Abstract
This review article presents a comprehensive literature review regarding extended trochanteric osteotomy (ETO).
The history, rationale, biomechanical considerations as well as indications are discussed.
The outcomes and complications as reported in the literature are presented, discussed and compared with our own practice.
Based on the available evidence, we present our preferred technique for performing ETO, its fixation, as well as post-operative rehabilitation.
The ETO aids implant removal and enhanced access. Reported union rate of ETO is high. The complications related to ETO are much less frequent than in cases when accidental intra-operative femoral fracture occurred that required fixation.
Based on the literature and our own experience we recommend ETO as a useful adjunct in the arsenal of the revision hip specialist.
Cite this article: EFORT Open Rev 2020;5:104-112. DOI: 10.1302/2058-5241.5.190005
Keywords: ETO, extended trochanteric osteotomy, revision hip arthroplasty, revision hip replacement, union rate of ETO
Background
Total hip arthroplasty (THA) is one of the most successful surgical procedures and has been named the ‘operation of the century’.1 Despite the success story of THA, there are some patients who will encounter further surgery because of failure of the implant or the surrounding bone. It is anticipated that the demand for revision surgery will increase2–5 and a change in the pattern in indications and timing of revisions has been described.6 Revision surgery is considered a more technically challenging, labour intensive and time-consuming procedure with overall poorer outcomes.7,8 Several techniques, reducing the surgical insult to the patient, have been described: retention of well-fixed components and modular head exchanges, liner exchanges or cementing liners in well-fixed shells, cement-in-cement revision techniques. However, sometimes the surgical team is left with no other choice than to remove well-fixed femoral implants or the complete cement mantle, or there may be a need to improve the exposure or a correction of femoral deformities. In such cases an extended trochanteric osteotomy (ETO) could facilitate the revision surgery.
The aim of this review article is to describe the history and rationale of the ETO, the indications for its use, the surgical technique, the post-operative treatment, the results and the complications.
History and rationale
Ollier described the lateral trans-trochanteric approach to the native hip in 1881. It was popularized by Sir John Charnley for use in low-friction arthroplasty in the 1960s.9,10 However, Charnley described a 4.2% non-union rate in his case series of 379 THAs in 1972.11 Current literature reports the non-union rate following the trans-trochanteric approach, with an associated increase in dislocations, Trendelenburg gait and patient dissatisfaction, to be closer to 10% (9.0–18.5%).12,13 Charnley advocated the trans-trochanteric approach for use in both primary as well as revision surgery. For revision cases Head14 described an extensile gluteus medius/vastus lateralis slitting whilst Glassman15 described a trochanteric slide to mitigate the risk of proximal migration. Cameron16 described his distal trochanteric osteotomy. A transfemoral approach, osteotomizing half of the proximal femur was advocated by Wagner to use with his revision stem.17 In 1995 Younger et al published series of Paprosky of the ETO and advocated its use in revision surgery.18
It is postulated that a longer osteotomy improves the area of bone contact and as such could improve the conditions for healing of the osteotomy. A longer osteotomy also reduces the migration risk by keeping the soft tissues of the vastus lateralis and anterolateral muscles attached to the osteotomy fragment, thereby counteracting the pull of the hip abductors in the coronal plane. It further stabilizes the osteotomized trochanter by creating compression forces which prevents proximal migration.19,20 A study using a three-dimensional biomechanical model of the hip has proven that in the flexed hip, the gluteus medius is primarily an internal rotator and secondarily a flexor and abductor.21 In vivo, the displacement force on the trochanteric fragment is a combination of abduction and anteriorly oriented forces22 and the vastus lateralis counteracts these proximally directed forces.
The indications and advantages for its use
The standard trochanteric osteotomy was advocated by Sir John Charnley for all routine cases. Nowadays, the osteotomy is only advocated for selective use in complex cases. Osteotomies have been used in the cases of proximal femoral deformities or high congenital hip dislocation to improve visualisation and provide improved access to both acetabulum and femur. Extended trochanteric osteotomy may be a useful adjunct in exposure of complex primary hip replacement or conversion of arthrodesis to hip arthroplasty. Luo et al23 report excellent results of extended trochanteric osteotomy in high congenital hip dislocation. They performed an ETO of 8 cm to 12 cm to facilitate the exposure of the acetabulum and the femur, reporting a 100% union rate with good clinical results in their small cohort. The authors concluded that the osteotomy offers excellent exposure of the hip, reduces the need for aggressive retraction, facilitates reduction of the hip and lowers the risk of nerve damage to the sciatic or femoral nerve.
During revisions, a well-executed ETO can facilitate the surgical procedure:
Removal of well-fixed cemented and uncemented stems
If a well-fixed stem needs to be removed, it may pose a significant challenge for the surgeon to retrieve it safely without causing an accidental fracture of the proximal femur or significant loss of bone stock. Extended trochanteric osteotomy allows for a controlled removal of well-fixed cemented and uncemented implants.18
Removal of a well-fixed cement mantle in septic and aseptic cases
Removal of the cement may be the most challenging part of the revision surgery. By using an ETO, all cement and the cement restrictor can be removed under direct vision, ensuring full cortical contact is achieved when reconstruction with an uncemented implant takes place. Lerch et al24 compared revision cases with ETO with cases without ETO and occurrence of an iatrogenic accidental femoral fracture. They reported a 14% complication rate, related to the fracture fixation and hardware in the non-ETO group, whereas none were reported in the ETO group. Furthermore, clinical, radiological outcomes and revision rate were all superior in ETO group. Park et al25 compared their series of revisions with and without ETO. Stem subsidence and cortical perforation rate were higher in the non-ETO group. It is important to remove old cement in cases where uncemented stem insertion is planned, as failure to do so may lead to stem under-sizing and subsequent subsidence, perforations and lack of integration. Removal of all cement is particularly important in infectious cases, when thorough debridement of the femoral canal is necessary and all cement should be removed to mitigate the recurrence of infection. Extended trochanteric osteotomy will allow the surgeon to access the femoral canal more easily and to remove the distal cement mantle more accurately. It enables an easier, less time consuming and more thorough debridement with a more detailed inspection of the femoral canal. An ETO will diminish the risk of iatrogenic femoral canal penetration by cement removal aids, such as OSCAR (Orthosonics System for Cemented Arthroplasty Revision- Orthofix, Verona, Italy). Lim et al26 reported on ETO use as part of the approach in two-stage revision of periprosthetic joint infections. In 23 consecutive cases, ETO was used during the first stage. After the closure of the osteotomy was performed, a cement spacer or temporary stem coated by cement was inserted. A 100% union of the ETO, as confirmed by radiological and clinical assessment during the second-stage procedure, was reported. In three cases, a new ETO was successfully performed at the time of the second stage. Successful eradication of infection was reported in 96% of cases. Petrie et al27 reported a large series of infected cases with ETO use during the first stage. In 70% cases they were able to use a standard prosthesis during the second stage. The use of an ETO in infected cases with similar results of ETO union has further been supported by other authors,28 even in cases of a delayed fixation of osteotomy.29
Improving exposure to the acetabulum
Firestone and Hedley reported six cases where extended proximal femoral osteotomies were used to access intra-pelvic displacement of acetabular components.30 In these cases an ETO could be performed prior to the dislocation of the hip to prevent acetabular or pelvic fractures. This technique is, in our opinion, very helpful in the conversion of a hemiarthroplasty to a THA in cases of severe wear of the native acetabulum and locking of the femoral head (Fig. 1, Fig. 2 and Fig. 3).
Fig. 1.
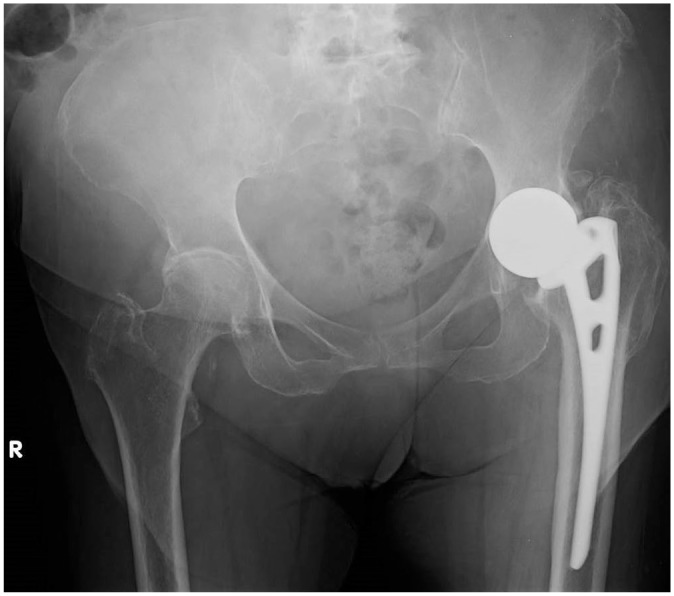
Radiograph showing hemiarthroplasty of the hip with acetabular erosion and significant protrusion in patient with significant pain and requiring revision to total hip arthroplasty.
Fig. 2.

Post-operative radiograph of the patient presented in Fig. 1. Extended trochanteric osteotomy (ETO) was used to allow safe hip dislocation and retrieval of the hemiarthroplasty, and following repair of the ETO an uncemented modular stem was implanted.
Fig. 3.
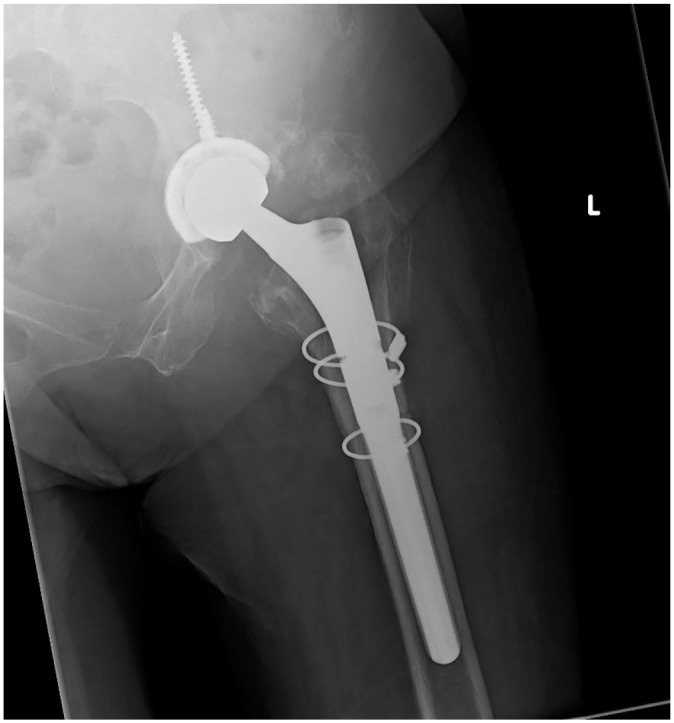
Post-operative radiograph of the patient presented in Fig. 1 showing femoral component in full with extended trochanteric osteotomy fully healed.
Correcting varus deformity of the proximal femur
A loose, short femoral component can cause the varus remodelling of the proximal femur. This usually occurs at the tip of the failed femoral implant. If the deformity is not acknowledged and not corrected, it may lead to varus insertion of the stem or anterior perforation of femoral cortex. Paprosky and Martin31 observed 30% varus remodelling of the femur after aseptic loosening of femoral stem. They recommended the use of an ETO in those cases, as it will allow a safe retrieval of the failed implant, an easier implantation of the revision stem and reduce the risk of perforation and fracture complications.
Adjusting the tension in the abductor mechanism
Similar to the ability to tension the abductors in the standard trochanteric osteotomy, an ETO enables the surgeon to adjust the tension of the abductors to some degree by re-fixing the ETO in a more proximal or distal position. Shortening the osteotomy fragment or the use of bone graft can facilitate the repositioning and the extended bone contact will likely increase the healing potential.32
Periprosthetic fractures
Femoral component revision is the treatment of choice for Vancouver type B2 and B3 fractures.33,34 Extended trochanteric osteotomy facilitates removal of the loose stem, debridement of the femoral canal, removal of cement and implantation of an uncemented, tapered, porous coated stem. Levine et al35 advocate use of ETO, and present good results from 17 consecutive cases with significant femoral deficiencies and the use of uncemented stems. They report a 100% union rate of the osteotomy and fracture. The length of osteotomy was dictated by the fracture pattern, and varied from 6 cm to 18 cm. Others have reported similar outcomes.36–38 There are, however, concerns about the high rates of dislocations, ranging from 7% to 21%. Whilst this increased risk is unlikely associated with the use of an ETO, it is important to assess the stability of the hip intra-operatively and, if necessary, to correct the abductor tension. Sheridan et al39 favour a cable plate combination over cables alone; however, most authors agree a satisfactory fixation and good outcomes can be achieved with use of cables alone.
Induction of bone healing and ingrowth
By performing an ETO is likely that the implant will be better engaged in the cortical bone, increasing the area of circumferential ingrowth instead of a three-point fixation. Causing a controlled fracture has been linked to improved bone healing and ingrowth.24 A thorough removal of all debris, cement and foreign material will undoubtedly improve the ingrowth of the new implant.
Trochanteric osteolysis in the presence of metallosis
In cases of revisions for big head Metal on Metal (MoM) THAs, an ETO can facilitate the access and removal of implants.40 Debridement of the debris caused by the MOM articulation will be made easier and it is likely that this will ensure a more complete removal of the debris. In our experience of ETO use in cases of metallosis, we believe there is a delayed healing of the osteotomy and there may be an increase in fractures of the osteotomized fragment.
Surgical technique and pitfalls
Approach
Whilst an ETO can be safely performed using a direct lateral approach (modified Hardinge approach), most surgeons prefer an ETO in combination with a posterior approach. It is likely that the healing potential of an ETO is dependent on the vascularity of the ETO fragment. It is anticipated that the posterior approach will better retain the vascularity of the osteotomized fragment. Whatever approach is performed, extreme care needs to be taken to preserve soft tissue attachments. The osteotomy can be performed through the anterior cortex as described by MacDonald et al.41 The authors report non-union requiring revision in 6% of the cases when cerclage wires were used, whilst a 100% union rate was described with cable fixation. Manrique et al42 describe a detailed description of their technique of the anterior to posterior ETO.
When a posterior approach is used the osteotomy is usually commenced anterior of the gluteus maximus insertion, extended distally and continued in an anterior direction. We would advocate a minimum of 12 cm (from the tip of the greater trochanter); however, the length of the ETO should be determined by the implant to be revised, the presence and size of osteolytic lesions, the position and quality of the femoral isthmus and the presence of cement. It is our preference to perform the posterior leg of the osteotomy using an oscillating saw, followed by a distal horseshoe shape drilling of the lateral cortex. The anterior cortex is then osteotomized, using broad osteotomes and the fragment is finally lifted up. It is easier to perform the ETO after the femoral implant has been removed; however, this technique works with the femoral implant still in situ. We would suggest viewing the following YouTube® videos, accompanied by tips and tricks, depicting the surgical technique: https://youtu.be/9dHECqHyLMw43 and https://youtu.be/cfrMipk76fo.44
Prophylactic cable distal to the osteotomy
We favour the placement of a prophylactic wire distal to the osteotomy site prior to the preparation of the femoral canal and rasping or impaction of an uncemented stem. This should prevent the propagation of fractures distal to osteotomy. Miner et al45 reported a 10.8% rate of small, undisplaced cracks extending distally from the distal end of the osteotomy at the time of placement of the trial or final femoral component. In all cases, a single cerclage wire was placed just distal to the transverse leg of the osteotomy to prevent propagation of these fractures. No subsidence or loosening was reported and the fractures whilst described were not considered a complication.
ETO fixation
In an uncomplicated osteotomy and with availability of a good femoral bone stock of the ETO fragment, we advocate fixation of the fragment using two or three cables, adequately tensioned and appropriately locked. There is good evidence that this provides sufficient stability of the fragment whilst minimizing trauma to the soft tissue. In their cadaveric study, Chassin et al46 examined the stability of the ETO in femora with significant bone loss and deficiencies. They performed a repair of the ETO with three cables followed by impaction bone grafting and cementing the stem. They reported a similar stability compared with a non-osteotomized femur. More recently Schab et al47 performed cadaveric study comparing fixation with two versus three cables. Nine cadavers had both hips osteotomized and randomly assigned to either two or three-cable fixation and implantation of cylindrical fully coated stem. No statistically significant difference was found between the two-cable group and the three-cable group with regard to peak force, stiffness, angular displacement, axial displacement, or axial displacement. Zhu et al48 reached similar conclusions after conducting a biomechanical study.
Alternative ETO fixation methods
Use of cerclage wires for ETO closure has now become less popular despite being advocated by Mei et al.49 Warren et al50 reported better results using cables compared to heavy cerclage wire, with higher union rates and less reported stem subsidence. Simank et al51 reported a 20% non-union rate of ETO in their series, attributing it to use of wires that were on many occasions too thin. Kuruvali et al52 proposed an alternative technique of fixation of the ETO using suture cord. The authors in their series of 20 patients, with a variety of femoral defects, used four strands of braided resorbable suture to make a cord. After implantation of the stem and drilling two holes in the ETO fragment, the fragment was subsequently attached to the stem directly by the suture. The authors reported a 95% union rate and no intra-operative or late fractures of the osteotomy fragment. This technique has theoretical advantages: it is inexpensive, there is an improved control over the fragment, more ability to adjust the tension of the abductor muscles and the cord does not encircle the femur and the osteotomy, thus preserving the local blood supply and facilitating healing of the osteotomy.
The spider clamp or trochanteric clamp is a cable-claw device that is designed to fix the greater trochanter to the proximal femur. Usually two cables are passed below the lesser trochanter and tensioned. This should be used in cases of ETO where the fragment is very fragile, and the greater trochanter is at high risk of fracturing or fractured. It is a load-sharing device, avoiding cheese-wiring through the greater trochanter. A cable-plate device is another tool that may be used in fixation of the osteotomy. Surgeons may choose the length of the plate and the number of cables used to re-attach the osteotomy. In vitro studies have shown that cable-plate devices provide a stiffer fixation and can withstand a larger load before mechanical failure compared to wires and cables alone.53 They are, however, bulky and can cause trochanteric pain, impingement, as well as stress shielding. In cases of fractures of the fragment or in the cases of thin osteotomies with or without poor bone quality we prefer to use a cable-plate device. Mei et al,49 in their recent systematic review, discussed a variety of fixation options related to a highly heterogeneous group of patients. Due to the poor quality of studies they concluded that it was difficult to support the use of one implant over another. They noted a high risk of complications and re-operations following cable-plate fixation, with an 18% non-union rate, a 17% trochanteric pain rate and a 7% re-operation rate. This is higher than in cable fixation, which is associated with a 5% non-union rate, a 3% trochanteric pain rate and a 5% re-operation rate. However, cable plate devices are often used for salvage in cases when simple fixation with cables alone is not possible, or which are associated with a very high risk of fracture of the osteotomy fragment. In situations where fractures of the fragment are noted intra-operatively, a fixation with cables could be suboptimal. It is likely that because a cable-plate device is used in more challenging cases, the possible complications may not only be related to the device itself, but to the complexity of the case.
Revision Stems with ETO
Ladurner et al54 examined bone restoration of the proximal femur after ETO and the use of uncemented stems. In their series of 54 cases, all patients did show bone restoration, occurring from distal to proximal. At two years, the modular junction of the stem was bypassed in 75% of the cases reducing potential risk of stem fracture or junction failure.
Use of extended trochanteric osteotomy with cemented implants remains more controversial. While pressurizing the cement, leakage into the osteotomy site might occur and healing might be delayed or prevented. Furthermore, heat generated by the polymerization might lead to localized necrosis and osteoblast death in proximity to the osteotomy, impacting the healing negatively.
Peters et al55 report a series of 21 extended trochanteric osteotomies for revision of cemented implants. All osteotomies healed by six months post-operatively. Hellman et al56 report 10 cases in which, after ETO repair, impaction bone grafting was performed and a cemented stem inserted using a third-generation cementing technique. In two cases this led to non-union of the osteotomy, one requiring revision of fixation. However, a strong case in defence of impaction bone grafting and cement use after osteotomy has been made by the Exeter Group.57 In their consecutive series of 18 patients with close follow up, there was a 100% union rate of ETO after impaction bone grafting and implantation of cemented Exeter stem. We have experience with using ETO in infected cases during first-stage revision surgeries. After debridement of the femoral canal and closure of the osteotomy, a highly polished, collarless, tapered stem is used with a first-generation cementing technique to achieve some stability but to allow easy retrieval during the second-stage procedure. In these cases, we routinely use wires and avoid cables to reduce infection complications. A recent article by Janz et al highlighted the potential of bacterial colonization of cerclage material.58
The suggested post-operative treatment
Charnley advocated initial bedrest with abduction pillows for three weeks, followed by in-hospital mobilization for one week before discharge.11 Whereas this regimen was subsequently relaxed and earlier mobilization became the norm, patients were mobilized for a prolonged length of time with two crutches. There were also some restrictions on active abduction in order to mitigate the risk of migration of the greater trochanter. Currently the standard rehabilitation protocol consists of a minimum of six weeks protected weight bearing initially with a Zimmer frame, progressing to crutches if compliant.
Protected weight bearing after osteotomy is also advocated by Noble et al.59 In their biomechanical cadaveric study, the authors found that the torsional strength of the femur following ETO, its repair and insertion of well-fixed cemented stem, is 23% weaker than of those intact femora with implanted stem. The authors, however, used cerclage wires as a method of ETO repair and cemented stems were used rather than uncemented, therefore their results might not be representative of the more contemporary techniques. In our practice and in the absence of conclusive studies, we prefer and suggest that patients remain on crutches until signs of healing at the osteotomy site are visible on standard pelvic X-rays. In the majority of patients these restrictions will be lifted at the three-month post-operative visit.
Results of ETO
Conventional trochanteric osteotomy has led to non-union rates of up to 20% in revision THA.60 Wieser et al61 reported a non-union rate of 20% when a traditional anterior trochanteric slide osteotomy was performed in revision surgery and 4% when an ETO was used. They reported that the use of a cemented stem, older age and revision of cemented stem were risk factors for osteotomy non-union. Widely reported results as reported in the literature of ETO union are favourable and summarized in Table 1. Our own results62 are in keeping with those reported in the literature. We noted that in a small proportion of patients (6%) the osteotomy is not completely healed radiologically, although without signs of instability, migration or reaction to the fixation device. These patients were asymptomatic. We conclude that in these cases either a fibrous union or partial bony union occurs but it is impossible to appreciate this difference on plain radiographs. We do not routinely use computed tomography (CT) scan for follow up in asymptomatic patients. In 8% of our cases a fracture of the greater trochanter occurred. In one symptomatic patient a greater trochanter reattachment was required, others remained asymptomatic or symptoms were minimal. Meek et al63 reported a 30% rate of greater trochanter fracture in a large series of revision hip arthroplasty when an ETO was not used. We postulate that in cases with significant femoral bone loss and a fragile osteotomy fragment, a more robust form of fixation is used, such as spider clamp or cable plate device.
Table 1.
Non-union rates following extended trochanteric osteotomy in revision hip arthroplasty when modern fixation methods were used
Post-operative complications
Risks of fracture of the ETO fragment, delayed, mal or non-union as well complications of the revision surgery have been described. Special attention is necessary during the fixation of the ETO in order to avoid neurovascular injuries. There are case reports of arterial injury after fixation with cerclage wire following ETO64 as well as fracture fixation.65 This is most likely to occur in the distal half of the femur, in proximity to Hunter’s canal. Care is needed when closing the ETO in order not to cause a soft tissue entrapment. We advocate keeping the wire-passing instruments close to the bone and passing the wires from posterior to anterior in order to reduce the risk of inadvertently causing excessive soft tissue damage and safeguarding the sciatic nerve. Complications related to ETO itself, when employed in revision hip surgery, are lower than those resulting from unintentional fracture of the femur.24
Discussion
Osteotomies of the proximal femur during revision surgery have been used in many variations. The ETO was popularized by Paprosky18 to aid in the removal of well-fixed cemented and uncemented stems, to aid in the complete removal of a well-fixed cement mantle in septic and aseptic cases, to improve the exposure to the acetabulum, and to correct a varus deformity of the proximal femur. It can be used during revision procedures for periprosthetic fractures and in cases of trochanteric osteolysis in the presence of metallosis. It could help in adjusting the tension in the abductors, and is described as potentially inducing bone healing and improving ingrowth. We describe surgical techniques, pitfalls, results and post-operative complications.
In conclusion, an ETO is a safe, reproducible and reliable technique that may be advantageous in revision hip arthroplasty surgery. When performed with care for the femur and the surrounding soft tissues, it leads to impressive results whilst not compromising post-operative recovery. We believe that all revision hip surgeons should be familiar with this technique for use in selected cases. The main limitation of the technique compared to an endo-femoral removal of the implant is the use of a longer stem, in order to bypass the osteotomy.
Footnotes
ICMJE Conflict of interest statement: EP reports employment by the HDU Health Board outside the submitted work.
PHJC reports employment by the Hywel Dda University Health Board outside the submitted work.
The other authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet 2007;370:1508–1519. [DOI] [PubMed] [Google Scholar]
- 2. Pabinger C, Lothaller H, Portner N, Geissler A. Projections of hip arthroplasty in OECD countries up to 2050. Hip Int 2018;28:498–506. [DOI] [PubMed] [Google Scholar]
- 3. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–785. [DOI] [PubMed] [Google Scholar]
- 4. Mont MA, Issa K. Updated projections of total joint arthroplasty demands in America. Commentary on an article by Steven M. Kurtz, PhD, et al.: ‘Impact of the economic downturn on total joint replacement demand in the United States. Updated projections to 2021’. J Bone Joint Surg Am 2014;96:e68. [DOI] [PubMed] [Google Scholar]
- 5. Patel A, Pavlou G, Mujica-Mota R, Toms A. The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Joint J 2015;97-B:1076–1081. [DOI] [PubMed] [Google Scholar]
- 6. Cnudde P, Nemes S, Bülow E, et al. Trends in hip replacements between 1999 and 2012 in Sweden. J Orthop Res 2018;36:432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Postler AE, Beyer F, Wegner T, et al. Patient-reported outcomes after revision surgery compared to primary total hip arthroplasty. Hip Int 2017;27:180–186. [DOI] [PubMed] [Google Scholar]
- 8. Adelani MA, Crook K, Barrack RL, Maloney WJ, Clohisy JC. What is the prognosis of revision total hip arthroplasty in patients 55 years and younger? Clin Orthop Relat Res 2014;472:1518–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res 1970;72:7–21. [PubMed] [Google Scholar]
- 10. Mulliken BD, Rorabeck CH, Bourne RB, Nayak N. The surgical approach to total hip arthroplasty: complications and utility of a modified direct lateral approach. Iowa Orthop J 1995;15:48–61. [PMC free article] [PubMed] [Google Scholar]
- 11. Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br 1972;54:61–76. [PubMed] [Google Scholar]
- 12. Hawkins A, Midwinter K, Macdonald DA. Trochanteric non-union in revision total hip arthroplasty: does it matter? Ann R Coll Surg Engl 2000;82:39–42. [PMC free article] [PubMed] [Google Scholar]
- 13. Mehra A, Hemmady MV, Hodgkinson JP. Trochanteric non-union – does it influence the rate of revision following primary total hip replacement? A minimum of 15 years follow-up. Surgeon 2008;6:79–82. [DOI] [PubMed] [Google Scholar]
- 14. Head WC, Mallory TH, Berklacich FM, Dennis DA, Emerson RH, Jr, Wapner KL. Extensile exposure of the hip for revision arthroplasty. J Arthroplasty 1987;2:265–273. [DOI] [PubMed] [Google Scholar]
- 15. Glassman AH, Engh CA, Bobyn JD. A technique of extensile exposure for total hip arthroplasty. J Arthroplasty 1987;2:11–21. [DOI] [PubMed] [Google Scholar]
- 16. Cameron HU. Use of a distal trochanteric osteotomy in hip revision. Contemp Orthop 1991;23:235–238. [PubMed] [Google Scholar]
- 17. Wagner M, Wagner H. The transfemoral approach for revision of total hip replacement. Orthop Traumatol Surg Res 1999;7:260–276. [Google Scholar]
- 18. Younger TI, Bradford MS, Magnus RE, Paprosky WG. Extended proximal femoral osteotomy: a new technique for femoral revision arthroplasty. J Arthroplasty 1995;10:329–338. [DOI] [PubMed] [Google Scholar]
- 19. Nicholson P, Mulcahy D, Fenelon G. Trochanteric union in revision hip arthroplasty. J Arthroplasty 2001;16:65–69. [DOI] [PubMed] [Google Scholar]
- 20. Plausinis D, Haddad FS, Oxland TR, Duncan CP. Trochanteric slide osteotomy: biomechanical considerations. Instr Course Lect 2001;50:247–252. [PubMed] [Google Scholar]
- 21. Dostal WF, Andrews JG. A three-dimensional biomechanical model of hip musculature. J Biomech 1981;14:803–812. [DOI] [PubMed] [Google Scholar]
- 22. Charnley J. Low friction arthroplasty of the hip. New York: Springer, 1979. [Google Scholar]
- 23. Luo Z, Chen M, Hu F, et al. Cementless total hip arthroplasty with extended sliding trochanteric osteotomy for high congenital hip dislocation: a retrospective study. Medicine (Baltimore) 2017;96:e6581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lerch M, von Lewinski G, Windhagen H, Thorey F. Revision of total hip arthroplasty: clinical outcome of extended trochanteric osteotomy and intraoperative femoral fracture. Technol Health Care 2008;16:293–300. [PubMed] [Google Scholar]
- 25. Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty 2007;22:993–999. [DOI] [PubMed] [Google Scholar]
- 26. Lim SJ, Moon YW, Park YS. Is extended trochanteric osteotomy safe for use in 2-stage revision of periprosthetic hip infection? J Arthroplasty 2011;26:1067–1071. [DOI] [PubMed] [Google Scholar]
- 27. Petrie MJ, Harrison TP, Buckley SC, Gordon A, Kerry RM, Hamer AJ. Stay short or go long? Can a standard cemented femoral prosthesis be used at second-stage total hip arthroplasty revision for infection following an extended trochanteric osteotomy? J Arthroplasty 2017;32:2226–2230. [DOI] [PubMed] [Google Scholar]
- 28. Levine BR, Della Valle CJ, Hamming M, Sporer SM, Berger RA, Paprosky WG. Use of the extended trochanteric osteotomy in treating prosthetic hip infection. J Arthroplasty 2009;24:49–55. [DOI] [PubMed] [Google Scholar]
- 29. Morshed S, Huffman GR, Ries MD. Extended trochanteric osteotomy for 2-stage revision of infected total hip arthroplasty. J Arthroplasty 2005;20:294–301. [DOI] [PubMed] [Google Scholar]
- 30. Firestone TP, Hedley AK. Extended proximal femoral osteotomy for severe acetabular protrusion following total hip arthroplasty: a technical note. J Arthroplasty 1997;12:344–345. [DOI] [PubMed] [Google Scholar]
- 31. Paprosky WG, Martin EL. Cemented stem failure requires extended trochanteric osteotomy. Orthopedics 2003;26:28, 38. [DOI] [PubMed] [Google Scholar]
- 32. Beck M, Krüger A, Katthagen C, Kohl S. Osteotomy of the greater trochanter: effect on gluteus medius function. Surg Radiol Anat 2015;37:599–607. [DOI] [PubMed] [Google Scholar]
- 33. Macdonald SJ, Paprosky WG, Jablonsky WS, Magnus RG. Periprosthetic femoral fractures treated with a long-stem cementless component. J Arthroplasty 2001;16:379–383. [DOI] [PubMed] [Google Scholar]
- 34. Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am 2003;85:2156–2162. [DOI] [PubMed] [Google Scholar]
- 35. Levine BR, Della Valle CJ, Lewis P, Berger RA, Sporer SM, Paprosky W. Extended trochanteric osteotomy for the treatment of vancouver B2/B3 periprosthetic fractures of the femur. J Arthroplasty 2008;23:527–533. [DOI] [PubMed] [Google Scholar]
- 36. Stiehl JB. Extended osteotomy for periprosthetic femoral fractures in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2006;35:20–23. [PubMed] [Google Scholar]
- 37. Drexler M, Dwyer T, Chakravertty R, Backstein D, Gross AE, Safir O. The outcome of modified extended trochanteric osteotomy in revision THA for Vancouver B2/B3 periprosthetic fractures of the femur. J Arthroplasty 2014;29:1598–1604. [DOI] [PubMed] [Google Scholar]
- 38. Mulay S, Hassan T, Birtwistle S, Power R. Management of types B2 and B3 femoral periprosthetic fractures by a tapered, fluted, and distally fixed stem. J Arthroplasty 2005;20:751–756. [DOI] [PubMed] [Google Scholar]
- 39. Sheridan GA, Galbraith A, Kearns SR, Curtin W, Murphy CG. Extended trochanteric osteotomy (ETO) fixation for femoral stem revision in periprosthetic fractures: Dall-Miles plate versus cables. Eur J Orthop Surg Traumatol 2018;28:471–476. [DOI] [PubMed] [Google Scholar]
- 40. Nagoya S, Sasaki M, Kaya M, Okazaki S, Tateda K, Yamashita T. Extraction of well-fixed extended porous-coated cementless stems using a femoral longitudinal split procedure. Eur Orthop Traumatol 2015;6:417–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. MacDonald SJ, Cole C, Guerin J, Rorabeck CH, Bourne RB, McCalden RW. Extended trochanteric osteotomy via the direct lateral approach in revision hip arthroplasty. Clin Orthop Relat Res 2003;417:210–216. [DOI] [PubMed] [Google Scholar]
- 42. Manrique J, Chen AF, Heller S, Hozack WJ. Direct anterior approach for revision total hip arthroplasty. Ann Transl Med 2014;2:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Crockarell J, Dabov G. Extended trochanteric osteotomy for total hip revision arthroplasty. https://youtu.be/9dHECqHyLMw (date last accessed 2 October 2014).
- 44. Paprosky W. The extended trochanteric osteotomy: getting home in time for dinner. https://youtu.be/cfrMipk76fo (date last accessed 25 November 2014).
- 45. Miner TM, Momberger NG, Chong D, Paprosky WL. The extended trochanteric osteotomy in revision hip arthroplasty: a critical review of 166 cases at mean 3-year, 9-month follow-up. J Arthroplasty 2001;16:188–194. [DOI] [PubMed] [Google Scholar]
- 46. Chassin EP, Silverton CD, Berzins A, Rosenberg AG. Implant stability in revision total hip arthroplasty: allograft bone packing following extended proximal femoral osteotomy. J Arthroplasty 1997;12:863–868. [DOI] [PubMed] [Google Scholar]
- 47. Schwab JH, Camacho J, Kaufman K, Chen Q, Berry DJ, Trousdale RT. Optimal fixation for the extended trochanteric osteotomy: a pilot study comparing 3 cables vs 2 cables. J Arthroplasty 2008;23:534–538. [DOI] [PubMed] [Google Scholar]
- 48. Zhu Z, Ding H, Shao H, Zhou Y, Wang G. An in-vitro biomechanical study of different fixation techniques for the extended trochanteric osteotomy in revision THA. J Orthop Surg Res 2013;8:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mei XY, Gong YJ, Safir OA, Gross AE, Kuzyk PR. Fixation options following greater trochanteric osteotomies and fractures in total hip arthroplasty: a systematic review. JBJS Rev 2018;6(6):e4. [DOI] [PubMed] [Google Scholar]
- 50. Warren PJ, Thompson P, Fletcher MD. Transfemoral implantation of the Wagner SL stem: the abolition of subsidence and enhancement of osteotomy union rate using Dall-Miles cables. Arch Orthop Trauma Surg 2002;122:557–560. [DOI] [PubMed] [Google Scholar]
- 51. Simank HG, Chatzipanagiotis C, Kaps HP. [Complication rate following trochanteric osteotomy in total hip endoprosthesis: a retrospective study with failure analysis]. Z Orthop Ihre Grenzgeb 1996;134:457–464. [DOI] [PubMed] [Google Scholar]
- 52. Kuruvalli RR, Landsmeer R, Debnath UK, Suresh SP, Thomas TL. A new technique to reattach an extended trochanteric osteotomy in revision THA using suture cord. Clin Orthop Relat Res 2008;466:1444–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hersh CK, Williams RP, Trick LW, Lanctot D, Athanasiou K. Comparison of the mechanical performance of trochanteric fixation devices. Clin Orthop Relat Res 1996;329:317–325. [DOI] [PubMed] [Google Scholar]
- 54. Ladurner A, Zdravkovic V, Grob K. Femoral bone restoration patterns in revision total hip arthroplasty using distally fixed modular tapered titanium stems and an extended trochanteric osteotomy approach. J Arthroplasty 2018;33:2210–2217. [DOI] [PubMed] [Google Scholar]
- 55. Peters PC, Jr, Head WC, Emerson RH., Jr. An extended trochanteric osteotomy for revision total hip replacement. J Bone Joint Surg Br 1993;75:158–159. [DOI] [PubMed] [Google Scholar]
- 56. Hellman EJ, Capello WN, Feinberg JR. Nonunion of extended trochanteric osteotomies in impaction grafting femoral revisions. J Arthroplasty 1998;13:945–949. [DOI] [PubMed] [Google Scholar]
- 57. Charity J, Tsiridis E, Gusmão D, Bauze A, Timperley J, Gie G. Extended trochanteric osteotomy followed by cemented impaction allografting in revision hip arthroplasty. J Arthroplasty 2013;28:154–160. [DOI] [PubMed] [Google Scholar]
- 58. Janz V, Wassilew GI, Perka CF, Müller M. Cerclages after femoral osteotomy are at risk for bacterial colonization during two-stage septic total hip arthroplasty revision. J Bone Jt Infect 2018;3:138–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Noble AR, Branham DB, Willis MC, et al. Mechanical effects of the extended trochanteric osteotomy. J Bone Joint Surg Am 2005;87:521–529. [DOI] [PubMed] [Google Scholar]
- 60. Hawkins A, Midwinter K, Macdonald DA. Trochanteric non-union in revision total hip arthroplasty: does it matter? Ann R Coll Surg Engl 2000;82:39–42. [PMC free article] [PubMed] [Google Scholar]
- 61. Wieser K, Zingg P, Dora C. Trochanteric osteotomy in primary and revision total hip arthroplasty: risk factors for non-union. Arch Orthop Trauma Surg 2012;132:711–717. [DOI] [PubMed] [Google Scholar]
- 62. Wronka KS, Cnudde PHJ. Union rates and midterm results after extended trochanteric osteotomy in revision hip arthroplasty: useful and safe technique. Acta Orthop Belg 2017;83:53–56. [PubMed] [Google Scholar]
- 63. Meek RM, Garbuz DS, Masri BA, Greidanus NV, Duncan CP. Intraoperative fracture of the femur in revision total hip arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am 2004;86:480–485. [DOI] [PubMed] [Google Scholar]
- 64. Aleto T, Ritter MA, Berend ME. Case report: superficial femoral artery injury resulting from cerclage wiring during revision THA. Clin Orthop Relat Res 2008;466:749–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Mehta V, Finn HA. Femoral artery and vein injury after cerclage wiring of the femur: a case report. J Arthroplasty 2005;20:811–814. [DOI] [PubMed] [Google Scholar]
- 66. King S, Berend ME, Ritter MA, Keating EM, Faris PM, Meding JB. Extended femoral osteotomy and proximally coated prosthesis for hip revision. Orthopedics 2008;31:67. [DOI] [PubMed] [Google Scholar]
- 67. Lakstein D, Kosashvili Y, Backstein D, Safir O, Lee P, Gross AE. The long modified extended sliding trochanteric osteotomy. Int Orthop 2011;35:13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lakstein D, Kosashvili Y, Backstein D, Safir O, Gross AE. Modified extended trochanteric osteotomy with preservation of posterior structures. Hip Int 2010;20:102–108. [DOI] [PubMed] [Google Scholar]
- 69. Huffman GR, Ries MD. Combined vertical and horizontal cable fixation of an extended trochanteric osteotomy site. J Bone Joint Surg Am 2003;85:273–277. [DOI] [PubMed] [Google Scholar]
- 70. Mardones R, Gonzalez C, Cabanela ME, Trousdale RT, Berry DJ. Extended femoral osteotomy for revision of hip arthroplasty: results and complications. J Arthroplasty 2005;20:79–83. [DOI] [PubMed] [Google Scholar]


