Abstract
Background
Persons with dementia (PwD) need support to remain in their own homes as long as possible. Family caregivers, homecare nurses and general practitioners (GPs) play an important role in providing this support, particularly in rural settings. Assessing caregiver burden is important to prevent adverse health effects among this population. This study analysed perceived burden and needs of family caregivers of PwD in rural areas from the perspectives of healthcare professionals and family caregivers.
Methods
This was a sequential explanatory mixed methods study that used both questionnaires and semi-structured interviews. Questionnaires measuring caregiver burden, quality of life and nursing needs were distributed to the caregivers; health professionals received questionnaires with adjusted items for each group. Additionally, in-depth qualitative interviews were carried out with eight family caregivers.
Results
The cross-sectional survey population included GPs (n = 50), homecare nurses (n = 140) and family caregivers (n = 113). Healthcare professionals similarly assessed the psychosocial burden and stress caused by behavioural disturbances as most relevant. Psychological stress, social burden and disruptive behaviour (in that order) were regarded as the most important factors from the caregivers’ perspective. It was found that 31% of caregivers reported permanent or frequent caregiver overload. Eight themes related to caregiver burden emerged from the subsequent interviews with caregivers.
Conclusions
Professional support at home on an hourly basis was found to be highly relevant to prevent social isolation and compensate for lack of leisure among caregivers of PwD. Improvement of interprofessional dementia-related education is needed to ensure high-quality primary care.
Keywords: caregiver burden, dementia, rural setting, homecare nurses, general practitioners, older people
Key points
The burden of family caregivers of people with dementia (PwD) is multifaceted and it is important to take into account numerous aspects.
Psychological burden is considered the most relevant form of burden by caregivers.
Professional support at home on an hourly basis is needed to prevent overload and adverse health effects.
Enhancing mobility among family caregivers in rural settings could reduce their perceived stress.
Healthcare professionals emphasise the need for improvement in interprofessional cooperation and dementia-related education.
Introduction
Worldwide, approximately 46.8 million people are diagnosed with dementia. By 2050, this number is projected to rise to 131.5 million [1]. The majority of persons with dementia (PwD) live in community settings and receive care from family members and friends [2]. In particular, high-income countries experience an increasing number of PwD related to life expectancy, ageing of the population and improved diagnostic options [3]. As the number of PwD rises, the number of family caregivers will probably increase simultaneously [4]. Due to youth depopulation, the proportion of aged people at risk for dementia is expected to be higher in rural areas compared with urban areas. In addition, rural areas are characterised by limited access to health and social services [5], a circumstance which may be more acute for older people with less mobility. Persons with dementia and their caregivers in rural areas have a considerable unmet need for support due to limited access to metropolitan centres and a lack of dementia specialists such as neurologists or psychiatrists [6, 7]. The Austrian public healthcare system operates a seven-level financial system for people in need of care. The amount of support depends on the extent of the need and is not dependent on income and age. Care recipients are examined by a doctor or nurse and then assessed according to their dependency in a seven-level system. Whether or not a PwD lives in a rural area is not specifically taken into consideration.
Several studies reported that caring for a PwD requires physical, psychological, social and financial resources for caregivers and their families [4, 8, 9]. Furthermore, caregivers of PwD have higher levels of caregiver burden than non-dementia caregivers [10, 11], and studies suggest multifactorial influences on burden in dementia caregiving [12, 13]. Caregiver burden has been identified as a key predictor of long-term care placement among PwD [14]. Thus, identification of relevant dimensions of burden is important to support family caregivers and to prevent early nursing home placement of PwD. Despite the challenges, dementia caregiving also has fulfilling aspects, such as connectedness, a sense of purpose or an experience of personal growth [15, 16].
Because of the demographic characteristic drawbacks and higher prevalence of dementia in rural settings, the role of general practitioners (GPs) and homecare nurses will gain importance with regard to ensuring quality in primary care [1]. To generate a more holistic view of the care situation, the collaboration of GPs, nurses and other health professionals is crucial [17, 18]. Both healthcare professionals and family caregivers are faced with the burdens attributable to caring for PwD. However, literature regarding the perceived needs of family caregivers of PwD in rural areas from the perspective of the family caregivers and healthcare professionals is scarce. [19]. Most studies highlighted caregiver burden and needs from the perspective of either the caregiver, the doctors or the nurses [20, 21].
Furthermore, several studies indicated gaps in GPs’ education on and management of cognitive diseases [22, 23]. Lack of special training and time and other issues such as missing reimbursement in context of rising dementia prevalence places a strain on GPs and other involved healthcare professionals working with PwD and their caregivers [24].
Objective
The objective of the interdisciplinary PAiS study (Pflegende Angehörige von Menschen mit Demenz in Salzburg—Family caregivers of persons with dementia in Salzburg) was to analyse family caregiver burden in a rural–provincial setting from different perspectives. This study therefore investigated attitudes, experiences and opinions regarding family caregiver burden of GPs, homecare nurses and caregivers of PwD in rural areas of Salzburg, Austria, and compared their perspectives.
Furthermore, this study aimed to explore interprofessional cooperation in dementia care between GPs and homecare nurses and to assess their relevant knowledge.
Methods
Design
This was a cross-sectional study that used a sequential explanatory mixed methods design comprising quantitative data and in-depth semi-structured qualitative interviews [25]. The study design emerges from the pragmatism paradigm, which focuses on the consequences of actions, is problem centred, pluralistic and real-world practice oriented [25].
Surveys of family caregivers of PwD, GPs and homecare nurses were conducted in rural areas of Salzburg between November 2016 and May 2017. Pre-tests of all questionnaires and instruments were performed within regions in Austria comparable to the rural area of Salzburg.
Instruments
Family caregivers, GPs and homecare nurses were administered questionnaires containing group-specific items to capture their perspectives on the burden of family caregivers of PwD, quality of life (QoL) among the family caregivers and limits of care at home regarding early nursing home placement. In an open-ended question, GPs and nurses were asked about one or more special qualification concerning dementia and/or geriatric psychiatry. Dependency among PwD was explored with the Barthel Index, which was used to assess activities of daily living (ADL) [26], and the Nurses’ Observation Scale for Geriatric Patients (NOSGER), which was used to evaluate the cognitive and behavioural aspects of PwD [27]. The Barthel Index assesses 10 daily activities with differently weighted scores that sum up to a total score of 100 (representing complete independence on all daily activities). Lower scores indicate higher dependency levels. The NOSGER consists of 30 items covering 6 dimensions represented by 5 items each. Each item is measured on a 5-point scale, and the scores for each subscale range from 5 to 25 points, with higher values indicating greater impairment. The subjective burden of family caregivers was analysed with the short version of the Burden Scale for Family Caregivers (BSFC-s) [28]. The overall QoL and general health of family caregivers were evaluated according to the EUROHIS-QOL [29]. The 10 items of the BSFC-s are rated on a 4-point scale (‘strongly disagree’ to ‘strongly agree’) with higher scores indicating greater caregiver burden. The EUROHIS-QOL is a self-assessment measure with eight items measured on a 5-point scale, each with higher scores representing a higher overall QoL. Our survey recorded the level of care allowance received by the PwD.
Sampling
Samples for GPs, homecare nurses and the family caregivers were drawn from rural areas in Salzburg. Rural areas are defined on the basis of their degree of urbanisation typology by the European Commission [30] as either intermediate or thinly populated areas. Of the 119 local administrative units of Salzburg, only the city of Salzburg is excluded as a densely populated area.
The sampling strategy differed significantly across the three samples. The sampling of GPs was public register-based. All 172 GPs in Salzburg received a postal paper-and-pencil questionnaire. Nurses were recruited through homecare nursing services organisations. Coordinators of these services distributed the self-administered paper-and-pencil questionnaires among their homecare nurses, collected the completed questionnaires and returned the questionnaires. Homecare nurses were asked to identify family caregivers and inform them via an information letter about the project, and the study was promoted through mass media and other channels. GPs were requested to inform family caregivers of PwD among their patients about the study. Family caregivers were provided with the self-administered paper-and-pencil questionnaire and a free return envelope. The survey mode was selected according to the requirements of the caregivers. Self-administered paper-and-pencil questionnaires seem particularly useful as the respondents are free from any pressure to respond and can take breaks as needed, e.g. to address spontaneous needs of the PwD.
Semi-structured interviews were conducted with a convenience sample of eight caregivers of PwD. Eligible interview partners were recruited from a sample of caregivers who voluntarily responded to the public invitation for study participation. All interviews were conducted by one of two experienced members of the study team. The guideline-based qualitative interviews included four topics: challenges in caregiving and experiences providing care; availability and utilisation of and satisfaction with local healthcare services; subjective opinion about interprofessional teamwork of GPs and homecare nurses and suggestions for improvement.
Analysis
Quantitative data were analysed using IBM SPSS Statistics v. 23.0 (IBM Corp., Armonk, NY, USA). We restricted our statistical analysis to descriptive measures to compare results of GPs, homecare nurses and family caregivers because we lacked data to cross validate our samples. The qualitative interviews were audiotaped, transcribed and anonymised. The transcripts were transferred to the qualitative data software MAXQDA (VERBI Software, Berlin, Germany), and the qualitative data material was analysed following thematic analysis according to Mayring, using the summarising approach with a combination of inductive category development and deductive category application. It aims to reduce the material in a manner to preserve essential content and create a manageable corpus by abstraction, which represents the basic material [31].
To triangulate findings form the quantitative and the qualitative branch of the study, a mixed methods matrix [32] (see Figure 1) was used for data integration.
Figure 1 .
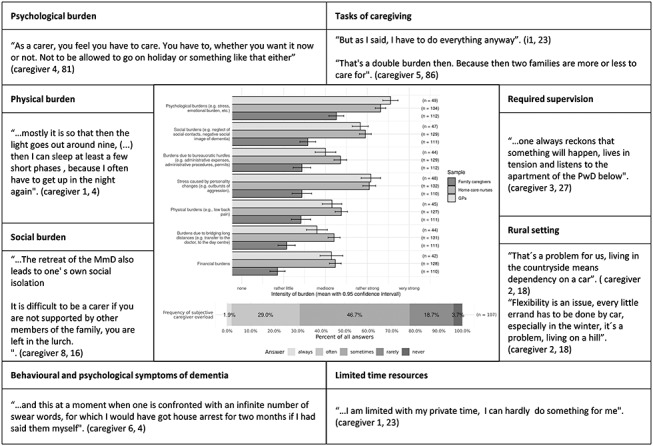
Overview of caregiver burden and potential overload from different perspectives: integration of the quantitative–qualitative data (mixed methods matrix).
Results
We received 55 questionnaires from GPs and excluded GPs from the city of Salzburg, GPs with private practices and those with patients in nursing homes only. In sum, the final sample consisted of 50 GPs from rural areas in Salzburg (response rate 29%). A total of 140 homecare nurses completed the survey, and we received 113 eligible and completed questionnaires from family caregivers.
Comparison of homecare nurses and GPs (see Table 1) showed that 36% (n = 18) of GPs were female and more than 90% (n = 130) of the nurses were female. Over 50% (n = 47) of GPs reported having extensive experience in caring for patients with dementia with an average of 23 patients per physician (22.6  16.1). Homecare nurses were caring for an average number of nine PwD (8.8
16.1). Homecare nurses were caring for an average number of nine PwD (8.8 7.5), which represents 20–30% of all their clients.
7.5), which represents 20–30% of all their clients.
Table 1 .
Sociodemographic characteristics of homecare nurses and general practitioners.
| Homecare nurses (n = 140) | GP (n = 50) | |
|---|---|---|
| Gender | ||
| Male | 10 (7.1%) | 32 (64%) |
| Female | 130 (92.9%) | 18 (36%) |
| Age | ||
| Under 30 years | 13 (9.3%) | 0 (0%) |
| 30–45 years | 56 (40%) | 10 (20%) |
| 46–60 years | 69 (49.3%) | 33 (66%) |
| Over 60 years | 2 (1.4%) | 7 (14%) |
| Professional experience | ||
| Under 5 years | 19 (13.7%) | 5 (10%) |
| 6–10 years | 22 (15.8%) | 12 (24%) |
| 11–20 years | 42 (30.2%) | 10 (20%) |
| Over 20 years | 56 (40.3%) | 23 (46%) |
| Number of dementia patients in care | ||
| Mean (SD) | 8.8 (7.5) | 22.6 (16.1) |
| Contact to family caregivers | ||
| Mean (SD) | 8.5 (8.3) | 23.3 (16.9) |
Specific knowledge and education with regard to geriatrics were reported by 44% (n = 22) of the GPs; however, only half of these (n = 11) indicated that their training included dementia-specific education in the open-ended responses and the other half (n = 11) indicated that their training included education in related topics like palliative care or psycho-social medicine. Only 9% (n = 12) of the homecare nurses reported having special training in geriatrics. The majority of caregivers in our study had been caring for a close family member for an average (SD) of 4.6 (4.0) years, spending an average (SD) of 7.5 (7.9) hours per day providing care (Table 2). In general, 83% (n = 94) of carers received informal support from other individuals, primarily from other family members (64%, n = 60). Of all included caregivers, 60% (n = 64) used homecare nursing services, 13% (n = 14) used 24-hour live-in care and 17% (n = 20) received no additional formal or informal help. Most respondents (82%, n = 92) lived in areas with less than 15,000 inhabitants. Sixty-one percent (n = 70) of caregivers were living in the same household with the PwD. The average distance (SD) for caregivers who were not living in the same household with the PwD was 31.8 (50.7) km by public transportation and 28.6 (41.7) km by car.
Table 2 .
Sociodemographic characteristics of family caregivers and patients with dementia
| Family caregivers (n = 113) | Interviewed caregivers (n = 8) | PwD (n = 115) | |
|---|---|---|---|
| Gender | |||
| Male | 27 (23.9%) | 36 (32.4%) | |
| Female | 86 (76.1%) | 8 | 75 (67.6%) |
| Age | |||
| Mean (SD) | 60.7 (14.9) | 57.7 | 83 (8.2) |
| Marital status | |||
| Married/cohabitation | 84 (74.3%) | 6 | 50 (44.2%) |
| Separated/divorced | 19 (16.8%) | 1 | 5 (4.4%) |
| Widowed | 3 (2.7%) | 1 | 54 (47.8%) |
| Single | 7 (6.2%) | 4 (3.5%) | |
| Population at place of residence | |||
| Less than 2,000 | 7 (6.5%) | 9 (8.3%) | |
| 2,001–5,000 | 43 (40.2%) | 41 (38%) | |
| 5,001–10,000 | 17 (15.9%) | 21 (19.4%) | |
| 10,001–15,000 | 18 (16.8%) | 20 (16.7%) | |
| 15,001–20,000 | 10 (6.5%) | 9 (5.6%) | |
| 20,001 or more | 17 (14%) | 15 (12%) | |
| Barthel Index (BI) | |||
| Mean (SD) | 66.56 (25.29) | ||
| NOSGER | |||
| Dimension memory mean (SD) | 16.59 (3.69) | ||
| Dimension disturbing behaviour mean (SD) | 10.16 ± 3.19 | ||
| BSFC-s | |||
| Mean (SD) | 13.59 (7.56) | ||
| EUROHIS-QOL | |||
| Mean (SD) | 3.71 (0.63)c | ||
| Employment status | |||
| Retired | 56 (50%) | 4 | |
| Full time employed | 23 (20.7%) | 1 | |
| Part time employed | 24 (21.4%) | 3 | |
| Housewife/househusband | 16 (14.3%) | ||
| In education | 1 (0.9%) | ||
| Unemployed | 3 (2.7%) | ||
| Monthly netto household income (€) | |||
| Less than 1,000 | 29 (30.5%) | ||
| 1,001–1,500 | 24 (25.3%) | ||
| 1,501–2,000 | 23 (24.2%) | ||
| 2,001–2,500 | 13 (13.7%) | ||
| 2,501–4,000 | 6 (6.3%) | ||
| Relationship with the care recipient | |||
| Spouse or partner | 36 (31.9%) | 2 | |
| Mother/father | 52 (46%) | 6 | |
| Brother/sister | 2 (1.8%) | ||
| Daughter/son | 7 (6.2%) | ||
| Daughter/son in law | 2 (1.8%) | ||
| Grandfather/grandmother | 7 (6.2%) | ||
| Friend | 7 (6.2%) | ||
| Proximity to patient | |||
| Lives in same house | 70 (60.9%) | 5 | |
| Caregiving duration (years) | |||
| Mean (SD) | 4.6 (4.0) | 4.6 | |
| Caregiving h/day | |||
| Mean (SD) | 7.5 (7.9) | 9.5 | |
| Caregiving d/week | |||
| Mean (SD) | 5.7 (2.0) | 7 | |
| Home nursing service | 64 (59.8%) | ||
Forty percent of the PwD were categorised as ‘independent’ based on the results of the self-care assessment using Barthel Index [26]. The remaining PwD were categorised as partly or fully dependent (Table 2). Most PwD in our study were categorised as level 3 recipients of the Austrian public care allowance system.
Cognitive impairment and behavioural disorders were assessed using the NOSGER scale. In this study, the mean (SD) score for the NOSGER subscale ‘disturbing behaviour’ was 10.16 (3.19) and for the NOSGER subscale ‘memory’ was 16.72 (3.62), both above the clinical cut-off score [27].
Caregiver burden from different perspectives
GPs, homecare nurses and family caregivers provided information on identical items measuring the perceived burden of family caregivers of PwD (Figure 1). In general, GPs and homecare nurses shared a similar perspective on the burden of family caregivers. However, the family caregivers themselves reported slightly lower levels of burden in all dimensions. All three groups considered psychological burden to be the most severe form of burden. On average, the GPs and the homecare nurses perceived the psychological burden placed on caregivers to be between ‘severe’ and ‘rather severe’, whereas caregivers themselves reported only mediocre burden.
In addition, GPs and homecare nurses identified stress caused by personality changes and social burden as the two dominant stress dimensions with a ‘rather strong’ or ‘very strong’ intensity. Both groups considered physical burden, financial burden and burden due to long distances or bureaucratic hurdles as mediocre with little differences in their evaluations; however, homecare nurses perceived these four burdens as slightly more severe compared with GPs.
Beyond psychological burden, the majority of family caregivers considered social burden, bureaucratic hurdles, stress due to personality changes and physical burden as significantly less pronounced and as between rather little and mediocre burden on average. From the perspective of the family caregivers, psychological burden, social burden and stress caused by personality changes were the dominant three stress dimensions; 31% reported a permanent or at least frequent feeling of caregiver overload. Social stress, the feeling of overload and captivity in the caregiver role were particularly accented in the interviews (overview of all dimensions see Figure 1).
Interprofessional cooperation from different perspectives
Eighty-four percent of GPs and 76% of homecare nurses agreed that improvement in interprofessional communication and teamwork were desirable. The main problems identified were missing interprofessional education (70% [n = 35] and 82% [n = 104], respectively), lack of time (63% [29] and 82% [109], respectively) and lack of remuneration (35% [17] and 60% [69], respectively).
Eighty-six percent (n = 84) of caregivers indicated the communication with the GPs as ‘good’ or even ‘very good’. Ninety-seven percent (n = 64) of caregivers indicated the communication with homecare nurses as ‘good’ or even ‘very good’. Communication with psychiatrists and neurologists was evaluated as ‘good’ or even ‘very good’ by the majority of caregivers. When asked whether a homecare nursing service was available, 86% (n = 92) of the caregivers responded affirmatively and almost 100% (n = 108) indicated that a GP was available locally. However, almost 30% (n = 26) of family caregivers reported a regional lack of dementia specialists, such as neurologists or psychiatrists.
Family caregivers’ perceived experiences
The results of the qualitative component of the study revealed that caregivers distinguish between different dimensions of caregiver burden. Eight broad subthemes related to the multifaceted nature of caregiver strain emerged from the analysis: physical, psychological and social burden, rural setting, required supervision, limited time resources, tasks of caregiving and behavioural symptoms of dementia (Figure 1).
During the interviews, family caregivers frequently reported feeling as if their social life was being limited by the social withdrawal of the PwD. Caregiver overload and role captivity were also common among the interviewees. Another reported challenge was the constant need for vigilance and supervision in caring for the PwD. A key theme in the interviews was the support offered by family members: lack of help and social reward from loved ones increased perceived caregiver burden and were described as a source of conflict between family members. Rurality and long distances were not directly linked with caregiver burden, but the issue of mobility was discussed in the interviews. With regard to mobility, some interviewees expressed a sense of dependency on driving.
Caregivers also reported on nocturnal care tasks, which has a particular impact on their recreation. Caregivers who do not cohabit with the PwD also spend extra time travelling to and from the PwD’s home and perceive the care for two households or families as an additional burden. Regarding the cooperation with professionals, the caregivers particularly talked about their experiences with the GPs. It was positively noted that the GPs acknowledge the caregiver in their role and inquire about their well-being. It was also observed, however, that GPs lack dementia-specific knowledge resulting in unnecessary referrals of PwD to specialists.
The general practitioners, as I said, there are some who make an incredible effort, some who simply say immediately, you don’t need to call me that’s something for the medical officer anyway. They’re overwhelmed, too (caregiver 6, 60).
Above all, the caregivers wished for the possibility of spontaneous respite care as a recommendation for improvement. One caregiver wished for more recognition from politics and society. In addition to the challenges of caring, the interviewees also described caregiver gain: the gratitude of the PwD, the stronger family cohesion due to the care for the PwD, the opportunity to give something good back to the PwD and the knowledge that providing care at home is in the PwD’s interest. The knowledge acquired also helps to better understand the needs of PwD and to cope with difficult situations in caring for the PwD, e.g. challenging behaviour is perceived as a symptom of dementia and should not be taken personally.
I’ve always said to myself and my husband, remember, he [the PwD] is suffering from dementia. We must not take that personally (caregiver 5, 37).
Discussion
This study analysed the burden of family caregivers of PwD in a rural setting from different perspectives. Psychological burden was considered to be the most pronounced form of burden by all groups. However, beyond the congruence in this perception, the evaluation differed in severity of the burden and the relevance of the other dimensions between healthcare professionals and family caregivers of PwD. Physical and social burden, stress due to behavioural changes and burden due to bureaucratic hurdles were also considered relevant by family caregivers, whereas GPs and nurses considered burden caused by behavioural changes and social strain particularly strong. Remarkably, GPs and homecare nurses tended to assess caregiver burden more severely than caregivers themselves who put the main emphasis on other dimensions, although 31% of caregivers experienced overload often or very often in their role. There can be manifold reasons for these results. One reason could be the fact that the majority of PwD in this study were categorised as ‘independent’ or only ‘partly dependent’ in the self-care assessment and were therefore apparently in quite good physical condition. The gap of the reported burden between healthcare professionals and caregivers could also have age-related reasons. The findings suggest that life satisfaction in people over the age of 85 is significantly associated with mental health and loneliness and hardly with physical health [33]. Furthermore, the caregiving role should not only be perceived as a burden but can also be an experience of emotional reward and satisfaction. Spousal carers of PwD reported strengthening of their relationship and a higher purpose in life [34, 35]. The caregivers in our interviews also reported on positive aspects of caring for the PwD, especially when the entire family works together.
The focus of this study was on the rural provincial area because most studies related to this topic were performed in urban areas. In a Swedish study comparing caregiver burden of PwD in urban and rural areas, the authors observed a higher financial burden in people living in rural areas, whereas urban caregivers had less support from family members [21]. This finding may be related to differences in availability of services. Another study did not find a significant difference in caregiver distress and burden between urban and rural areas, although caregivers in rural areas may have had more difficulty accessing the services of specialised dementia institutions [7]. Our findings do not suggest a particularly strong burden related to the rural environment reported by the caregivers themselves. Further studies need to be carried out in order to validate this observation.
Median length of day care (7.5 hours per day) spent by the caregivers was comparable to other study results, which revealed daily length of providing care as one of the most consistent predictors of caregiver burden and depression [36]. Although the PwDs in our study appeared to be in good physical condition, a lot of time had to be spent on care. It is well known that supervision services are very time-consuming, especially for mobile dementia patients. This expenditure of time is not included in the classic nursing services and is also not reflected in the Barthel Index. Since these services are not taken into account in the Austrian care allowance system either, they are not financially remunerated. Another notable result was that caregivers did not consider financial strain to be very relevant. This is all the more intriguing because the majority were retired and had low income. This finding may be due to the recruitment strategy because many family caregivers in our study had professional support (107/113) and therefore most likely a more comfortable financial situation. However, this result does not reflect the common point of view or the results from previous studies [37]. An obligatory general care insurance is currently an issue of political debate in Austria, because not everyone can afford professional homecare services.
Another aim of this study was to explore interprofessional cooperation in dementia care between GPs and homecare nurses and to assess their knowledge. As several other authors have reported, primary care physicians often lack special education concerning dementia diseases, although they play a pivotal role in caring for PwD and their relatives. A French study identified gaps in GPs training regarding diagnosis and managing behavioural disorders in patients with Alzheimer’s disease. Other authors have reported that <50% of GPs have satisfactory knowledge about dementia diagnosis and management [22, 23]. The lack of healthcare services and specialists in rural areas increases the pressure on GPs providing high-quality care for dementia patients [38]. GPs and other primary healthcare professionals face time constraints and limited personnel and financial resources in their daily practice. Although we did not systematically check the specific knowledge of GPs, only a minority of included GPs (22%) reported having undergone special training related to dementia. This situation was even more apparent for homecare nurses (8.6%). The insufficient training of health professionals with regard to dementia could also be one reason why the caregiver burden was assessed differently. From our point of view, high-quality medical teaching would be important in order to learn how to deal with challenging behaviour in dementia care. Family caregivers of PwD with severe behavioural disorders, in particular, need support, but this can only be provided by well-qualified professionals.
The PAiS study emphasises the importance of interprofessional teamwork, particularly in rural areas. The collaboration of different healthcare professionals in dementia care seems desirable and can aid in the sharing of knowledge and skills [38]. This collaboration would also strengthen the role of primary care networks, which would gain importance in the dementia care system [1]. The results of the PAiS study suggest that there are different points of view among family caregivers, homecare nurses and GPs regarding family caregiver burden. Furthermore, the importance of vigilance for the needs and resources of caregivers is highlighted. Caregivers reported good communication and teamwork with nurses and GPs, which can be seen as a resource. The research has also shown that health professionals expressed the wish for interprofessional education and financial remuneration for non-conventional care services like conversation or activity.
The perceived burden of caregivers was not particularly related to the rural environment, but simply to the dependency on a car. It can therefore be assumed that supporting family caregivers in their mobility would reduce their perceived stress. The study revealed that carers in rural areas wish for respite care for temporary flexible relief. As an essential finding of our study, it should be taken seriously that psychological strain was considered by all three respondent groups to be the most stressful dimension.
Strengths and limitations
This study has several limitations. First, the diagnosis of dementia was not based on medical records but on family caregivers’ reports of symptoms. It cannot be ruled out that a few caregivers were providing care to a family member suffering from conditions other than dementia. Second, the response rate of homecare nurses and family caregivers was not documented due to the sampling strategy. Besides the recruiting difficulties, there was a lack of information on homecare nurses and family caregivers in rural areas of Salzburg to validate our sample. This study is the first to survey caregivers in the rural areas of Salzburg and caregivers and PwD are insufficiently captured in register data. The family caregiver and homecare nurse samples are non-random samples of rural areas of Salzburg with a probability of sampling bias. Therefore, the results need to be interpreted with caution. For future research, it would be beneficial to use the general population as sampling frame and apply a random sampling strategy to provide reliable prevalence figures. To avoid method effects across the samples, self-administered paper-and-pencil questionnaires were used for all samples, although for the GPs and homecare nurses, alternative modes like online surveys or telephone interviews might have been a reasonable alternative. In addition, 60% of our caregivers received help from homecare nurses, which is rather high and of course contributes to relief of the burden. This may explain why caregiver burden was not as high as expected.
Despite these limitations, the present study has some notable strengths. This study is one of the first to investigate the three different perspectives of groups involved in dementia caregiving including GPs and nurses and, therefore, provides a more holistic view on the issue. The chosen mixed methods approach with in-depth qualitative interviews provides a more profound understanding of the multifaceted stress dimensions of dementia caregiving.
Conclusion
This study emphasises the need for an increased offer of respite care for PwD in rural areas to relieve family caregivers’ strain. Dementia-specific interprofessional training and education should be strengthened for GPs and other healthcare professionals who are involved in the dementia care in primary care. In addition, Austria would benefit from the development of advanced professional nursing roles, such as the community health nurse, who have long since worked with families and across generations to support the families affected by dementia to live well in the community setting [18].
Acknowledgements
We would like to express our appreciation of and thanks to the participants for their contribution to the study. We also would like to thank Detlef Ruesing for support and guidance, and Antje van der Zee-Neuen for her thoughtful review of content.
Declaration of Conflict of Interest
None.
Declaration of Funding
Stifterverband für die Deutsche Wissenschaft e.V.
Ethical approval
Ethical approval was obtained from the local ethics committee of Salzburg County, Austria (ID: 415-E/2055/4-2016).
Trial registration
The study is registered in the German Clinical Trials Register (ID:DRKS00014749).
References
- 1. Prince M, Comas-Herrera A, Knapp M, Guerchet M, Karagiannidou M. World Alzheimer Report 2016: Improving Healthcare for People Living with Dementia: Coverage, Quality and Costs Now and in the Future. London: Alzheimer’s Disease International (ADI), 2016. [Google Scholar]
- 2. Prince M, Prina M, Guerchet M. World Alzheimer Report 2013. Journey of Caring. An Analysis of Long-Term Care for Dementia. Alzheimer’s Disease International, 2013. [Google Scholar]
- 3. Satizabal CL, Beiser AS, Chouraki V, Chêne G, Dufouil C, Seshadri S: Incidence of dementia over three decades in the Framingham heart study. N Engl J Med 2016; 374:523–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chiao CY, Wu HS, Hsiao CY: Caregiver burden for informal caregivers of patients with dementia: A systematic review. Int Nurs Rev 2015; 62:340–50. [DOI] [PubMed] [Google Scholar]
- 5. Morgan D, Innes A, Kosteniuk J: Dementia care in rural and remote settings: a systematic review of formal or paid care. Maturitas 2011; 68:17–33. [DOI] [PubMed] [Google Scholar]
- 6. Morgan DG, Semchuk KM, Stewart NJ, D'Arcy C: Rural families caring for a relative with dementia: Barriers to use of formal services. Soc Sci Med (1982) 2002; 55:1129–42. [DOI] [PubMed] [Google Scholar]
- 7. O'Connell ME, Germaine N, Burton R, Stewart N, Morgan DG: Degree of rurality is not related to dementia caregiver distress, burden, and coping in a predominantly rural sample. J Appl Gerontol 2013; 32:1015–29. [DOI] [PubMed] [Google Scholar]
- 8. Dauphinot V, Delphin-Combe F, Mouchoux C, Dorey A, Bathsavanis A, Makaroff Z, Rouch I, Krolak-Salmon P: Risk factors of caregiver burden among patients with Alzheimer's disease or related disorders: a cross-sectional study. J Alzheimer's Dis 2015; 44:907–16. [DOI] [PubMed] [Google Scholar]
- 9. Kim H, Chang M, Rose K, Kim S: Predictors of caregiver burden in caregivers of individuals with dementia. J Adv Nurs 2012; 68:846–55. [DOI] [PubMed] [Google Scholar]
- 10. Brodaty H, Donkin M: Family caregivers of people with dementia. Dialogues Clin Neurosci 2009; 11:217–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ory MG, HoffmanRR, 3rd, Yee JL, Tennstedt S, Schulz R: Prevalence and impact of caregiving: a detailed comparison between dementia and nondementia caregivers. Gerontologist 1999; 39:177–85. [DOI] [PubMed] [Google Scholar]
- 12. Pearlin LI, Mullan JT, Semple SJ, Skaff MM: Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 1990; 30:583–94. [DOI] [PubMed] [Google Scholar]
- 13. Campbell P, Wright J, Oyebode J, Job D, Crome P, Bentham P, Jones L, Lendon C: Determinants of burden in those who care for someone with dementia. Int J Geriatr Psychiatry 2008; 23:1078–85. [DOI] [PubMed] [Google Scholar]
- 14. Stephan A, Afram B, Koskenniemi J, Verbeek H, Soto ME, Bleijlevens MH, Sutcliffe C, Lethin C, Risco E, Saks Ket al . Older persons with dementia at risk for institutionalization in eight European countries: a cross-sectional study on the perceptions of informal caregivers and healthcare professionals. J Adv Nurs 2015; 71:1392–404. [DOI] [PubMed] [Google Scholar]
- 15. Egilstrod B, Ravn MB, Petersen KS. Living with a partner with dementia: a systematic review and thematic synthesis of spouses' lived experiences of changes in their everyday lives. Aging Ment Health 2018; 1–10. [DOI] [PubMed] [Google Scholar]
- 16. Todorova I, Turner H, Castaneda-Sceppa C, Young D, Bonner A. "I Do It With love": Engagement in caring for people with dementia. Global Qual Nurs Res 2016; 3: 2333393616668634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hämel K, Vössing C: The collaboration of general practitioners and nurses in primary care: a comparative analysis of concepts and practices in Slovenia and Spain. Prim Health Care Res Dev 2017; 18:492–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dening KH, Hibberd P: Exploring the community nurse role in family-centred care for patients with dementia. Br J Commun Nurs 2016; 21:198–202. [DOI] [PubMed] [Google Scholar]
- 19. Behrman S, Wilkinson P, Lloyd H, Vincent C: Patient safety in community dementia services: What can we learn from the experiences of caregivers and healthcare professionals? Age Ageing 2017; 46:518–21. [DOI] [PubMed] [Google Scholar]
- 20. Hirakawa Y, Chiang C, Aoyama A: A qualitative study on barriers to achieving high-quality, community-based integrated dementia care. J Rural Med 2017; 12:28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ehrlich K, Bostrom AM, Mazaheri M, Heikkila K, Emami A: Family caregivers' assessments of caring for a relative with dementia: a comparison of urban and rural areas. Int J Older People Nurs 2015; 10:27–37. [DOI] [PubMed] [Google Scholar]
- 22. Somme D, Gautier A, Pin S, Corvol A. General practitioner's clinical practices, difficulties and educational needs to manage Alzheimer's disease in France: analysis of national telephone-inquiry data. BMC Fam Pract 2013; 14: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pathak KP, Montgomery A: General practitioners' knowledge, practices, and obstacles in the diagnosis and management of dementia. Aging Ment Health 2015; 19:912–20. [DOI] [PubMed] [Google Scholar]
- 24. Parmar J, Dobbs B, McKay R, Kirwan C, Cooper T, Marin A, Gupta N; Diagnosis and management of dementia in primary care: exploratory study. Can Fam Physician (Medecin de famille canadien) 2014; 60:457–65. [PMC free article] [PubMed] [Google Scholar]
- 25. Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research, 2nd edition. Thousand Oaks, CA: Sage, 2011. [Google Scholar]
- 26. Sinoff G, Ore L. The Barthel activities of daily living index: self-reporting versus actual performance in the old-old (> or = 75 years). J Am Geriatr Soc 1997; 45:832–6. [DOI] [PubMed] [Google Scholar]
- 27. Spiegel R, Brunner C, Ermini-Funfschilling D, Monsch A, Notter M, Puxty J, Tremmel L: A new behavioral assessment scale for geriatric out- and in-patients: the NOSGER (Nurses' observation scale for geriatric patients). J Am Geriatr Soc 1991; 39:339–47. [DOI] [PubMed] [Google Scholar]
- 28. Graessel E, Berth H, Lichte T, Grau H. Subjective caregiver burden: validity of the 10-item short version of the burden scale for family caregivers BSFC-s. BMC Geriatr 2014; 14: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brähler E, Mühlan H, Albani C, Schmidt S. Teststatistische Prüfung und Normierung der deutschen Versionen des EUROHIS-QOL Lebensqualität-index und des WHO-5 Wohlbefindens-index. Diagnostica 2007; 53:83–96. [Google Scholar]
- 30. Dijkstra L, Poelman H. A harmonised definition of cities and rural areas: the new degree of urbanisation. In: Working Paper 01/2014 of the European Commission, 2014.
- 31. Mayring P. Qualitative Inhaltsanalyse. In: Grundlagen und Techniken, 12th edition. Beltz Verlag: Weinheim/Basel, 2015. [Google Scholar]
- 32. O'Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010; 341: c4587. [DOI] [PubMed] [Google Scholar]
- 33. Puvill T, Lindenberg J, de Craen AJ, Slaets JP, Westendorp RG: Impact of physical and mental health on life satisfaction in old age: A population based observational study. BMC Geriatr 2016, 16:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lloyd J, Patterson T, Muers J: The positive aspects of caregiving in dementia: a critical review of the qualitative literature. Dementia (London) 2016, 15:1534–61. [DOI] [PubMed] [Google Scholar]
- 35. Polenick CA, Sherman CW, Birditt KS, Zarit SH, Kales HC. Purpose in life among family care partners managing dementia: links to caregiving gains. Gerontologist 2018, 59, e424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA 2014, 311:1052–60. [DOI] [PubMed] [Google Scholar]
- 37. Williams AM, Forbes DA, Mitchell J, Essar M, Corbett B. The influence of income on the experience of informal caregiving: Policy implications. Health Care Women Int 2003; 24:280–91. [DOI] [PubMed] [Google Scholar]
- 38. Kosteniuk J, Morgan D, Innes A, Keady J, Stewart N, D'Arcy C, Kirk A. Who steers the ship? Rural family physicians' views on collaborative care models for patients with dementia. Prim Health Care Res Dev 2014; 15:104–10. [DOI] [PubMed] [Google Scholar]


