Abstract
Loneliness poses a significant risk for morbidity and mortality in the context of older adulthood. Research shows that older persons living with HIV (PLWH) often face increased and complex vulnerability in terms of physical and psychosocial needs which may promote loneliness. The current study sought to identify correlates of loneliness in a sample of 146 older PLWH (age ≥50) recruited from an outpatient HIV clinic in Atlanta, GA. Participants completed a survey on loneliness, depression, HIV-related stigma, social network size, HIV-disclosure status, disease burden, and demographics. HIV biomarkers were abstracted from electronic medical records. Participants were predominantly male (60%) and African American (86%). Twelve percent (n=17) reported past homelessness/unstable housing. Multivariable modeling revealed that depression and HIV-related stigma explained 41% of the variance in loneliness, above and beyond the effects of past homelessness/unstable housing and disease burden (R2=0.41, F(7, 138)=13.76, p<.001). Findings suggest that targeting HIV-related stigma and depression may reduce loneliness in older PLWH, but more studies are needed to elucidate causal pathways. A greater understanding of the mechanisms by which loneliness affects health among older PLWH could help better inform efforts to improve health in this patient population.
Keywords: loneliness, HIV, depression, stigma, aging
Introduction
Loneliness is an aversive emotional experience that arises from a perceived deficiency in quantity or quality of social relationships (Peplau & Perlman, 1982). A 2010 national survey by the AARP Foundation found that about one-third of adults age 45 and older were lonely (Wilson & Moulton, 2010). These estimates are concerning because loneliness poses a significant risk for morbidity and mortality and is linked to poor outcomes (Cornwell & Waite, 2009; Rico-Uribe et al., 2018). The clinical and research implications of loneliness for older persons living with HIV (PLWH; age 50 and older) are becoming more relevant in the United States with the rise in the number of older PLWH. According to Centers for Disease Control and Prevention, an estimated 47% of PLWH in 2015 were 50 years old or older (CDC, 2016) and this number is projected to grow to 70% by 2020 (Brooks, Buchacz, Gebo, & Mermin, 2012).
Older PLWH often face increased and complex vulnerability in terms of physical and psychosocial needs; this may exacerbate loneliness. PLWH exhibit higher numbers of age-associated comorbidities at a much younger age than their uninfected counterparts (Pathai, Bajillan, Landay, & High, 2014; Guaraldi et al., 2011), indicating that older PLWH may experience a greater burden of diseases. Health disparities in older PLWH are also reflected in depression, with older PLWH frequently reporting depression whereas uninfected older adults are less likely to report depression (Greene et al., 2015; Havlik, Brennan, & Karpiak, 2011). Older PLWH tend to live alone and have limited and inadequate social networks compared to their younger counterparts (Schrimshaw & Siegel, 2003; Shippy & Karpiak, 2005) because of barriers to receiving support from family and friends. Long-term survivors among older PLWH may be particularly susceptible to isolation and loneliness related to peer network shrinkage due to HIV. On the other hand, newly infected older adults may experience fear of rejection from their loved ones due to perceived stigma. Stigma can lead to feelings of shame and “silencing” or non-disclosure of HIV status (Enriquez, Lackey, & Witt, 2008), which may increase feelings of loneliness. Social marginalization linked to HIV-related stigma and disclosure status is a common barrier to building social relationships (Ware, Wyatt, & Tugenberg, 2006). These health and psychosocial concerns may further heighten the feelings of loneliness in this subpopulation of older adults.
To our knowledge, only two studies have investigated the effects of loneliness on the health of older PLWH, and these studies suggest that loneliness affects quality of life, functional status, and cognitive function (Greene et al., 2018; Han et al., 2017). However, there remains a dearth of information on the risk factors for loneliness in older PLWH. Since loneliness is potentially modifiable (Masi, Chen, Hawkley, & Cacioppo, 2011), identification of key correlates of loneliness may reveal possible intervention targets to prevent or reduce loneliness and its associated negative health sequelae. The current study sought to identify factors related to loneliness in a sample of older PLWH. Based on the previous literature, we devised a conceptual model to assess specific factors in relation to loneliness (Figure 1). Specifically, we examined the relationships of non-modifiable factors (demographic factors and disease burden) and potentially modifiable factors (HIV-related stigma, HIV disclosure status, depressive symptoms, and social network size) to loneliness.
Figure 1.
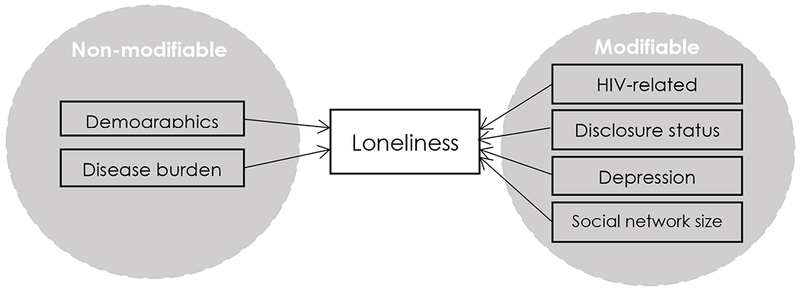
Conceptual Model of Loneliness
Methods
Recruitment and Data Collection
A cross-sectional, computer-administered survey with electronic medical record (EMR) review was completed with a sample of older PLWH enrolled at a comprehensive HIV clinic in Atlanta, GA. Participants were recruited through flyers, word of mouth, and healthcare provider referrals between August 2016 and April 2017. Eligible individuals were 50 years old or older, living with HIV, and had at least one medical visit established in the recruiting clinic. Due to the likelihood of low literacy, information about informed consent was provided both verbally and in writing to eligible individuals with sufficient time for questions. A consent post-test was given to assess individual’s capacity to provide informed consent and understanding of the content prior to enrollment into the study. Individuals who failed the consent post-test after three attempts were excluded from the study (n=3). A trained researcher was available during study survey administration to accommodate participants in completing the survey items on the computer. Total time to complete the survey was approximately 45-60 minutes. Participants were compensated with $25 in cash for their participation. Approval for the study protocol was granted from the university’s Institutional Review Board and the recruiting clinic’s Research Oversight Committee prior to study enrollment.
Measures
Loneliness was measured with the Patient-Reported Outcomes Measurement Information System (PROMIS)-Social Isolation (SI) Short Form v2.0 8a. The PROMIS-SI measure uses 8-items that are derived from social relationship scales and the UCLA-Loneliness Scale (Cyranowski et al., 2013) on a 5-point Likert scale (1=“Never” to 5=“Always”). The items include: “I feel left out,” “I feel that people barely know me,” “I feel isolated from others,” “I feel that people are around me but not with me,” “I feel isolated even when I am not alone,” “I feel that people avoid talking to me,” “I feel detached from other people,” and “I feel like a stranger to those around me.” A total raw score ranging from 8 to 40 is calculated by summing the values of the response to each item. The total raw score was converted into a standardized T-score with a mean of 50 and a standard deviation (SD) of 10 (Cella et al., 2010), following the score conversion table in the scoring instruction (PROMIS, 2015). Hence, a T-score of 50 represents an average score and a T-score of 60 represents one SD higher score of loneliness than the average persons in the United States (PROMIS, 2015). Based on the cutoff score of PROMIS-SI scale used in previous studies (Karayannis, Baumann, Sturgeon, Melloh, & Mackey, 2018), participants were dichotomized into lonely (T-score >50) and not lonely (T-score ≤50) when characterizing the differences based on loneliness severity. The mean T-score (continuous variable) was used in the bivariate and regression analyses. Cronbach’s alpha for our sample was 0.95.
HIV-related stigma was measured with Kalichman et al.’s Internalized AIDS-Related Stigma Scale (Kalichman et al., 2009), which contains 6 items rated dichotomously (1=“agree”, 0=“disagree”), with scores ranging from 0 to 6. A higher score indicates greater HIV-related stigma. This scale shows good internal reliability (α= .73 to .76) and criterion validity. The Cronbach’s alpha for our sample was 0.83.
HIV-disclosure status was assessed using one-item that assessed whether participants disclosed their HIV status to someone. Participants were dichotomized into two groups based on their response (0=“disclosure to no one”, 1=“disclosure to someone”).
Depressive symptoms were assessed using the 20-item Center for Epidemiologic Studies Depression Scale Revised (CESD-R; Eaton, Smith, Ybarra, Muntaner, & Tien, 2004) that assesses nine symptoms of depression (dysphoria, anhedonia, appetite, sleep, concentration, worthlessness, fatigue, agitation, and suicidal ideation) in accordance with the Diagnostic and Statistical Manual (DSM-V) criteria for Major Depressive Disorder. Participants answered 0= “Not at all or less than one day” to 3= “Nearly every day for 2 weeks,” with possible scores ranging from 0 to 60. A score ≥ 16 indicates at risk for clinical depression. The Cronbach’s α was 0.93 in our sample.
Social network size was measured using the Social Network Index (SNI), which assesses social contact with or participation in 12 types of social relationships at least once every 2 weeks in person or on the phone (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997) The types of social relationships include relationships with a spouse, parents, parents-in-law, children, other close family members, close neighbors, friends, colleagues/coworkers, schoolmates, fellow volunteers, members of groups without religious affiliation, and members of religious groups. The total number of people with whom the participants have regular contact was summed across the 12 possible social relationships. A higher score indicates greater social network size.
Disease burden and demographic covariates
Disease burden was assessed using comorbidity burden and functional status. Comorbidity burden was measured using the self-reported version of the Charlson Comorbidity Index (CCI; Charlson, Pompei, Ales, & MacKenzie, 1987). The CCI includes 19 conditions (myocardial infarction, congestive heart failure, peripheral vascular disease, etc.) in which participants were asked to identify the conditions that they were diagnosed (0=“No”, 1=“Yes”). The comorbidities were assigned a weight based on the adjusted 1-year mortality risk (Charlson et al., 1987). AIDS diagnosis was omitted in our study as its weight is outdated in the current era of combination ART (Zavascki & Fuchs, 2007) and age was not adjusted in this study as our sample consisted of only those who are age 50 and older. The CCI has strong construct validity and reliability (Hall, 2006) and has been used in previous studies with PLWH (Rodriguez-Penney et al., 2013). Functional Status was measured using a modified version of Instrumental Activities of Daily Living Scale (IADL; Lawton & Brody, 1969), which consists of self-reported levels of functionality on eight daily tasks (e.g., using the telephone, shopping, preparing meals, doing housework, doing laundry, traveling methods, medication management, and managing finances) with possible scores ranging from 0 (low function, dependent) to 8 (high function, independent). The IADL has been used frequently in HIV research and shows good reliability (α= .85) and validity.
We collected demographic data on age, gender, sexual orientation, years since HIV diagnosis, level of education, race/ethnicity, monthly income, self-rated health, and homelessness/unstable housing in the previous 12 months via self-report. Past homelessness/unstable housing was assessed by a question, “in the past 12 months, have you been homeless at any time? By homeless, I mean you were living on the street, in a shelter, a Single Room Occupancy (SRO) hotel, temporarily staying with friends/family, or living in a car” with a response of 0 (No) and 1 (Yes). Self-rated health was assessed using a single item, “in general, how would you rate your health” on a 5-point Likert scale and participants were dichotomized into two groups (0=“Poor/fair”, 1=“Good to Excellent”) based on their response.
HIV biomarkers including CD4+ T cell count and viral load were obtained from EMR. The lab values reported within the closest time from the day of study survey completion were selected, not to exceed two months. Values were dichotomized into clinically relevant groups or reported cutoff values from the EMR (CD4 ≥200 cells/mm3 or <200 cells/mm3; viral load undetectable [<40 copies/mL] or detectable [≥40 copies/mL]).
Data Analysis
Data were analyzed with SPSS version 24. Descriptive statistics were calculated for all study variables and covariates. Bivariate relationships between independent variables and loneliness were assessed using Pearson correlations and ANOVA, as appropriate. Demographic covariates that showed association with loneliness in bivariate analysis with p<.10 were included in the first step of multivariable linear regression analysis. The variables were entered sequentially with non-modifiable factors (demographic, disease burden) in the first step and potentially modifiable factors in the second step. Violations of key assumptions for multiple linear regression and multicollinearity were assessed. All p-values are two-tailed and considered statistically significant at p <.05, unless noted otherwise.
Sensitivity Analyses
Preliminary analysis showed that a significant number of this sample were homeless or unstably housed in the past 12 months (n=17), conditions that might place individuals at a more heightened risk for vulnerability and may confound the results. Therefore, two separate post-hoc sensitivity analyses were conducted. First, the same univariate, bivariate, and multivariable linear regression analyses were conducted only with cases without past homelessness/unstable housing (n=129). Second, a propensity score analysis using inverse probability of treatment weighting approach (Austin, 2011) was performed.
Results
A total of 146 older PLWH completed the study; sample characteristics are presented in Table 1. The sample was predominantly African American (AA; 85.6%), male (60.3%), heterosexual (63%), and had greater than high school education/GED (78%). Seventeen reported past homelessness/unstable housing, of which five were female and 16 were AA. About 25% of participants had a score of ≥16 on the depression scale, indicating possible clinical depression.
Table 1.
Demographic and Clinical Characteristics (N=146)
| Characteristic | n | % | ||
|---|---|---|---|---|
| Race/ethnicity | ||||
| African American/Black | 125 | 85.6 | ||
| White/Non-Hispanic | 12 | 8.2 | ||
| Other | 9 | 6.2 | ||
| Gender | ||||
| Born Male/Identify Male | 88 | 60.3 | ||
| Born Female/Identify Female | 55 | 37.7 | ||
| Born Male/Identify Female | 2 | 1.4 | ||
| I choose not to answer | 1 | 0.7 | ||
| Marital status | ||||
| Never married/Single | 86 | 58.9 | ||
| Divorced/Separated | 30 | 20.5 | ||
| Married/Living with Significant Other | 14 | 9.6 | ||
| Widow/Widower | 14 | 9.6 | ||
| Other | 2 | 1.4 | ||
| Sexual orientation | ||||
| Homosexual, Gay, or Lesbian | 30 | 20.5 | ||
| Heterosexual or Straight | 92 | 63.0 | ||
| A Man Who Has Sex With Men | 6 | 4.1 | ||
| Bisexual | 16 | 11.0 | ||
| Other | 2 | 1.4 | ||
| Homelessness or unstably housed in the past 12 months | ||||
| No | 129 | 88.4 | ||
| Yes | 17 | 11.6 | ||
| Education | ||||
| Some high school or less | 32 | 22.0 | ||
| High school graduate or equivalent (GED) | 54 | 37.0 | ||
| Some college or higher | 60 | 41.0 | ||
| HIV disclosure status | ||||
| Disclosure to someone | 129 | 88.4 | ||
| Disclosure to no one | 17 | 11.6 | ||
| Baseline HIV RNA viral loada | ||||
| Undetectable (<40 copies/mL) | 96 | 66.2 | ||
| Detectable | 49 | 33.8 | ||
| Baseline CD4 T Cell countb | ||||
| ≥ 200 cells/mm3 | 130 | 90.3 | ||
| < 200 cells/mm3 | 14 | 9.7 | ||
| Lonely participants* | 58 | 39.7 | ||
| Mean ± SD | Min | Max | ||
| Age | 56.53 ± 4.55 | 50 | 72 | |
| Years since HIV diagnosis | 18.10 ± 8.36 | 2 | 34 | |
| Comorbidity burden | 1.28 ± 1.54 | 0 | 8 | |
| Functional status | 7.66 ± 0.78 | 3 | 8 | |
| HIV-related stigma | 1.94 ±1.95 | 0 | 6 | |
| Depressive symptoms | 10.86 ± 10.31 | 0 | 47 | |
| Social network size | 16.14 ± 10.56 | 0 | 48 | |
| Loneliness | 47.19 ± 10.09 | 33.9 | 71.8 | |
Notes: SD=standard deviation.
n=145.
n=144.
T-score greater than 50 on PROMIS-Social Isolation scale.
Table 2 delineates characteristics of participants who are lonely (T-score >50) compared to those who are not lonely (T-score ≤50). Lonely participants were more likely to have poor/fair self-rated health, clinical depression, non-disclosure of HIV status, lower CD4+ T cell count, low social network size, and greater HIV-related stigma than non-lonely participants (p<.05). There were no differences in loneliness by gender or sexual orientation.
Table 2.
Differences in Participant Characteristics by Loneliness Severity.
| Lonelya N=58 (40%) | Not lonely N=88 (60%) | p | |
|---|---|---|---|
| Frequencies | |||
| Age group (χ2=0.62) | .73 | ||
| 50-59 | 44 | 68 | |
| 60-64 | 12 | 15 | |
| >=65 | 2 | 5 | |
| Gender (χ2=0.16) | .92 | ||
| Male | 36 | 52 | |
| Female | 21 | 34 | |
| Other | 1 | 2 | |
| Race (χ2=0.12) | .94 | ||
| White | 5 | 7 | |
| Black/AA | 49 | 76 | |
| Other | 4 | 5 | |
| Sexual orientation (χ2=0.48) | .79 | ||
| Homosexual | 12 | 18 | |
| Heterosexual | 35 | 57 | |
| MSM | 11 | 13 | |
| Education (χ2=1.31) | 0.52 | ||
| Some high school or less | 10 | 22 | |
| High school graduate/GED | 22 | 32 | |
| Some college or higher | 26 | 34 | |
| Homelessness or unstably housed in the past 12 months (χ2=5.01) | 0.03 | ||
| Yes | 11 | 6 | |
| No | 47 | 82 | |
| Self-rated health (χ2=17.63) | <.001 | ||
| Poor/fair | 24 | 10 | |
| Good to excellent | 34 | 78 | |
| HIV disclosure status (χ2=5.01) | 0.03 | ||
| To no one | 11 | 6 | |
| To someone | 47 | 82 | |
| Clinical depression (CESD-R ≥16; χ2=22.88) | <.001 | ||
| Yes | 27 | 10 | |
| No | 31 | 78 | |
| Baseline HIV RNA viral loadb (χ2=0.78) | .38 | ||
| Undetectable (<40 copies/mL) | 17 | 32 | |
| Detectable | 41 | 56 | |
| Baseline CD4 T Cell countc (χ2=0.12) | .73 | ||
| ≥ 200 cells/mm3 | 53 | 78 | |
| < 200 cells/mm3 | 5 | 9 | |
| Mean (SD) | |||
| Monthly income | 874.72 (470.45) | 1012.90 (797) | 0.24 |
| Comorbidity burden | 5.33 (3.39) | 4.27 (3.22) | .06 |
| Functional status | 7.48 (0.99) | 7.78 (0.58) | .02 |
| Depressive symptoms | 16.95 (12.01) | 6.85 (6.45) | <.001 |
| Social network size | 13.33 (10.63) | 17.99 (10.15) | .01 |
| HIV-related stigma | 3.02 (2.17) | 1.23 (1.39) | <.001 |
Notes: Items in bold were statistically significant. CESD-R= Center for Epidemiologic Studies Depression Scale Revised. SD=standard deviation.
T-score greater than 50 on PROMIS-Social Isolation scale.
n=145.
n=144.
Bivariate Analysis
Bivariate and multivariable analyses were conducted using the mean T-score for loneliness as the outcome variable. Depressive symptoms (r=.50, p<.001), HIV-related stigma (r=.46, p<.001), social network size (r= −.27, p=.001), HIV-disclosure status (r= −.18, p=.03), comorbidity burden (r=.27, p=.001), and functional status (r=−.21, p=.01) had statistically significant correlations with loneliness.
There were no statistically significant associations between demographic/clinical factors and loneliness, except for past homelessness (r=.23, p=.01); therefore, only past homelessness/unstable housing was included in the regression analysis. Marital status was excluded from the analysis because the SNI assessed marital status.
Multivariable Regression Analysis
Results of the two-step hierarchical multivariable linear regression on loneliness are presented in Table 3. In the first step, homelessness/unstable housing, comorbidity burden, and functional status were included. The second step considered potentially modifiable variables including HIV-related stigma, HIV-disclosure status, depressive symptoms, and social network size.
Table 3.
Multivariable Linear Regression Analysis on Lonelinessa (N=146).
| Variable | B | SE B | β | p | R2 | F | p |
|---|---|---|---|---|---|---|---|
| Step 1 | 0.15 | 8.35 | <.001 | ||||
| Homelessness or unstably housed in the past 12 months | 6.65 | 2.43 | 0.21 | .01 | |||
| Comorbidity burden | 1.57 | 0.51 | 0.24 | .00 | |||
| Functional status | −2.26 | 1.006 | −0.18 | .03 | |||
| Step 2 | 0.41 | 13.76 | <.001 | ||||
| Homelessness or unstably housed in the past 12 months | 1.27 | 2.20 | 0.04 | .56 | |||
| Comorbidity burden | 0.85 | 0.45 | 0.13 | .06 | |||
| Functional status | −1.59 | 0.86 | −0.12 | .07 | |||
| Depressive symptoms | 0.34 | 0.07 | 0.35 | <.001 | |||
| HIV-related stigma | 1.51 | 0.38 | 0.29 | <.001 | |||
| Social network size | −0.10 | 0.07 | −0.10 | .14 | |||
| Disclosure of HIV status to someone | −1.04 | 2.21 | −0.03 | .64 | |||
Notes: Items in bold were statistically significant. SE=Standard Error. Step 1 adjusted R2=0.13. Step 2 adjusted R2=0.38.
The mean T-score on PROMIS-Social Isolation scale.
The results of the first step found that homelessness/unstable housing (β = 0.21, p=.007), comorbidity burden (β = 0.24, p=.002), and functional status (β = −0.18, p=.026) were significant correlates of loneliness and the model explained 15% of the variance in loneliness (R2 = 0.15, F(3, 142)= 8.35, p < .001). In the second step, the addition of modifiable variables in the regression analysis accounted for an additional 26% of the variance in loneliness (R2 = 0.41, F(7, 138)= 13.76, p < .001). Depressive symptoms (β = 0.35, p < .001) and HIV-related stigma (β = 0.29, p < .001) were significantly associated with loneliness. Inclusion of the variables in the second step reduced the independent effects of homelessness/unstable housing and disease burden on loneliness, rendering their coefficients non-significant.
Sensitivity Analyses
Post-hoc sensitivity analyses were conducted using the subcases without past homelessness in the previous 12 months (n=129). Results of the subcase analysis were similar to the original results. Additionally, the propensity-weighted data results remained similar to the original results. These similar results establish further credibility and robustness for our original findings.
Discussion
This study investigated correlates of loneliness in older PLWH. We found that a meaningful proportion of our sample of older PLWH experience loneliness; approximately 40% were categorized as lonely. This rate is similar to a recent study that found a significant proportion of older PLWH reporting loneliness (Greene et al., 2018) and to the general population of adults in the United States (Wilson & Moulton, 2010).
In line with the well-established association between loneliness and disease burden found in the general gerontology literature (Pinquart & Sorensen, 2001), we found that past homelessness/unstable housing and greater disease burden were associated with loneliness in older PLWH. No other demographic characteristics related significantly to loneliness except for the past homelessness/unstable housing. We know that homeless individuals have small and fragile social networks (Bower, Conroy, & Perz, 2018; Gray, Shaffer, Nelson, & Shaffer, 2016). Homelessness may, thus, disproportionately expose older PLWH to additional stressors that predispose them to marginalization and psychosocial vulnerabilities including trauma, financial insecurities, social exclusion, and discrimination (Gray, Shaffer, Nelson, & Shaffer, 2016), all of which may further exacerbate loneliness. Furthermore, it is recognized that experiences of homelessness exacerbate psychiatric conditions, including schizophrenia and depression (Castellow, Kloos, & Townley, 2015), which have been shown to be associated with loneliness (Badcock et al., 2015; Grov et al., 2010). Future studies might profitably examine the differences in levels of loneliness in homeless older PLWH based on other inequalities and mental health conditions. More descriptive and qualitative research is required to identify potential gaps in implementation science to improve well-being and reduce loneliness in older PLWH with past homelessness.
Higher loneliness was associated with greater depressive symptoms and HIV-related stigma above and beyond the influence of past homelessness/unstable housing and disease burden. The relationship between depression and loneliness has been previously established, and growing evidence in the general older adult population suggests that loneliness is a unique proximal factor preceding depression (Barg et al., 2006; Cacioppo, Hawkley, & Thisted, 2010). Our finding on the effects of HIV-related stigma on loneliness is consistent with other studies (Grov et al., 2010; Fekete, Williams, & Skinta, 2018). Growing old with HIV or being diagnosed with HIV as an older person may come with multi-layered stigma and misconceptions, including prejudices related to sexual orientation, sexual and marginalized behaviors, and/or stereotypes related to aging, any or all of which may affect individuals’ social lives and well-being. Our results demonstrate a continuing and important need for interventions to reduce HIV-related stigma and services that assess loneliness in older PLWH. Studies are needed to understand and identify the complex issues of multilayered stigma in older PLWH for appropriate intervention testing and to assess whether stigma reduction intervention improves associated outcomes including loneliness.
Although disclosure of HIV-status and larger social network size were negatively related to loneliness in bivariate analyses, these factors were not related to loneliness in multivariable regression. Our findings imply that HIV-related stigma and depressive symptoms are so strongly associated with loneliness that they suppress the effects of social network size on loneliness. Future studies might, therefore, consider assessing whether there are differences in loneliness depending on one’s disclosure of HIV to certain groups of contacts.
This study should be considered with its limitations. Its cross-sectional design precludes inferences about causality. Temporal effects of loneliness were not assessed, and therefore future studies should utilize longitudinal designs to assess for changes in loneliness and its correlates. Generalizability may be limited since our sample was predominately male, AA, heterosexual, and had been living with HIV for many years. However, some of these characteristics are similar to the current HIV epidemic in the South (CDC, 2017). Many potentially positive factors of aging, such as resiliency, mastery, and wisdom, may protect older PLWH from loneliness, but these factors were not assessed. Future studies should explore how these protective factors may affect loneliness. Study data were collected from a convenience sample of older PLWH attending a comprehensive HIV care clinic in a high resource setting offering a “one-stop shop” practice that provides multidisciplinary services, including support groups. This setting and opportunity to engage in social activities may have affected our sample’s social network size and its influence on loneliness. Despite these limitations, this study contributes to the literature by identifying key correlates to loneliness in older PLWH. As such, it may single out targets for interventions designed to reduce loneliness and prevent negative outcomes.
The experience of loneliness among older PLWH is multifaceted and is affected by HIV-related stigma and depression. Loneliness was prevalent among our sample of older PLWH residing in high resource setting. As HIV/AIDS has transformed into a chronic and manageable condition, more PLWH will enter into an older age and loneliness may become a more pronounced concern for older PLWH in the future. Loneliness and issues related to social isolation need to be assessed in order to comprehensively address the care of older PLWH.
Acknowledgements
This work was supported by the National Institute of Nursing Research [F31NR015975; P30AI050409].
Footnotes
Disclosure Statement
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Contributor Information
Moka Yoo-Jeong, Columbia University, School of Nursing, New York, NY, USA.
Kenneth Hepburn, Emory University Nell Hodgson Woodruff School of Nursing, Atlanta, Georgia, USA.
Marcia Holstad, Emory University Nell Hodgson Woodruff School of Nursing, Atlanta, Georgia, USA.
Regine Haardörfer, Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Atlanta, Georgia, USA.
Drenna Waldrop-Valverde, Emory University Nell Hodgson Woodruff School of Nursing, Atlanta, Georgia, USA.
References
- Austin PC (2011). An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behavioral Research, 46(3), 399–424. doi: 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badcock JC, Shah S, Mackinnon A, Stain HJ, Galletly C, Jablensky A, & Morgan VA (2015). Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophrenia Research, 169(1-3), 268–273. doi: 10.1016/j.schres.2015.10.027 [DOI] [PubMed] [Google Scholar]
- Barg FK, Huss-Ashmore R, Wittink MN, Murray GF, Bogner HR, & Gallo JJ (2006). A mixed-methods approach to understanding loneliness and depression in older adults. The Journals of Gerontology. Series B, Psychological sciences and social sciences, 61(6), S329–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower M, Conroy E, & Perz J (2018). Australian homeless persons’ experiences of social connectedness, isolation and loneliness. Health & Social Care in the Community, 26(2), e241–e248. doi: 10.1111/hsc.12505 [DOI] [PubMed] [Google Scholar]
- Brooks JT, Buchacz K, Gebo KA, & Mermin J (2012). HIV infection and older Americans: the public health perspective. American Journal of Public Health, 102(8), 1516–1526. doi: 10.2105/ajph.2012.300844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453–463. doi: 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellow J, Kloos B, & Townley G (2015). Previous homelessness as a risk factor for recovery from serious mental illnesses. Community Mental Health Journal, 51(6), 674–684. doi: 10.1007/s10597-014-9805-9 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). HIV Surveillance Report, 2015. Retrieved from Atlanta, GA: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- Centers for Disease Control and Prevention. (2017). HIV Surveillance Report, 2017. Retrieved from Atlanta, GA: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, … Hays R (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. doi: 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, & MacKenzie CR (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases, 40(5), 373–383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, & Gwaltney JM Jr. (1997). Social ties and susceptibility to the common cold. Journal of the American Medical Association, 277(24), 1940–1944. [PubMed] [Google Scholar]
- Cornwell EY, & Waite LJ (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. doi: 10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranowski JM, Zill N, Bode R, Butt Z, Kelly MA, Pilkonis PA, … Cella D (2013). Assessing social support, companionship, and distress: National Institute of Health (NIH) Toolbox Adult Social Relationship Scales. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 32(3), 293–301. doi: 10.1037/a0028586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Smith C, Ybarra M, Muntaner C, & Tien A (2004). Center for Epidemiologic Studies Depression Scale: review and revision (CESD and CESD-R).
- Enriquez M, Lackey N, & Witt J (2008). Health concerns of mature women living with HIV in the Midwestern United States. Journal of the Association of Nurses in AIDS Care, 19(1), 37–46. doi: 10.1016/j.jana.2007.09.004. [DOI] [PubMed] [Google Scholar]
- Fekete EM, Williams SL, & Skinta MD (2018). Internalised HIV-stigma, loneliness, depressive symptoms and sleep quality in people living with HIV. Psychology & Health, 33(3), 398–415. [DOI] [PubMed] [Google Scholar]
- Gray HM, Shaffer PM, Nelson SE, & Shaffer HJ (2016). Changing Social Networks Among Homeless Individuals: A Prospective Evaluation of a Job- and Life-Skills Training Program. Community Mental Health Journal, 52(7), 799–808. doi: 10.1007/s10597-014-9817-5 [DOI] [PubMed] [Google Scholar]
- Greene M, Covinsky KE, Valcour V, Miao Y, Madamba J, Lampiris H, … Deeks SG (2015). Geriatric Syndromes in Older HIV-Infected Adults. Journal of Acquired Immune Deficiency Syndromes, 69(2), 161–167. doi: 10.1097/QAI.0000000000000556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene M, Hessol NA, Perissinotto C, Zepf R, Parrott AH, Foreman C, … & John M (2018). Loneliness in older adults living with HIV. AIDS and Behavior, 22(5), 1475–1484. doi: 10.1007/s10461-017-1985-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Golub SA, Parsons JT, Brennan M, & Karpiak SE (2010). Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care, 22(5), 630–639. doi: 10.1080/09540120903280901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guaraldi G, Orlando G, Zona S, Menozzi M, Carli F, Garlassi E, … Palella F (2011). Premature age-related comorbidities among HIV-infected persons compared with the general population. Clinical Infectious Diseases, 53(11), 1120–1126. doi: 10.1093/cid/cir627 [DOI] [PubMed] [Google Scholar]
- Hall SF (2006). A user’s guide to selecting a comorbidity index for clinical research. Journal of Clinical Epidemiology, 59(8), 849–855. doi: 10.1016/j.jclinepi.2005.11.013 [DOI] [PubMed] [Google Scholar]
- Han SD, Adeyemi O, Wilson RS, Leurgans S, Jimenez A, Oullet L, … Barnes LL (2017). Loneliness in Older Black Adults with Human Immunodeficiency Virus Is Associated with Poorer Cognition. Gerontology, 63(3), 253–262. doi: 10.1159/000455253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havlik RJ, Brennan M, & Karpiak SE (2011). Comorbidities and depression in older adults with HIV. Sex Health, 8(4), 551–559. doi: 10.1071/sh11017 [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, & Ginindza T (2009). Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care, 21(1), 87–93. doi: 10.1080/09540120802032627 [DOI] [PubMed] [Google Scholar]
- Karayannis NV, Baumann I, Sturgeon JA, Melloh M, & Mackey SC (2018). The Impact of Social Isolation on Pain Interference: A Longitudinal Study. Annals of Behavioral Medicine, 53(1), 65–74. doi: 10.1093/abm/kay017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist, 9(3), 179–186. [PubMed] [Google Scholar]
- Masi CM, Chen H-Y, Hawkley LC, & Cacioppo JT (2010). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review. doi: 10.1177/1088868310377394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathai S, Bajillan H, Landay AL, & High KP (2014). Is HIV a model of accelerated or accentuated aging? Journals of Gerontology Series A: Biological Sciences and Medical sciences, 69(7), 833–842. doi: 10.1093/gerona/glt168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peplau LA, & Perlman D (1982). Perspective on Loneliness In Peplau LA & Perlman D (Eds.), Loneliness: A Sourcebook of Current Theory, Research, and Therapy (pp. 1–18). New York, NY: Wiley-Interscience. [Google Scholar]
- Pinquart M, & Sorensen S (2001). Influences on loneliness in older adults: A meta-analysis. Basic and Applied Social Psychology, 23(4), 245–266. doi: 10.1207/153248301753225702 [DOI] [Google Scholar]
- PROMIS. (2015). PROMIS social isolation: a brief guide to the PROMIS social isolation instruments. Retrieved from https://www.assessmentcenter.net/documents/PROMIS%20Social%20Isolation%20Scoring%20Manual.pdf
- Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, & Miret M (2018). Association of loneliness with all-cause mortality: A meta-analysis. PloS one, 13(1), e0190033. doi: 10.1371/journal.pone.0190033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Penney AT, Iudicello JE, Riggs PK, Doyle K, Ellis RJ, Letendre SL, … Woods SP (2013). Co-Morbidities in Persons Infected with HIV: Increased Burden with Older Age and Negative Effects on Health-Related Quality of Life. AIDS Patient Care and STDs, 27(1), 5–16. doi: 10.1089/apc.2012.0329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrimshaw EW, & Siegel K (2003). Perceived barriers to social support from family and friends among older adults with HIV/AIDS. Journal of Health Psychology, 8(6), 738–752. doi: 10.1177/13591053030086007 [DOI] [PubMed] [Google Scholar]
- Shippy RA, & Karpiak SE (2005). The aging HIV/AIDS population: fragile social networks. Aging Mental Health, 9(3), 246–254. doi: 10.1080/13607860412331336850 [DOI] [PubMed] [Google Scholar]
- Ware N, Wyatt M, & Tugenberg T (2006). Social relationships, stigma and adherence to antiretroviral therapy for HIV/AIDS. AIDS Care. 18(8), 904–910. [DOI] [PubMed] [Google Scholar]
- Wilson C, & Moulton B (2010). Loneliness among Older Adults: A National Survey of Adults 45+. Retrieved from https://assets.aarp.org/rgcenter/general/loneliness_2010.pdf
- Zavascki AP, & Fuchs SC (2007). The need for reappraisal of AIDS score weight of Charlson comorbidity index. Journal of Clinical Epidemiology, 60(9), 867–868. doi: 10.1016/j.jclinepi.2006.11.004 [DOI] [PubMed] [Google Scholar]


