Abstract
A tarsal coalition is an abnormal connection between two or more tarsal bones caused by failure of mesenchymal segmentation.
The two most common tarsal coalitions are calcaneonavicular coalition (CNC) and talocalcaneal coalition (TCC). Both CNC and TCC can be associated with significant foot and ankle pain and impaired quality of life; there may also be concomitant foot and ankle deformity.
Initial, non-operative management for symptomatic tarsal coalition commonly fails, leaving surgical intervention as the only recourse.
The focus of this article is to critically describe the variety of methods used to surgically manage CNC and TCC. In review of the pertinent literature we highlight the ongoing treatment controversies in this field and discuss new innovations.
The evidence-based algorithmic approach used by the authors in the management of tarsal coalitions is illustrated alongside some clinical pearls that should help surgeons treating this common, and at times complex, condition.
Cite this article: EFORT Open Rev 2020;5:80-89. DOI: 10.1302/2058-5241.5.180106
Keywords: interposition graft, surgical resection, tarsal coalition
Introduction
A tarsal coalition is an aberrant connection between two of more tarsal bones. It occurs as a result of lack of mesenchymal segmentation of these tarsal bones due to an embryological failure of joint cleft development. Whilst the true incidence of tarsal coalition is unknown, estimates vary from 1% to 13%,1,2 thereby making it one of the commonest foot and ankle pathologies in children. Coalitions are bilateral in approximately 50% of cases, and there is a heritable component to their development.3,4
Over 90% of coalitions are either calcaneonavicular coalitions (CNC) or talocalcaneal coalitions (TCC),5 although other sites have been described in the literature including cuboid-navicular,6 calcaneocuboid,7 talonavicular,8 navicular-medial cuneiform9 and cuneiform metatarsal.10 The coalition itself can be classified on underlying pathoanatomy into fibrous, cartilaginous and bony coalitions. Soft tissue coalitions may ossify as patients enter adolescence and it is often at this time that they become symptomatic. Diagnosis is usually made with plain radiographs of the foot and ankle, magnetic resonance imaging (MRI) and computed tomography (CT) scan are useful advanced imaging techniques to further define the pathology.
Tarsal coalitions can cause significant foot and ankle pain as well as deformity and loss of function. In these cases, non-operative treatment is initially favoured, commonly in the form of analgesia, immobilization and activity modification. In the authors’ experience, non-operative treatment rarely results in significant, durable improvement of clinical symptoms. Therefore, we are of the belief that most tarsal coalitions that become symptomatic will ultimately require surgical management. The focus of this review is to describe the approach to the surgical management of tarsal coalitions in the paediatric population. Important considerations will be taken of preoperative planning, surgical techniques and outcomes for the most prevalent coalitions – those affecting the CNC and TCC articulations.
Calcaneonavicular coalitions
Calcaneonavicular coalitions are the most common form of coalition,5 and often present with pain in the sinus tarsi region. Patients may present with a rigid flat, or cavus foot, but significant deformity is uncommon. Diagnosis is often made on the oblique foot radiograph where it may be possible to see the abnormal connection between the os calcis and the navicular as well as the so-called ‘anteater nose sign’,11 caused by a prominent elongated anterior process of the os calcis (Fig. 1). The ‘reverse anteater sign’ is observed on either the oblique or anteroposterior (AP) radiograph and represents the navicular extending further posteriorly and laterally than normal.12
Fig. 1.

Calcaneonavicular coalition on standing oblique radiograph, with ‘anteater sign’ highlighted.
Surgical resection of calcaneonavicular coalitions was first reported by Badgley in 1927,13 and numerous other techniques have been subsequently described. In recent years arthroscopic resection has been attempted, with the purported benefits being a more aesthetic scar, quicker recovery and equivalent recurrence rates compared to open surgery.14,15 The accepted gold standard, however, remains open surgical resection of the coalition and interposition graft. It is rare that such bars present with a foot deformity requiring realignment procedures alongside the resection. The open approach is that preferred by the authors and is described in detail below, alongside potential pitfalls which could affect clinical outcomes.
Surgical resection of calcaneonavicular coalition with fat interposition
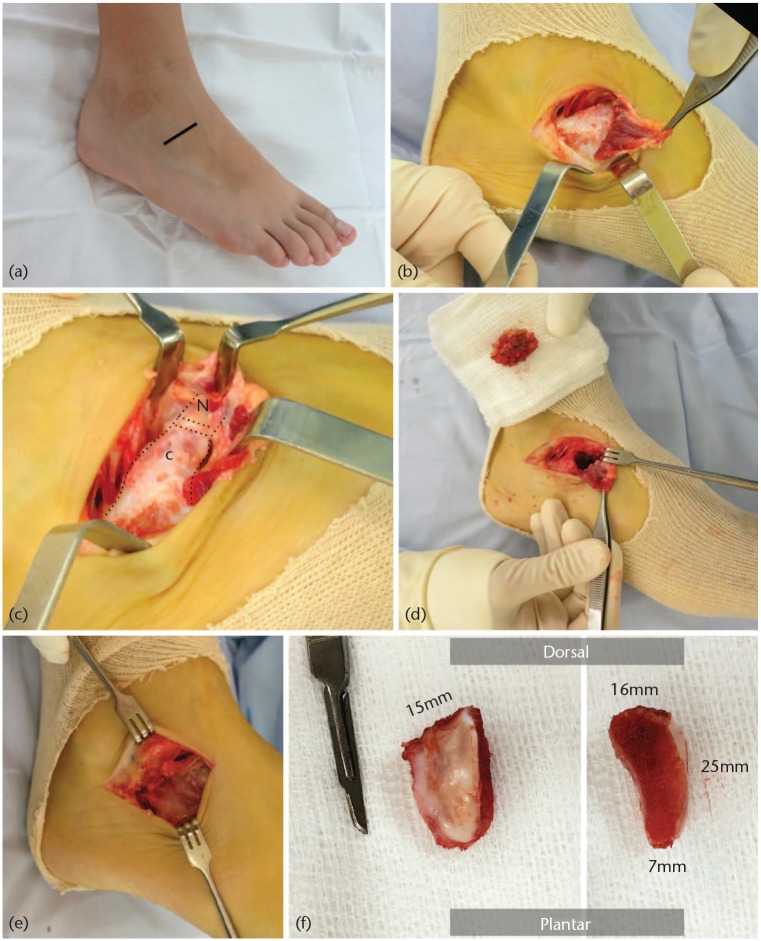
Surgery is undertaken with the patient supine, under general anaesthesia, with a thigh tourniquet and prophylactic antibiotics given at induction. To allow adequate access to the sinus tarsi, a ‘bump’ is placed under the ipsilateral buttock to internally rotate the lower limb. Surgery is performed on a radiolucent table and fluoroscopy is used throughout the procedure. The procedure is illustrated in Fig. 2.
Fig. 2.
Surgical technique for calcaneonavicular coalition excision: (a) Ollier’s incision, (b) mobilizing extensor digitorum brevis (EDB), (c) the calcaneonavicular coalition, (d) defect post coalition resection and fat interposition graft, (e) repair of EDB origin, (f) resected specimen.
An oblique lateral Ollier’s approach over the sinus tarsi is undertaken, tailoring the skin incision to the skin creases to optimize the aesthetics. Care is taken to avoid the sural nerve and peroneal tendons at the lower part of the incision and branches of the superficial peroneal nerve at the upper part of the incision. The fascia overlying extensor digitorum brevis (EDB) is incised and EDB is detached from its proximal origin and mobilized distally. Fluoroscopy is used to help define the extent of the resection and confirm adequate resection. Freer elevators are placed into the talonavicular joint (to protect the head of the talus), and between the coalition and the cartilage of the lateral cuneiform-cuboid joint, respectively. The calcaneonavicular coalition is resected using 5 mm and 10 mm Lambotte osteotomes. Fat is harvested from the proximal medial thigh region and is placed in the defect as interposition material. Fat from this region or the buttock is structurally more robust that local fat which can be soft and friable; as such it is better for interposition. The EDB is then repaired, with haemostasis and a sound closure.
Postoperatively, the patient is rested in a short leg cast for two weeks to facilitate wound healing. At the two-week mark the patient transitions to an Aircast™ boot and begins physiotherapy, focusing on foot and ankle range-of-motion exercises. The patient is permitted to progress to fully weight-bearing from the fourth postoperative week onwards. The return to sporting activity is authorized at three months postoperatively.
Common pitfalls:
Failure to recognize associated coalitions – More than one coalition can be present in the same foot in up to 4% of cases. This would be identified using CT imaging.16
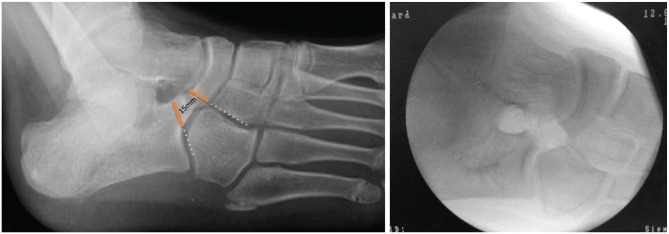
Inadequate resection – The average depth of the bar is approximately 2.5 cm.17 If osteotomes are not placed orthogonally to the plane of the coalition there is a risk that only the dorsal portion of the bar is resected leaving a plantar bridge (Fig. 3 & Fig. 4).
Over-resection – Excessive resection of the navicular can cause uncovering of the talus (iatrogenic dysplasia capitis pedis), which may lead to abnormal loading mechanics and early joint degeneration. Intraoperatively we use the calcaneocuboid joints as a guide to the proximal limit of the resection and the joint between the cuboid and the lateral cuneiform and distal limit to guide resection (Fig. 5).
Injuring the cuboid or the talar head during resection of the bar – As the coalition becomes narrower in a posterior-plantar direction, one should use 10 mm osteotomes to start cutting the most dorsal area of the bar and then 5 mm osteotomes to avoid this complication.
Fig. 3.
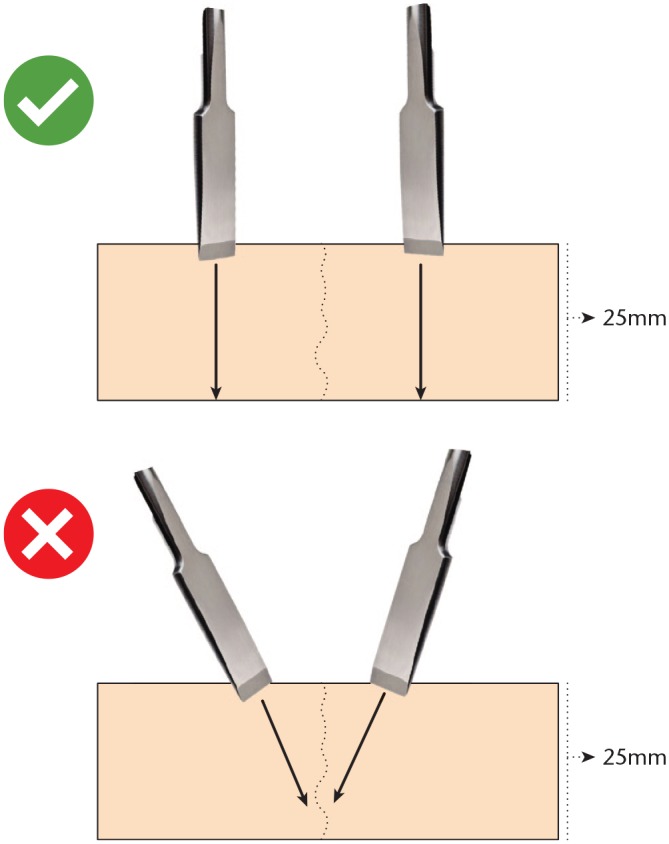
Correct and incorrect resection technique for a calcaneonavicular bar.
Fig. 4.
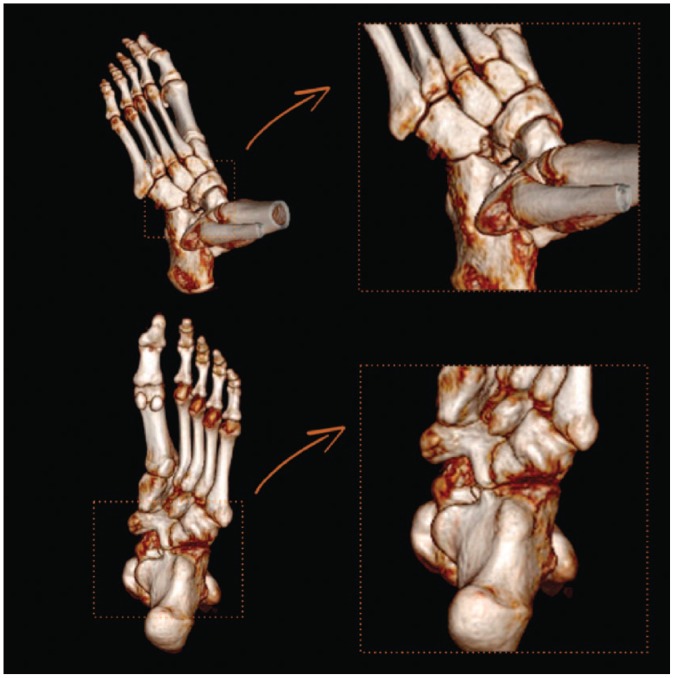
A 14-year-old who consulted for pain and limited mobility after two failed attempts at removal of a calcaneonavicular bar. Note from the dorsum what appears to be a successful resection; however, the plantar view demonstrates incomplete resection of the coalition.
Fig. 5.
(a) Resection margins of a calcaneonavicular bar, (b) intraoperative image after proper resection.
Outcomes after calcaneonavicular coalition resection
Evaluating the outcomes of calcaneonavicular coalition resection is difficult due to the heterogeneity in data, different outcome measures and variable follow-up durations. A historical report from Mitchell and Gibson, who undertook open resection without interposition, demonstrated a recurrence rate of 66%.18 In response to this and other reports of high recurrence rates,19 Cowell20 described the open resection with EDB interposition to act as a physical barrier to reduce the risk of recurrence. Gonzalez and Kumar reported an excellent or good outcome in 58 of 75 feet (77%) with a 23% recurrence rate in a cohort of patients followed up for 2–23 years.21 Chambers et al reported no recurrence in 29 CNC resected with EDB interposition.22 In a small comparative study, Moyes et al demonstrated a reduction in recurrence rate from 43% to 10% by using EDB to fill the defect instead of the traditional non-interposition method.23
For a time, EDB interposition was a commonly accepted practice in many institutions across the world; however, there have been some doubts about the suitability of EDB as a void filler after coalition resection. Mubarak et al demonstrated that EDB only filled on average 64% of the gap after coalition resection, thereby risking recurrence, and as such advocated fat as the best void filler.17 There is also evidence that osteoprogenitor cells may reside in muscle, and as such it may not be the best option when a goal of surgery is to minimize the risk of re-synostosis.24 A final less well recorded problem with EDB interposition is that it results in bony prominence on the lateral aspect of the foot which can cause discomfort when wearing shoes. A number of alternative void fillers have been used in the literature, including bone wax,25 fibrin glue,26 adipofascial flaps27 and deepithelialized skin flap graft.28 There is, however, only one comparative study in the literature assessing the utility of different void fillers after CNC resection. Masquijo et al demonstrated, in a three-leg study, that use of bone wax or fat as interposition was superior to EDB with respect to patient-reported outcomes and re-ossification rates.25 It is our belief that fat interposition is the best, biologic method to fill the gap left after TCC resection, as illustrated previously. Recently an arthroscopic approach has been described for surgical resection of CNC.14 Whilst good outcomes have been reported, the cases series is small with limited follow-up. In this approach no interposition material is used, thus raising concerns about the risk of coalition re-ossification. Limited space also makes access difficult and runs the risk of iatrogenic chondral or nerve injury. As such it remains the case, whether or not, an arthroscopic approach to CNC excision is superior to open with interposition graft.
Talocalcaneal coalitions
Talocalcaneal coalitions (TCC) represent the second most frequent tarsal coalition.5 Clinically, TCC is commonly associated with a rigid flatfoot deformity (rarely with rigid hindfoot varus), a stiff subtalar joint and in some cases a ‘double medial malleolus’ sign secondary to a bulky middle facet.29 The diagnosis can be made on plain radiographs, with the classic observation of a C-sign or ring-sign on the lateral view (Fig. 6). This sign, however, may only be seen in around two fifths of cases, and its absence cannot exclude a TCC.30 Other indirect radiological signs include talar beaking (secondary to a dorsal osteophyte arising from the talus), a poorly visible middle facet of the subtalar joint or a narrowed subtalar joint line. Where there is concern clinically and concerning features on plain X-rays, CT and/or MRI are advocated as the next most appropriate investigations. Magnetic resonance imaging is useful to illustrate bony oedema and can elucidate other local pathology distinguishing a symptomatic coalition from an incidental finding. Computed tomography can evaluate the characteristics of the coalition and exclude the presence of additional bars. In addition, CT allows further evaluation of the extent of fusion and degree of degeneration of the subtalar and Chopart joints. Assessment of the hindfoot alignment is critical, and this is evaluated by means of the talocalcaneal angle, which has been shown to be a reliable measurement for preoperative planning in a recent study.31 Rozansky et al have recently proposed a CT-based classification in 3-D which allows better preoperative planning.32 This classification groups TCCs into five types:
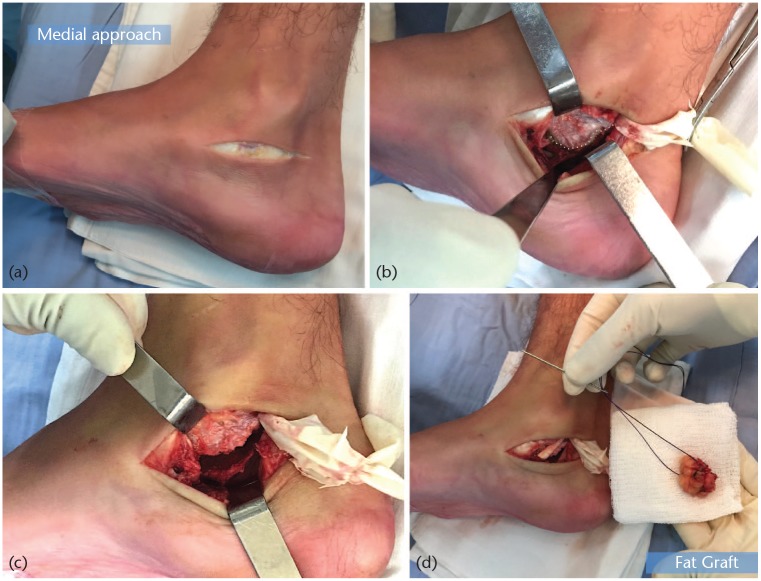
Fig. 6.
Clinical photographs of resection of Type I talocalcaneal coalition in a symptomatic 13-year-old boy. (a) Medial approach centred over the sustentaculum tali. (b) The tibialis posterior is identified and retracted dorsally. The flexor digitorum longus (FDL) is retracted plantarward. The deep sheath is incised to expose the coalition. The synchondrosis between the talus and calcaneus is identified. (c) Resection is performed with small osteotomes and rongeurs, and is considered complete when range of motion is improved and the entire posterior facet is visualized. (d) The fat graft is placed in the defect and the wounds are closed.
Type I (Linear) are the most common and simplest to resect.
Type II (Linear with posterior hook) are similar to Type I but have a hook on the posterior aspect of the sustentaculum tali, which should be resected to recover the subtalar mobility.
Type III (Shingled) have a hypoplastic sustentaculum tali. In this type is important to perform resection in a plane higher than usual (caudal to cephalic) inclination.
Type IV (bone) is the most controversial as to whether it should be resected or whether the foot should just be realigned.
Type V (Posterior) is usually small and located in the most rear of the subtalar joint in intimate relationship with the neurovascular bundle.
As an adjunct to this CT-based classification, to aid surgical planning one must further consider the anatomical location of the TCC. The TCC may be extra-articular (either posteromedial or anterolateral) or intra-articular (mid-facet, posterior facet and anterior facet).
There continues to be debate in the literature about how best to surgically manage TCC. Where possible it is felt that resection of the synostosis is appropriate management. However, poorer results have been observed in some series where the coalition forms greater than 50% of the posterior subtalar articulation and where there is significant rigid hindfoot valgus.33,34 This has been contested by other authors, who believe that resection of a symptomatic TCC is appropriate no matter how severe the deformity or extensive the coalition.35
As with calcaneonavicular coalitions, there is also debate about the best interpositional material to use to minimize the risk of recurrence. Commonly used materials include fat, bone wax and the tendon of the flexor hallucis longus.36–38 Other interposition grafts include the pediculated tibialis posterior tendon sheath,39 fascia lata allograft40 and even particulate juvenile hyaline cartilage allograft.41 There are no comparative studies assessing the superiority of a particular interposition graft material.
Some surgeons are also of the belief that resection of the coalition alone is appropriate management,42 but others would recommend resection combined with reconstruction of the foot.43,44 In a patient with marked valgus deformity, hindfoot bar resection has two potential effects: 1 the loss of the medial tether allowing further collapse of the hindfoot into valgus,2 reduction of the load-bearing surface area of the subtalar joint. These two factors, if left unaddressed, would lead to shear forces on a smaller articular surface resulting in accelerated chondropathy and degenerative changes. It is for this reason that under certain circumstances we would advocate resection with concomitant reconstruction.
Ultimately symptoms may be caused by the presence of the bar, the associated deformity, or both. We are of the belief that the treatment must be based on the location of pain, type and size of the bar, foot alignment and the presence of associated degenerative signs (infrequently in this age group). Our approach to the surgical management of TCC is summarized below, and is akin to that published by Masquijo et al45 categorizing TCCs into three common presentations.
Coalition consisting of < 50% of the posterior subtalar facet, acceptable foot alignment (< 16° hindfoot valgus), no degenerative signs in the subtalar joint (STJ)
In this case the pain is caused by the bar so the prescribed treatment is resection. This would be achieved through a medial approach centred on the sustentaculum tali, as illustrated in Fig. 6. As per resection of a calcaneonavicular bar, our interposition graft of choice is autogenous fat from the buttock. The radiological result of this surgery is illustrated in Fig. 7.
Fig. 7.
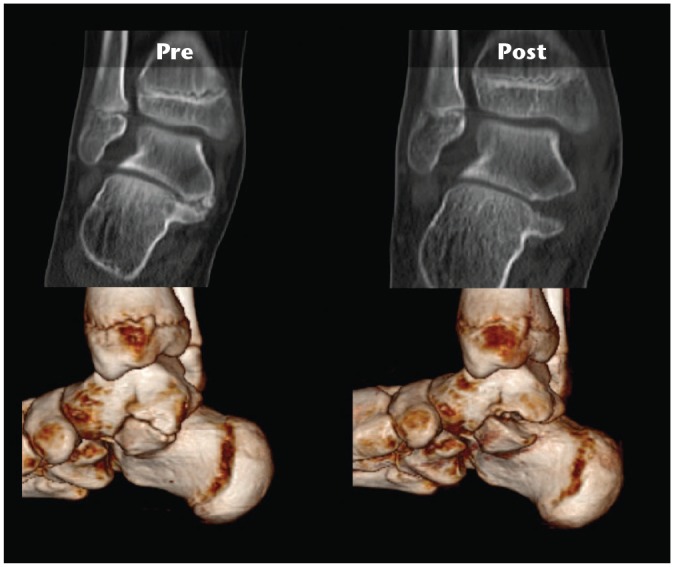
The coronal and 3D reconstruction shows a linear talocalcaneal bar (Type I). Postoperative scan shows resection to undamaged articular cartilage respecting the sustentaculum tali.
Coalition < 50% posterior facet, hindfoot valgus > 16°, no STJ degenerative changes
In this scenario we would undertake combined resection of the coalition alongside foot realignment surgery. Reconstruction surgery in these cases is with the use of a lateral column lengthening (LCL) using an Evans/Mosca-type calcaneal osteotomy and a medial sliding calcaneal osteotomy. Most cases have severe deformities and require a combination of the aforementioned procedures. After correction of the hindfoot if there is residual forefoot supination deformity the LCL would be combined with a medial cuneiform opening wedge plantarflexion osteotomy. Soft tissue surgery in the form of tendoachilles and/or peroneus brevis lengthening is undertaken if there is evidence of contracture (Fig 8).
Fig. 8.
Female, 11 years old with severe flatfoot deformity, limited range of motion and pain. (A) Lateral radiograph of the left foot with severe flatfoot and positive C-sign (+). (B) Coronal CT scan with severe hindfoot valgus deformity, and TC bony bar (Type V). (C) CT scan 3D reconstruction. (D) Lateral radiograph of the left foot after realignment without tarsal coalition resection (lateral column lengthening + medial sliding calcaneal osteotomy + medial cuneiform opening wedge plantarflexion osteotomy + tendoachilles lengthening). Foot is plantigrade and patient reported no symptoms or activities limitations at the two-year follow-up.
Coalition > 50% posterior facet, hindfoot valgus > 16°, ± STJ degenerative signs
In this third scenario, we believe that the cause of pain is predominantly due to the marked deformity of the foot. The bar acts as an arthrodesis, holding the joint in a poor position. Some authors consider that this is a good indication for arthrodesis; however, the malalignment makes arthrodesis technically more demanding. For this reason, our preference is to realign the foot without attempting to resect the bar and reserve arthrodesis and salvage surgery for those cases that have previously failed resection/reconstruction.
Outcomes after talocalcaneal coalition surgery
Appraising the outcomes after TCC surgery is difficult due to inherent heterogeneity in the population and various surgical prescriptions employed. Talocalcaneal coalitions are quite variable in terms of location, size, involvement of the posterior facet (< 50% versus > 50%), type (bony versus cartilaginous), foot alignment, and associated STJ osteoarthritis; which makes reports difficult to interpret. Outcomes from surgery have been reported in a number of ways, varying from simple Likert scales, to use of tools such as the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score. Few of these measures, including the AOFAS hindfoot score, have been validated in the paediatric population; nonetheless they can still provide some useful insight. More objective measures of outcome including assessment of subtalar joint motion and recurrence rates have also been evaluated in some studies, but these results should be placed in the context of the follow-up duration.
Overall short to medium-term results from surgical intervention to treat TCC are favourable in most cases.36,46,47 However, TCC that share some characteristics have shown poor outcomes following surgical resection. Wilde et al33 recommended against resection in patients in whom preoperative CT had shown the area of relative coalition to be greater than 50%, and heel valgus was greater than 16°. Luhmann and Schoenecker34 confirmed these findings with a further study. The authors investigated 25 feet that had had resection of the TC coalition alone and observed mean AOFAS scores of 81.9 with mean follow-up of 2.5 years. They did, however, report significantly less favourable results when the coalition was > 50% of the joint surface and the heel valgus was excessive.
Mosca and Bevan43 recommended surgical realignment with calcaneal osteotomies in this subset of patients to avoid stress transfer to the ankle joint associated to triple arthrodesis. Mosca reported on a series of eight patients (13 TCCs) who had undergone calcaneal lengthening osteotomy, gastrocnemius, or Achilles tendon lengthening with or without coalition resection. In their series, mean clinical scores (AOFAS ankle-hindfoot) improved from 65 to 94 points. All radiographic angles were corrected to normal except for one patient, who had the most severe deformity in the group. Masquijo et al45 provided further insights into this concept, and demonstrated quite dramatic improvements in AOFAS scores with an individualized comprehensive approach based on coalition size, foot alignment, and the health of the posterior facet of the subtalar joint. In eight feet treated with combined foot reconstruction and TC coalition resection, preoperative mean scores of 45 points improved to 98 points (near perfect) postoperatively. Even with reconstruction alone without coalition resection AOFAS scores in six feet improved from a mean of 60 to 92.3 postoperatively. Postoperative improvements in AOFAS scores of this magnitude were also seen by Hubert et al in their study of 12 feet with TC coalitions.39
Whilst clinical outcomes from surgery have been good, objective assessments of the function of the feet and ankle have demonstrated persistent abnormalities post surgery. Lyon et al48 demonstrated ongoing differences in plantar pressure distribution post tarsal coalition excision, as well as alterations in electromyographic activity in the lower limb musculature. Hetsroni et al49 also observed persistent abnormal subtalar kinematics even after clinically successful tarsal coalition resection. Skwara et al50 corroborated these abnormal gait analysis findings. These findings highlight that in cases of tarsal coalition the articulations are not normal to begin with, thus expecting entirely normal function is unrealistic, and maybe more emphasis should be placed on clinical outcomes.
The future of surgical management of tarsal coalitions
The surgical management of tarsal coalitions has been an iterative, evolving approach with learning through trial and error. Few well-constructed comparative studies exist to truly inform the surgeon about best practice, nonetheless there are exciting avenues by which we may improve our future practice.
It is evident, especially in cases of TCC that the anatomy is complex, and two-dimensional fluoroscopy may not suffice in the intraoperative evaluation of whether adequate resection has occurred or not. With the technological advances in imaging hardware, CT scanners are increasingly available in the operating room to allow a formal 3-D assessment of the coalition at the time of surgery. It has been suggested that use of CT in this manner reduces surgical morbidity and optimizes the coalition resection whilst minimizing violation of the intact subtalar articulation.51 Three-dimensional printing is a transformative technology when applied to orthopaedics. Three-dimensional printing models can allow surgeons to evaluate the exact location of the coalition, the coexisting deformity, and plan for a more precise resection and deformity correction. The low cost of 3D printers makes this technology available to almost every surgeon. Navigation methods may further enhance surgical outcomes.52 An alternative but related approach is to use preoperative CT scans to help construct patient-specific coalition resection tools to optimize the surgical procedure. This is a novel idea, but preliminary reports about its utility are encouraging.40
To truly judge success of a procedure it is important to have well-validated outcome measures, and the research community is increasingly placing more stock in patient-reported outcome measures (PROMs). There is a relative dearth of PROMs in the paediatric population; however, the Oxford Ankle Foot Questionnaire for Children (OxAFQ-C) represents a well-validated site-specific tool perfect for use in children undergoing tarsal coalition surgery.53 Use of tools such as the OxAFQ-C in the context of prospective research studies, would help us gain a better understanding of the true efficacy of our surgical interventions.
Discussion
Tarsal coalitions are ubiquitous and can be a source of significant pain and deformity. It is likely that most, if not all, paediatric orthopaedic surgeons will routinely treat children with symptomatic coalitions and thus a contemporary perspective on the surgical management of this condition is important. When surgically treating a child with a tarsal coalition it is important to remember that unlike in trauma, where one is restoring anatomy to a previous uninjured state, here one is dealing with articulations which have never been entirely normal. This in itself imparts inherent limitations on the success of treatment; however, the surgical rationale to, where possible, provide a well-aligned, mobile, pain-free foot and ankle is sound and logical. To ensure that this surgical objective is achieved it is incumbent on the surgeon to have a comprehensive understanding of the anatomy of the coalition, any concomitant deformity and degenerative changes. To attain this understanding, advanced imaging methods, commonly CT, are useful in the preoperative phase, and intraoperatively may further facilitate surgical intervention.
Whilst there are some common themes in the surgical approach to tarsal coalitions there is still significant variability in treatment methods within centres nationally and internationally. The variation in practice highlights the uncertainty that remains in the orthopaedic community about the best methods to treat this common condition. Debate continues about the role and timing of foot reconstructive surgery, the best interposition graft material, the place of novel technologies, and minimally invasive techniques. Topics like these should be made research priorities and hypotheses should be tested using robust methodology and validated patient-reported outcome measures. It is only by doing this that we can ensure the best possible treatment for patients in the future.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Nalaboff KM, Schweitzer ME. MRI of tarsal coalition: frequency, distribution, and innovative signs. Bull NYU Hosp Jt Dis 2008;66:14–21. [PubMed] [Google Scholar]
- 2. Rühli FJ, Solomon LB, Henneberg M. High prevalence of tarsal coalitions and tarsal joint variants in a recent cadaver sample and its possible significance. Clin Anat 2003;16:411–415. [DOI] [PubMed] [Google Scholar]
- 3. Murphy JS, Mubarak SJ. Talocalcaneal coalitions. Foot Ankle Clin 2015;20:681–691. [DOI] [PubMed] [Google Scholar]
- 4. Leonard MA. The inheritance of tarsal coalition and its relationship to spastic flat foot. J Bone Joint Surg Br 1974;56B:520–526. [PubMed] [Google Scholar]
- 5. Stormont DM, Peterson HA. The relative incidence of tarsal coalition. Clin Orthop Relat Res 1983;181:28–36. [PubMed] [Google Scholar]
- 6. Sarage AL, Gambardella GV, Fullem B, Saxena A, Caminear DS. Cuboid-navicular tarsal coalition: report of a small case series with description of a surgical approach for resection. J Foot Ankle Surg 2012;51:783–786 [DOI] [PubMed] [Google Scholar]
- 7. Craig CL, Goldberg MJ. Calcaneocuboid coalition in Crouzon’s syndrome (craniofacial dysostosis): report of a case and review of the literature. J Bone Joint Surg Am 1977;59:826–827. [PubMed] [Google Scholar]
- 8. Macera A, Teodonno F, Carulli C, Frances Borrego A, Innocenti M. Talonavicular coalition as a cause of foot pain. Joints 2017;5:246–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Malone JB, Raney EM. Bilateral navicular-medial cuneiform synostosis manifesting as medial foot pain: a case report and review of the literature. J Pediatr Orthop B 2016;25:138–141. [DOI] [PubMed] [Google Scholar]
- 10. Stevens BW, Kolodziej P. Non-osseous tarsal coalition of the lateral cuneiform-third metatarsal joint. Foot Ankle Int 2008;29:867–870. [DOI] [PubMed] [Google Scholar]
- 11. Oestreich AE, Mize WA, Crawford AH, Morgan RC., Jr. The ‘anteater nose’: a direct sign of calcaneonavicular coalition on the lateral radiograph. J Pediatr Orthop 1987;7:709–711. [PubMed] [Google Scholar]
- 12. Ridley LJ, Han J, Ridley WE, Xiang H. Anteater nose and reverse anteater signs: calcaneo-navicular coalition. J Med Imaging Radiat Oncol 2018;62:118–119. [DOI] [PubMed] [Google Scholar]
- 13. Badgley CE. Coalition of the calcaneus and the navicular. Arch Surg 1927;15:75–88. [Google Scholar]
- 14. Knörr J, Accadbled F, Abid A, et al. Arthroscopic treatment of calcaneonavicular coalition in children. Orthop Traumatol Surg Res 2011;97:565–568. [DOI] [PubMed] [Google Scholar]
- 15. Nehme AH, Bou Monsef J, Bou Ghannam AG, Imad JP, Moucharafieh R, Wehbe J. Arthroscopic resection of a bilateral calcaneonavicular coalition in a child. J Foot Ankle Surg 2016;55:1079–1082. [DOI] [PubMed] [Google Scholar]
- 16. Masquijo JJ, Jarvis J. Associated talocalcaneal and calcaneonavicular coalitions in the same foot. J Pediatr Orthop B 2010;19:507–510. [DOI] [PubMed] [Google Scholar]
- 17. Mubarak SJ, Patel PN, Upasani VV, Moor MA, Wenger DR. Calcaneonavicular coalition: treatment by excision and fat graft. J Pediatr Orthop 2009;29:418–426. [DOI] [PubMed] [Google Scholar]
- 18. Mitchell GP, Gibson JM. Excision of calcaneo-navicular bar for painful spasmodic flat foot. J Bone Joint Surg Br 1967;49:281–287. [PubMed] [Google Scholar]
- 19. Andreasen E. Calcaneo-navicular coalition: late results of resection. Acta Orthop Scand 1968;39:424–432. [DOI] [PubMed] [Google Scholar]
- 20. Cowell HR. Talocalcaneal coalition and new causes of peroneal spastic flatfoot. Clin Orthop Relat Res 1972;85:16–22. [DOI] [PubMed] [Google Scholar]
- 21. Gonzalez P, Kumar SJ. Calcaneonavicular coalition treated by resection and interposition of the extensor digitorum brevis muscle. J Bone Joint Surg Am 1990;72:71–77. [PubMed] [Google Scholar]
- 22. Chambers RB, Cook TM, Cowell HR. Surgical reconstruction for calcaneonavicular coalition: evaluation of function and gait. J Bone Joint Surg Am 1982;64:829–836. [PubMed] [Google Scholar]
- 23. Moyes ST, Crawfurd EJ, Aichroth PM. The interposition of extensor digitorum brevis in the resection of calcaneonavicular bars. J Pediatr Orthop 1994;14:387–388. [DOI] [PubMed] [Google Scholar]
- 24. Bosch P, Musgrave DS, Lee JY, et al. Osteoprogenitor cells within skeletal muscle. J Orthop Res 2000;18:933–944. [DOI] [PubMed] [Google Scholar]
- 25. Masquijo J, Allende V, Torres-Gomez A, Dobbs MB. Fat graft and bone wax interposition provides better functional outcomes and lower reossification rates than extensor digitorum brevis after calcaneonavicular coalition resection. J Pediatr Orthop 2017;37:e427–e431. [DOI] [PubMed] [Google Scholar]
- 26. Weatherall JM, Price AE. Fibrin glue as interposition graft for tarsal coalition. Am J Orthop (Belle Mead NJ) 2013;42:26–29. [PubMed] [Google Scholar]
- 27. Okada M, Saito H. Resection interposition arthroplasty of calcaneonavicular coalition using a lateral supramalleolar adipofascial flap: case report. J Pediatr Orthop B 2013;22:252–254. [DOI] [PubMed] [Google Scholar]
- 28. Sperl M, Saraph V, Zwick EB, Kraus T, Spendel S, Linhart WE. Preliminary report: resection and interposition of a deepithelialized skin flap graft in tarsal coalition in children. J Pediatr Orthop B 2010;19:171–176. [DOI] [PubMed] [Google Scholar]
- 29. Rocchi V, Huang MT, Bomar JD, Mubarak S. The ‘double medial malleolus’: a new physical finding in talocalcaneal coalition. J Pediatr Orthop 2018;38:239–243. [DOI] [PubMed] [Google Scholar]
- 30. Moraleda L, Gantsoudes GD, Mubarak SJ. C sign: talocalcaneal coalition or flatfoot deformity? J Pediatr Orthop 2014;34:814–819. [DOI] [PubMed] [Google Scholar]
- 31. Masquijo J, Tourn D, Torres-Gomez A. Fiabilidad del ángulo astrágalo-calcáneo para la evaluación de la alineación del retropié. Rev Esp Cir Ortop Traumatol 2019;63:20–23. [DOI] [PubMed] [Google Scholar]
- 32. Rozansky A, Varley E, Moor M, Wenger DR, Mubarak SJ. A radiologic classification of talocalcaneal coalitions based on 3D reconstruction. J Child Orthop 2010;4:129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wilde PH, Torode IP, Dickens DR, Cole WG. Resection for symptomatic talocalcaneal coalition. J Bone Joint Surg Br 1994;76:797–801. [PubMed] [Google Scholar]
- 34. Luhmann SJ, Schoenecker PL. Symptomatic talocalcaneal coalition resection: indications and results. J Pediatr Orthop 1998;18:748–754. [PubMed] [Google Scholar]
- 35. Khoshbin A, Law PW, Caspi L, Wright JG. Long-term functional outcomes of resected tarsal coalitions. Foot Ankle Int 2013;34:1370–1375. [DOI] [PubMed] [Google Scholar]
- 36. Comfort TK, Johnson LO. Resection for symptomatic talocalcaneal coalition. J Pediatr Orthop 1998;18:283–288. [PubMed] [Google Scholar]
- 37. McCormack TJ, Olney B, Asher M. Talocalcaneal coalition resection: a 10-year follow-up. J Pediatr Orthop 1997;17:13–15. [PubMed] [Google Scholar]
- 38. Raikin S, Cooperman DR, Thompson GH. Interposition of the split flexor hallucis longus tendon after resection of a coalition of the middle facet of the talocalcaneal joint. J Bone Joint Surg Am 1999;81:11–19. [DOI] [PubMed] [Google Scholar]
- 39. Hubert J, Hawellek T, Beil FT, et al. Resection of medial talocalcaneal coalition with interposition of a pediculated flap of tibialis posterior tendon sheath. Foot Ankle Int 2018;39:935–941. [DOI] [PubMed] [Google Scholar]
- 40. de Wouters S, Tran Duy K, Docquier PL. Patient-specific instruments for surgical resection of painful tarsal coalition in adolescents. Orthop Traumatol Surg Res 2014;100:423–427. [DOI] [PubMed] [Google Scholar]
- 41. Tower DE, Wood RW, Vaardahl MD. Talocalcaneal joint middle facet coalition resection with interposition of a juvenile hyaline cartilage graft. J Foot Ankle Surg 2015;54:1178–1182. [DOI] [PubMed] [Google Scholar]
- 42. Gantsoudes GD, Roocroft JH, Mubarak SJ. Treatment of talocalcaneal coalitions. J Pediatr Orthop 2012;32:301–307. [DOI] [PubMed] [Google Scholar]
- 43. Mosca VS, Bevan WP. Talocalcaneal tarsal coalitions and the calcaneal lengthening osteotomy: the role of deformity correction. J Bone Joint Surg Am 2012;94:1584–1594. [DOI] [PubMed] [Google Scholar]
- 44. Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot: results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 1995;77:500–512. [DOI] [PubMed] [Google Scholar]
- 45. Masquijo J, Vazquez I, Allende V, Lanfranchi L, Torres-Gomez A, Dobbs MB. Surgical reconstruction for talocalcaneal coalitions with severe hindfoot valgus deformity. J Pediatr Orthop 2017;37:293–297. [DOI] [PubMed] [Google Scholar]
- 46. Takakura Y, Sugimoto K, Tanaka Y, Tamai S. Symptomatic talocalcaneal coalition: its clinical significance and treatment. Clin Orthop Relat Res 1991;269:249–256. [PubMed] [Google Scholar]
- 47. Olney BW, Asher MA. Excision of symptomatic coalition of the middle facet of the talocalcaneal joint. J Bone Joint Surg Am 1987;69:539–544. [PubMed] [Google Scholar]
- 48. Lyon R, Liu XC, Cho SJ. Effects of tarsal coalition resection on dynamic plantar pressures and electromyography of lower extremity muscles. J Foot Ankle Surg 2005;44:252–258. [DOI] [PubMed] [Google Scholar]
- 49. Hetsroni I, Nyska M, Mann G, Rozenfeld G, Ayalon M. Subtalar kinematics following resection of tarsal coalition. Foot Ankle Int 2008;29:1088–1094. [DOI] [PubMed] [Google Scholar]
- 50. Skwara A, Zounta V, Tibesku CO, Fuchs-Winkelmann S, Rosenbaum D. Plantar contact stress and gait analysis after resection of tarsal coalition. Acta Orthop Belg 2009;75:654–660. [PubMed] [Google Scholar]
- 51. Aibinder WR, Young EY, Milbrandt TA. Intraoperative three-dimensional navigation for talocalcaneal coalition resection. J Foot Ankle Surg 2017;56:1091–1094. [DOI] [PubMed] [Google Scholar]
- 52. Stokman JJ, Mitchell J, Noonan K. Subtalar coalition resection utilizing live navigation: a technique tip. J Child Orthop 2018;12:42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Morris C, Doll HA, Wainwright A, Theologis T, Fitzpatrick R. The Oxford ankle foot questionnaire for children: scaling, reliability and validity. J Bone Joint Surg Br 2008;90:1451–1456. [DOI] [PubMed] [Google Scholar]