. Two months later, a contralateral groin wound developed, which was treated with another 10-day course of doxycycline. This wound continued to have purulent drainage after two weeks of outpatient management, so he was advised to present to the emergency room for further workup and management.
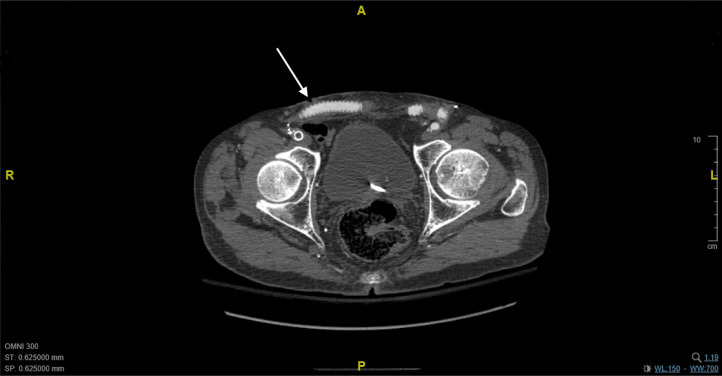
In the emergency room, the patient was evaluated by the vascular surgery service, and was found to be afebrile with a punctate purulent wound, without any significant associated erythema, induration, or fluctuance. Imaging workup included a computed tomography angiogram (CTA), which showed a soft tissue irregularity just superficial to the patent femorofemoral bypass graft in the right groin (Fig. 1). An infectious disease consultation was obtained, and the patient was started on piperacillin-tazobactam, 4.5 mg IV every 8 h, and vancomycin, 15 mg/kg IV every 12 h.
Fig. 1.
Computed tomography scan of the pelvis. The arrow marks the site of an open groin wound over the bypass graft.
The decision was made to proceed with explantation of the infected PTFE graft, redo femorofemoral bypass with autogenous vein graft, and bilateral sartorius muscle flap reconstruction. Based on the patient's vein mapping results, the left superficial femoral vein was selected for use as the conduit for the left common femoral artery to right profunda femoral artery bypass. The PTFE graft was well-incorporated and there were no gross signs of infection surrounding the graft, however it was sent off for cultures regardless. The explant incisions were packed, and a separate tunnel was made for the new vein bypass. The patient tolerated the procedure well.
Post-operatively, the patient was maintained on both vancomycin and piperacillin-tazobactam. The aerobic and anaerobic cultures from the PTFE graft showed no bacterial growth. On postoperative day seven, after having completed 11 days of vancomycin and piperacillin-tazobactam, the patient was discharged to rehab on a four-week course of vancomycin, 1 g IV daily, and ceftriaxone, 2 g IV daily, as prescribed by our infectious disease colleagues.
In the weeks following discharge, he completed his course of vancomycin and ceftriaxone. His immunotherapy was then restarted. At two months post-op, the acid-fast bacilli (AFB) cultures from the PTFE graft resulted, demonstrating Mycobacterium tuberculosis complex. The culture sensitivities demonstrated resistance to pyrazinamide, indicative of Mycobacterium bovis, one of the organisms within this complex. The Mycobacterium bovis was susceptible to ethambutol, isoniazid, and rifampin. Given his prior history of BCG treatment and relative immunocompromised status, it was felt that this was a case of disseminated BCG. He is being treated now with a planned course of at least 6 months of isoniazid, 300 mg orally daily, and rifampin, 600 mg orally daily, and he is otherwise recovering well at three months post-op.
3. Discussion
Staphylococcus species, namely Staphylococcus epidermidis and Staphylococcus aureus, are the most commonly isolated bacteria in prosthetic graft infections, including those involving the femoral artery [13]. Mycobacterium species are very uncommon isolates in cases of vascular graft infection. One of the limited situations where Mycobacterium infection can be seen is following BCG treatment for bladder cancer, which involves instillation of live attenuated Mycobacterium bovis into the bladder. The most common of the vascular complications seen in local or disseminated BCG infection is a mycotic aneurysm or pseudoaneurysm, with aortoenteric fistulas and vascular bypass graft infections being more unusual [6].
BCG immunotherapy has been commonly used for bladder cancer treatment for over forty years, however, there have only been three prior cases of Mycobacterium bovis vascular bypass graft infections following BCG therapy reported in the literature [11,14,15]. The first reported case, like the case presented here, involved a femoral crossover PFTE graft [11]. That patient was successfully treated with resection of the graft, placement of an interposition vein graft, and antibiotic therapy with isoniazid, ethambutol, and rifampin. The second and third cases both involved axillo-femoral bypass grafts, and the treatment similarly consisted of graft explantation with nine months antituberculous therapy with isoniazid, ethambutol, and rifampin [14,15]. There was also a recently reported similar case of a BCG prosthetic joint infection, which was approached with removal of the incision and drainage, removal of the prosthetic device, placement of a temporary antibiotic-laden spacer, and treatment with 12 months of rifampin, isoniazid, and ethambutol [16]. That orthopedic case followed the same general concepts as in the present case and the above mentioned cases, with removal of the prosthetic material, reconstruction as needed with a material more resistant to infection (temporary in their case), and antituberculous medical therapy.
The present case differs from the previously reported cases of Mycobacterium vascular bypass graft infection following BCG therapy, because our patient also had received treatment with pembrolizumab, an immune checkpoint inhibitor. Of note, reactivation of pulmonary tuberculosis has recently been reported in patients treated with this medication and with similar immunotherapy agents [17]. It is possible that a similar reactivation phenomenon occurred in our patient.
4. Conclusions
In patients with a history of bladder cancer treated with BCG who present with an infection, including those involving vascular bypass grafts, the possibility of Mycobacterium bovis infection needs to be considered, especially if they were also treated with pembrolizumab. For these infections, treatment with graft explantation, bypass revision as necessary with autogenous vein graft, and antituberculous medical therapy appears to be effective.
Declaration of Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Antoni S., Ferlay J., Soerjomataram I., Znaor A., Jemal A. Bladder cancer incidence and mortality: a global review and recent trends. Eur Urol. 2017;71:96–108. doi: 10.1016/j.eururo.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–13. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 3.Burger M., Catto J.W.F., Dalbagni G., Grossman H.B., Herr H. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013;63:234–241. doi: 10.1016/j.eururo.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 4.Morales A., Eidinger D., Bruce A.W. Intracavitary bacillus Calmette–Guerin in the treatment of superficial bladder tumors. J Urol. 1976;116(2):180–183. doi: 10.1016/s0022-5347(17)58737-6. [DOI] [PubMed] [Google Scholar]
- 5.Larsen E.S., Joensen U.N., Poulsen A.M., Goletti D., Johansen I.S. Bacillus Calmette–Guerin immunotherapy for bladder cancer: a review of immunological aspects, clinical effects and BCG infections. APMIS. 2020 doi: 10.1111/apm.13011. [DOI] [PubMed] [Google Scholar]; https://onlinelibrary.wiley.com/doi/abs/10.1111/apm.13011.
- 6.Asín M.A.P.-J., Fernández-Ruiz M., López-Medrano F., Lumbreras C., Á T., San Juan R. Bacillus Calmette–Guerin (BCG) infection following intravesical bcg administration as adjunctive therapy for bladder cancer: incidence, risk factors, and outcome in a single-institution series and review of the literature. Medicine (Baltimore) 2014;93(17):236–254. doi: 10.1097/MD.0000000000000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woods J.M., Schellack J., Stewart M.T., Murray D.R., Schwartzman S.W. Mycotic abdominal aortic aneurysm induced by immunotherapy with bacilli Calmette–Guerin vaccine for malignancy. J Vasc Surg. 1988;7:808–810. doi: 10.1067/mva.1988.avs0070808. [DOI] [PubMed] [Google Scholar]
- 8.Farber A., Grigoryants V., Palac D.M., Chapman T., Cronenwett J.L. Primary aortoduodenal fistula in a patient with a history of intravesical therapy for bladder cancer with bacillus Calmette–Guerin: review of primary aortoduodenal fistula without abdominal aortic aneurysm. J Vasc Surg. Apr 2001;33(4):868–873. doi: 10.1067/mva.2001.112327. [DOI] [PubMed] [Google Scholar]
- 9.Roylance A., Mosley J., Jameel M., Sylvan A., Walker V. Aorto-enteric fistula development secondary to mycotic abdominal aortic aneurysm following intravesical bacillus Calmette–Guerin (BCG) treatment for transitional cell carcinoma of the bladder. Int J Surg Case Rep. 2013;4(1):88–90. doi: 10.1016/j.ijscr.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mizoguchi H., Iida O., Dohi T., Tomoda K., Kimura H. Abdominal aortic aneurysmal and endovascular device infection with iliopsoas abscess caused by mycobacterium bovis as a complication of intravesical bacillus Calmette–Guerin therapy. Ann Vasc Surg. Nov 2013;27(8):1186.e1–1186.e5. doi: 10.1016/j.avsg.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Seelig M.H., Oldenburg W.A., Klingler P.J. Mycotic vascular infections of large arteries with mycobacterium bovis after intravesical bacillus Calmette–Guerin therapy: case report. J Vasc Surg. 1999;29:377–381. doi: 10.1016/s0741-5214(99)70391-5. [DOI] [PubMed] [Google Scholar]
- 12.Christ M., Iyer G., Hsu M., Huang W.C., Balar A.V. Pembrolizumab in the treatment of locally advanced or metastatic urothelial carcinoma: clinical trial evidence and experience. Ther Adv Uro. 2019;11:1–9. doi: 10.1177/1756287219839285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siracuse J.J., Nandivada P., Giles K.A., Hamdan A.D., Wyers M.C., Chaikof E.L. Prosthetic graft infections involving the femoral artery. J Vasc Surg. March 2013;57(3):700–705. doi: 10.1016/j.jvs.2012.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shakir F., Dang V., Bronze M.S., Liu C., Machado L. Mycobacterium bovis infection of an axillary-femoral bypass graft after intravesical bacille Calmette-Guérin immunotherapy for bladder cancer. Am J Med Sci. January 2009;337(1):63–64. doi: 10.1097/01.MAJ.0000308884.50320.8a. [DOI] [PubMed] [Google Scholar]
- 15.DeSimone D.C., Tande A.J. Infection of an axillo-bifemoral bypass graft following intravesical bacillus Calmette–-Guerin (BCG) immunotherapy for urothelial cancer due to Mycobacterium bovis and Staphylococcus aureus. J Clin Tuberc Other Mycobact Dis. December 2016;5:1–3. doi: 10.1016/j.jctube.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen M.H., Giordani M.M., Thompson G.R. The double-edged sword – prosthetic joint infection following BCG treatment for bladder cancer: a case report. BMC Infect Dis. Apr 2019;19(1):331. doi: 10.1186/s12879-019-3951-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Eeden R., Rapoport B.L., Smit T., Anderson R. Tuberculosis infection in a patient treated with nivolumab for non-small cell lung cancer: case report and literature review. Front Oncol. July 2019;24(9):659. doi: 10.3389/fonc.2019.00659. [DOI] [PMC free article] [PubMed] [Google Scholar]