Abstract
Background
The aims of the present study were to determine whether a nurse-led program of care can improve medication adherence, quality of life (QoL), rates of rehospitalization, and all-cause mortality for chronic heart failure (CHF) patients.
Material/Methods
CHF patients were randomly assigned into either a control group or an intervention group. At 12 weeks, patients were followed up to evaluate the rate of medication adherence, QoL (as assessed by SF-12 physical and mental component score [PCS and MCS]), rehospitalization, and all-cause mortality.
Results
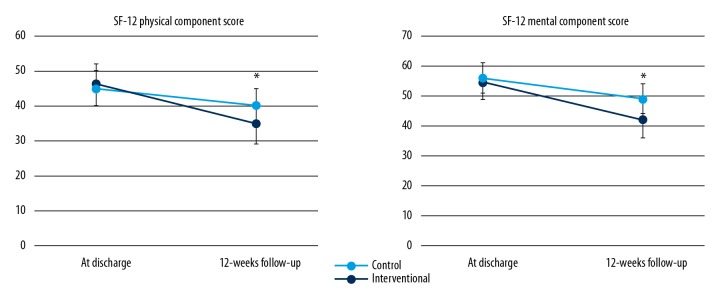
We recruited 152 patients. No significant differences in demographics, comorbidities, CHF severity, or etiology at baseline were observed. At discharge, no significant differences in medications prescription, PCS (46 vs. 45), or MCS (55 vs. 56) were observed. However, at 12-week follow-up, compared to the control group, patients in the intervention group were more likely to keep on medications therapy, with a significantly higher use of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker [73.8% vs. 59.7%], beta-blocker (62.5% vs. 51.4%), and aldosterone receptor antagonist (60% vs. 54.2%). Both PCS (35 vs. 40) and MCS (42 vs. 49) were also significantly lower in the control group versus the intervention groups (P<0.05). Patients in the control group had higher incident rate of rehospitalization (8.0% vs. 5.2% per person-week) than in the intervention group, with an incident rate ratio of 1.54 (95% confidence interval [CI]: 1.06–2.23).
Conclusions
A nurse-led discharge program of care can be a cost-effective and feasible approach for management of CHF patients in China.
MeSH Keywords: Heart Failure, Medication Adherence, Prognosis
Background
Chronic heart failure (CHF) is a leading cause of morbidity and mortality worldwide, including in China, although improvements in management have been achieved in the past decade [1–3]. In addition, patients with CHF have poor quality of life (QoL) and experience recurrent hospitalization due to HF exacerbation [3–5]. Developing and applying effective and efficient approaches to improve QoL and reduce rehospitalization for CHF patients is clinically relevant.
Prior studies from Western countries that have evaluated post-discharge programs designed to reduce rehospitalization and increase survival rates of CHF patients have demonstrated the effectiveness of such interventional strategies [6–9]. Interestingly and importantly, studies of nurse-led programs of care for CHF also confirmed these benefits, suggesting that nurses can play positive roles in the management of CHF patients after discharge [10–14]. However, data on the effectiveness and feasibility of these nurse-led programs for CHF patients in China are limited.
According to cardiovascular disease reports [15,16], the prevalence and incidence of CHF are continuously increasing in China. The economic loss related to CHF is also growing dramatically. Given the huge burden CHF imposes to the public health and economy in China, it is imperative to establish a cost-effectiveness approach. Nurse-led programs may be a feasible strategy for CHF patient management in China. Therefore, the aims of the present study were to evaluate whether nurse-led programs of care can improve medication adherence, QoL, rehospitalization, and all-cause mortality.
Material and Methods
Study populations
Patients were recruited through in-patient screening at our hospital. The inclusion criteria were: exacerbation of CHF during index hospitalization, left ventricular ejection fraction (LVEF) ≤45% as assessed by echocardiography, and discharge to home with stable status. The exclusion criteria were: life expectancy <6 months, mental illness (e.g., dementia), terminal illness (e.g., advanced stage of malignant disease), or received elective cardiac procedures (e.g., coronary artery bypass grafting or heart valve replacement) during the index hospitalization. Baseline characteristics and laboratory data were collected. This was an open-label interventional study that was approved by the Clinical Research Ethics Committee of Hainan Western Central Hospital. Informed consent was obtained before enrollment.
Nurse-led program of post-discharge intervention
Patients who were qualified and agreed to participate in our study were randomly assigned into 2 groups based on the last digit of their telephone number. Specifically, patients with an odd last digit were assigned to the control group and those with an even last digit were assigned to the intervention group. Patients in the control group received standard care (i.e., explanation of disease status, importance of adherence to guideline-directed medications therapy, low-salt diet, fluid restriction, and body weight monitoring daily by the ward nurses on the day of discharge). Patients in the interventional group received standard care plus post-discharge program of care during the first14 days (±2 days) after discharge. Specifically, nurse-specialists called patients by telephone to ask about their conditions (e.g., clinical symptoms and signs of HF and body weight change), to evaluate medications adherence, and to provide immediate feedbacks about what to do in the next step.
Study follow-up and endpoints
Patients were followed up via telephone call by nurse-specialists at 12 weeks (±5 days) after discharge. Study endpoints include the following domains: 1) the rate of medications adherence; in specific, during the follow-up, patients were asked by investigators how often they missed taking their medications, and medication adherence was defined as taking medications during >80% of the follow-up period, and medications refilled in the electronic healthcare system were used to confirm medications adherence; 2) the differences in QoL as assessed by the Short Form-12 (SF-12) physical and mental component scores (PCS and MCS) [17]; and 3) the incident rate of rehospitalization due to CHF exacerbation and all-cause mortality.
Statistical analysis
Continuous variables are presented as mean and standard deviation (SD) and categorial variables are presented as number and percentage. The t test was used to assess differences in continuous variables and the chi-square test was to assess differences in categorical variables. Incident rates of rehospitalization due to CHF exacerbation and all-cause mortality were calculated by dividing the number of events by person-weeks of follow-up accrued, and we then calculated the incident rate ratio (IRR) for rehospitalization and all-cause mortality for control versus intervention groups. The hazard ratio (HR) and 95% confidence interval (CI) for the adjusted Cox proportional hazards models were determined. All analyses were performed using SPSS 23.0, and a two-sided P value <0.05 was considered as statistical significance.
Results
Baseline characteristics comparisons by control and interventional groups
A study flowchart and patient enrollment are presented in Figure 1. A total of 152 patients were recruited into final analysis. As presented in Table 1, the mean of age, blood pressure, heart rate, estimated glomerular filtration rate (eGFR), and serum N-terminal pro-B-type natriuretic peptide (NT-proBNP) level at baseline were comparable between the control and intervention groups. The percentages of patients with comorbidities (smoking, obesity, hypertension, dyslipidemia, and diabetes) were also similar. The etiologies of CHF were also comparable, with ischemic etiology of 62.5% vs. 61.3%, idiopathic dilated cardiomyopathy of 18.1% vs. 18.8%, and valvular heart disease of 19.4% vs. 19.5% in both groups, respectively. The mean left ventricular ejection fraction (LVEF, 39.4% vs. 39.0%) and percentage of patients with New York Heart Association (NYHA) class III–IV (55.7% vs. 57.5%) were also without significant differences.
Figure 1.
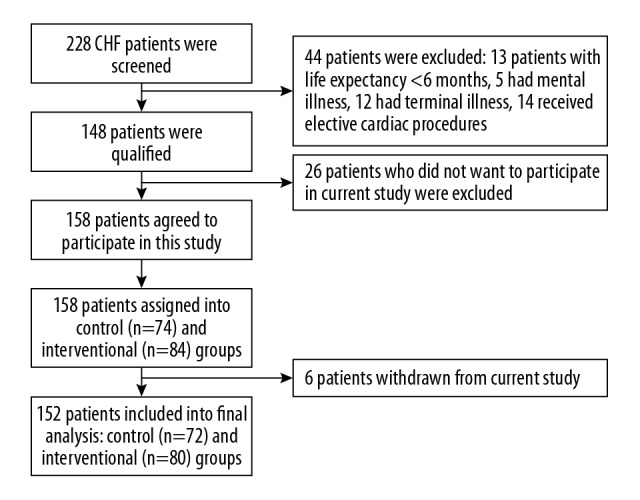
Study flowchart.
Table 1.
Comparisons of baseline characteristics.
| Variables | Control group (n=72) | Intervention group (n=80) |
|---|---|---|
| Age (years) | 51.3±10.6 | 50.8±9.9 |
| Male, n (%) | 53 (73.6) | 59 (73.8) |
| Systolic blood pressure, mm Hg | 135±14 | 133±13 |
| Diastolic blood pressure, mm Hg | 80±11 | 80±12 |
| Heart rate, beat per minute | 84±17 | 86±16 |
| Obese, n (%) | 22 (30.6) | 25 (31.3) |
| Smoking, n (%) | 35 (48.6) | 37 (46.3) |
| Hypertension, n (%) | 52 (72.2) | 57 (71.3) |
| Dyslipidemia, n (%) | 48 (66.7) | 53 (66.3) |
| Diabetes mellitus, n (%) | 43 (59.7) | 47 (58.8) |
| Creatinine (umol/L) | 72.4±17.5 | 73.1±15.9 |
| eGFR (ml/min/1.73 m2) | 70.8±14.6 | 69.6±15.5 |
| Glycated hemoglobin A1c (%) | 6.6±1.3 | 6.7±1.3 |
| LDL-cholesterol (mmol/L) | 3.2±0.9 | 3.3±1.0 |
| NT-proBNP (pg/mL) | 908.7±245.1 | 924.0±266.8 |
| Coronary heart disease, n (%) | 45 (62.5) | 49 (61.3) |
| Idiopathic dilated cardiomyopathy, n (%) | 13 (18.1) | 15 (18.8) |
| Valvular heart disease, n (%) | 14 (19.4) | 16 (19.9) |
| Left ventricular ejection fraction, (%) | 39.4±5.0 | 39.0±5.3 |
| NYHA class III–IV, n (%) | 39 (55.7) | 46 (57.5) |
eGFR – estimated glomerular filtration rate; LDL – low density lipoprotein; NT-proBNP – N-terminal pro-B type natriuretic peptide; NYHA – New York Heart Association
Medications use at discharge and follow-up
Medications use at discharge and follow-up were compared and are presented in Table 2, showing no significant differences in medications prescription at discharge. However, after 12 weeks of follow-up, compared to the control group, patients in the intervention group were more likely to keep on guideline-directed medications therapy, with a significantly higher use in angiotensin-converting enzyme inhibitor/angiotensin receptor blocker [(ACEi/ARB) 73.8% vs. 59.7%], beta-blocker (62.5% vs. 51.4%) and aldosterone receptor antagonist (60% vs. 54.2%).
Table 2.
Medications use at discharge and follow-up.
| Medications | Control group (n=72) | Intervention group (n=80) |
|---|---|---|
| At discharge | ||
| ACEi/ARB, n (%) | 58 (80.6) | 65 (81.3) |
| Beta-blocker, n (%) | 52 (72.2) | 58 (72.5) |
| Loop diuretic, n (%) | 72 (100) | 80 (100) |
| Aldosterone receptor antagonist, n (%) | 46 (63.9) | 49 (61.3) |
| Antiplatelet, n (%) | 50 (69.4) | 55 (68.7) |
| Statins, n (%) | 50 (69.4) | 58 (72.5) |
| Antidiabetic, n (%) | 40 (55.6) | 44 (55) |
| At 12-week follow-up | ||
| ACEi/ARB, n (%) | 43 (59.7) | 59 (73.8)* |
| Beta-blocker, n (%) | 37 (51.4) | 50 (62.5)* |
| Loop diuretic, n (%) | 67 (93.1) | 74 (92.5) |
| Aldosterone receptor antagonist, n (%) | 39 (54.2) | 48 (60)* |
| Antiplatelet, n (%) | 49 (68.1) | 53 (66.3) |
| Statins, n (%) | 50 (69.4) | 55 (68.9) |
| Antidiabetic, n (%) | 36 (50) | 41 (51.3) |
ACEi/ARB – angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; P<0.05 versus control group.
Comparisons of QoL
Quality of life as assessed by SF-12 PCS and MCS were compared between the control and intervention groups. As shown in Figure 2, no significant differences in PCS (46 vs. 45) or MCS (55 vs. 56) were observed at discharge. However, at 12-week follow-up, both PCS (35 vs. 40) and MCS (42 vs. 49) were significantly lower in the control group versus the intervention group (P<0.05).
Figure 2.
Comparison of physical component score and mental component score at discharge and at 12-week follow-up. * P<0.05 vs. interventional group.
Comparisons of rehospitalization and all-cause mortality
As presented in Table 3, at 12-week follow-up, patients in the control group had a higher incident rate of rehospitalization (8.0% vs. 5.2% per person-week) than in the interventional group due to acute exacerbation, with an incident rate ratio of 1.54 (95% confidence interval [CI]: 1.06–2.23). In addition, the composite of rehospitalization and all-cause mortality incident rate was also higher in the control group (8.5% vs. 5.4% per person-week), with an incident rate ratio of 1.57 (95% CI: 1.09–2.25).
Table 3.
Comparisons of rehospitalization and all-cause mortality.
| Control group (n=72) | Intervention group (n=80) | ||||
|---|---|---|---|---|---|
| Follow-up (weeks) | 828 | 944 | |||
| Average follow-up (weeks) | 11.5±0.2 | 11.6±0.3 | |||
| Events (n) | Rate | Events (n) | Rate | IRR (95% CI) | |
| Rehospitalization | 66 | 8.0% | 49 | 5.2% | 1.54 (1.06–2.23) |
| All-cause mortality | 4 | 0.5% | 2 | 0.2% | 2.28 (0.40–17.8) |
| Composite endpoints | 70 | 8.5% | 51 | 5.4% | 1.57 (1.09–2.25) |
IRR – incident rate ratio; CI – confidence interval.
Discussion
To the best of our knowledge, this is the first study to evaluate the efficacy of a nurse-led post-discharge program of care for CHF patients in China. Results of our study indicate that standard care plus a post-discharge program of care can improve adherence to guideline-directed medications therapy. In addition, this program is also beneficial for improvement of QoL and reduction of rehospitalization. These findings demonstrate that a nurse-led program of care can be a cost-effective and feasible approach for improvement of prognosis for CHF patients in China.
Although advancements in medications and devices therapy have been achieved in the last decade, CHF remains the leading cause of cardiovascular-related death and incurs huge economic losses worldwide [2,18]. Prior studies have demonstrated that CHF patients have a low rate of adherence to guideline-directed medications therapy [19–21]. In addition, these patients also tend to have recurrent hospitalizations due to rapid progression and worsening of their condition. It is notable that the 5-year mortality rate of CHF patients since first symptoms occurred is up to 50% [22,23]. These findings together strongly indicate that QoL and prognosis of CHF patients remain extremely poor. Studies to search for a cost-effective approach for risk reduction for these high-risk populations are needed.
Studies from Western countries have indicated that nurse-led programs of care can be a cost-effective and feasible approach. For example, Thompson et al. [13] reported that among CHF patients in northern England, a nurse-led clinic plus home-based intervention program of care reduced HF rehospitalization and mortality. Results from Hebert et al. [11] also show that a nurse-led disease management program was a reasonably cost-effective way to reduce the burden of CHF in a community-living USA population. Using case series, Coen et al. [10] also observed that a clinical nurse-specialist-led program of care can improve outcomes among CHF patients. Consistent with prior reports, findings from the present study also demonstrate that a nurse-led program of care plus standard care can provide additional benefits for CHF management in China. Specifically, we observed that during the first 2 weeks after discharge, making phone calls to follow up on CHF patients’ conditions, and then giving them immediate feedback based on the assessment, can improve patient adherence to guideline-directed medications therapy. In addition, the QoL and rehospitalization due to CHF exacerbation were also improved, which we considered might be at least partly due to the higher rate of adherence to medications therapy. Indeed, evidence from prior studies also demonstrated that CHF patients with good adherence to medications therapy had lower incidence of rehospitalization and mortality [24–26]. However, as presented in Table 2, although patients in the intervention group had higher rates of adherence to medications therapy than in the control group, compared to medications prescribed at discharge, the percentage of patients who continued on these medications therapy declined. Importantly, we also observed that QoL, as reflected by SF-12 physical and mental component scores, was also lower than at discharge. These findings together indicate that there is still room for improvement of CHF patient management. For example, more frequent follow-up strategies using phone calls or home-based interview by a nurse-specialist may be a viable option. Further studies are warranted to evaluate this hypothesis. The potential reasons for the efficacy of nurse-led programs are likely multifactorial. In conjunction with physicians, nurses can help monitor lifestyle modification and medications adherence among HF patients. Nurses can also help to identify the early stage of fluid overload and guide patients to increase their use of diuretics. Finally, nurses can also help provide consultation to HF patients regarding depression or anxiety. These roles played by nurses may in turn help to better manage HF patients.
Evaluating the time used for follow-up of each individual patient in the intervention group, we found that the average time used was 56 min (with SD of 8 min). Importantly, additional time used to follow-up these high-risk populations can reduce the absolute incident rate of rehospitalization by 2.8% per person-week and reduce the relative rate by 54%. Because recurrent hospitalization causes huge economic losses and burdens health care providers, we considered that the nurse-led post-discharge program of care would be a cost-effective and feasible approach, and findings from the present single-center study need to be corroborated in larger and multi-center national studies.
There are some limitations of the present study that need to be mentioned. First of all, although patients were randomly assigned to the control and intervention groups, nurse-specialists and physicians were not blinded to the assignments, which might have caused inherent biases such as observer bias. Randomized double-blinded trials are needed to confirm our findings. Second, the small sample size and short-term follow-up did not allow us to observe a mortality benefit of this interventional strategy. Studies with larger sample sizes and long-term follow-up are needed to evaluate whether this strategy can provide survival benefits. Third, this was a single-center study, and whether this strategy can be extrapolated to other areas of China and other population groups are unknown. Future studies in different populations are needed to corroborate the present findings. Third, no direct economic savings related to rehospitalization reduction was calculated in our current analysis. Future studies are needed to specifically collect data on economic expenditures. However, based on the experience at our center, prevention of one individual rehospitalization case due to HF exacerbation can avoid the expenditure of approximately $1000 US dollars on average. Last but not the least, due to the heterogeneous nature of culture, attitudes, and beliefs of urban vs. rural people and their utilization of health care, it is unknown whether the present findings can be extrapolated to other populations. Indeed, these non-clinical factors also play important roles in the management of HF patients around the world. Our preliminary findings suggest that future research should focus on whether longer-term of nurse-led programs can improve outcomes in terms of cardiovascular-related or all-cause death in HF patients and whether the benefits of nurse-led programs are associated with the duration of these interventional programs.
Conclusions
In conclusion, the results of the present study indicate that among patients with CHF, a nurse-led discharge program of care can increase adherence to guideline-directed medications therapy, improve QoL, and reduce rehospitalization. This appears to be a cost-effective and feasible approach that warrants corroboration by larger and multi-center national studies in the future.
Acknowledgment
We thank all the study participants. We also thank Dr. Fang Yang for helping with statistical analyses.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Liu S, Li Y, Zeng X, et al. Burden of cardiovascular diseases in China, 1990–2016: Findings from the 2016 Global Burden of Disease Study. JAMA Cardiol. 2019;4(4):342–52. doi: 10.1001/jamacardio.2019.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics – 2018 update: A report from the American Heart Association. Circulation. 2018;137:e67–492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 3.Balmforth C, Simpson J, Shen L, et al. Outcomes and effect of treatment according to etiology in HFrEF: An analysis of PARADIGM-HF. JACC Heart Fail. 2019;7:457–65. doi: 10.1016/j.jchf.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Cai A, Li X, Zhong Q, et al. Associations of high HDL cholesterol level with all-cause mortality in patients with heart failure complicating coronary heart disease. Medicine. 2016;95:e3974. doi: 10.1097/MD.0000000000003974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aimo A, Emdin M, Maisel AS. Sacubitril/valsartan, cardiac fibrosis, and remodeling in heart failure. J Am Coll Cardiol. 2019;73:3038–39. doi: 10.1016/j.jacc.2019.03.510. [DOI] [PubMed] [Google Scholar]
- 6.Maru S, Mudge AM, Suna JM, Scuffham PA. One-year cost-effectiveness of supervised center-based exercise training in addition to a post-discharge disease management program for patients recently hospitalized with acute heart failure: The EJECTION-HF study. Heart Lung. 2019;48(5):414–20. doi: 10.1016/j.hrtlng.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Milfred-LaForest SK, Gee JA, Pugacz AM, et al. Heart failure transitions of care: A pharmacist-led post-discharge pilot experience. Prog Cardiovasc Dis. 2017;60:249–58. doi: 10.1016/j.pcad.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Plakogiannis R, Mola A, Sinha S, et al. Impact of pharmacy student-driven postdischarge telephone calls on heart failure hospital readmission rates: A pilot program. Hosp Pharm. 2019;54:100–4. doi: 10.1177/0018578718769243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tak HJ, Chen LW, Wilson FA, et al. Post-discharge services for different diagnoses than index hospitalization predict decreased 30-day readmissions among medicare beneficiaries. J Gen Intern Med. 2019;34(9):1766–74. doi: 10.1007/s11606-019-05115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coen J, Curry K. Improving heart failure outcomes: The role of the clinical nurse specialist. Crit Care Nurs Q. 2016;39:335–44. doi: 10.1097/CNQ.0000000000000127. [DOI] [PubMed] [Google Scholar]
- 11.Hebert PL, Sisk JE, Wang JJ, et al. Cost-effectiveness of nurse-led disease management for heart failure in an ethnically diverse urban community. Ann Intern Med. 2008;149:540–48. doi: 10.7326/0003-4819-149-8-200810210-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luo ZC, Zhai L, Dai X. Does a Nurse-Led Program of Support and Lifestyle Management for patients with coronary artery disease significantly improve psychological outcomes among the patients?: A meta-analysis. Medicine. 2018;97:e12171. doi: 10.1097/MD.0000000000012171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson DR, Roebuck A, Stewart S. Effects of a nurse-led, clinic and home-based intervention on recurrent hospital use in chronic heart failure. Eur J Heart Fail. 2005;7:377–84. doi: 10.1016/j.ejheart.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review. Patient Educ Couns. 2018;101:363–74. doi: 10.1016/j.pec.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: A systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–72. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 16.Wang W, Hu SS, Kong LZ, et al. Summary of report on cardiovascular diseases in China, 2012. Biomed Environ Sc. 2014;27:552–58. doi: 10.3967/bes2014.085. [DOI] [PubMed] [Google Scholar]
- 17.Olseng MW, Olsen BF, Hetland A, et al. Quality of life improves in patients with chronic heart failure and Cheyne-Stokes respiration treated with adaptive servo-ventilation in a nurse-led heart failure clinic. J Clin Nurs. 2017;26:1226–33. doi: 10.1111/jocn.13416. [DOI] [PubMed] [Google Scholar]
- 18.Maggioni AP. Epidemiology of heart failure in Europe. Heart Fail Clin. 2015;11:625–35. doi: 10.1016/j.hfc.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Ruppar TM, Delgado JM, Temple J. Medication adherence interventions for heart failure patients: A meta-analysis. Eur J Cardiovasc Nurs. 2015;14:395–404. doi: 10.1177/1474515115571213. [DOI] [PubMed] [Google Scholar]
- 20.Diamant MJ, Virani SA, MacKenzie WJ, et al. Medical therapy doses at hospital discharge in patients with existing and de novo heart failure. ESC Heart Fail. 2019;6(4):774–83. doi: 10.1002/ehf2.12454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schofield T, Bhatia RS, Yin C, et al. Patient experiences using a novel tool to improve care transitions in patients with heart failure: A qualitative analysis. BMJ Open. 2019;9:e026822. doi: 10.1136/bmjopen-2018-026822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gandhi S, Mosleh W, Sharma UC, et al. Multidisciplinary heart failure clinics are associated with lower heart failure hospitalization and mortality: Systematic review and meta-analysis. Can J Cardiol. 2017;33:1237–44. doi: 10.1016/j.cjca.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Ni H, Xu J. Recent trends in heart failure-related mortality: United States, 2000–2014. NCHS Data Brief. 2015;(231):1–8. [PubMed] [Google Scholar]
- 24.Knafl GJ, Moser DK, Wu JR, Riegel B. Discontinuation of angiotensin-converting enzyme inhibitors or beta-blockers and the impact on heart failure hospitalization rates. Eur J Cardiovasc Nurs. 2019;18(8):667–78. doi: 10.1177/1474515119860321. [DOI] [PubMed] [Google Scholar]
- 25.Wu JR, Mark B, Knafl GJ, et al. A multi-component, family-focused and literacy-sensitive intervention to improve medication adherence in patients with heart failure-A randomized controlled trial. Heart Lung. 2019;48(6):507–14. doi: 10.1016/j.hrtlng.2019.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGee BT, Phillips V, Higgins MK, Butler J. Prescription drug spending and medication adherence among medicare beneficiaries with heart failure. J Manag Care Spec Pharm. 2019;25:705–13. doi: 10.18553/jmcp.2019.25.6.705. [DOI] [PMC free article] [PubMed] [Google Scholar]