Madam,
Pulse oximetry is a standard ASA monitor which enhances hypoxia detection and prevents perioperative adverse events.[1] However, it provides no indication of falling PaO2 until saturation begins to decrease. Oxygen Reserve Index (ORI) is a novel real-time pulse oximeter based non-dimensional index that ranges from 1 to 0 as PaO2 decreases from 200 mmHg to 80 mmHg. It is measured by optically detecting changes in venous oxygen saturation (SvO2) after arterial oxygen saturation (SaO2) saturates to the maximum.[2] ORI may thereby provide a clinically important warning of impending desaturation ahead of standard pulse oximetry in high risk procedures such as bronchoscopy.
A three-year-old, male child weighing 11 kg, was brought by parents with complaints of cough since 10 days and increased respiratory activity with retraction since 4 days. CT scan showed patchy consolidation in left middle and lower zone with soft tissue density in left main bronchus suggestive of foreign body bronchus. Patient was posted for rigid bronchoscopy SOS flexible bronchoscopy. After informed consent and intravenous Midazolam premedication, patient was taken inside the operating room (OR). Standard monitors were attached along with Masimo SET rainbow pulse oximeter (Masimo, Irvine, CA) with the ORI probe on the right index finger. Anesthesia was induced using Inj. Propofol 3 mg/kg and Inj. Atracurium 0.5 mg/kg and a 4.5 mm ID rigid bronchoscope was inserted, and was subsequently ventilated though the side port of ventilating bronchoscope.
The baseline ORI was 0.38 which increased to 0.68 after preoxygenation. The ORI dropped progressively to 0.28 to 0.18 during the apneic periods when instrumentation was done, and improved to 0.33 when ventilation was resumed. The pulse oximeter showed 100% saturation during this period. The ORI dropped to 0 after the final instrumentation and suctioning was done to remove mucus plugs from the left mainstem and lobar bronchi [Figure 1]. The oxygen saturation decreased from 100% to 97% 2 minutes after ORI came down to 0. Following the procedure, the patient was intubated with 4.5 mm ID uncuffed endotracheal tube and ventilated with 100% Oxygen. The saturation rose to 100% and ORI gradually increased to 0.33. The child was then extubated and shifted to the ICU.
Figure 1.
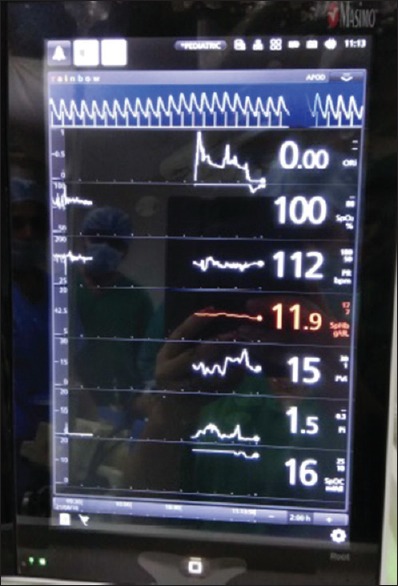
Masimo SET Rainbow monitor showing ORI zero at SpO2 of 100%
Pulse oximetry is a sensitive indicator of desaturation, but it delays detection of hypoventilation or hypoxemia in children when oxygen supplementation is provided as oxyhemoglobin saturation remains 100% over a wide range of oxygen partial pressures >80 mmHg.[3,4] Hence, it is difficult to predict when desaturation will start in an apneic patient or during procedures like bronchoscopy. ORI serves to indicate PaO2 trends (rising or falling Pao2) when Spo2 is over 98%. It also reflects oxygenation in the moderate hyperoxic range (PaO2100–200 mmHg).
In our patient, SpO2 remained at 100% during the period of preoxygenation and apnea. However, ORI showed changes in either direction with maximum value at preoxygenation (0.68) and decreasing gradually during apnea (0.2) when instrumentation was done. It improved when ventilation was resumed. Only after ORI dropped to zero did the SpO2 value decrease. Monitoring ORI detects impending desaturation before evident changes in SPO2 occur. This gives the clinician an important warning ahead of time to take corrective measures in vulnerable population. However, ORI cannot replace pulse oximetry or PaO2 measurements, but only act as a complementary tool. The measurements and calculation of ORI are affected by temperature, pH, PaCO2 and low perfusion states.[2]
Once desaturation starts during airway instrumentation, which is likely in procedures like bronchoscopy, it typically progresses at an exponential rate more so in premature babies, infants, young children, and also those with respiratory pathology/respiratory tract infections. Obtaining PaO2 values from ABG is not practical in such situations as it is time consuming and also invasive.[2] So during such situations, having a reliable estimate of time before hypoxemia becomes critical and helps us guide management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Applegate RL, 2nd, Dorotta IL, Wells B, Juma D, Applegate PM. The relationship between oxygen reserve index and arterial partial pressure of oxygen during surgery. Anesth Analg. 2016;123:626–33. doi: 10.1213/ANE.0000000000001262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheeren TWL, Belda FJ, Perel A. The oxygen reserve index (ORI): A new tool to monitor oxygen therapy. J Clin Monit Comput. 2018;32:379–89. doi: 10.1007/s10877-017-0049-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Szmuk P, Steiner JW, Olomu PN, Ploski RP, Sessler DI, Ezri T. Oxygen reserve index: A novel noninvasive measure of oxygen reserve--A pilot study. Anesthesiology. 2016;124:779–84. doi: 10.1097/ALN.0000000000001009. [DOI] [PubMed] [Google Scholar]
- 4.Yoshida K, Isosu T, Murakawa M. Making use of the oxygen reserve index (ORiTM): A new parameter of oxygenation reserve potential. Pulm Crit Care Med. 2018;3:1–2. [Google Scholar]


