Abstract
In cases of suspected scaphoid fracture where the initial radiographs are negative, a supplementary MRI, or alternatively CT, should be carried out within three to five days.
Fracture classification, assessment of dislocation as well as evaluation of fracture healing is best done on CT with reconstructions in the coronal and sagittal planes, following the longitudinal axis of the scaphoid.
After adequate conservative management, union is achieved at six weeks for approximately 90% of non-displaced or minimally displaced (≤ 0.5 mm) scaphoid waist fractures.
Scaphoid waist fractures with moderate displacement (0.5–1.5 mm) can be treated conservatively, but require prolonged cast immobilization for approximately eight to ten weeks.
Internal fixation is recommended for all scaphoid waist fractures with dislocation ≥ 1.5 mm.
Distal scaphoid fractures can be treated conservatively. The majority heal uneventfully after four to six weeks of immobilization, depending on fracture type.
In general, proximal scaphoid fractures should be treated with internal fixation.
Cite this article: EFORT Open Rev 2020;5:96-103. DOI: 10.1302/2058-5241.5.190025
Keywords: internal fixation, non-operative treatment, scaphoid fracture
Introduction
Post-traumatic radial-sided wrist pain is common and can represent a fracture, wrist sprain, ligament disruption or a combination of injuries. Previous studies have shown that a scaphoid fracture is the most common fracture among patients with post-traumatic radial-sided wrist pain.1,2 Scaphoid fractures are notorious for being difficult to diagnose as well as to achieve fracture union. The serious consequences of non-union, such as progressive degenerative changes and carpal collapse, the so-called SNAC (scaphoid non-union advanced collapse) wrist have for patients, typically young and active, resulted in a restrictive treatment regime with immobilization from eight to 12 weeks.3 However, in the case of the non-displaced scaphoid waist fracture, which is the most common among scaphoid fractures, it has been suggested that union can occur after just four to six weeks of immobilization.4–6
It is well known that scaphoid fractures can be difficult to diagnose on initial radiographs. In cases of suspected scaphoid fracture where the initial radiographs are negative, magnetic resonance imaging (MRI) is recommended for diagnostics, while computed tomography (CT) has proven more reliable and accurate in the assessment of scaphoid fracture characteristics and union.7–9
The aim of this review is to present an algorithm for diagnosis and treatment of acute scaphoid fractures.
Anatomy
The scaphoid forms an important mechanical linkage between the proximal and distal carpal rows. Approximately 80% of the surface of the scaphoid is covered with cartilage to articulate proximally with the distal radius, ulnarly with the lunate and capitate, and distally with the trapezoid and trapezium bone.10
Blood vessels that originate from the dorsal carpal branch of the radial artery enter the scaphoid through a capsular insertion on the dorsal ridge. They account for 70–80% of the scaphoid’s inter-osseous blood supply and represent the only vascular supply to the proximal pole. It has been suggested, but not confirmed, that the proximal pole receives additional blood supply through the radioscapholunate (Testut) ligament. On the palmar side, vessels from the superficial palmar branch of the radial artery enter at the palmar lateral aspect of the scaphoid tubercle. This accounts for 20–30% of the scaphoids inter-osseous blood supply, but solely in the distal pole area.11
Epidemiology
The scaphoid is the most commonly fractured carpal bone. It accounts for 60% of carpal fractures, 11% of hand fractures, and 2% of all fractures. Estimated annual incidence of scaphoid fractures is somewhere between 29 and 43 fractures per 100,000 persons.1,12,13 Most commonly, it occurs in young males from 15 to 25 years of age. The typical patient describes radial-sided wrist pain after a sports-related trauma involving a fall onto an outstretched hand, causing some extent of wrist hyperextension.
Fractures in the waist area account for two-thirds of all scaphoid fractures, of which the majority (60–85%) are non-displaced. Fractures in the distal third of the scaphoid represent 25% of scaphoid fractures, while 5–10% occur in the proximal third.14
Classification
Fracture classification adds important information for treatment and expected outcome. Available classification systems today are all based on radiographs. The most frequently used classification system is Herbert’s classification which is based on expected fracture instability.15,16 All bi-cortical fractures, except for fractures of the tubercle, are considered unstable and candidates for internal fixation. We find that such an approach may lead to considerable overtreatment. Russe classified scaphoid fractures based on fracture plane orientation into transverse, horizontal oblique and vertical oblique fractures.17 Vertical oblique fractures, which account for < 5% of scaphoid fractures, are highly unstable, which is why internal fixation is generally recommended. The Mayo classification that we use at our institution is essentially based on fracture location, and provides an appendix on factors attributable to instability.18 It provides a straight morphologic description that we find practical for clinical use. For comparison, the Mayo classification has a somewhat higher inter-observer reliability than the Herbert and Russe systems.19 Even though proximal pole fractures are incorporated within the Herbert and Mayo classification they lack a common definition. A more proximal fracture site has a higher probability of non-union, which is why it has been suggested to define proximal fractures as those within the proximal fifth of the scaphoid.20,21 Prosser developed a separate classification system for distal scaphoid fractures which has recently been modified by Clementson et al.22,23
Diagnosis
Clinical investigation
A thorough clinical investigation always includes a comparison with the opposite uninjured hand. The three most commonly used clinical tests for evaluation of patients with suspected scaphoid fracture include: anatomical snuff box tenderness, scaphoid tubercle tenderness, and pain on axial compression of the thumb.24 Sensitivity for the three individual tests has been reported to be 100%, with specificity increasing to 74% if all tests combined are positive. Of the clinical tests, pain on axial compression of the thumb has been demonstrated to have the weakest diagnostic performance.25 In concordance, it is our clinical experience that this test cannot stand alone as a predictor of scaphoid fracture (Fig.1).
Fig. 1.
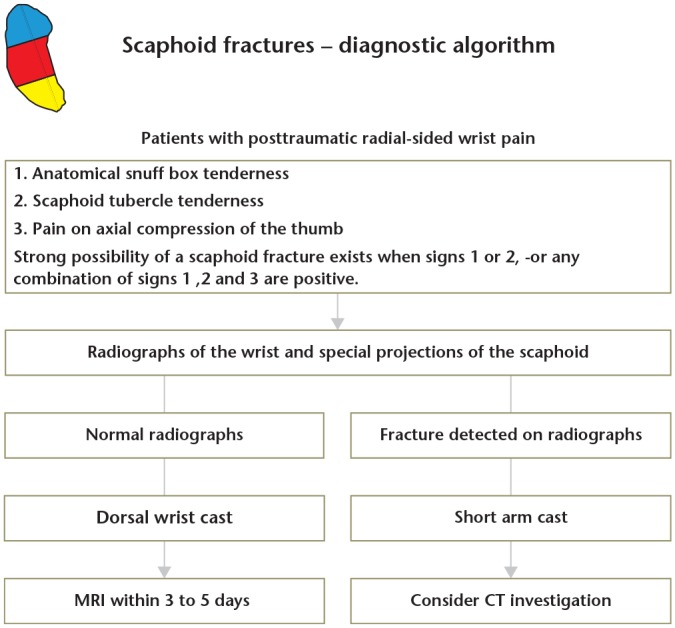
Scaphoid fractures: diagnostic algorithm.
Radiological investigation
Conventional radiography, including dorsopalmar and lateral imaging of the wrist are obtained in neutral position. Optimal visualization of the scaphoid on the dorsopalmar projection is achieved with closed fist and ulnar deviation. The purpose of this so-called Stecher’s view is to extend and thereby project the scaphoid in its entire length.26 A non-displaced or minimally displaced scaphoid fracture will only be detected if the X-ray beam is pointed parallel to the fracture line, which is why three to four special projections at difference angles of the scaphoid are recommended. However, the sensitivity of radiography to detect a scaphoid fracture is no higher than 70%.27
Traditionally, in cases of suspected scaphoid fracture where the initial radiographs are negative, patients had their wrist immobilized in a cast or splint for two weeks which was followed by repeated clinical and radiological examination. Consequently, this approach may lead to considerable overtreatment as in the end only 4–20% of cases are diagnosed with a fracture.13 As an alternative, several recent studies recommend MRI early on in cases of suspected scaphoid fracture, (Fig.1).2,9 With a sensitivity of 99–100%, it is cost effective to assure immediate diagnosis and adequate treatment.28 In addition, MRI can provide information on other fractures or ligament injuries in the affected wrist. Nonetheless, it is important to be aware that the difficulty of distinguishing a fracture from a bone bruise creates a potential risk for false-positive MRI scans.29 If MRI is not available, CT with a sensitivity of 93–95% is a reliable alternative.2 Latent class analysis, used in the absence of a reference standard, has estimated sensitivity for follow-up radiographs to be 91%.30 However, the reliability of six-week follow-up radiographs for diagnosis of scaphoid fractures has been questioned due to a low inter-observer agreement.31
When a diagnosis is established, reliable fracture classification is mandatory to support the surgeon in deciding on treatment as well as to estimate prognosis. Radiographs have been demonstrated to be less reliable to describe fracture morphology and to evaluate displacement. However, CT with the possibility of coronal and sagittal plane reconstructions in the longitudinal axis of the scaphoid provides more detailed fracture characteristics and allows quantitative measurement of fracture gap, translation (step-off), and angulation given by the intra-scaphoid angle.8,32
At our institution, if a scaphoid fracture is presented as a hair-thin line on some radiographs but not necessarily all, or diagnosed by MRI only, we do not proceed with CT. However, if the fracture is clearly visible on the radiographs and displacement or instability is suspected, we recommend supplementary CT (Fig.1).
It is agreed that fracture displacement and/or instability is correlated with prolonged time to union and increased risk of non-union.33 Generally, signs of instability include: fracture displacement > 1 mm, DISI (dorsal inter-calated segment instability) scaphoid-lunate angle > 60 degrees, lateral intra-scaphoid angle > 35 degrees, fracture comminution and a scaphoid fracture as part of a perilunate injury.18,34 At our institution fracture displacement is categorized as: non or minimally displaced (≤ 0.5 mm), moderately displaced (0.5–1.5 mm) or severely displaced (≥ 1.5 mm).5,6,32
A strong correlation has been demonstrated between scaphoid fracture comminution in the form of a radial-sided cortico or cortico-spongeous fragment and arthroscopically verified fracture instability.35 However, while fracture displacement in the majority of cases indicates instability, instability may also be found in non-displaced fractures. Also, arthroscopically verified scaphoid-lunate (SL) ligament rupture may co-exist with a non-displaced scaphoid fracture in up to 25% of cases.36
Radiation load after CT
A concern in CT investigations is the radiation load. Even so, the wrist does not contain radiation-sensitive red bone marrow. Additionally, a CT scan performed with the wrist above the head (superman position), keeps the radiation load to approximately 0.02 mSv, which is equivalent to seven days of background radiation. In comparison, CT of the shoulder exposes the patient to a radiation load of 2.0 mSv.37
Treatment
Before MRI
For patients with suspected scaphoid fracture where the initial radiographs are negative, major fracture displacement or instability is not expected. Consequently, we trust that immobilization in a dorsal wrist cast is sufficient until supplementary MRI has been carried out.
Negative MRI
In cases of post-traumatic radial-sided wrist pain and negative MRI, patients do not benefit from cast immobilization and can be mobilized early on.38 However, in such cases it is important to not overlook other wrist pathology such as intrinsic ligament injuries. Typically, radiologic signs of SL ligament rupture such as SL gap or DISI configuration may not appear until months after trauma. Even though contrast enhanced, high-field MRI may improve diagnostic sensitivity to detect intrinsic ligament injuries, arthroscopy is still considered the reference standard.39,40 A repeat clinical examination is advocated if symptoms have not diminished three to four weeks post trauma. If an SL ligament rupture is suspected, then surgery is recommended within six weeks post trauma.41
Scaphoid waist fractures
After adequate cast treatment, union is achieved at six weeks for approximately 90% of non or minimally displaced (≤ 0.5 mm) scaphoid waist fractures.5 Nevertheless, it is important to be aware that fracture comminution represented by a separate cortical or cortico-spongeous fragment on the radial side of the scaphoid, even in otherwise non-displaced fractures is associated with instability and prolonged time to union (Fig.2).5,35,42
Fig. 2.
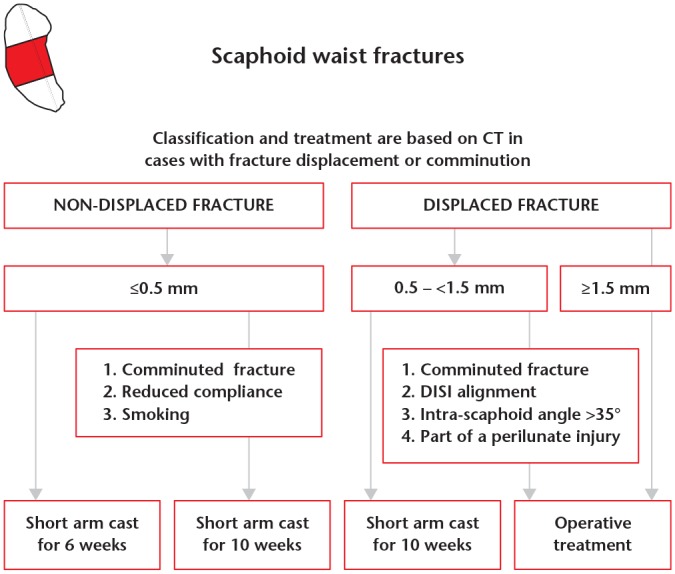
Scaphoid waist fractures: treatment algorithm.
Note. DISI, dorsal inter-calated segment instability.
In vivo studies have demonstrated that control of wrist extension and ulnar deviation is essential to stabilize the fracture site, while immobilization of forearm rotation or thumb metacarpophalangeal motion has limited impact on fracture stability.43 These findings have been supported in clinical studies demonstrating that the rate of fracture union is identical in cases with or without immobilization of the thumb.44 At our institution, we recommend conservative treatment with a standard short arm cast without thumb immobilization which, besides comfort, improves patients’ hand function as it allows thumb opposition and thereby enhances pinch grip.45
With development of minimally invasive, percutaneous techniques there has been a trend towards operative management of non or minimally displaced waist fractures. The short-term advantage of operative treatment is return to work or sports a few weeks earlier.46 However, internal fixation is associated with a higher complication rate (up to 30%) in terms of protruding hardware, infection, and scar-related problems.47–49 Furthermore, it may be followed by an increased (10%) long-term risk for development of scaphotrapezial (ST) joint osteoarthritis.46
Usually, a scaphoid waist fracture with a displacement > 1 mm has been considered unstable and thereby a candidate for internal fixation.18 We have previously demonstrated that fractures with a displacement < 1.5 mm united uneventfully in a thumb spica cast.5 Correspondingly, other authors have demonstrated that scaphoid fractures, even with dorsal or volar gapping of ≤ 2 mm, united after conservative treatment.4 We advocate internal fixation for all cases with ≥ 1.5 mm fracture displacement (Fig.2).5,6
Scaphoid fractures with moderate displacement (0.5–1.5 mm) require prolonged cast immobilization for eight to 10 weeks.5 However, surgical management should be considered if fracture instability (e.g. fracture comminution, DISI configuration, lateral intra-scaphoid angle > 35 degrees or a scaphoid fracture as part of a perilunate injury) is suspected (Fig.2).
In general, a volar approach is recommended for all scaphoid fractures in the waist and distal area.50 In accordance, when operative treatment is indicated for moderately displaced waist fractures, we advocate retrograde percutaneous internal fixation. A short incision over the distal, radial aspect of the scaphoid allows dissection down to the scaphoid-trapezium joint. A small periosteal elevator can help lever the scaphoid in a volar, radial direction, in order to get the guidewire entrance point in a more central axis than otherwise possible, or perpendicular to the fracture plane for horizontal oblique fractures. A trans-trapezial approach can sometimes be necessary to obtain sufficient central screw placement.51 For the rare vertical oblique fracture, we prefer screw positioning along the central axis, from the volar approach instead of screw placement perpendicular to the fracture plane, as it has limited biomechanical advantage and would only be possible using a dorsal approach.52 Minor fracture displacement can often be corrected with longitudinal traction and ulnar deviation of the carpus. Correct screw length is always 4–5 mm shorter than measured to avoid protrusion of the screw. Before closure, confirm alignment and screw position by fluoroscopy at multiple angles and make sure that passive motion of the wrist can be achieved without hindrance.
For severely displaced or angulated waist fractures, we recommend an open volar approach. With a dorsal approach, the important blood supply which enters at the dorsal ridge is at danger. Furthermore, the wrist hyperflexion, necessary with the dorsal approach, increases fracture angulation and hampers reduction of any humpback deformity. The open volar approach provides an excellent exposure of the volar surface of the scaphoid. Beware of not stripping the blood supply entering at the radial side of the tubercle. During closure it is essential to suture the volar radio-carpal ligaments as they are important constraints against ulnar translocation of the carpus as well as stabilizing the distal pole of the scaphoid.53
Arthroscopic assisted surgery has the advantage of providing direct fracture visualization, to ensure more accurate fracture reduction, to permit direct assessment for screw protrusion, and to allow detection of associated intrinsic and extrinsic ligament injuries.36 We recommend retrograde screw fixation with visualization of fracture reduction through the mid-carpal portals. Particularly, in cases with severe fracture dislocation/angulation, arthroscopy becomes technically demanding and requires long-term consistent experience with wrist arthroscopy. A thorough understanding of anatomy, portals and equipment is essential. Complications include iatrogenic cartilage injury, tendon and nerve injury, as well as equipment-related burns.54
Scaphoid proximal pole fractures
Proximal pole fractures have an inherent instability due to the small size of the fragment and an unbalanced linkage with the SL ligament on its dorsoulnar side only. Even so, there may be no ligament attachment at all depending on the orientation of the fracture line.55 The scaphoid following kinematics of both the proximal and distal carpal row leads to a large lever-arm stress affecting the proximal scaphoid especially during extension.56 Together with a tenuous blood supply, it predisposes proximal pole fractures to prolonged time to union and increased risk of non-union. Conservative treatment has been reported to result in a non-union rate of 10–14% for non-displaced fractures and as high as 50% for displaced fractures.57 A distinction between non-displaced and displaced fractures is crucial, which is why we recommend CT investigation for all proximal fractures and internal fixation if displacement is found (Fig.3). However, based on CT, a truly non-displaced fractures without signs of instability and not part of a high-energy trauma, can be considered for conservative treatment but with prolonged immobilization for 8 to 10 weeks (Fig.3).58
Fig. 3.
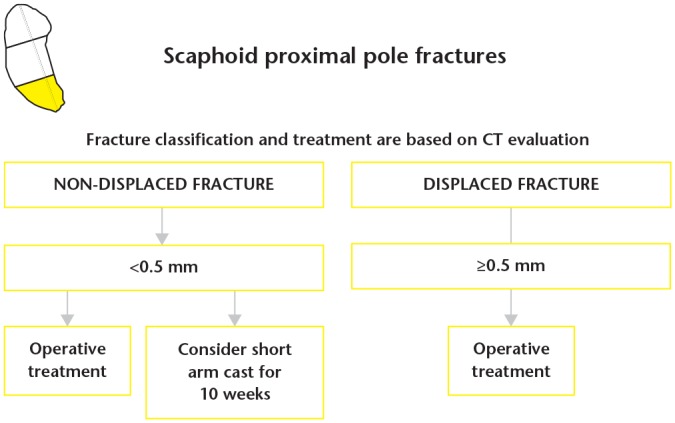
Scaphoid proximal pole fractures: treatment algorithm.
A volar surgical approach with the wrist in extension has an increased risk for displacement of a proximal pole fragment. Furthermore, it is difficult to securely engage the proximal fragment with the leading threads of the compression screw when inserted in the distal-to-proximal direction. Therefore, a dorsal approach is generally recommended.7 At our institution, we prefer a mini-open technique to visualize the fracture line as it allows a more precise screw placement as perpendicular to the fracture plane as possible. Also, it reduces the risk of extensor tendon damage. Small screw diameters such as 1.7 mm or 1.9 mm should be used to reduce the risk of splitting the fracture fragment. However, for the smallest fracture fragments of the proximal sixths of the scaphoid 0.8 mm or 0.9 mm K-wires may be the only possibility. There is no consensus regarding addition of bone grafting for internal fixation of acute proximal pole fractures.58,59
Distal scaphoid fractures
The distal third of the scaphoid is well vascularized, and fractures in this part of the scaphoid are often non or minimally displaced which has led to the current experience that these fractures heal uneventfully after conservative management.7 An avulsion of the radio-volar tip of the tuberosity with non or minimal articular involvement is the most common among this fracture type and accounts for more than 50% of all distal fractures.22,60 These fractures are sufficiently treated with four weeks of immobilization in a short arm cast or orthosis (Fig.4). The second most common fracture type of the distal scaphoid is an intra-articular fracture in the radial half of the joint surface caused by compression or shearing forces through the trapezium. A prolonged immobilization for four to six weeks is recommended (Fig.4). In rare cases, a comminute fracture pattern which involves the entire articular surface of the distal scaphoid is found. In such cases, we recommend a short arm cast with immobilization of the thumb for four to six weeks (Fig.4).
Fig. 4.
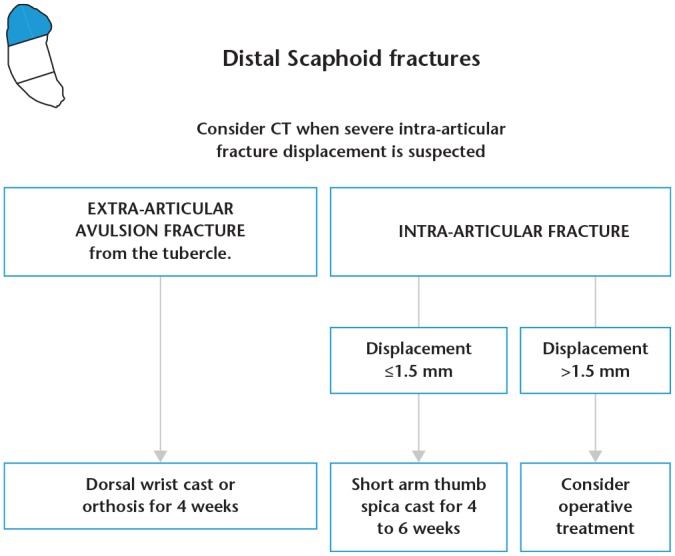
Distal scaphoid fractures: treatment algorithm.
From radiographs it can be difficult to assess displacement and congruency of the distal articular surface; CT is therefore of value if fracture displacement is suspected. If severe displacement is found, operative treatment may be considered.
Assessment of fracture union
Bone union should always be assessed by combining clinical investigation of the wrist with radiological findings. Persistent pain over the fracture site may indicate incomplete or delayed union, but may also relate to an associated injury. Still, long-term anatomical snuff box soreness is not uncommon even years after a united scaphoid fracture.23,61
Scaphoid fractures unite by primary bone healing; with direct remodelling of lamellar bone, the Haversian canals and blood vessels, and without external callous formation.62,63 This is similar to other intra-capsular fractures. However, primary bone healing is difficult to visualize and evaluate on radiographs and limited by poor inter-observer agreement.64 CT with its higher spatial resolution and possibilities to reconstruct images in the longitudinal axis of the scaphoid, has been demonstrated as a more reliable method to assess bone union.65 At our institution, using 1 mm or 2 mm thick reconstructions in the coronal and sagittal planes along the longitudinal axis of the scaphoid, we define bone union as continuous trabecular bridging over more than 50% of the cross-section of the fracture site.5,6,65
With CT to evaluate bone union, 90% of all non or minimally displaced scaphoid waist fractures can be mobilized at six weeks.5,6 However, if bone union is < 50%, but no adverse features such as increased fracture displacement, fracture line sclerosis or cystic changes are identified, then cast immobilization should be prolonged repeatedly in four week periods until union is achieved.7 The vast majority of fractures unite within 10 to 12 weeks of continuous cast treatment, which must be weighed against the risk of surgical complications if early surgical intervention is considered.66 However, with doubtful or delayed union at 12 to 14 weeks a change in treatment strategy towards internal fixation is recommended.5,67
We believe, that if the patient is more or less pain free and CT demonstrates substantial bone union, no further radiological examination is needed. However, in those cases where pain in the scaphoid area has not evidently diminished, and CT despite bone contact leaves an uncertainty about trabecular bridging the fracture site, a repeat CT after three to six months should be considered.
Return to work
A short arm cast without thumb immobilization will allow many patients with non or minimally physical work demands to resume their job early on. For manual workers with a repetitive or heavy upper extremity workload, a return to work requires that the scaphoid fracture is united as judged by CT (> 50% trabeculae bridging across the fracture site) and clinical examination.68 Furthermore, it is our experience that wrist range of motion and grip strength should be within 20–40% of the contralateral side.68
Conclusion
Scaphoid fractures are notorious for being difficult to diagnose as well as to obtain fracture union. In this report, we present our algorithms for diagnosis and treatment of acute scaphoid fractures. In the early phase post trauma, MRI is considered the reference standard for diagnosis of scaphoid fractures, while CT has an advantage in evaluation of fracture displacement and instability. At follow-up, CT investigation is the most reliable method to determine fracture union. After adequate conservative management, successful fracture union is achieved for approximately 90% of non or minimally displaced scaphoid waist fractures, at six weeks. With conservative treatment, a below-elbow cast leaving the thumb free is recommended. Severely displaced and unstable fractures should always be treated operatively. The choice of conservative or operative treatment of moderately displaced fractures may be based on the surgeon’s or patient’s preferences.
In recent years, MRI and CT have improved the diagnostics and classification of scaphoid fractures. For the future, a better understanding of, and ability to detect, true fracture instability is essential to help pinpoint cases with risk for prolonged healing or non-union.
The diagnostic and treatment algorithms are reproduced from Läkartidningen, Diagnostik och behandling av akuta skafoideumfrakturer, 18 June 2019, 18;116. pii: FL9M [Swedish], with permission.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg 1999;33:423–426. [DOI] [PubMed] [Google Scholar]
- 2. Jørgsholm P, Thomsen NO, Besjakov J, Abrahamsson SO, Björkman A. The benefit of magnetic resonance imaging for patients with posttraumatic radial wrist tenderness. J Hand Surg Am 2013;38:29–33. [DOI] [PubMed] [Google Scholar]
- 3. Ram AN, Chung KC. Evidence-based management of acute nondisplaced scaphoid waist fractures. J Hand Surg Am 2009;34:735–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Amirfeyz R, Bebbington A, Downing ND, Oni JA, Davis TR. Displaced scaphoid waist fractures: the use of a week 4 CT scan to predict the likelihood of union with nonoperative treatment. J Hand Surg Eur Vol 2011;36:498–502. [DOI] [PubMed] [Google Scholar]
- 5. Clementson M, Jørgsholm P, Besjakov J, Björkman A, Thomsen N. Union of scaphoid waist fractures assessed by CT scan. J Wrist Surg 2015;4:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Geoghegan JM, Woodruff MJ, Bhatia R, et al. Undisplaced scaphoid waist fractures: is 4 weeks’ immobilisation in a below-elbow cast sufficient if a week 4 CT scan suggests fracture union? J Hand Surg Eur Vol 2009;34:631–637. [DOI] [PubMed] [Google Scholar]
- 7. Suh N, Grewal R. Controversies and best practices for acute scaphoid fracture management. J Hand Surg Eur Vol 2018;43:4–12. [DOI] [PubMed] [Google Scholar]
- 8. Gilley E, Puri SK, Hearns KA, Weiland AJ, Carlson MG. Importance of computed tomography in determining displacement in scaphoid fractures. J Wrist Surg 2018;7:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ring D, Lozano-Calderón S. Imaging for suspected scaphoid fracture. J Hand Surg Am 2008;33:954–957. [DOI] [PubMed] [Google Scholar]
- 10. Berger RA. The anatomy of the scaphoid. Hand Clin 2001;17:525–532. [PubMed] [Google Scholar]
- 11. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg Am 1980;5:508–513. [DOI] [PubMed] [Google Scholar]
- 12. Larsen CF, Brøndum V, Skov O. Epidemiology of scaphoid fractures in Odense, Denmark. Acta Orthop Scand 1992;63:216–218. [DOI] [PubMed] [Google Scholar]
- 13. Duckworth AD, Jenkins PJ, Aitken SA, Clement ND, Court-Brown CM, McQueen MM. Scaphoid fracture epidemiology. J Trauma Acute Care Surg 2012;72:E41–E45. [DOI] [PubMed] [Google Scholar]
- 14. Garala K, Taub NA, Dias JJ. The epidemiology of fractures of the scaphoid: impact of age, gender, deprivation and seasonality. Bone Joint J 2016;98-B:654–659. [DOI] [PubMed] [Google Scholar]
- 15. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br 1984;66:114–123. [DOI] [PubMed] [Google Scholar]
- 16. Ten Berg PW, Drijkoningen T, Strackee SD, Buijze GA. Classifications of acute scaphoid fractures: a systematic literature review. J Wrist Surg 2016;5:152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Russe O. Fracture of the carpal navicular: diagnosis, non-operative treatment, and operative treatment. J Bone Joint Surg Am 1960;42-A:759–768. [PubMed] [Google Scholar]
- 18. Cooney WP, Dobyns JH, Linscheid RL. Fractures of the scaphoid: a rational approach to management. Clin Orthop Relat Res 1980;149:90–97. [PubMed] [Google Scholar]
- 19. Dean BJF, Riley ND, McCulloch ER, Lane JCE, Touzell AB, Graham AJ. A new acute scaphoid fracture assessment method: a reliability study of the ‘long axis’ measurement. BMC Musculoskelet Disord 2018;19:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Eastley N, Singh H, Dias JJ, Taub N. Union rates after proximal scaphoid fractures: meta-analyses and review of available evidence. J Hand Surg Eur Vol 2013;38:888–897. [DOI] [PubMed] [Google Scholar]
- 21. Ramamurthy C, Cutler L, Nuttall D, Simison AJ, Trail IA, Stanley JK. The factors affecting outcome after non-vascular bone grafting and internal fixation for nonunion of the scaphoid. J Bone Joint Surg Br 2007;89:627–632. [DOI] [PubMed] [Google Scholar]
- 22. Prosser AJ, Brenkel IJ, Irvine GB. Articular fractures of the distal scaphoid. J Hand Surg [Br] 1988;13:87–91. [DOI] [PubMed] [Google Scholar]
- 23. Clementson M, Thomsen N, Besjakov J, Jorgsholm P, Bjorkman A. Long-term outcomes after distal scaphoid fractures: a 10-year follow-up. J Hand Surg Am 2017;42:e921–e927. [DOI] [PubMed] [Google Scholar]
- 24. Parvizi J, Wayman J, Kelly P, Moran CG. Combining the clinical signs improves diagnosis of scaphoid fractures: a prospective study with follow-up. J Hand Surg [Br] 1998;23:324–327. [DOI] [PubMed] [Google Scholar]
- 25. Duckworth AD, Buijze GA, Moran M, et al. Predictors of fracture following suspected injury to the scaphoid. J Bone Joint Surg Br 2012;94:961–968. [DOI] [PubMed] [Google Scholar]
- 26. Compson JP, Waterman JK, Heatley FW. The radiological anatomy of the scaphoid. Part 2: radiology. J Hand Surg [Br] 1997;22:8–15. [DOI] [PubMed] [Google Scholar]
- 27. Gäbler C, Kukla C, Breitenseher MJ, Trattnig S, Vécsei V. Diagnosis of occult scaphoid fractures and other wrist injuries: are repeated clinical examinations and plain radiographs still state of the art? Langenbecks Arch Surg 2001;386:150–154. [DOI] [PubMed] [Google Scholar]
- 28. Hansen TB, Petersen RB, Barckman J, Uhre P, Larsen K. Cost-effectiveness of MRI in managing suspected scaphoid fractures. J Hand Surg Eur Vol 2009;34:627–630. [DOI] [PubMed] [Google Scholar]
- 29. De Zwart AD, Beeres FJ, Ring D, et al. MRI as a reference standard for suspected scaphoid fractures. Br J Radiol 2012;85:1098–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yin ZG, Zhang JB, Kan SL, Wang XG. Diagnostic accuracy of imaging modalities for suspected scaphoid fractures: meta-analysis combined with latent class analysis. J Bone Joint Surg Br 2012;94:1077–1085. [DOI] [PubMed] [Google Scholar]
- 31. Mallee WH, Mellema JJ, Guitton TG, Goslings JC, Ring D, Doornberg JN; Science of Variation Group. 6-week radiographs unsuitable for diagnosis of suspected scaphoid fractures. Arch Orthop Trauma Surg 2016;136:771–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bhat M, McCarthy M, Davis TR, Oni JA, Dawson S. MRI and plain radiography in the assessment of displaced fractures of the waist of the carpal scaphoid. J Bone Joint Surg Br 2004;86:705–713. [DOI] [PubMed] [Google Scholar]
- 33. Singh HP, Taub N, Dias JJ. Management of displaced fractures of the waist of the scaphoid: meta-analyses of comparative studies. Injury 2012;43:933–939. [DOI] [PubMed] [Google Scholar]
- 34. Grewal R, Suh N, Macdermid JC. Use of computed tomography to predict union and time to union in acute scaphoid fractures treated nonoperatively. J Hand Surg Am 2013;38:872–877. [DOI] [PubMed] [Google Scholar]
- 35. Buijze GA, Jørgsholm P, Thomsen NO, Björkman A, Besjakov J, Ring D. Factors associated with arthroscopically determined scaphoid fracture displacement and instability. J Hand Surg Am 2012;37:1405–1410. [DOI] [PubMed] [Google Scholar]
- 36. Jørgsholm P, Thomsen NO, Björkman A, Besjakov J, Abrahamsson SO. The incidence of intrinsic and extrinsic ligament injuries in scaphoid waist fractures. J Hand Surg Am 2010;35:368–374. [DOI] [PubMed] [Google Scholar]
- 37. Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am 2009;91:1882–1889. [DOI] [PubMed] [Google Scholar]
- 38. Clementson M, Thomsen N, Jørgsholm P, Besjakov J, Björkman A. Is early mobilisation better than immobilisation in the treatment of wrist sprains? J Plast Surg Hand Surg 2016;50:156–160. [DOI] [PubMed] [Google Scholar]
- 39. Andersson JK, Andernord D, Karlsson J, Friden J. Efficacy of magnetic resonance imaging and clinical tests in diagnostics of wrist ligament injuries: a systematic review. Arthroscopy 2015;31:2014–2020.e2. [DOI] [PubMed] [Google Scholar]
- 40. Thomsen NOB, Besjakov J, Björkman A. Accuracy of pre- and postcontrast, 3 T indirect MR arthrography compared with wrist arthroscopy in the diagnosis of wrist ligament injuries. J Wrist Surg 2018;7:382–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rohman EM, Agel J, Putnam MD, Adams JE. Scapholunate interosseous ligament injuries: a retrospective review of treatment and outcomes in 82 wrists. J Hand Surg Am 2014;39:2020–2026. [DOI] [PubMed] [Google Scholar]
- 42. Grewal R, Suh N, Macdermid JC. Use of computed tomography to predict union and time to union in acute scaphoid fractures treated nonoperatively. J Hand Surg Am 2013;38:872–877. [DOI] [PubMed] [Google Scholar]
- 43. Kawanishi Y, Oka K, Tanaka H, Sugamoto K, Murase T. In vivo scaphoid motion during thumb and forearm motion in casts for scaphoid fractures. J Hand Surg Am 2017;42:475. [DOI] [PubMed] [Google Scholar]
- 44. Buijze GA, Goslings JC, Rhemrev SJ, et al. ; CAST Trial Collaboration. Cast immobilization with and without immobilization of the thumb for nondisplaced and minimally displaced scaphoid waist fractures: a multicenter, randomized, controlled trial. J Hand Surg Am 2014;39:621–627. [DOI] [PubMed] [Google Scholar]
- 45. Karantana A, Downs-Wheeler MJ, Webb K, Pearce CA, Johnson A, Bannister GC. The effects of scaphoid and Colles casts on hand function. J Hand Surg [Br] 2006;31:436–438. [DOI] [PubMed] [Google Scholar]
- 46. Clementson M, Jørgsholm P, Besjakov J, Thomsen N, Björkman A. Conservative treatment versus arthroscopic-assisted screw fixation of scaphoid waist fractures: a randomized trial with minimum 4-year follow-up. J Hand Surg Am 2015;40:1341–1348. [DOI] [PubMed] [Google Scholar]
- 47. Ibrahim T, Qureshi A, Sutton AJ, Dias JJ. Surgical versus nonsurgical treatment of acute minimally displaced and undisplaced scaphoid waist fractures: pairwise and network meta-analyses of randomized controlled trials. J Hand Surg Am 2011;36:1759–1768. [DOI] [PubMed] [Google Scholar]
- 48. Bushnell BD, McWilliams AD, Messer TM. Complications in dorsal percutaneous cannulated screw fixation of nondisplaced scaphoid waist fractures. J Hand Surg Am 2007;32:827–833. [DOI] [PubMed] [Google Scholar]
- 49. Dias JJ, Wildin CJ, Bhowal B, Thompson JR. Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am 2005;87:2160–2168. [DOI] [PubMed] [Google Scholar]
- 50. Geissler WB, Adams JE, Bindra RR, Lanzinger WD, Slutsky DJ. Scaphoid fractures: what’s hot, what’s not. Instr Course Lect 2012;61:71–84. [PubMed] [Google Scholar]
- 51. Meermans G, Verstreken F. A comparison of 2 methods for scaphoid central screw placement from a volar approach. J Hand Surg Am 2011;36:1669–1674. [DOI] [PubMed] [Google Scholar]
- 52. Luria S, Lenart L, Lenart B, Peleg E, Kastelec M. Optimal fixation of oblique scaphoid fractures: a cadaver model. J Hand Surg Am 2012;37:1400–1404. [DOI] [PubMed] [Google Scholar]
- 53. Berger RA. The ligaments of the wrist: a current overview of anatomy with considerations of their potential functions. Hand Clin 1997;13:63–82. [PubMed] [Google Scholar]
- 54. Leclercq C, Mathoulin C; Members of EWAS. Complications of wrist arthroscopy: a multicenter study based on 10,107 arthroscopies. J Wrist Surg 2016;5:320–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Krimmer H. Management of acute fractures and nonunions of the proximal pole of the scaphoid. J Hand Surg [Br] 2002;27:245–248. [DOI] [PubMed] [Google Scholar]
- 56. Rainbow MJ, Kamal RN, Leventhal E, et al. In vivo kinematics of the scaphoid, lunate, capitate, and third metacarpal in extreme wrist flexion and extension. J Hand Surg Am 2013;38:278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Grewal R, Lutz K, MacDermid JC, Suh N. Proximal pole scaphoid fractures: a computed tomographic assessment of outcomes. J Hand Surg Am 2016;41:54–58. [DOI] [PubMed] [Google Scholar]
- 58. Brogan DM, Moran SL, Shin AY. Outcomes of open reduction and internal fixation of acute proximal pole scaphoid fractures. Hand (N Y) 2015;10:227–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Schreiber JJ, Kang L, Hearns KA, Pickar T, Carlson MG. Micro screw fixation for small proximal pole scaphoid fractures with distal radius bone graft. J Wrist Surg 2018;7:319–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Cockshott WP. Distal avulsion fractures of the scaphoid. Br J Radiol 1980;53:1037–1040. [DOI] [PubMed] [Google Scholar]
- 61. Dias JJ, Dhukaram V, Abhinav A, Bhowal B, Wildin CJ. Clinical and radiological outcome of cast immobilisation versus surgical treatment of acute scaphoid fractures at a mean follow-up of 93 months. J Bone Joint Surg Br 2008;90:899–905. [DOI] [PubMed] [Google Scholar]
- 62. Marsell R, Einhorn TA. The biology of fracture healing. Injury 2011;42:551–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kozin SH. Internal fixation of scaphoid fractures. Hand Clin 1997;13:573–586. [PubMed] [Google Scholar]
- 64. Dias JJ, Taylor M, Thompson J, Brenkel IJ, Gregg PJ. Radiographic signs of union of scaphoid fractures: an analysis of inter-observer agreement and reproducibility. J Bone Joint Surg Br 1988;70:299–301. [DOI] [PubMed] [Google Scholar]
- 65. Singh HP, Forward D, Davis TR, Dawson JS, Oni JA, Downing ND. Partial union of acute scaphoid fractures. J Hand Surg [Br] 2005;30:440–445. [DOI] [PubMed] [Google Scholar]
- 66. Buijze GA, Doornberg JN, Ham JS, Ring D, Bhandari M, Poolman RW. Surgical compared with conservative treatment for acute nondisplaced or minimally displaced scaphoid fractures: a systematic review and meta-analysis of randomized controlled trials. J Bone Joint Surg Am 2010;92:1534–1544. [DOI] [PubMed] [Google Scholar]
- 67. Rhemrev SJ, van Leerdam RH, Ootes D, Beeres FJ, Meylaerts SA. Non-operative treatment of non-displaced scaphoid fractures may be preferred. Injury 2009;40:638–641. [DOI] [PubMed] [Google Scholar]
- 68. Fowler JR, Hughes TB. Scaphoid fractures. Clin Sports Med 2015;34:37–50. [DOI] [PubMed] [Google Scholar]


