Abstract
Objectives:
Anemia, either chronic or newly developed in the hospital as results of underlying diseases and/or phlebotomy, is commonly seen among general medical inpatients and its impacts on the quality and efficiency of care are unknown.
Methods:
This study investigates the relationship between hemoglobin level, length of stay, and 30-day unplanned readmission rate in a cohort of 314 general medical patients age 18 and older admitted to one teaching service over a period of 4 months in a large urban academic medical center, using retrospective chart review of the electronic health record.
Results:
Anemia was common among this cohort of general medical inpatients (44.6%), and there was a statistically significant decrease in hemoglobin levels during their hospitalization. Anemic patients, as compared to non-anemic patients, had significantly longer mean and median length of stay. Importantly, the admission hemoglobin level and its change during hospitalization were significant predictors of increased length of stay. For every one unit increase in admission hemoglobin level, the median length of stay was reduced by 0.5 day. For every one unit increase in the level of hemoglobin change, the median length of stay was extended by 1.5 days. Likewise, the discharge hemoglobin level predicted rate of 30-day unplanned readmission. For every one unit decrease in discharge hemoglobin level, the readmission rate increased by nearly 4%. These relationships remained after adjusting for common demographic and clinical variables including age, gender, nutritional status, and numbers of comorbidities.
Conclusion:
Anemia is common among general medical inpatients and adversely affects their length of stay and 30-day unplanned readmission rate.
Keywords: Anemia, General medical inpatients, Length of stay, 30-day unplanned readmission rate
Brief Description:
Anemia is common among general medical inpatients and its impact on the quality and efficacy of care is unknown. This paper investigates the relationship between anemia and the length of stay and 30-day unplanned readmission rate of a cohort of 314 general medical inpatients in a large urban academic medical center.
Introduction:
The World Health Organization defines anemia as hemoglobin level < 12 g/dL in females and < 13 g/dL in males.1 The causes of anemia are diverse, especially in the elderly, including iron deficiency, nutritional deficiency, malignancies, chronic kidney disease, chronic heart failure, and chronic inflammation.2 While traditionally considered an outpatient problem, newly developed anemia and/or worsening of chronic anemia as results of phlebotomy, diagnostic procedures, and impaired bone marrow production, is increasingly recognized in hospitalized patients.3 It leads to adverse clinical outcomes such as increased mortality among patients with acute myocardial infarction;4 increased risk of delirium and falls among geriatric inpatients;5,6 and increased length of stay, readmission rate, and mortality among medical inpatients in New Zealand.7 In the large scale OPTIMIZE-HF registry composed of hospitalized heart failure patients, nearly half are anemic and they have higher in-hospital mortality, length of stay, and 30-day unplanned readmission rate.8 Interestingly, although widely considered a quality indicator for hospital care,9 the 30-day unplanned readmission rate has been previously shown to correlate only with medical/psychiatric comorbidities and prior use of medical services.10 Finally, although adverse effects of anemia are apparent from these studies, increased rates of infection and death from the use of erythropoiesis-stimulating agents to increase hemoglobin level have also been reported,11 and a fairly conservative transfusion threshold of 7 g/dL in hospitalized patients has recently been established.12 We hypothesize that the presence of anemia predicts adverse clinical outcomes in general medical inpatients such as prolonged length of stay and higher 30-day unplanned readmission rate. Clinical courses, demographic data, and hemoglobin level of a cohort of 314 general medical inpatients in an urban teaching hospital are retrospectively analyzed in relation to their length of stay and rate of 30-day unplanned readmission to the same institution.
Material and Methods:
The study cohort, after excluding 11 patients who were transferred to another service or who had fewer than two hemoglobin (hgb) values measured during their hospitalization, included 314 adult patients age 18 and older admitted to one general medicine teaching service at our institution over a 4 months period. No single discharge diagnosis accounted for more than 10 patients. The demographic and laboratory data including age, gender, admission albumin level, admission and discharge hgb level, and numbers of medical comorbidities, were manually extracted from the electronic health record. Length of stay (LOS) was expressed as continuous variable while gender and 30-day unplanned readmission was expressed as dichotomous variables. Medical comorbidities defined by ICD-9 code included malignant accelerated hypertension, coronary artery disease, congested heart failure, diabetes mellitus, stroke, cirrhosis, HIV/AIDs, any cancer or hematologic malignancies, asthma, chronic obstructive pulmonary disease, chronic kidney disease or end stage renal disease, diverticulosis/diverticulitis, autoimmune or inflammatory/rheumatic disease, as well as diagnosis of chronic anemia. Pearson or Spearman rank test was used to generate co-linearity correlations among predictor variables. Student’s t-test was used to compare means and nonparametric Fisher’s test was used to compare medians. We generated predictor models for LOS and 30-day unplanned readmission rate using median regression and logistic regression respectively. Variables significant at p < 0.2 on univariate analysis were included in the preliminary multivariate analysis. After such analysis, predictors not significant at p < 0.05 were removed from the final multivariate regression model. All statistical analyses were performed in STATA10. This study was approved by the Institutional Review Board (IRB) at Weill Cornell Medical College.
Results:
Table 1 showed clinical characteristics of this cohort of 314 patients. The mean age was 58.7 years. Female accounted for 53.5% of patients. Most patients had 1–3 medical comorbidities. The mean albumin level was 3.37 g/dL. Based on the World Health Organization (WHO) definition, anemia was present in 44.6% (140/314) of patients on admission (45.9% of males and 43.5% of females, p = 0.773). The mean admission hgb (sthgb) level was 12.3 g/dL and the mean discharge hgb (lasthgb) level was 11.7 g/dL, which was statistically significant (p = 0.0007). The average hgb decrease of 0.6 g/dL during hospitalization was consistent with previous findings.13,14 As expected, female patients had lower hgb level on admission and discharge as compared to male patients. The mean and median LOS was 6.47 and 3 days, respectively, and the overall 30-day unplanned readmission rate in this cohort of patients was 16.2%, consistent with previously published data.9
Table 1.
Epidemiological and clinical characteristics of the cohort
| Variables | Results |
|---|---|
| Mean age, year | 58.7 |
| Female, (%) | 168/314 (53.5%) |
| Prevalence of anemia at admission | 140/314 (44.6%) |
| Female, (%) | 73/168 (43.5%) |
| Male, (%) | 67/146 (45.9%) |
| Albumin, g/dL (SD) | 3.37 (0.71) |
| Mean admission hemoglobin, g/dL (SD) | 12.3 (2.4) |
| Female | 12.0 |
| Male | 12.6 |
| Mean discharge hemoglobin, g/dL (SD) | 11.7 (2.0) |
| Female | 11.3 |
| Male | 12.1 |
| Mean (median) length of stay, days | 6.47 days (3 days) |
| 30-day readmission rate, (%) | 51/314 (16.2%) |
| Number of medical comorbidities, (%) | |
| Zero | 37/314 (11.8%) |
| One | 79/314 (25.2%) |
| Two | 86/314 (27.4%) |
| Three | 67/314 (21.3%) |
| Four or more | 45/314 (14.3%) |
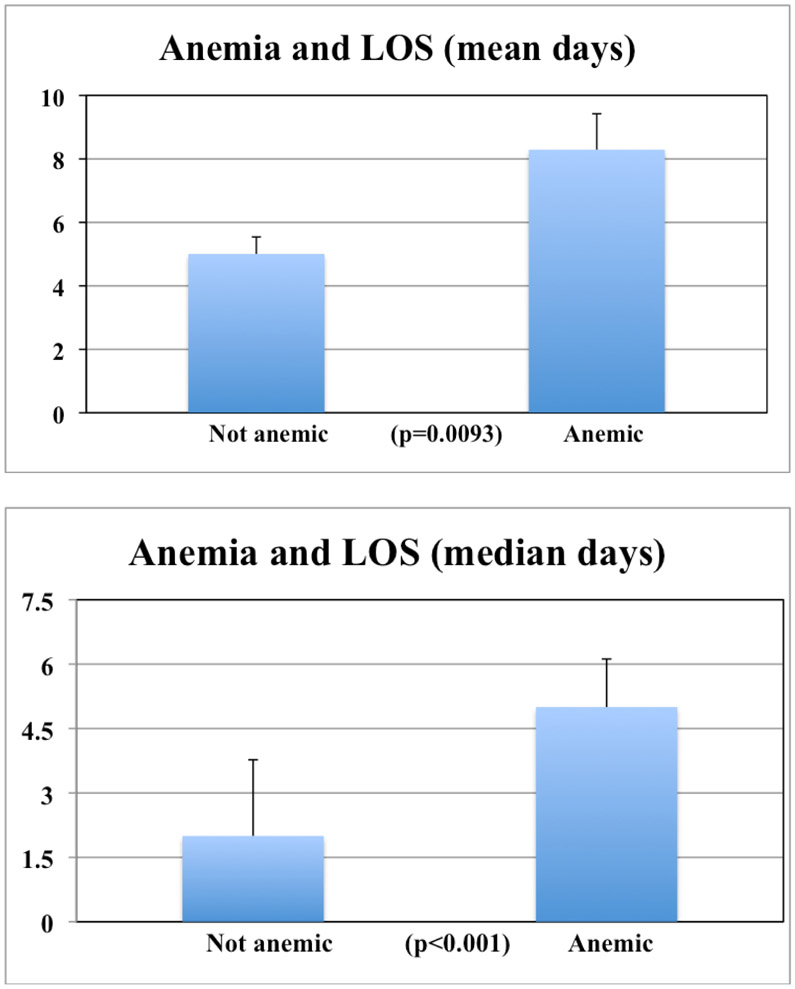
As shown in Figure 1, anemic patients defined by the WHO criteria had significantly longer mean and median LOS comparing to non-anemic patients, 8.29 days versus 5 days (p = 0.0093) for the mean, and 5 days versus 2 days (p < 0.001) for the median, respectively. We next examined correlations among all variables listed in Table 1, age, gender, numbers of medical comorbidities, albumin level, and hgb levels. We used nonparametric correlation analyses and found that both admission and discharge hgb levels significantly interacted with age, gender, numbers of medical comorbidities, and with each other to various extents (data not shown). Therefore, hgb change during the index hospitalization, d-hgb (admission hgb level minus discharge hgb level), was used additionally as a predictor variable. 247 patients had d-hgb level >= 0.
Figure 1.
Adverse effect of anemia on inpatient LOS
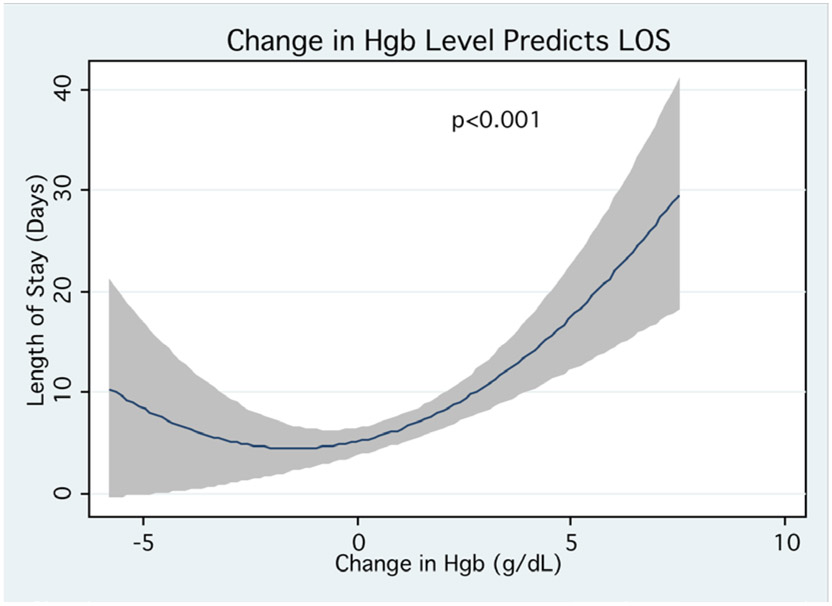
As LOS was not normally distributed, median quintile regression was used in univariate and multivariate analyses to generate a predictor model based on hgb levels. After the initial univariate analysis, variables with p > 0.2 were dropped, as well as variables of gender and comorbidities, which had significant interactions with all hgb levels. As shown in Table 2, the final multivariate predictor model for LOS included sthgb level, d-hgb level, and albumin level after adjusting for age, gender, and numbers of medical comorbidities. There were no significant interactions among these three variables and the complete analysis was tabulated in supplemental Table 1. For every one-unit increase in d-hgb level, the median LOS was extended by 1.5 days. Likewise, for every one-unit increase in sthgb level or albumin level, the median LOS was reduced by 0.5 or 1.9 days respectively. When we analyzed the cohort of 247 patients with d-hgb level >= 0, these three variables remained highly significant for prediction of LOS (tabulated in supplemental Table 1). Figure 2 depicted the regression relationship between d-hgb level and LOS. Interestingly, there was a paradoxical increase in LOS at negative d-hgb range, possibly resulting from time-consuming inpatient investigations and/or blood transfusion.
Table 2.
Multivariate predictors of inpatient LOS*
| Predictor | Coefficient | 95% CI | P value |
|---|---|---|---|
| D-hgb (g/dL) | 1.49 | 1.20 to 1.77 | <0.001 |
| Sthgb (g/dL) | −0.50 | −0.69 to −0.31 | <0.001 |
| Albumin (g/dL) | −1.87 | −2.42 to −1.32 | <0.001 |
Predictor variables with p > 0.2 in the univariate analysis, as well as gender and comorbidities, which had significant interaction with hgb levels, were dropped from final multivariate model.
Figure 2.
The relationship (95%CI in shade) between change in hgb (d-hgb) level and LOS
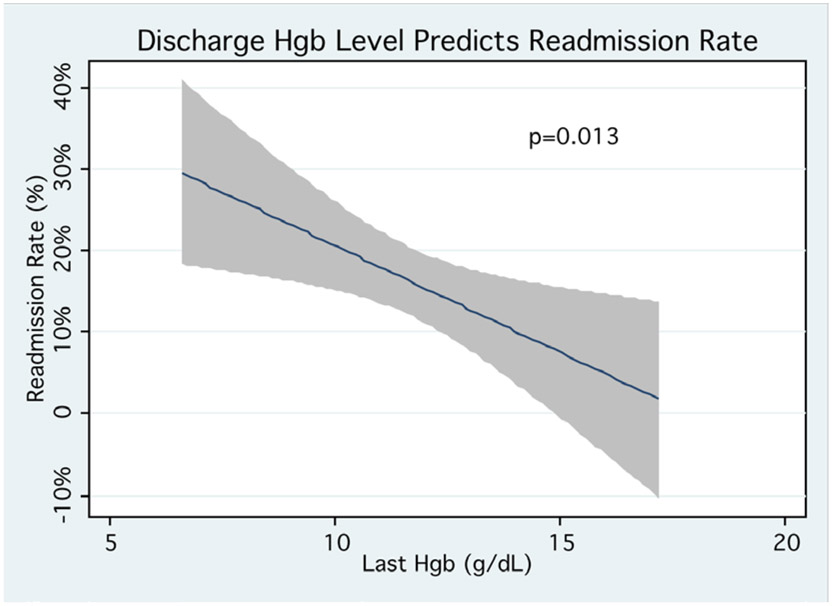
Finally, we generated a predictor model for the rate of 30-day unplanned readmission to the same institution based on hgb levels. This was accomplished using the logistic regression model. In the univariate analysis, only lasthgb level, d-hgb level, and age were significant predictors with p < 0.2. Age and comorbidities had significant interactions with all hgb levels and therefore were dropped from subsequent multivariate analysis. In a stepwise multivariate analysis controlling for age, gender, albumin level, and numbers of medical comorbidities, only lasthgb level remained significant predictor as shown in Table 3 (OR 0.82, p = 0.013, 95% CI 0.70 to 0.96). The complete analysis was tabulated in supplemental Table 2. For every one unit decrease in lasthgb level, the 30-day unplanned readmission rate increased by nearly 4%. The final regression model of predicting 30-day unplanned readmission rate based on lasthgb level was illustrated in Figure 3.
Table 3.
Multivariate predictor of 30-day unplanned readmission rate*
| Predictor | Odds Ratio | 95% CI | P value |
|---|---|---|---|
| Lasthgb (g/dL) | 0.82 | 0.70 to 0.96 | 0.013 |
Predictor variables with p > 0.2 in the univariate analysis, as well as gender and comorbidities, which had significant interaction with hgb levels, were dropped from final multivariate model. In addition, d-hgb has a p-value of 0.154 in the initial multivariate analysis and was dropped from final multivariate model.
Figure 3.
The relationship (95%CI in shade) between discharge hgb (lasthgb) level and 30-day unplanned readmission rate
Discussion:
The quality, safety, and efficiency of inpatient care is under increasing scrutiny.9 Previous studies have shown that inpatient LOS and 30-day unplanned readmission rate, the hospital benchmarks for efficiency and quality of care respectively, may be predicted by certain clinical and demographic characteristics.10 We demonstrate here for the first time that, among US general medical inpatients, sthgb and d-hgb levels are significant predictors for LOS; while lasthgb level predicts rate of 30-day unplanned readmission. Their predictive accuracy remains after adjusting for common demographic and clinical variables such as age, gender, albumin level, and numbers of medical comorbidities. Given the high prevalence of anemia in our and several other patient populations,3-7,14 these findings set the stage for designing and testing of innovative and collaborative care approaches to its investigation and treatment.
Anemia in general medical inpatients is often the extension of chronic anemia and has additional etiologies such as phlebotomy, diagnostic testing, hemodilution, nutritional deficiency, or occult bleeding.2-4,13,14 Of those diagnoses, iron deficiency anemia from occult gastrointestinal bleeding, malignancy, or celiac disease is probably the most worrisome.15 Inpatient clinical providers must track these important results and ensure close follow-up with outpatient gastroenterology providers. Quality improvement initiatives based on information technology such as automatic flagging of low ferritin level may prove to be useful. In addition, given the adverse impact of phlebotomy in causing new anemia or worsening of chronic anemia, clinical algorithms or standardization of laboratory testing may be necessary to avoid excessive phlebotomy in the hospital.3,4,13,14 Finally, while treating iron deficiency anemia with intravenous iron in heart failure patients improved their quality of life,16 inpatient providers should be cautious in using erythropoiesis-stimulating agents and/or blood transfusion to raise hgb levels, given their significant mortality and morbidity risks.11,12 Simpler treatment options such as nutritional repletion, oral iron supplementation, and avoidance of unnecessary phlebotomy, may be equally effective in maintaining hgb levels.
Many laboratory tests, such as serum creatinine or albumin level, have been used to predict 30-day unplanned readmission rate with various degree of success.10 To our knowledge, this is the first US study examining the accuracy of a single laboratory test, hgb level, in predicting 30-day unplanned readmission rate among general medical inpatients. We show that for every unit decrease in lasthgb level, there is a nearly 4% increase in readmission rate. Given the extensive etiologies of anemia and its pleotropic physiologic effect, especially in the elderly, it is possible that anemia is a proxy of the underlying overall health and/or severity of illness.2,3 However, given that no single discharge diagnosis accounts for more than 10 patients, anemia in our study likely represent an “additional disease” with various degrees of severity. Thus the observed prolonged LOS and increased 30-day unplanned readmission rate in anemic patients may result from and correlate with the severity of this “additional disease”.
Our study has several limitations. First, this study is retrospective in design with small sample size in one institution thus limiting its generalization. Second, it lacks control for the severity of the principle illness or other potential confounding factors such as patient volume status or units of transfusion received. Finally, we show that there were associations between anemia and LOS and 30-day unplanned readmission rate, and the causal relationship cannot be inferred from these results. Nevertheless, our findings are consistent with the results of many previous studies examining the impacts of anemia in the inpatient setting,3-8, 13,14 and importantly, are novel in identifying the inverse relationship between the severity of anemia and the quality and efficiency of care for general medical inpatients. Moreover, our predictor models control for age, gender, numbers of medical comorbidities, and nutritional status, and their predictive accuracy is comparable to more complicated models.10 Taken together, our results reveal high prevalence of anemia among general medical inpatients, and demonstrate its associated adverse impacts on inpatient care delivery. Large scale investigations on the etiologies of anemia and its treatment in general medical inpatients are needed.
Conclusion:
Anemia is highly prevalent among general medical inpatients, and is significantly associated with increases in LOS and 30-day unplanned readmission rate. Hospitalists and outpatient providers should collaborate closely to ensure the timely investigation, treatment monitoring, and follow up care for anemic inpatients.
Supplementary Material
Key Points:
In a cohort of 314 hospitalized general medical patients, anemia is a common laboratory finding on admission and discharge.
The admission hemoglobin level and its decrease during hospitalization inversely correlate with length of stay; and the discharge hemoglobin level inversely correlates with rate of 30-day unplanned readmission.
Acknowledgments
The authors would like to thank Mary Elizabeth Kelser, RN, MBA, for administrative assistance
Footnotes
The authors have no financial disclosures to declare and no conflicts of interest to report
References:
- 1.World Health Organization. Nutritional Anemias. Technical Report Series No. 405. Geneva, Switzerland: WHO, 1968. [Google Scholar]
- 2.Bross MH, Soch K, Smith-Knuppel T. Anemia in older persons. Am Fam Physician 2010; 82: 480–487. [PubMed] [Google Scholar]
- 3.Spence RK. Medical and economic impact of anemia in hospitalized patients. Am J Health-Syst Pharm. 2007; 64: S3–10. [DOI] [PubMed] [Google Scholar]
- 4.Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med 2011; 171: 1646–53. [DOI] [PubMed] [Google Scholar]
- 5.Dharmarajan TS, Avula S, Norkus EP. Anemia increases risk for falls in hospitalized older adults. J Am Med Dir Assoc 2006; 7: 287–293. [DOI] [PubMed] [Google Scholar]
- 6.Joosten E, Lemiengre J, Nelis T, Verbeke G, Milisen K. Is anemia a risk factor for delirium in an acute geriatric population? Gerontology 2006; 52: 382–5. [DOI] [PubMed] [Google Scholar]
- 7.Nathavitharana RL, Murray JA, D’Sousa N, Sheehan T, Frampton CM, Baker BW. Anemia is highly prevalent among unselected internal medicine inpatients and is associated with increased mortality, earlier readmission and more prolonged hospital stay: an observational retrospective cohort study. Intern Med J. 2012; 42: 683–91. [DOI] [PubMed] [Google Scholar]
- 8.Young JB, Abraham WT, Albert NM, et al. Relation of low hemoglobin and anemia to morbidity and mortality in patients hospitalized with heart failure (insight from the OPTIMIZE-HF registry). Am J Cardiol 2008; 101: 223–30. [DOI] [PubMed] [Google Scholar]
- 9.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare Fee-for-Service Program. N Engl J Med 2009; 360: 1418–28. [DOI] [PubMed] [Google Scholar]
- 10.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systemic review. JAMA 2011; 306: 1688–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phrommintikul A, Haas SJ, Elsik M, Krum H. Mortality and target haemoglobin concentrations in anaemia patients with chronic kidney disease treated with erythropoietin: a meta-analysis. Lancet 2007; 369: 381–8. [DOI] [PubMed] [Google Scholar]
- 12.Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med 2012; 157: 49–58. [DOI] [PubMed] [Google Scholar]
- 13.Thavendiranathan P, Bagai A, Ebidia A, et al. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med 2005; 20: 520–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Languasco A, Agustin L, Nicolas C, et al. Hemoglobin concentration variations over time in general medical inpatients. J Hosp Med 2010; 5: 283–8. [DOI] [PubMed] [Google Scholar]
- 15.Goddard AF, James MW, McIntyre AS, et al. Guidelines for the management of iron deficiency anemia. Gut 2011; 60: 1309–16. [DOI] [PubMed] [Google Scholar]
- 16.Anker SD, Colet JC, Filippatos G, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. NEJM 2009; 361: 2436–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.