ABSTRACT
Background
there are around 100,000 new stroke cases and over a million people living with its consequences annually in the UK. This has large impacts on health and social care, unpaid carers and lost productivity. We aimed to estimate associated costs.
Methods
we estimated 2014/2015 annual mean cost per person and aggregate UK cost of stroke for individuals aged ≥40 from a societal perspective. Health and social care costs in the first and subsequent years after stroke were estimated from discrete event simulation modelling, with probability of progression and length of receipt of different health and social care services obtained from routine registry and audit data. Unpaid care hours and lost productivity were obtained from trial data. UK unit costs were applied to estimate mean costs. Epidemiological estimates of stroke incidence and prevalence were then applied to estimate aggregate costs for the UK.
Results
mean cost of new-onset stroke is £45,409 (95% CI 42,054-48,763) in the first year after stroke and £24,778 (20,234–29,322) in subsequent years. Aggregate societal cost of stroke is £26 billion per year, including £8.6 billion for NHS and social care. The largest component of total cost was unpaid care (61%) and, given high survival, £20.6 billion related to ongoing care.
Conclusion
the estimated aggregate cost of stroke substantially exceeds previous UK estimates. Since most of the cost is attributed to unpaid care, interventions aimed at rehabilitation and reducing new and recurrent stroke are likely to yield substantial benefits to carers and cost savings to society.
Keywords: burden, cost, economic, older people, simulation, stroke
Key Points
There are around 100,000 new stroke cases and over a million people living with its consequences each year in the UK.
On average, new onset strokes cost £45 k in the first year & £25 k in subsequent years, totalling £26 billion per year (UK).
Interventions for rehabilitation and reducing new and recurrent stroke could yield substantial benefits and savings.
Introduction
The global lifetime risk of stroke is approximately 25% from the age of 25 years [1], making it the second largest cause of death worldwide and fourth in the UK. There are over 113,000 new strokes annually in the UK [2], a quarter of which occur among the under 65 s [3]. Many of the estimated 950,000 stroke survivors [4] experience significant and long-term residual physical and psychological impacts, repeat strokes, transient ischaemic attacks and/or death within a year of stroke. [3] Stroke prevention and treatment, and its morbidity and mortality impacts, carry economic consequences across society [5,6]. Despite significant progress in prevention, treatment and rehabilitation, there is a great capacity for further improvements and thus reduced economic impacts. This is ever more important given pressures faced by both formal and unpaid care sectors.
Understanding the scale and range of consequences can help prioritize scarce resources. The annual societal cost of stroke in the UK has previously been estimated at £9 billion (2005 prices), with over half attributed to lost employment and unpaid (‘informal’) care [5]. There is a need for updated estimates to ensure future service, and policy responses can be discussed in the context of timely and relevant data.
Methods
We synthesized data from multiple sources to estimate annual mean cost per person and the aggregate UK cost of stroke affecting individuals aged ≥40 years. A societal perspective incorporated formal health and social care (hospitals, community care and care homes), unpaid care and lost productivity arising due to stroke-related morbidity and early mortality. Costs in the year following a first-stroke episode formed the basis for costs of incident (new) stroke, while annual costs in subsequent years represented costs of prevalent stroke (stroke survivors). Mean costs were further gauged by sex, age (40–64, 65–74, 75–84, ≥85 years), stroke type (ischaemic or haemorrhagic) and stroke severity (National Institutes of Health Strokes Score (NIHSS) 1–2 for no/mild stroke (NIHSS score of 0–4), 3 for moderate stroke (scores 5–15) and 4–5 for severe stroke (scores 16–42)). Reported costs are for the 2014/2015 cost year in Great British Pound Sterling (GBP, £).
Average cost of formal health and social care
Estimates for National Health Service (NHS) and Personal Social Services (PSS) costs were obtained using a modified version of a cost-of-illness model [7,8] developed by the National Guideline Centre (NGC) and the Sentinel Stroke National Audit Programme (SSNAP) at the Royal College of Physicians (RCP) on behalf of NHS England. They used data from SSNAP (April 2013—March 2015; n = 111,846) and the South London Stroke Register (SLSR) to inform a discrete event simulation (DES) model, which represented the probability of progression and length of stay in various settings in the stroke pathway, conditional on patient characteristics. The pathway started with admission to a hospital acute stroke unit. Subsequent progression to other settings (stroke unit, early supported discharge, community rehabilitation), discharge (to care home or own home) or death was conditional on individual factors, such as age, sex and stroke severity. Upon discharge from hospital, the patient’s journey continues through repeat strokes, care home admission or death. Stroke services included in the model are detailed by Xu et al. [7,8] and are summarized in Figure 1 and Supplementary Appendix 1.
Figure 1.
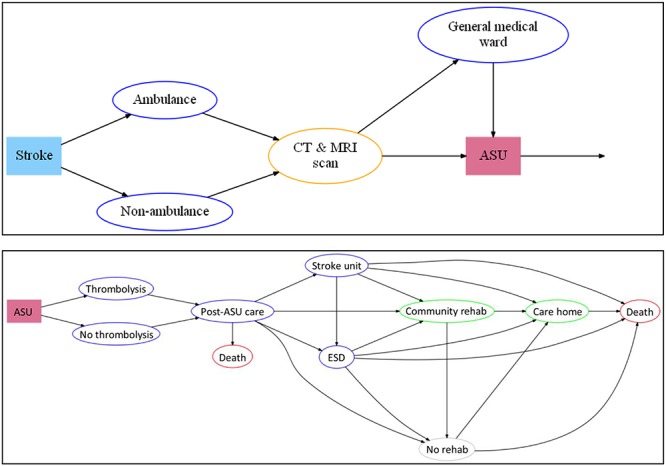
Pathways represented in the NGC model.
We modified the NGC model to generate separate estimates for incident and prevalent stroke. Cross-sectional data collection points were changed from 1 and 5 years post-stroke to 1, 2, 3 and 4 years post-stroke. Costs incurred in the first 12 months were then attributed to incident stroke and average costs incurred in years 2, 3 and 4 were used as a proxy for prevalent stroke. Costs incurred in years 2, 3 and 4 post-stroke were adjusted for the proportion of patients alive at the start of the corresponding year to avoid underestimating the true cost of follow-up care of stroke survivors. Unit costs were also updated (see below).
Average cost of unpaid care
Costs of care provided by family and other unpaid carers were estimated using control arm data from two large UK-based randomized controlled stroke rehabilitation trials: TRACS [9] and LoTS Care [10]. Both provided self-reported data at 6 and 12 months post-recruitment on number of hours spent by all resident and non-resident unpaid carers on personal care and a range of other tasks such as preparing meals, gardening and help with managing finances. Neither trial sought to assess inputs specifically attributable to stroke due to the difficulties in doing so but did ask respondents to report assistance received due to illness/injury over and above any help they received normally. For stroke incidence costs, we used unpaid care hours over the full 12-month period from the TRACS trial; for stroke prevalence costs, we used unpaid care hours from only the last 6 months of follow-up from the LoTS Care trial to better reflect longer-term inputs (the trial recruited patients at hospital discharge, thus data collected at 12 months post-recruitment [covering the previous 6 months] relates at least partially to the period beyond 1 year post-stroke).
Since the requirement for a primary unpaid carer for inclusion in TRACS risked over-estimating unpaid care inputs for our purposes, we used the trial’s participant inclusion flow chart [11] to determine the proportion of patients screened but excluded for absence of a primary carer, and added the equivalent proportion of simulated participants into the model. Mean unpaid care costs for these additional patients were assumed as 25% of those for people with a primary carer.
Average cost of lost productivity
LoTS Care trial data [10] were also used for estimating lost productivity. We used data on changed employment status (e.g. moving from full- to part-time working, or not working) and mortality 6 months after stroke for stroke incidence costs and the equivalent figures at 12 months for stroke prevalence costs. Number of hours spent in full- (37.6 hours per week) and part-time (16.2 hours per week) work were assumed from national data [12].
Unit costs
Unit costs (Supplementary Appendix 2) for health and social care were derived from published UK sources for the 2014/2015 financial year [13–15].
National aggregate costs and estimates of incidence and prevalence
To derive the aggregate cost of stroke in the UK, we multiplied estimated mean cost of incident and prevalent stroke by estimated absolute incidence and prevalence. These in turn were calculated by combining age-specific incidence and prevalence rates per 1,000 people reported in literature with mid-2016 age-specific population figures [17] for adults aged ≥40 years; this accounted for changes in the age structure of the UK population.
A focused review of UK studies identified three key studies each for stroke incidence [2,18,19] and prevalence [4,20,21]. We excluded three incidence studies for inclusion of transient ischaemic attack [22,23] and focused only on ischaemic stroke [24].
From included studies, we estimated stroke incidence in 2015 ranged from 113,400 to 119,100, with a potential range from 85,800 to 147,600 when using low and high estimates reported in individual studies (We later used these ranges in our sensitivity analyses—see below.) As a point estimate, we focused on the mid-point estimate of 117,600 [19].
Similarly, we estimated stroke prevalence ranged from 950,000 to 1.3 million, or 797,000 to 1.4 million when accounting for reported ranges. In estimating ranges for stroke prevalence, we adjusted numbers from individual studies to represent the full population of interest e.g. Geddes et al. [4] only sampled individuals aged ≥55 years, so we used estimates from O’Mahony et al. [21] to generate estimates for younger adults. As the mid-point estimate of 1,002,600 reported by Jagger et al. [20] was from a simulation and based on old data (1991–1994), we instead used Geddes et al.’s [4] figure (950,200; based on n = 18,827) for our point estimate.
Analysis of uncertainty
Estimates of mean cost produced by a DES model can be influenced by sampling variation across individuals within the model, particularly in subgroups containing small patient numbers (i.e. Monte Carlo error). To minimize individual-level uncertainty and obtain stable estimates of 95% confidence intervals (CI) for mean cost, input values were repeatedly sampled over a large number of iterations. Repeated testing and validation determined that 500 replications of the model output with 4,000 individuals per run were necessary to achieve stable values for the point estimate and standard error.
To determine the effect of uncertainty around individual parameters, we used one-way sensitivity analyses to vary values such as assumed length of stay in stroke units and transition probabilities (Supplementary Appendix 3).
Uncertainty in aggregate cost estimates was gauged by substituting lower and upper estimates of incidence and prevalence and by applying 95% CI for mean cost in each cost category derived from the NGC model.
Results
Mean costs of stroke
The mean annual cost per person from an NHS and PSS perspective in the first year post-stroke is £18,081 (95% CI 17,621–18,542) with £13,269 (95% CI 13,058–13,480) and £4,812 (95% CI 4,434–5,190) attributable to NHS and PSS, respectively (Table 1). Annual NHS and PSS costs for subsequent years total £7,759 (95% CI 7,200–8,318), but a greater portion becomes attributable to PSS rather than NHS care (£5,544 versus £2,215).
Table 1.
Mean cost of incident and prevalent stroke
| NHS & PSS cost | Unpaid care & lost productivity cost | Total cost | ||||
|---|---|---|---|---|---|---|
| Category | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI |
| First year cost (incident stroke) | ||||||
| All patients | 18,081 | 17,621–18,542 | 27,328 | 24,434–30,221 | 45,409 | 42,054–48,763 |
| Age (years) | ||||||
| 40–64 | 12,770 | 12,089–13,451 | 33,191 | 26,567–39,815 | 45,961 | 38,656–53,266 |
| 65–74 | 15,577 | 14,742–16,412 | 25,800 | 21,351–30,248 | 41,377 | 36,093–46,660 |
| 75–84 | 20,011 | 19,201–20,820 | 27,487 | 22,924–32,050 | 47,497 | 42,124–52,870 |
| ≥85 | 22,961 | 21,892–24,029 | 18,234 | 11,274–25,194 | 41,195 | 33,166–49,223 |
| Sex | ||||||
| Male | 17,338 | 16,725–17,950 | 29,062 | 24,914–33,210 | 46,400 | 41,639–51,160 |
| Female | 18,824 | 18,198–19,451 | 25,090 | 21,196–28,984 | 43,914 | 39,394–48,435 |
| Stroke type | ||||||
| Ischaemic | 17,063 | 16,432–17,694 | 27,167 | 23,928–30,407 | 44,231 | 40,360–48,101 |
| Haemorrhage | 19,099 | 18,455–19,743 | 27,599 | 22,124–33,074 | 46,698 | 40,578–52,817 |
| Subsequent year cost (prevalent stroke) | ||||||
| All patients | 7,759 | 7,200–8,318 | 17,019 | 13,034–21,005 | 24,778 | 20,234–29,322 |
| Age (years) | ||||||
| 40–64 | 5,169 | 4,057–6,280 | 20,848 | 14,671–27,025 | 26,017 | 18,728–33,305 |
| 65–74 | 5,761 | 4,394–7,129 | 21,739 | 10,408–33,071 | 27,501 | 14,802–40,199 |
| 75–84 | 10,753 | 8,495–13,011 | 11,443 | 8,254–14,633 | 22,196 | 16,749–27,644 |
| ≥85 | 9,873 | 7,404–12,343 | 14,249 | 7,838–20,661 | 24,123 | 15,242–33,004 |
| Sex | ||||||
| Male | 7,221 | 5,741–8,701 | 18,681 | 12,308–25,053 | 25,901 | 18,049–33,754 |
| Female | 8,287 | 6,566–10,007 | 14,857 | 11,102–18,612 | 23,144 | 17,668–28,619 |
| Stroke type | ||||||
| Ischaemic | 7,225 | 5,750–8700 | 17,094 | 12,632–21,555 | 24,318 | 18,381–30,255 |
| Haemorrhage | 8,230 | 6,529–9931 | 18,315 | 9,855–26,775 | 26,545 | 16,384–36,706 |
The mean annual cost of unpaid care is £25,897 (95% CI 23,621–28,173) and £15,354 (95% CI 12,501–18,656) in the first and subsequent years after stroke respectively. For lost productivity, respective costs are £1,431 (95% CI 813–2,049) and £1,666 (95% CI 983–2,349); individuals aged 40–64 years (more likely to be of working age) had highest lost productivity costs (£5,172 per stroke case in the first year, £5,895 in subsequent years). Supplementary Appendices 4–7 provide further breakdowns for unpaid care and lost productivity.
Combining mean costs for NHS, PSS, unpaid care and lost productivity, the total mean cost of stroke from a societal perspective was £45,409 (42,054–48,763) in the first 12 months after stroke and £24,778 (20,234–29,322) in subsequent years.
Unit cost and length of stay in acute stroke units, probability of repeat stroke and probability of care home admission had a significant impact on costs estimates (Supplementary Appendix 3).
Aggregate cost of stroke
Aggregate annual costs are estimated at £26 billion (NHS £3.4 billion, 13%; PSS £5.2 billion, 20%; unpaid care £15.8 billion, 61%; lost productivity £1.6 billion, 6%) (Table 2). Costs for prevalent stroke are the main driver of aggregate societal costs due to the much larger number of stroke survivors (950,200) compared to new stroke cases each year (117,600).
Table 2.
Aggregate cost of incident and prevalent stroke in the UK: base case, low- and high-cost estimates
| Mean aggregate cost (£ million, range†), base case estimates‡ | Mean aggregate cost (£ million, range), low estimates‡ | Mean aggregate cost (£ million, range), high estimates‡ | |
|---|---|---|---|
| First year cost (incident stroke) | |||
| NHS | 1,560 (1138,1958) | 1,535 (1120,1927) | 1,585 (1156,1989) |
| Formal social care | 565 (412,710) | 521 (380,654) | 610 (445,766) |
| Unpaid care | 3,045 (2221,3822) | 2,777 (2026,3486) | 3,313 (2417,4158) |
| Lost productivity | 168 (122,211) | 95 (69,120) | 240 (175,302) |
| NHS & PSS perspective | 2,126 (1551,2668) | 2,072 (1511,2600) | 2,180 (1590,2736) |
| Societal perspective | 5,340 (3896,6702) | 4,945 (3608,6207) | 5,734 (4183,7197) |
| Subsequent year cost (prevalent stroke) | |||
| NHS | 1,844 (1576,2681) | 1,762 (1506,2563) | 1,925 (1645,2799) |
| Formal social care | 4,616 (3945,6712) | 4,174 (3567,6069) | 5,058 (4322,7355) |
| Unpaid care | 12,783 (10,925,18,588) | 10,034 (8575,14,590) | 15,532 (13,275,22,586) |
| Lost productivity | 1,387 (1185,2016) | 818 (699,1189) | 1,955 (1671,2843) |
| NHS & PSS perspective | 6,460 (5521,9393) | 5,994 (5123,8717) | 6,925 (5918,10,070) |
| Societal perspective | 20,630 (17,632,29,999) | 16,847 (14,398,24,497) | 24,413 (20,865,35,500) |
| Incident and prevalent stroke cost | |||
| NHS | 3,404 (2714,4639) | 3,298 (2626,4490) | 3,510 (2802,4789) |
| Formal social care | 5,181 (4358,7422) | 4,695 (3947,6724) | 5,668 (4768,8121) |
| Unpaid care | 15,828 (13,147,24,100) | 12,811 (10,602,18,077) | 18,845 (15,692,26,744) |
| Lost productivity | 1,555 (1308,2228) | 913 (769,1309) | 2,196 (1847,3146) |
| NHS & PSS perspective | 8,586 (7072,12,062) | 8,066 (6635,11,317) | 9,105 (7509,12,807) |
| Societal perspective | 25,970 (21,528,26,701) | 21,792 (18,006,30,704) | 30,148 (25,049,42,698) |
†Range based on low- and high-incidence and prevalence estimates.
‡Low- and high-cost estimates based on range of mean cost.
Unpaid care dominates forming 57 and 62% of costs of incident and prevalent stroke, respectively. The contribution of PSS costs doubles from 11% in the first year after stroke to 22% in subsequent years, reflecting shifting patterns of post-stroke care over time, i.e. reduced inputs from hospital services and increased dependence on formal and unpaid social care.
Discussion
Interpretation of findings
About, £26 billion represents a substantial cost impact in both formal and unpaid care sectors. Productivity losses were relatively small, but the trial data we drew on indicate that these persist a year after stroke. Of particular note, unpaid carers contribute substantially to stroke care.
Discussion of findings in context of existing evidence
Our estimates for NHS and social care costs align with those obtained by Xu et al. [7], since we used their model and underlying data for these cost domains. Drawing valid comparisons with other cost-of-illness studies is challenging given inevitable variations in methodology and context. For some context, Smith et al. [25] reported total direct and indirect costs of stroke for Ireland; while their total cost estimates (0.5–0.8 billion Euros as a lower bound estimate at 2007 prices) are lower due to smaller population size, it is nevertheless interesting to note that the proportional contributions to total costs were different. For example, nursing home costs accounted for 44% of total costs, with only 9% attributable to informal care. Wilkins et al. [26] presented total health care costs for cerebrovascular diseases at 2.6 billion Euros per year for the UK (2015 prices) and 3.3 billion Euros for unpaid care and lost productivity. Insufficient details prevent meaningful comparisons, but the overall size of those figures and the proportion that might be attributable to stroke is clearly substantially lower than ours.
Other estimates for aggregate annual costs in the UK are less recent and also generated much lower totals of £7 billion (2004 prices) for England [27] and £9 billion (2005 prices) for the UK [5] from similar cost perspectives. Using data now almost a decade older than used here, Saka et al. [5] estimated direct medical care costs as £4.4 billion compared to our estimate of £8.6 billion. More strikingly, they calculated unpaid care at £2.4 billion per year, compared to our £15.8 billion. Such differences may be driven by several factors. For instance, their primary data (the SLSR) represents a specific population and service context, and unpaid care was estimated using different data sources and estimation approaches.
Strengths and limitations
Our data sources are robust but do not reflect substantial recent changes to stroke care. Impacts of these are mixed in nature (e.g. increased short-term treatment costs, reduced length of stay, greater rates of survival), so their overall economic impact remains unclear. All cost-of-illness studies also carry uncertainty in parameter values. Detailed unpaid care and lost productivity data [9,10] represent the full economic implications of stroke but may also overestimate costs because longer term costs may be lower than assessed during the trial periods. Until improved precision in underlying data can reduce estimation uncertainty, estimates should be taken as indicative, rather than definitive.
Policy recommendations
Although significant progress in primary prevention and urgent care has improved stroke incidence and survival, there is scope to achieve more and to reduce costs for both ischaemic and haemorrhagic stroke e.g. through better stroke prevention. Substantial costs of stroke prevalence underline gaps in evidence-based cost-effective rehabilitation interventions [28], which could improve functioning and quality of life, reduce stroke recurrence and reduce need for longer-term care.
Greater policy support could help extend provision already available and recommended in clinical guidelines, but currently offered at sub-optimal levels risking inequitable variations in care, health and quality of life, and also wasted resources. For example, Xu et al. [7] estimated that each extra person thrombolyzed or receiving early supported discharge services could respectively generate NHS & PSS savings of approximately £6000 or £4000 in just 1 year. Similarly, reduced mortality and length of hospital stay achieved in London through centralizing services to increase delivery of effective urgent care could be replicated elsewhere [29,30].
Finally, contributions from unpaid carers reduce pressures on formal services but represent the transfer of significant responsibilities, which can carry negative health, well-being and economic consequences. It is thus important to assess and meet carers’ own needs for support [31,32].
Conclusion
Inevitably, current resource constraints, system pressures and practical hurdles create challenges for addressing the economic impacts and associated issues. However, it is likely that increased investments and a more co-ordinated approach to care, and research [33], would go a long way towards containing/reducing future impacts of stroke, improving outcomes and reducing variations in stroke care.
Supplementary Material
Acknowledgements:
We thank Xiang-Ming Xu and David Wonderling at the National Guideline Centre for generously sharing and explaining their economic model; Kate Holmes and Shamim Quadir at the Stroke Association for support and feedback throughout the project; William Day for providing support with focused literature reviews; our clinical advisor, Anne Forster at University of Leeds, for advice and support; and finally four anonymous peer reviewers who, on behalf of the funders, provided enormously helpful feedback on a draft report of this work.
Declaration of Conflicts of Interest:
None.
Declaration of Funding:
This work was supported by the UK Stroke Association [TSA CR 2016/01]. Views are authors’ own and not necessarily those of the Stroke Association.
Guarantor:
AP
Informed consent:
Informed consent was not sought for the present study because it used only secondary data in aggregated form.
Ethical approval:
Ethical approval was not sought for the present study because it used only secondary data in aggregated form.
References
- 1. The GBD 2016 Lifetime Risk of Stroke Collaborators Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. NEJM 2018; 379: 2429–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rothwell PM, Coull AJ, Giles MF et al. . Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford vascular study). Lancet 2004; 363: 1925–33. [DOI] [PubMed] [Google Scholar]
- 3. Stroke Association State of the nation: stroke statistics. London: Stroke Association, 2016. [Google Scholar]
- 4. Geddes JM, Fear J, Tennant A et al. . Prevalence of self reported stroke in a population in northern England. J Epidemiol Community Health 1996; 50: 140–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saka O, McGuire A, Wolfe C. Cost of stroke in the United Kingdom. Age Ageing 2009; 38: 27–32. [DOI] [PubMed] [Google Scholar]
- 6. National Audit Office Progress in improving stroke. Report on the findings from our modelling of stroke care provision. London: National Audit Office, 2010; (HC 291 2009-2010). [Google Scholar]
- 7. Xu XM, Vestesson E, Paley L et al. . The economic burden of stroke care in England, Wales and Northern Ireland: Using a national stroke register to estimate and report patient-level health economic outcomes in stroke. Eur Stroke J 2018; 3: 82–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Forster A, Dickerson J, Young J et al. . A structured training programme for caregivers of inpatients after stroke (TRACS): A cluster randomised controlled trial and cost-effectiveness analysis. Lancet 2013; 382: 2069–76. [DOI] [PubMed] [Google Scholar]
- 10. Forster A, Young J, Chapman K et al. . Cluster randomized controlled trial: Clinical and cost-effectiveness of a system of longer-term stroke care. Stroke 2015; 46: 2212–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Forster A, Dickerson J, Young J et al. . A cluster randomised controlled trial and economic evaluation of a structured training programme for caregivers of inpatients after stroke: The TRACS trial. Health Technol Assess 2013; 17: 1–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Office for National Statistics UK labour market: Feb 2017. London: ONS, 2017. [Google Scholar]
- 13. Curtis L, Burns A. Unit costs of health and social care. Canterbury: University of Kent, 2015. [Google Scholar]
- 14. Curtis L, Burns A. Unit costs of health and social care. Canterbury: University of Kent, 2014. [Google Scholar]
- 15. Department of Health and Social Care NHS Reference Costs 2014/15, 2015. https://www.gov.uk/government/publications/nhs-reference-costs-2014-to-2015 (Accessed 6 December 2019).
- 17. Office for National Statistics Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid-2016. London: ONS, 2016. [Google Scholar]
- 18. Wolfe CD, Rudd AG, Howard R et al. . Incidence and case fatality rates of stroke subtypes in a multiethnic population: The South London stroke register. J Neurol Neurosurg Psychiatry 2002; 72(2): 211–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stewart JA, Dundas R, Howard RS et al. . Ethnic differences in incidence of stroke: Prospective study with stroke register. BMJ 1999; 318(7189): 967–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jagger C, Matthews R, Spiers N et al. . Compression or expansion of disability. London: King's Fund, 2006. [Google Scholar]
- 21. O'Mahony PG, Thomson RG, Dobson R et al. . The prevalence of stroke and associated disability. J Public Health Med 1999; 21(2): 166–71. [DOI] [PubMed] [Google Scholar]
- 25. Smith S, Horgan F, Sexton E et al. . The cost of stroke and transient ischaemic attack in Ireland: A prevalence-based estimate. Age Ageing 2012; 41: 332–8. [DOI] [PubMed] [Google Scholar]
- 26. Wilkins E, Wilson L, Wickramasinghe K et al. . European cardiovascular disease statistics. Brussels: European Heart Network, 2017. [Google Scholar]
- 27. National Audit Office Reducing brain damage: faster access to better stroke care. London: National Audit Office, 2005. [Google Scholar]
- 28. Pollock A, St George B, Fenton M et al. . Top ten research priorities relating to life after stroke. Lancet Neurol 2012; 11: 209. [DOI] [PubMed] [Google Scholar]
- 29. Morris S, Hunter RM, Ramsay AI et al. . Impact of centralising acute stroke services in English metropolitan areas on mortality and length of hospital stay: Difference-in-differences analysis. BMJ 2014; 349: g4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ramsay AI, Morris S, Hoffman A et al. . Effects of centralizing acute stroke services on stroke care provision in two large metropolitan areas in England. Stroke 2015; 46: 2244–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brimblecombe N, Fernandez J-L, Knapp M et al. . Review of the international evidence on support for unpaid carers. J Long-Term Care 2018; 1: 25–40. [Google Scholar]
- 32. Adelman RD, Tmanova LL, Delgado D et al. . Caregiver burden: A clinical review. JAMA 2014; 311: 1052–60. [DOI] [PubMed] [Google Scholar]
- 33. Luengo-Fernandez R, Leal J, Gray A. UK research spend in 2008 and 2012: Comparing stroke, cancer, coronary heart disease and dementia. BMJ Open 2015; 5: e006648. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


