Abstract
Despite high levels of traffic-related mortality, injury, and impairment among former service members, measures validated to assess problematic driving in this population remain limited. The current study examined characteristics of the Driving Behavior Survey (DBS) in male veterans (76.3% White; age: M = 56.4, SD = 12.3) meeting criteria for PTSD. Confirmatory factor analyses indicated acceptable fit of a 3-factor model specifying dimensions of anxiety-based performance deficits, exaggerated safety/caution, and hostile/aggressive driving behavior. Concurrent associations with indices of anxiety, depression, trauma history, and clinician-rated PTSD were consistent with small (r = .10–.29) to medium (r = .30–.49) effects. Discriminative validity was noted through elevations in performance deficit (d = .26), safety/caution (d = .50), and hostile/aggressive (d = .39) scales relative to published data from student drivers. Scores comparable to civilian motorists with accident-related PTSD help to qualify the severity of problematic driving behavior in trauma-exposed veterans.
Keywords: Driving anxiety, Driving behavior, Military veterans, Posttraumatic stress disorder, Assessment
1. Introduction
Motor vehicle collisions are identified as the leading cause of accidental death in military veterans (U.S. Department of Veterans Affairs, 2009) with multiple studies suggesting elevated risk in former service members relative to the population as a whole (e.g., Bullman et al., 2017; Lincoln et al., 2006; Watanabe & Kang, 1996; but see Kang & Bullman, 1996). Veteran status is also associated with an increase in the occurrence of traffic violations and non-fatal accidents (e.g., Amick, Kraft, & McGlinchey, 2013). Difficulties with travel-related hypervigilance, disorientation, and aggression are shown to be further elevated in service members with symptoms of posttraumatic stress (Classen et al., 2017; Kuhn, Drescher, Ruzek, & Rosen, 2010; Lew et al., 2011), placing this population at greater risk for negative social, health, and financial outcomes associated with collisions and repeated citations (e.g., Hickling, Blanchard, Silverman, & Schwarz, 1992; Mayou, Bryant, & Ehlers, 2001; Possis et al., 2014). Despite recognition as a significant veteran health issue (Hwang, Peyton, Kim, Nakama-Sato, & Noble, 2014; Possis et al., 2014; Zinzow, Brooks, & Stem, 2013), few measures have been validated to assess problematic driving in former military. The aim of the current study was to examine the psychometric properties of the Driving Behavior Survey – a measure of anxiety-related driving behavior – in veterans completing a larger study involving the treatment of posttraumatic stress disorder (PTSD; Sloan, Unger, Lee, & Beck, 2018).
Evidence of morbidity, accident risk, and global impairment as a result of negative traffic events has triggered interest in identifying factors associated with problematic driving in current and former service members (e.g., Hwang et al., 2014; Lew et al., 2011; Possis et al., 2014; Zinzow et al., 2013). Much of the existing work in this area targets the role of negligent or impulsive behaviors such as speeding, disregarding traffic laws, failing to utilize safety restraints, and driving under the influence of alcohol or substances (e.g., Fear et al., 2008; Hoggatt et al., 2015; Sheppard & Earleywine, 2013). Behavior in these domains is often attributed to a greater propensity for risk taking in individuals self-selecting for military service as well as perceptions of “invincibility” in combat-deployed veterans. Aspects of formal military training are also seen as a potential contributing factor. Lew, Amick, Kraft, Stein, and Cifu, 2010; 2011) note that military personnel receive formal instruction in evasive driving techniques (e.g., traveling at high speeds; maintaining distance from other vehicles; executing unpredictable maneuvers) that are critical to survival during active duty. Post-deployment interventions such as Battlemind Training and Battlemind Debriefing (Adler, Bliese, McGurk, Hoge, & Castro, 2009; Adler, Castro, & McGurk, 2009; Castro, Hoge, & Cox, 2006) include modules developed to highlight the dangers of combat-oriented driving in civilian settings. Still, difficulty inhibiting overlearned tactical behaviors may underlie some aspects of problematic driving in this population.
Mental health difficulties including anxiety, depression, and PTSD are an additional set of factors thought to contribute to driving-related impairment. Trauma-related symptoms, in particular, have been linked to a variety of negative behaviors. Zinzow et al. (2013) found that service members with PTSD were more likely to acknowledge changes in post-deployment driving (95%) as compared to those with no diagnosis (70%). Elevations in travel anxiety and driving-related hypervigilance also were noted in service members with PTSD. Lew et al. (2011) similarly found that post-9/11 conflict veterans with diagnoses of PTSD were more likely to acknowledge becoming lost or disoriented during post-deployment travel than were non-PTSD controls. Deficits observed in driving simulation research offer convergent evidence of self-reported difficulties in service members with PTSD (Amick et al., 2013; Classen et al., 2017). Finally, existing data offers robust support for associations between trauma-related symptoms and self-reported driving-related anger and aggression (e.g., Kuhn et al., 2010; Lew et al., 2011). Problematic behavior in this domain includes frustration, irritability, verbal outbursts, aggressive gesturing, and other hostile acts (e.g., tailgating, cutting off other motorists).
Recognition of these difficulties has prompted the development of treatment packages targeting maladaptive driving in former service members (e.g., Classen et al., 2017; Strom et al., 2013). Research is complicated, however, by a lack of validated measures targeting problematic driving in this population. Review of the literature indicates that the majority of existing studies employ project-specific measures and/or single item scales isolating particular behaviors of interest. Whereas face-valid/single-item instruments can be effective, the psychometric characteristics of project-specific scales remain untested, and the idiosyncratic nature of assessment limits meaningful comparisons across studies. Established measures or scales derived from validated instruments are used in some research, although phenomena captured in these assessments generally target only a subset of problematic behavior (e.g., driving anger; Hwang et al., 2014; Strom et al., 2013). Whipple, Schultheis, and Robinson (2016)) begin to fill gaps in this literature with the introduction of the Veteran Driving Questionnaire (VDQ). Initial scale development examines situational anxiety, driving behaviors, and affective states in a small sample of well-adjusted veterans and veterans with comorbid brain injury and PTSD. Preliminary work with the VDQ is promising although the specification of post-deployment driving behavior (i.e., “driving habits since returning home from deployment”) complicates administration in non-deployed military. The length of the measure (81 items across situational anxiety, driving behavior, and affective scales) may also limit use of the full VDQ in routine clinical settings.
The Driving Behavior Survey (DBS; Clapp et al., 2011) is an alternate measure that may address gaps in the current veteran driving literature. The DBS is a brief, self-report instrument developed to evaluate the occurrence of anxiety-related driving behavior. Anxious driving behavior, as operationalized for the purpose of the scale, refers to any increase, decrease, or general disorganization of behavior occurring as a result of anxiety during the operation of a motor vehicle (Clapp et al., 2011). Item generation for the DBS was informed by existing research (e.g., Taylor, Deane, & Podd, 2007), empirical reviews (e.g., Taylor, Deane, & Podd, 2002; Taylor & Koch, 1995), treatment protocols (e.g., Antony, Craske, & Barlow, 2006; Blanchard & Hickling, 2004), standardized driving assessments (e.g., Practical Driving Assessment), and developers’ experience with the assessment and treatment of driving-related anxiety (Beck, Coffey, Foy, Keane, & Blanchard, 2009; Clapp, Masci, Bennett, & Beck, 2010; Grant, Beck, Marques, Palyo, & Clapp, 2008).
Development of the DBS across independent samples of civilian motorists identified three domains of anxious behavior (Clapp et al., 2011). Anxiety-based performance deficits target problematic behaviors including difficulty maintaining lane position, sudden or inappropriate adjustments in speed, and impaired execution of basic traffic operations. Deficits are believed to stem from state-level cognitive interference, with heightened anxiety overwhelming resources necessary for the completion of driving-related tasks (e.g., monitoring speed, direction, and vehicle position; Taylor, Deane, & Podd, 2008). DBS performance deficits demonstrate reliable associations with travel-related fear as well as measures of clinical depression (Clapp et al., 2011; Clapp, Baker, Litwack, Sloan, & Beck, 2014). Behaviors on this scale closely resemble difficulties with orientation, attention, and performance linked to PTSD in the larger veteran driving literature (e.g., Amick et al., 2013; Lew et al., 2011).
Exaggerated safety and/or excessively cautious behavior include strategies intended to amplify perceptions of safety and/or situational control (e.g., maintaining excessive distances from other motorists, driving far below the posted speed limit, reducing speed before progressing through intersections). While effective in managing immediate distress, excessively cautious behavior is likely to violate routine traffic norms, placing anxious drivers at increased risk for negative traffic events (e.g., accidents, near collisions). Exaggerated compensatory behaviors are frequently noted in clinical settings (e.g., Antony et al., 2006; Taylor & Koch, 1995) with DBS safety/caution demonstrating concurrent associations with measures of driving anxiety and overt travel avoidance (Clapp et al., 2011).
Anxiety-based hostility and driving aggression targets behavioral indicators of fear-based aggression. While impairment associated with global driving anger has received broad clinical attention (e.g., Deffenbacher, Huff, Lynch, Oetting, & Salvatore, 2000; Del Vecchio & O’Leary, 2004), interest in anxiety-specific aggression is more recent. Problematic behavior in this domain (e.g., shouting, honking, aggressive gesturing) is thought to reflect a lowered threshold for aggressive responding as a result of traffic-related anxiety. DBS hostile/aggressive scores demonstrate expected associations with accident fear, travel avoidance, PTSD, and global driving anger (Clapp et al., 2011, 2014). Although specific to anxiety-focused reactions, items on this scale closely resemble aggressive behaviors noted in some veteran drivers (e.g., Lew et al., 2011; Possis et al., 2014).
The psychometric characteristics of DBS scales have been previously examined in student drivers (Clapp et al., 2011) and in treatment-seeking adults with motor vehicle accident (MVA)-related PTSD (Clapp et al., 2014). Reductions in performance deficit, exaggerated safety/caution, and hostile/aggressive scales in survivors receiving exposure-based treatment for PTSD offer additional support for the viability of the DBS as a clinical outcome measure (Baker, Litwack, Clapp, Beck, & Sloan, 2014). Aims of the current study were to examine the factorial, concurrent, discriminant, and discriminative validity of DBS scores in veterans participating in a group-based treatment for PTSD (Sloan et al., 2018). For these data, confirmatory factor analyses were used to assess the global fit of a 3-factor model previously identified in student motorists (Clapp et al., 2011). Concurrent associations were examined through bivariate correlations with indices of PTSD, anxiety, and depression. Correlations between performance deficit and depression scores were expected to be particularly strong based on effects noted in prior clinical research (Clapp et al., 2014). Associations with cumulative trauma history were also examined given links between driving difficulties and exposure severity in the larger veteran literature (e.g., Hoggatt et al., 2015; Lew et al., 2011). Discriminant relations were assessed through correlations with dissimilar constructs including reading performance and gross cognitive impairment. Evidence for the discriminative validity of DBS scales was assessed via comparisons with data from published validation samples. Specifically, veterans were expected to report safety/caution, performance deficit, and hostile/aggressive behaviors at a greater frequency than university students surveyed in the original development research (Clapp et al., 2011). By contrast, veteran scores were expected to be similar to those observed in community members receiving exposure-based treatment for MVA-related PTSD (Clapp et al., 2014).
2. Materials and methods
2.1. Participants
2.1.1. Veteran sample
Participants included 160 male veterans participating in research evaluating the efficacy of a cognitive-behavioral, group-based intervention for PTSD (Sloan et al., 2018). Participants were recruited at two VA medical centers through clinic referrals and flyers posted at each facility. Inclusion criteria required participants to be male, at least 18 years of age, and hold a primary diagnosis of PTSD as specified in DSM-5 (American Psychiatric Association, 2013). Exclusion criteria included evidence of psychosis, current diagnoses of substance dependence, unstable bipolar disorder, and English illiteracy. Veterans currently engaged in psychosocial treatment for PTSD were also excluded.
Investigators were contacted by a total of 307 individuals. Of these, 74 did not qualify based on responses to a preliminary phone screen. Of the 223 individuals consented for initial assessment, 23 did not meet inclusion criteria, 11 declined to continue with the study, and 1 was not a veteran. One hundred and ninety-eight participants were randomized either to a group therapy or active control condition. Of these, 38 failed to identify as current drivers and were excluded from the current analyses.
Veterans in the final sample (N = 160) reported an average age of 56.4 years (SD = 12.3). Participants identified predominantly as White (76.3%) and Non-Hispanic/Latino (94.4%). Nearly three-quarters of the sample indicated at least some level of college or vocational training (74.4%). Roughly equal proportions reported full- or part-time employment (44.4%) or receiving retirement/disability support (41.9%). Three quarters of veterans identified combat exposure as the index trauma during the subsequent assessment of PTSD. Full demographic characteristics are presented in Table 1.
Table 1.
Sample Characteristics (N = 160).
| Age | M = 56.4 | SD = 12.3 |
|---|---|---|
| Race | ||
| White | 122 | 76.3% |
| Black/African American | 25 | 16.7% |
| Other | 13 | 8.1% |
| Ethnicity | ||
| Hispanic or Latino | 9 | 5.6% |
| Education | ||
| ≤ High School | 41 | 25.6% |
| Some college/vocation | 83 | 51.9% |
| College degree | 19 | 11.9% |
| Graduate coursework | 17 | 10.6% |
| Employment | ||
| Full-time | 51 | 31.9% |
| Part-time | 20 | 12.6% |
| Unemployed | 14 | 8.8% |
| Retired/Disability | 67 | 41.9% |
| Student | 3 | 1.9% |
| Service | 2 | 1.3% |
| Index Trauma | ||
| Combat/Warfare | 120 | 75.0% |
| Death or Violence to a Loved One | 9 | 5.6% |
| Physical Assault | 5 | 3.1% |
| Sexual Assault | 4 | 2.5% |
| Motor Vehicle Accident | 2 | 1.3% |
| Other Accident/Disaster | 11 | 6.9% |
| Other | 5 | 3.1% |
2.1.2. Student development sample
The student sample (N = 515) was composed of college-aged motorists participating in the original development research for the DBS (see Clapp et al., 2011; Samples 2 & 3). Roughly half of participants were male (54.4%) with a mean age of 19 (SD = 1.7). Students were predominantly White/Non-Hispanic (79.2%) with 7.0% identifying as Black/Non-Hispanic, 8.0% as Asian, and 1.9% as White/Hispanic. Less than half of the sample (42.7%) reported prior involvement in a traffic collision.
2.1.3. MVA-related PTSD sample
The MVA sample (N = 40) included community members participating in research evaluating the efficacy of a brief, exposure-based intervention for PTSD (see Baker et al., 2014; Clapp et al., 2014; Sloan, Marx, Bovin, Feinstein, & Gallagher, 2012). Participants were predominantly female (62.5%) with a mean age of 41 (SD = 13.3). The sample was ethnically diverse with participants identifying as White/Non-Hispanic (35.0%), Black/Non-Hispanic (37.5%), White/Hispanic (10.0%), and Other (17.5%). Educational background was similarly represented across individuals completing high school (20.0%), some college (37.5%), Bachelor-level degrees (20.0%), and graduate-level coursework (22.5%). Sixty percent of participants reported some level of employment (full or part-time). Average duration from the criterion MVA was 35.5 months (SD = 48.3). All participants in the MVA sample met DSM-IV (American Psychiatric Association, 1994) criteria for PTSD.
2.2. Procedure
Informed consent was obtained from veterans in the larger treatment study upon their arrival for initial assessment. Participants then completed a series of self-report measures and semi-structured clinical interviews. Interviews were conducted by advanced doctoral students, under close supervision by a doctoral-level psychologist. All assessments were recorded with approximately 20% (n = 33) of cases selected for independent review. All procedures received approval from relevant Institutional Review Boards.
2.3. Measures
2.3.1. Driving Behavior Survey (DBS)
The DBS (Clapp et al., 2011) is a 21-item scale indexing the frequency of anxious driving behavior across three domains: exaggerated safety/caution behavior, anxiety-based performance deficits, and hostile/aggressive behavior. Items are rated on a 1 (never) to 7 (always) Likert-type scale with scores calculated as the mean of endorsed scale items. Higher scores indicate greater frequency of anxious driving behavior within a given domain. Evidence of factorial validity and convergent associations are provided by Clapp et al. (2011). Estimates of internal consistency range from good to excellent in both college-aged drivers (αDeficit = .77–.80; αCaution = .75–.78; αAggression = .86–.87; Clapp et al., 2011) and help-seeking MVA survivors (αDeficit = .93; αCaution = .93; αAggressive = .85; Clapp et al., 2014). Four-week (rxxDeficit = .61; rxxCaution = .68; rxxAggression = .89) and 12-week (rxxDeficit = .85; rxxCaution = .80; rxxAggression = .80) test-retest reliabilities were acceptable in development and MVA samples, respectively. Baker et al. (2014) provide evidence of treatment sensitivity as evidenced by pre- to post-treatment reductions in DBS scores in individuals receiving treatment for MVA-related PTSD.
2.3.2. Clinician-Administered PTSD Scale for DSM-5 (CAPS-5)
The CAPS-5 (Weathers et al., 2013) was used to determine eligibility for the larger study and to derive continuous indices of PTSD symptom severity. CAPS-5 items correspond to the cardinal indicators of PTSD as specified in DSM-5 (American Psychiatric Association, 2013). Symptoms are rated on a 0–4 Likert-type scale with total severity computed as the sum of item ratings (range: 0–80). Continuous measures of Intrusion (range: 0–20), Avoidance (range: 0–8), Alterations in Cognitions and Mood (range: 0–28), and Alterations in Arousal and Reactivity (range: 0–24) were calculated as item totals for each symptom cluster. Weathers et al. (2018) provide evidence for the internal consistency, reliability, and construct validity of the CAPS-5 in military veterans. Interrater reliability of CAPS total scores in the current sample was good (ICC = .80).
2.3.3. Beck Anxiety Inventory (BAI)
The BAI (Beck, Epstein, Brown, & Steer, 1988) is a 21-item self-report measure of anxiety-related somatic arousal and subjective distress. Items are rated on a 0–3 Likert scale and summed to form a continuous index of anxiety severity (range: 0–63). Interpretive guidelines identify scores from 0 to 7, 8–15, 16–25, and 26–63 as consistent with minimal, mild, moderate, and severe symptoms of anxiety, respectively (Beck & Steer, 1993). Existing research provides strong evidence for reliability and construct validity of scores (e.g., Beck et al., 1988; deBeurs, Wilson, Chambless, Goldstein, & Feske, 1997). Internal consistency of the BAI in this sample was excellent (α = .92).
2.3.4. Beck Depression Inventory-II (BDI-II)
The BDI-II (Beck, Steer, & Brown, 1996) is a 21-item self-report measure targeting symptoms of clinical depression. Items are rated on a 0–3 Likert scale and summed to form a continuous severity sore. Values ranging from 0 to 13, 14–19, 20–28, and 29–63 serve as benchmarks for minimal, mild, moderate, and severe symptoms of depression (Beck et al., 1996). Extensive research with the BDI-II provides strong evidence for the reliability and construct validity of scores (Beck et al., 1996; Quilty, Zhang, & Bagby, 2010). Internal consistency of BDI-II scores in the current sample was high (α = .93).
2.3.5. Traumatic Life Events Questionnaire (TLEQ)
The TLEQ (Kubany et al., 2000) is a self-report checklist developed to document exposure to 22 potentially traumatic events. To account for greater severity as a result of multiple exposures, respondents indicate the number of lifetime occurrences for each event on a 7-point Likert scale (0 = never to 6 = more than 5 times). For the current project, cumulative trauma history was operationalized as the sum of ratings across TLEQ domains. Development research with the TLEQ provides evidence for the temporal stability of reported events as well as convergence across self-report and interview-based administrations (Kubany et al., 2000).
2.3.6. Montreal Cognitive Assessment (MoCA)
The MoCA (Nasreddine et al., 2005) is a brief mental state examination developed to identify symptoms of mild cognitive impairment. Respondents complete a series of tasks targeting eight domains of basic cognitive functioning. Scores ≤ 20 out of a possible 30 are recommended for the identification of probable impairment in help-seeking veterans (Waldron-Perrine & Axelrod, 2012). The MoCA demonstrates positive psychometric properties in existing research with several studies indicating superior performance to traditional mental state examinations (e.g., Nasreddine et al., 2005; Pendlebury, Cuthbertson, Welch, Mehta, & Rothwell, 2010; Smith, Gildeh, & Holmes, 2007).
2.3.7. Wide Range Achievement Test 4 (WRAT-4)
The reading subtest of the WRAT-4 (Wilkinson & Robertson, 2006) was incorporated as a discriminant measure of letter and word decoding. For this subtest, respondents pronounce a list of increasingly obscure words of increasing phonological complexity. WRAT-4 reading scores demonstrate evidence of internal consistency and alternate-form reliability (Wilkinson & Robertson, 2006). Correlations with raw reading scores were examined for the current analyses.
2.4. Analytic approach
2.4.1. Factorial validity
Confirmatory factor analyses were used to assess fit of the DBS 3-factor model specified in development research by Clapp et al. (2011). Correlated performance deficit, safety/caution, and hostile/aggressive factors were identified by a unique set of seven indicators (see Table 2 for specific scale items). An error covariance between items 1 (I lose track of where I’m going) and 9 (I forget where I am driving to) was specified a priori, consistent with the final model reported by Clapp et al.
Table 2.
Factor Loadings, Communalities, Observed Score Descriptives, and Factor Correlations for the Confirmatory 3-Factor Modela.
| λ | h2 | M | SD | |
|---|---|---|---|---|
| Anxiety-Based Performance Deficits (DEF) | 2.23 | 1.02 | ||
| I have trouble finding the correct lane (dbs14) | 0.69 | 0.48 | 1.73 | 1.21 |
| I lose track of where I’m going (dbs1) | 0.48 | 0.23 | 2.92 | 1.51 |
| I have trouble staying in the correct lane (dbs4) | 0.80 | 0.64 | 1.82 | 1.24 |
| I drift into other lanes (dbs5) | 0.89 | 0.79 | 1.78 | 1.17 |
| I forget to make appropriate adjustments in speed (dbs6) | 0.57 | 0.32 | 2.43 | 1.57 |
| I forget where I am driving to (dbs9) | 0.50 | 0.25 | 2.60 | 1.55 |
| I have difficulty merging into traffic (dbs21) | 0.59 | 0.35 | 2.32 | 1.50 |
| Exaggerated Safety/Excessively Cautious Behavior (CAUT) | 4.39 | 1.17 | ||
| I maintain a large distance between myself and the driver in front of me (dbs8) | 0.67 | 0.45 | 4.67 | 1.66 |
| I slow down when approaching intersections even when the light is green (dbs3) | 0.45 | 0.20 | 4.06 | 1.70 |
| I try to put distance between myself and other cars (dbs11) | 0.82 | 0.67 | 4.74 | 1.67 |
| I maintain my speed in order to calm myself down (dbs12) | 0.52 | 0.27 | 4.16 | 1.70 |
| I try to stay away from other cars (dbs13) | 0.74 | 0.55 | 4.65 | 1.82 |
| I decrease my speed until I feel comfortable (dbs16) | 0.51 | 0.26 | 3.23 | 1.77 |
| During bad weather, I drive more cautiously than other vehicles on the road (dbs19) | 0.46 | 0.21 | 5.14 | 1.75 |
| Anxiety-Based Hostility and Driving Aggression (ANG) | 3.38 | 1.61 | ||
| I make gestures at the driver/drivers who made me nervous (dbs10) | 0.93 | 0.86 | 3.25 | 2.02 |
| I yell at the driver/drivers who made me nervous (dbs2) | 0.75 | 0.56 | 4.10 | 1.76 |
| I let the driver who made me nervous know that I am upset (dbs7) | 0.92 | 0.84 | 3.55 | 1.95 |
| I pound on the steering wheel when I am nervous (dbs15) | 0.62 | 0.39 | 2.47 | 1.85 |
| I honk my horn at the driver who made me nervous (dbs17) | 0.81 | 0.66 | 3.39 | 2.10 |
| I try to find ways to let other drivers know that they are making me nervous (dbs18) | 0.82 | 0.67 | 2.96 | 1.97 |
| I swear/use profanity while I am driving (dbs20) | 0.76 | 0.57 | 3.96 | 1.88 |
| Factor Variances, Covariances, and Correlationsa | DEF | CAUT | ANG | |
| DEF | 0.689 | 0.241 | 0.490 | |
| CAUT | 0.261 | 1.240 | 0.224 | |
| ANG | 0.317 | 0.108 | 3.469 |
Note: λ = standardized factor loadings; h2 = communalities; Error covariance between dbs1 and dbs9 was estimated as cov = 1.31 (r = .74).
Diagonal contains factor variances (in bold); upper triangle contains covariances; lower triangle contains latent correlations; association between DEF & CAUT and DEF & ANG scales are significant at p ≤ .003.
Confirmatory analyses were evaluated in MPlus 8.1 using maximum likelihood (ML) estimation. Of relevance to the current study, Herzog, Boomsma, and Reinecke (2007) note that the ML chi-square statistic forming the basis for most indices of global fit is positively biased for N ≤ 400, resulting in the systematic overrejection of otherwise acceptable models. Simulation research by Herzog et al. indicates that incorporation of a Swain correction to may address these biases given adequate performance of in models with sample-to-parameter ratios as low as 2:1 (Herzog & Boomsma, 2009; Herzog, Boomsma, & Reinecke, 2007). Based on these recommendations, the plausibility of the hypothesized 3-factor model was assessed using and adjusted indices of fit.
Swain-corrected values for the root-mean-square of approximation (RMSEA), comparative fit index (CFI), and Tucker-Lewis index (TLI) were evaluated as indicators of global fit (Herzog & Boomsma, 2009). Uncorrected values for the standardized root-mean-square residual (SRMR) – which is not derived from – were also examined. For these data, RMSEA ≤ .08, SRMR ≤ .10, and CFI and TLI ≥ .90 served as criterion for adequate model fit (Bentler, 1990; Browne & Cudeck, 1993; Kline, 2011). RMSEA ≤ .06, SRMR ≤ .08, and CFI and TLI ≥ .95 were interpreted as evidence of close fit (Hu & Bentler, 1999).
2.4.2. Convergent and discriminant validity
Convergent (PTSD, anxiety, depression, cumulative trauma) and discriminant (cognitive impairment, reading) relations were calculated as Pearson correlations with 95% confidence intervals for safety/caution, performance deficit, and hostile/aggressive scales. Cohen’s (1988) benchmarks for small (r = .10), medium (r = .30), and large (r = .50) effects were used to qualify the magnitude of correlations between DBS scales and external measures.
2.4.3. Discriminative validity
The discriminative validity of DBS scores was examined through comparisons with published data for non-clinical college and help-seeking MVA samples. Discrepancies in the severity of anxious driving behaviors were evaluated in a series of independent-samples t-tests. Effect sizes and 95% confidence intervals for means-based comparisons are reported as Cohen’s d (small = .20, medium = .50, large = .80; Cohen, 1988).1
3. Results
3.1. Factorial validity
Confirmatory analysis provided evidence of adequate model fit with indices similar to those observed in the original development sample ( = 359.7; = 341.3; CFIS = .91; TLIS = .90; RMSEAS = .07, 90% CI [.06, .08]; SRMR = .09).2 All indicators demonstrated salient loadings across respective performance deficit, safety/caution, and hostile/aggressive factors (λ ≥ .45; see Table 2). Corresponding communality estimates verify that the 3-factor model accounted for substantial variability in the frequency of individual driving behaviors (h2 = .20–.86). Small to medium correlations were observed between latent DBS factors (rDEF◦CAUT = .26; rDEF◦ANG = .32; rCAUT◦ANG = .11).
3.2. Internal consistency and scale correlations
Mirroring results of the structural analyses, internal consistencies ranged from good to excellent for performance deficit (α = .85), safety/caution (α = .79), and hostile/aggressive (α = .93) dimensions. Moderate to near-null correlations were noted across observed scores for each scale (rDEF◦CAUT = .22, p = .006; rDEF◦ANG = .41, p < .001; rCAUT◦ANG = .07, p = .350).
3.3. Concurrent and discriminant relations
Correlations and 95% confidence intervals for associations with PTSD severity, anxiety, depression, cumulative trauma history, cognitive impairment, and reading performance are provided in Table 3. DBS performance deficits demonstrated small to moderate associations with total CAPS severity, PTSD symptom clusters, and cumulative trauma history. Correlations with measures of anxiety and depression fell in the medium to large range with elevations relative to corresponding associations for safety/caution and hostile/aggressive scales.
Table 3.
Correlations, 95% Confidence Intervals, and Descriptive Statistics for Clinical Measures.
| DEF | CAUT | ANG | M | SD | ||||
|---|---|---|---|---|---|---|---|---|
| CAPS-5 | .400*** | [.26, .52] | .201* | [.05, .35] | .365*** | [.22, .49] | 39.99 | 9.43 |
| - Intrusions | .223** | [.07, .37] | .089 | [−.07, .24] | .203** | [.05, .35] | 9.73 | 2.86 |
| - Avoidance | .241** | [.09, .38] | .032 | [−.12, .19] | .166* | [.01, .31] | 5.08 | 1.40 |
| - Cognition-Mood | .337** | [.19, .47] | .203* | [.05, .34] | .258** | [.11, .40] | 14.04 | 4.76 |
| - Arousal-Reactivity | .362** | [.22, .49] | .190* | [.04, .34] | .422** | [.29, .54] | 11.15 | 3.31 |
| Trauma History | .182* | [.03, .33] | −.045 | [−.20, .11] | .191* | [.04, .34] | 29.55 | 15.45 |
| BAI | .526** | [.40, .63] | .240** | [.09, .38] | .370** | [.23, .50] | 19.89 | 11.72 |
| BDI-II | .451** | [.32, .57] | .177* | [.02, .32] | .310** | [.16, .44] | 24.54 | 11.78 |
| MoCA | −.145 | [−.29, .01] | .009 | [−.15, .16] | −.019 | [−.17, .14] | 25.68 | 2.49 |
| WRAT-4 Reading | .043 | [−.11, .20] | .029 | [−.13, .18] | .066 | [−.09, .22] | 60.08 | 5.66 |
Note: DEF = Driving Behavior Survey (DBS) performance deficits; CAUT = DBS exaggerated safety/caution; ANG = DBS hostile/aggressive behavior; CAPS-5 = Clinician-Administered PTSD Scale for DSM-5 total scores; BAI = Beck Anxiety Inventory; BDI-II = Beck Depression Inventory-II; Trauma History = Traumatic Life Events Questionnaire total exposures; MoCA = Montreal Cognitive Assessment; WRAT Reading = Wide Range Achievement Test 4 Reading subtest (raw scores).
p ≤ .05.
p ≤ .01.
p ≤ .001.
Exaggerated safety/caution demonstrated small to medium associations with CAPS total, Cognition-Mood, and Arousal-Reactivity scales although absolute correlations were weaker than those for DBS performance deficits. Results failed to provide evidence of reliable associations with Intrusions, Avoidance, and overall trauma history. Correlations with anxiety and depression fell in the small to medium range.
Associations of hostile/aggressive scores with CAPS total, symptom clusters, and cumulative trauma history were similar to those noted for anxiety-based performance deficits although the correlation with PTSD Arousal-Reactivity was elevated for hostile/aggressive behavior. Concurrent relations with anxiety and depression fell in the small to medium range.
Consistent with hypotheses, data failed to support reliable associations with discriminant measures of cognitive impairment and general reading ability. A marginal relation was noted, however, between anxiety-based performance deficits and cognitive impairment assessed by the MoCA (p = .067).
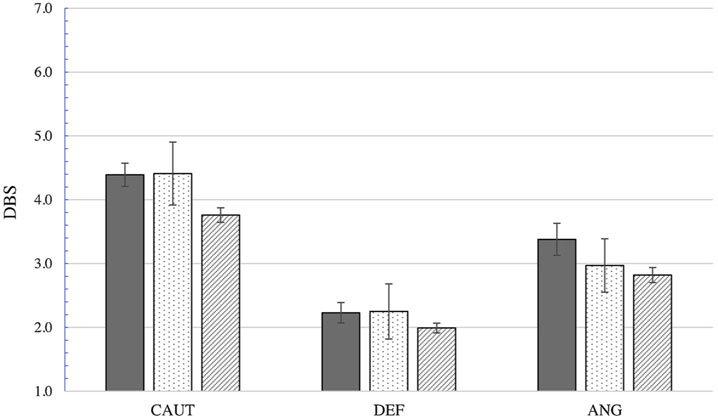
3.4. Discriminative validity
Comparisons with published data collected from student motorists and community members with MVA-related PTSD are illustrated in Fig. 1. As expected, veterans in the current sample reported greater frequency of performance deficit (p = .001; d = .29, CI95 [.11, .47]), exaggerated safety/caution (p < .001; d = .53, CI95 [.35, .71]), and hostile/aggressive behavior (p < .001; d = .51, CI95 [.33, .68]) than student drivers in the initial development sample. Behavior was comparable across veterans and community survivors with MVA-related PTSD (performance deficits: p = .918; d = .02, CI95 [−.32, .36]; safety/caution: p = .928; d = .02 CI95 [−.33, .36]; hostile/aggressive behavior: p = .138; d = .26, CI95 [−.08, .61]).
Fig. 1.
Driving Behavior Survey (DBS) scores and 95% confidence intervals for clinical and non-clinical samples. CAUT = DBS excessive safety/caution behaviors; DEF = DBS anxiety-based performance deficits; ANG = DBS hostile/aggressive driving behavior.
 Veteran PTSD (N = 160): CAUT (M = 4.39, SD = 1.17); DEF (M = 2.23, SD = 1.02); ANG (M = 3.38, SD = 1.61).
Veteran PTSD (N = 160): CAUT (M = 4.39, SD = 1.17); DEF (M = 2.23, SD = 1.02); ANG (M = 3.38, SD = 1.61).
 Motor vehicle accident PTSD sample from Clapp et al. (2014; N = 40): CAUT (M = 4.41, SD = 1.54); DEF (M = 2.25, SD = 1.35); ANG (M = 2.97, SD = 1.31).
Motor vehicle accident PTSD sample from Clapp et al. (2014; N = 40): CAUT (M = 4.41, SD = 1.54); DEF (M = 2.25, SD = 1.35); ANG (M = 2.97, SD = 1.31).
 Unselected student sample from Clapp et al. (2011; N = 518): CAUT (M = 3.88, SD = 0.89); DEF (M = 2.00, SD = 0.70); ANG (M = 2.74, SD = 1.14).
Unselected student sample from Clapp et al. (2011; N = 518): CAUT (M = 3.88, SD = 0.89); DEF (M = 2.00, SD = 0.70); ANG (M = 2.74, SD = 1.14).
4. Discussion
Problematic driving behavior in former service members has gained increasing attention as a public health issue given the potential impacts on mortality, physical and emotional well-being, and overall adaptive functioning (e.g., Hwang et al., 2014; Lew et al., 2011; Possis et al., 2014; Zinzow et al., 2013). The current study of help-seeking veterans with PTSD looked to examine the characteristics of a brief measure of anxious driving behavior previously validated in civilian motorists. Results suggest the structural properties of DBS scales are remarkably consistent across discrepant populations. Confirmatory analysis indicated support for the 3-factor model specified by Clapp et al. (2011) with fit indices nearly identical to those in the initial sample of student drivers. Factor loadings were also similar, although trends were noted for stronger associations of performance deficit and hostile/aggressive indicators with their respective factors in veteran (DEF: ; ANG: ) versus student (DEF: ; ANG: ) respondents. Factor and observed scale correlations both provide support for DBS dimensions as distinct domains of problematic driving. Internal consistencies were also strong and comparable to those reported in prior validation samples (Clapp et al., 2011, 2014). The only notable discrepancy in this pattern was a stronger estimate of internal consistency for DBS safety/caution in MVA survivors with PTSD (α = .93) relative to veterans in the current sample (α = .79). Greater interrelatedness of safety/caution items among MVA survivors is not entirely unexpected given the functional relation between accident exposure and specific changes in exaggerated driving safety.
Concurrent relations provide additional support for the construct validity of DBS scales in veterans with PTSD. Specifically, anxiety-based performance deficits demonstrated small to medium correlations with cumulative trauma history, CAPS-5 severity, and PTSD symptom dimensions. Analyses also indicated moderate to large associations with clinical measures of anxiety and depression. The strength of the convergent relation with depression, combined with the prominence of this association in previous research (i.e., Clapp et al., 2014), is consistent with the conceptualization of performance deficits occurring as a result of cognitive demands associated with rumination and heightened anxiety. These data, as well as others demonstrating associations between anxiety and impaired driving performance (e.g., Amick et al., 2013; Lew et al., 2011; Matthews et al., 1998; Taylor et al., 2007), suggest that anxiety management or other emotion regulation techniques could be used to augment existing driving-focused interventions (e.g., Classen et al., 2017).
DBS hostile/aggressive behaviors also produced a robust pattern of convergent relations with anxiety, depression, trauma history, CAPS-5 severity, and PTSD symptom dimensions. The absolute magnitude of correlations were somewhat smaller than those observed for performance deficit scores with a notable exception in the association with Arousal-Reactivity. The modest increase in the relation with hostile/aggressive driving behavior is relevant given the introduction of aggressive (E1) and impulsive (E2) behaviors as cardinal symptoms of PTSD in DSM-5. The prominence of this association is consistent with meta-analytic research demonstrating links between posttrauma symptoms and measures of anger/hostility among military samples (Orth & Wieland, 2006). Overlap between DBS hostile/aggressive items and behaviors noted in the larger veteran driving literature (e.g., Kuhn et al., 2010; Lew et al., 2011) offers additional evidence for the potential utility of the DBS in this population.
Concurrent associations with exaggerated safety/caution scores were modest relative to those for performance deficit and hostile/aggressive scales. However, correlations with anxiety, depression, Cognition-Mood, Arousal-Reactivity, and PTSD symptom severity did provide evidence of greater caution in veterans reporting elevated levels of psychopathology. Lack of support for an association between DBS safety/caution scores and CAPS-5 Avoidance was unexpected, however, given the conceptualization of exaggerated safety as a form of avoidant coping behavior (Clapp et al., 2011). For these data, the failure of trauma-specific avoidance (i.e., avoidance thoughts and feelings [C1]; avoidance of people, places, activities [C2]) to correlate with the frequency of excessive driving safety could be attributable to the specification of non-accident trauma by the majority of veterans in this sample. It is also possible that excessive driving safety reported in the current study was due, in part, to overlearned tactical behaviors continuing post-deployment. For many participants, a preoccupation with managing speed and maintaining distance from other vehicles could be tied more closely to military training than to trauma-specific symptoms. Information regarding veterans’ driving history during service (e.g., duties involving the operation of motor vehicles, history of driving-related incidents during deployment) was not collected as part of the larger treatment study (Sloan et al., 2018). Continued research exploring a more inclusive set of contributing factors would be helpful in understanding elevated levels of exaggerated safety and excessive caution in veteran drivers.
Formal comparison with existing psychometric samples produced expected differences across clinical and non-clinical populations. Consistent with hypotheses, veterans with a diagnosis of PTSD reported performance deficits, exaggerated safety/caution, and hostile/aggressive driving behavior at a greater frequency than student motorists sampled for the development of the DBS (Clapp et al., 2011). Confidence intervals for Cohen’s d suggest small to medium effects for differences in anxious driving behavior across veteran and student populations. Although discrepancies in the endorsement of performance deficits were somewhat modest, the increased occurrence of anxiety-related errors in former service members is notable given the comparison against a younger and considerably less experienced group of drivers. Performance deficit and exaggerated safety/caution scores were functionally identical across clinical samples although veterans did show a small, but statistically non-significant, elevation in hostile/aggressive driving relative to community survivors of MVA. Similarities suggest the DBS may hold promise as a marker of functional impairment in veterans with PTSD.
Interpretation of results should be made within the context of the study’s strengths and limitations. These data, along with preliminary work by Whipple et al. (2016), are among the first to examine the characteristics of a structured driving measure in a sample of former service members. The availability of a large clinical dataset and the incorporation of gold-standard, interview-based measures of PTSD are notable strengths of the project. It is important to acknowledge, however, that participants in this study were restricted to military veterans with a current diagnosis of PTSD. Again, evidence of near identical fit in this sample relative to college-aged motorists (Clapp et al., 2011) provides compelling support for the factorial validity of the DBS. However, in the absence of a reference sample of service members with no psychiatric diagnoses, it is unclear whether corresponding elevations in anxious driving behavior are attributable to veteran status, PTSD diagnosis, or some combination of these. The larger veteran driving literature has identified a number of trait- (e.g., impulsivity, sensation seeking), environmental- (e.g., deployment history, tactical training), and health- (e.g., chronic pain, traumatic brain injury) related factors that could contribute to increased risk in current and former service members (e.g., Hoggatt et al., 2015; Hwang et al., 2014; Lew et al., 2010; Possis et al., 2014). Although mental health symptoms demonstrate robust associations with driving-related concerns, it is unclear whether psychological difficulties are better conceptualized as a causal or aggravating factor for subsequent impairment. Further investigation comparing both clinical and non-clinical samples is needed to determine the extent to which mental health symptoms directly impact driving-related outcomes in this population.
Respondent characteristics also limit the potential generalization of results. Participants in this study were noticeably older than those in both the student and community MVA samples. Enrollment in the larger study was further restricted to male veterans given concerns with the feasibility of mixed-sex treatment groups for service members with PTSD (see Sloan et al., 2018; Sloan, Unger, & Beck, 2016). Implications for the interpretation of group-level effects are mixed. Existing research has linked male gender to greater levels of impulsivity, risk taking, aggression, and perceived driving skill as well as lower levels of travel anxiety and driving avoidance (e.g., Arnett, Offer, & Fine, 1997; Deffenbacher, Lynch, Filetti, Dahlen, & Oetting, 2003; Taylor & Paki, 2008; Ulleberg, 2002). Increasing age, by contrast, is associated with reductions in reckless driving behavior, greater perceptions of risk, lower behavioral aggression, and reduced driving speed (e.g., Gregersen & Bjurulf, 1996; Horberry, Anderson, Regan, Triggs, & Brown, 2006; Krahé, 2005; Krahé & Fenske, 2002). Comparable performance deficit and safety/caution scores across male veterans and participants in the predominantly female MVA sample are therefore notable. Elevations in performance deficit and safety/caution scales relative to student drivers, by contrast, could be attributable to age-related differences, although moderate increases in hostile/aggressive behavior (d = .53) run counter to trends in the larger population. Unfortunately, the current data are unable to provide information on the frequency of anxious behavior in female veterans. A lack of diversity with respect to participant sex is a major limitation of the veteran driving literature more broadly, with women consistently under-represented (or often absent) in the existing research. The inclusion of increasingly diverse samples in terms of sex, age, race/ethnicity, and socioeconomic background will be important for continued investigation given the potential impact of driving impairment on social, health, and other financial outcomes.
While large from the perspective of clinical research and adequate for the evaluation of correlations and means-based comparisons, the current sample of N = 160 is small based on traditional standards for factor analytic research. However, modern approaches for estimating the power of confirmatory analyses draw on features of the population model (e.g., number of factors, number of indicators, strength of factor loadings) to determine the sample necessary for estimation (Brown, 2006). For example, simulation research by Wolf, Harrington, Clark, and Miller (2013)) identified samples between N = 110 and N = 190 as adequately powered for the estimation of 3-factor models containing six to eight indicators per factor, with item loadings set to .50 and .65. Factor loadings in the current model, as well as coefficients observed in development research by Clapp et al. (2011), suggest that estimates by Wolf et al. provide a reasonable approximation of the minimum sample required for evaluation of the DBS. Incorporation of Swain-corrected statistics to account for known biases in (Herzog & Boomsma, 2009; Herzog et al., 2007) provides additional confidence in the reliable estimation of the hypothesized 3-factor model.
As in much of the existing literature, evaluation of maladaptive driving in the current study was limited to self-reported behavior. Although self-report scores do not limit assessment of the structural properties of the DBS, access to observational and/or archival indicators of problematic driving (e.g., traffic records, informant reports, road tests, simulator performance) could provide external confirmation of respondent-identified difficulties. Behavioral measures of performance have become increasingly common in the larger driving literature (e.g., Amick et al., 2013; Classen et al., 2017; Taylor et al., 2007) and will be an important consideration in the continued validation of self-report assessments.
5. Conclusions
Best-practice standards for psychological testing require formal evaluation of an instrument prior to use in populations for which psychometric data are unavailable (American Psychiatric Association, 1999; Standard, 1.4). Results of the current study provide robust support for the internal consistency of DBS scales as well as evidence for the factorial, concurrent, discriminant, and discriminative validity of scores among help-seeking veterans with PTSD. Similarities in behaviors captured by the DBS and those reported in the larger veteran driving literature suggest the measure may have utility in assessing reactions believed to contribute to negative traffic outcomes in military service members.
Acknowledgments
This work was supported by the Department of Veteran Affairs [I01 CX000467].
Footnotes
Pooled variance estimates were used to standardize effect sizes for means-based comparisons: .
Whereas fit for the current study was assessed in a strictly confirmatory model, modification indices identified potential improvement with the addition of error covariances for selected performance deficit [dbs5: I drift into other lanes; dbs4: I have trouble staying in the correct lane] and hostile/aggressive [dbs18: I try to find ways to let other drivers know they are making me nervous; dbs17: I honk my horn at the driver who made me nervous] items. The inclusion of error covariances for performance deficit (; ; CFIS = .93; TLIS = .91; RMSEAS = .07, 90% CI [.05, .08]; SRMR = .08) and hostile/aggressive (; ; CFIS = .94; TLIS = .94; RMSEAS = .06, 90% CI [.05, .07]; SRMR = .08) indicators produced improvements in overall fit across successive exploratory models.
References
- Adler AB, Bliese PD, McGurk D, Hoge CW, & Castro CA (2009). Battlemind debriefing and battlemind training as early interventions with soldiers returning from iraq: Randomization by platoon. Journal of Consulting and Clinical Psychology, 77, 928–940. 10.1037/a0016877. [DOI] [PubMed] [Google Scholar]
- Adler AB, Castro CA, & McGurk D (2009). Time-driven battlemind psychological debriefing: A group-level early intervention in combat. Military Medicine, 174, 21–28. 10.7205/MILMED-D-00-2208. [DOI] [PubMed] [Google Scholar]
- Amick MM, Kraft M, & McGlinchey R (2013). Driving simulator performance of veterans from the Iraq and Afghanistan wars. Journal of Rehabilitation Research and Development, 50, 463–470. 10.1682/JRRD2012.06.0108. [DOI] [PubMed] [Google Scholar]
- Antony MM, Craske MG, & Barlow DH (2006). Mastery of your specific phobia: Client workbook (2nd ed.). New York: Oxford University Press. [Google Scholar]
- American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington DC: Author. [Google Scholar]
- American Psychiatric Association (1999). Standards for educational and psychological testing. Washington, DC: American Educational Research Association. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington DC: Author. [Google Scholar]
- Arnett JJ, Offer D, & Fine MA (1997). Reckless driving in adolescence:’ State’ and’ trait’ factors. Accident; Analysis and Prevention, 29, 57–63. 10.1016/S0001-4575(97)87007-8. [DOI] [PubMed] [Google Scholar]
- Baker AS, Litwack SD, Clapp JD, Beck JG, & Sloan DM (2014). The driving Behavior Survey as a measure of behavioral stress responses to MVA-related PTSD. Behavior Therapy, 45, 444–453. 10.1016/j.beth.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, & Steer RA (1993). Beck anxiety inventory manual San Antonio, TX: Psychological Cooperation. [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56, 893–897. 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown G (1996). Manual for the beck depression inventory II. (BDI-II). San Antonio: Psychological Corporation. [Google Scholar]
- Beck JG, Coffey SF, Foy DW, Keane TM, & Blanchard EB (2009). Group cognitive behavior therapy for posttraumatic stress disorder: An initial randomized pilot study. Behavior Therapy, 40, 82–92. 10.1016/j.beth.2008.01.003. [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, & Hickling EJ (2004). After the crash: Psychological assessment and treatment of survivors of motor vehicle accidents (2nd ed.). Washington DC: American Psychological Association. [Google Scholar]
- Brown TA (2006). Confirmatory factor analysis for applied research. New York: Guilford Press. [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit In Bollen KA, & Long JS (Eds.). Testing structural equation models. Newbury Park, CA: Sage Publications. [Google Scholar]
- Bullman TA, Kang HK, Smolenski DJ, Skopp NA, Gahm GA, & Reger MA (2017). Risk of motor vehicle accident death among 1.3 million veterans of the Iraq and Afghanistan wars. Traffic Injury Prevention, 18, 369–374. 10.1080/15389588.2016.1206201. [DOI] [PubMed] [Google Scholar]
- Castro CA, Hoge CW, & Cox AL (2006). Battlemind training: Building soldier resiliency. Human dimensions in military operations – Military leaders’ strategies for addressing stress and psychological support 42–1–42–46 Meeting Proceedings RTO-MP-HFM-134, Paper 42. Neuilly-sur-Seine, France: RTO. [Google Scholar]
- Clapp JD, Baker AS, Litwack SD, Sloan DM, & Beck JG (2014). Properties of the Driving Behavior Survey among individuals with motor vehicle accident-related posttraumatic stress disorder. Journal of Anxiety Disorders, 28, 1–7. 10.1016/j.janxdis.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clapp JD, Masci J, Bennett SA, & Beck JG (2010). Physical and psychosocial functioning following motor vehicle trauma: Relationships with chronic pain, posttraumatic stress, and medication use. European Journal of Pain, 14, 418–425. 10.1016/j.ejpain.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clapp JD, Olsen SA, Beck JG, Palyo SA, Grant DM, Gudmundsdottir B, ... Marques L (2011). The driving behavior survey: Scale construction and validation. Journal of Anxiety Disorders, 25, 96–105. 10.1016/j.janxdis.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Classen S, Winter S, Monahan M, Yarney A, Link Lutz A, Platek K, ... Levy C (2017). Driving intervention for returning combat veterans: Interim analysis of a randomized controlled trial. OTJR Occupation Participation Health, 37, 62–71. 10.1177/1539449216675582. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- deBeurs E, Wilson K, Chambless DL, Goldstein A, & Feske U (1997). Convergent and divergent validity of the Beck Anxiety Inventory for patients with panic disorder and agoraphobia. Depression and Anxiety, 6, 140–146. . [DOI] [PubMed] [Google Scholar]
- Deffenbacher JL, Huff ME, Lynch RS, Oetting ER, & Salvatore NF (2000). Characteristics and treatment of high-anger drivers. Journal of Counseling Psychology, 47, 5–17. 10.1037/0022-0167.47.1.5. [DOI] [Google Scholar]
- Deffenbacher JL, Lynch RS, Filetti LB, Dahlen ER, & Oetting ER (2003). Anger, aggression, risky behavior, and crash-related outcomes in three groups of drivers. Behaviour Research and Therapy, 41, 333–349. 10.1016/S0005-7967(02)00014-1. [DOI] [PubMed] [Google Scholar]
- Del Vecchio T, & O’Leary KD (2004). Effectiveness of anger treatments for specific anger problems: A meta-analytic review. Clinical Psychology Review, 24, 15–34. 10.1016/j.cpr.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Fear NT, Iversen AC, Chatterjee A, Jones M, Greenberg N, Hull L, ... Wessely S (2008). Risky driving among regular armed forces personnel from the United Kingdom. American Journal of Preventive Medicine, 35, 230–236. 10.1016/j.amepre.2008.05.027. [DOI] [PubMed] [Google Scholar]
- Grant DM, Beck JG, Marques LM, Palyo SA, & Clapp JD (2008). The structure of distress following trauma: Posttraumatic stress disorder, major depressive disorder, and generalized anxiety disorder. Journal of Abnormal Psychology, 117, 662–672. 10.1037/a0012591. [DOI] [PubMed] [Google Scholar]
- Gregersen NP, & Bjurulf P (1996). Young novice drivers: Towards a model of their accident involvement. Accident; Analysis and Prevention, 28, 229–241. 10.1016/0001-4575(95)00063-1. [DOI] [PubMed] [Google Scholar]
- Herzog W, & Boomsma A (2009). Small-sample robust estimators of noncentrality-based and incremental model fit. Structural Equation Modeling, 16, 1–27. 10.1080/10705510802561279. [DOI] [Google Scholar]
- Herzog W, Boomsma A, & Reinecke S (2007). The model-size effect on traditional and modified tests of covariance structures. Structural Equation Modeling, 14, 361–390. 10.1080/10705510701301602. [DOI] [Google Scholar]
- Hickling EJ, Blanchard EB, Silverman DJ, & Schwarz SR (1992). Motor vehicle accidents, headaches and post-traumatic stress disorder: Assessment findings in a consecutive series. Headache the Journal of Head and Face Pain, 32, 147–151. 10.1111/j.1526-4610.1992.hed3203147.x. [DOI] [PubMed] [Google Scholar]
- Hoggatt KJ, Prescott MR, Goldmann E, Tamburrino M, Calabrese JR, Liberzon I, ... Galea S (2015). The prevalence and correlates of risky driving behavior among National Guard soldiers. Traffic Injury Prevention, 16, 17–23. 10.1080/15389588.2014.896994. [DOI] [PubMed] [Google Scholar]
- Horberry T, Anderson J, Regan MA, Triggs TJ, & Brown J (2006). Driver distraction: The effects of concurrent in-vehicle tasks, road environment complexity and age on driving performance. Accident; Analysis and Prevention, 38, 185–191. 10.1016/j.aap.2005.09.007. [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. 10.1080/10705519909540118. [DOI] [Google Scholar]
- Hwang EJ, Peyton CG, Kim DK, Nakama-Sato KK, & Noble AE (2014). Postdeployment driving stress and related occupational limitations among veterans of Operation Iraqi Freedom and Operation Enduring Freedom. American Journal of Occupational Therapy, 68, 386–394. 10.5014/ajot.2014.011668. [DOI] [PubMed] [Google Scholar]
- Kang HK, & Bullman TA (1996). Mortality among US veterans of the persian gulf war. The New England Journal of Medicine, 335, 1498–1504. 10.1056/NEJM199611143352006. [DOI] [PubMed] [Google Scholar]
- Kline RB (2011). Principals and practice of structural equation modeling (3rd ed.). New York: Guilford Press. [Google Scholar]
- Krahé B (2005). Predictors of women’s aggressive driving behavior. Aggressive Behavior, 31, 537–546. 10.1002/ab.20070. [DOI] [Google Scholar]
- Krahé B, & Fenske I (2002). Predicting aggressive driving behavior: The role of macho personality, age, and power of car. Aggressive Behavior, 28, 21–29. 10.1002/ab.90003. [DOI] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, ... Burns K (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment, 12, 210–224. 10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Kuhn E, Drescher K, Ruzek J, & Rosen C (2010). Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. Journal of Traumatic Stress, 23, 399–402. 10.1002/jts.20536. [DOI] [PubMed] [Google Scholar]
- Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, & Cifu DX (2011). Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. Journal of Rehabilitation Research and Development, 48, 913–926. 10.1682/JRRD.2010.08.0140. [DOI] [PubMed] [Google Scholar]
- Lew HL, Amick MM, Kraft M, Stein MB, & Cifu DX (2010). Potential driving issues in combat returnees. NeuroRehabilitation, 26, 271–278. 10.3233/NRE-2010-0562. [DOI] [PubMed] [Google Scholar]
- Lincoln AE, Hooper TI, Kang HK, DeBakey SF, Cowan DN, & Gackstetter GD (2006). Motor vehicle fatalities among Gulf War era veterans: Characteristics, mechanisms, and circumstances. Traffic Injury Prevention, 7, 31–37. 10.1080/15389580500412028. [DOI] [PubMed] [Google Scholar]
- Matthews G, Dorn L, Hoyes TW, Davies DR, Glendon AI, & Taylor RG (1998). Driver stress and performance on a driving simulator. Human Factors, 40, 136–149. 10.1518/001872098779480569. [DOI] [PubMed] [Google Scholar]
- Mayou R, Bryant B, & Ehlers A (2001). Prediction of psychological outcomes one year after a motor vehicle accident. The American Journal of Psychiatry, 158, 1231–1238. 10.1176/appi.ajp.158.8.1231. [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, ... Chertkow H (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53, 695–699. 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- Orth U, & Wieland E (2006). Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology, 74, 698–706. 10.1037/0022-006X.74.4.698. [DOI] [PubMed] [Google Scholar]
- Pendlebury ST, Cuthbertson FC, Welch SJ, Mehta Z, & Rothwell PM (2010). Underestimation of cognitive impairment by Mini-Mental State Examination versus the Montreal Cognitive Assessment in patients with transient ischemic attack and stroke. Stroke, 41, 1290–1293. 10.1161/STROKEAHA.110.579888. [DOI] [PubMed] [Google Scholar]
- Possis E, Bui T, Gavian M, Leskela J, Linardatos E, Loughlin J, ... Strom T (2014). Driving difficulties among military veterans: Clinical needs and current intervention status. Military Medicine, 179, 633–639. [DOI] [PubMed] [Google Scholar]
- Quilty LC, Zhang KA, & Bagby RM (2010). The latent symptom structure of the Beck Depression Inventory–II in outpatients with major depression. Psychological Assessment, 22, 603–608. 10.7205/MILMED-D-13-00327. [DOI] [PubMed] [Google Scholar]
- Sheppard SC, & Earleywine M (2013). Using the unmatched count technique to improve base rate estimates of risky driving behaviours among veterans of the wars in Iraq and Afghanistan. Injury Prevention, 19, 382–386. 10.1136/injuryprev-2012-040639. [DOI] [PubMed] [Google Scholar]
- Sloan DM, Marx BP, Bovin MJ, Feinstein BA, & Gallagher MW (2012). Written exposure as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. Behaviour Research and Therapy, 50, 627–635. 10.1016/j.brat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan DM, Unger W, & Beck JG (2016). Cognitive-behavioral group treatment for veterans diagnosed with PTSD: Design of a hybrid efficacy-effectiveness clinical trial. Contemporary Clinical Trials, 47, 123–130. 10.1016/j.cct.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan DM, Unger W, Lee DJ, & Beck JG (2018). A randomized controlled trial of group cognitive behavioral treatment for veterans diagnosed with chronic posttraumatic stress disorder. Journal of Traumatic Stress, 31, 886–898. 10.1002/jts.22338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T, Gildeh N, & Holmes C (2007). The Montreal Cognitive Assessment: Validity and utility in a memory clinic setting. The Canadian Journal of Psychiatry, 52, 329–332. [DOI] [PubMed] [Google Scholar]
- Strom T, Leskela J, Possis E, Thuras P, Leuty ME, Doane BM, ... Rosenzweig L (2013). Cognitive–Behavioral group treatment for driving-related anger, aggression, and risky driving in combat veterans: A pilot study. Journal of Traumatic Stress, 26, 405–408. 10.1177/070674370705200508. [DOI] [PubMed] [Google Scholar]
- Taylor J, Deane FP, & Podd J (2002). Driving-related fear: A review. Clinical Psychology Review, 22, 631–645. 10.1016/S0272-7358(01)00114-3. [DOI] [PubMed] [Google Scholar]
- Taylor J, Deane FP, & Podd J (2007). Driving fear and driving skills: Comparison between fearful and control samples using standardised on-road assessment. Behaviour Research and Therapy, 45, 805–818. 10.1016/j.brat.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Taylor J, Deane FP, & Podd J (2008). The relationship between driving anxiety and driving skill: A review of human factors and anxiety-performance theories to clarify future research needs. New Zealand Journal of Psychology, 37, 28–37. [Google Scholar]
- Taylor S, & Koch WJ (1995). Anxiety disorders due to motor vehicle accidents: Nature and treatment. Clinical Psychology Review, 15, 721–738. 10.1016/0272-7358(95)00043-7. [DOI] [Google Scholar]
- Taylor J, & Paki D (2008). Wanna drive? Driving anxiety and fear in a New Zealand community sample. New Zealand Journal of Psychology, 37, 31–37. [Google Scholar]
- Ulleberg P (2002). Personality subtypes of young drivers: Relationship to risk-taking preferences, accident involvement, and response to a traffic safety campaign. Transportation Research Part F, Traffic Psychology and Behaviour, 4, 279–297. 10.1016/S1369-8478(01)00029-8. [DOI] [Google Scholar]
- U.S. Department of Veterans Affairs (2009). VA, DOT, DOD steer vets toward safe driving. Retrieved from https://www1.va.gov/opa/pressrel/pressrelease.cfm?id=1643.
- Watanabe KK, & Kang HK (1996). Mortality patterns among Vietnam veterans: A 24-year retrospective analysis. Journal of Occupational and Environmental Medicine, 38(3), 272–278. [DOI] [PubMed] [Google Scholar]
- Waldron-Perrine B, & Axelrod BN (2012). Determining an appropriate cutting score for indication of impairment on the Montreal Cognitive Assessment. International Journal of Geriatric Psychiatry, 27, 1189–1194. 10.1002/gps.3768. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The clinician-administered PTSD scale for DSM-5 (CAPS-5). Retrieved fromwww.ptsd.va.gov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, ... Marx BP (2018). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30, 383–395. 10.1037/pas0000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whipple EK, Schultheis MT, & Robinson KM (2016). Preliminary findings of a novel measure of driving behaviors in Veterans with comorbid TBI and PTSD. Journal of Rehabilitation Research and Development, 53, 827–837. 10.1682/JRRD.2015.09.0172. [DOI] [PubMed] [Google Scholar]
- Wilkinson GS, & Robertson GJ (2006). Wide range achievement test 4 professional manual Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Wolf EJ, Harrington KM, Clark SL, & Miller MW (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement, 73, 913–934. 10.1177/0013164413495237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinzow HM, Brooks J, & Stern EB (2013). Driving-related anxiety in recently deployed service members: Cues, mental health correlates, and help-seeking behavior. Military Medicine, 178, e357–e361. 10.7205/MILMED-D-12-00303. [DOI] [PubMed] [Google Scholar]