Abstract
BACKGROUND:
The economic recession of 2008–2009 resulted in unprecedented employment and economic losses leading to deterioration of cardiovascular health. We examined the trends in ideal cardiovascular health as measured by the American Heart Association’s (AHA’s) Life’s Simple 7 metric during the periods of economic recession and subsequent economic recovery.
METHODS:
Data on adults ages ≥20 years from the NHANES from economic-recession (2007–2010) and post-recession (2011–2016) periods was analyzed. The AHA’s Life’s Simple 7 score of 10–14 was used to classify ideal cardiovascular health status. Socioeconomic status was divided into 3 categories: high, middle, and low based on education and income status. Multivariable linear and logistic regression models including demographics, insurance status, health care access, and adjustment for multiple testing were used to analyze the trends in prevalence of ideal cardiovascular health across socioeconomic strata.
RESULTS:
We observed a decline in the multivariable-adjusted mean cardiovascular health score from 8.18 in 2007–2010 to 7.94 in 2015–2016 (Plinear = 0.02). This was primarily driven by the increasing prevalence of obesity (34% in 2007–2010 vs 41% in 2015–2016, Plinear = 0.005) and poor fasting glucose (8% in 2007–2010 vs 12% in 2015–2016, Plinear = 0.003). In multivariable-adjusted models, we observed the decreasing prevalence of ideal cardiovascular health with a nonlinear trend in the participants in the highest (51% in 2007–2010 vs 42% in 2015–2016, Pquadratic = 0.01) and lowest socioeconomic strata (16% in 2007–2010 vs 13% in 2015–2016, Pquadratic = 0.02). The prevalence of ideal cardiovascular health was higher in participants with high-socioeconomic status compared with other socioeconomic status participants.
CONCLUSIONS:
Despite economic recovery, ideal cardiovascular health metrics have not yet recovered. Cardiovascular health appears to be further deteriorating for US adults, particularly those in high- and lower-socioeconomic strata.
Keywords: Cardiovascular disease, Diabetes mellitus, Obesity
INTRODUCTION
Economic downturn can impact the general health of the population.1,2 The effect on cardiovascular health may be particularly profound.3 From the mid 2000s to 2010, there was a significant economic decline with a concomitant deterioration in population-level health.4,5 This period was characterized by a staggering rise in unemployment and financial losses and has, therefore, been widely accepted as a period of economic recession.6 A prior population-based cohort study has shown the deleterious effects of the economic recession on blood pressure and blood glucose levels in the United States.3 There has also been evidence to suggest that economic recession had varying degrees of adverse effects on population health among subgroups (eg, younger vs older individuals, women vs men, whites vs other races, higher vs lower level of educational attainment).1,3,7–9
The AHA’s Life’s Simple 7 is a relatively simple metric to capture the state of cardiovascular health at the population level.10 The Life’s Simple 7 is composed of the following 7 metrics that can be used to signify “ideal cardiovascular health”: nonsmoking, body mass index (BMI) less than 25 kg/m2, physical activity at goal levels, diet consistent with current guideline recommendations, total cholesterol less than 200 mg/dL, blood pressure less than 120/80 mm Hg, and fasting serum glucose less than 100 mg/dL.11 A poor status of Life’s Simple 7 score has been associated with multiple adverse cardiovascular outcomes such as incident heart failure,12,13 atrial fibrillation,14 and prognosis after myocardial infarction.15
We hypothesized that the macroeconomic fluctuations noted during the economic recession and the subsequent economic recovery would be associated with cardiovascular health metrics of US adults ages 20 years and older. Furthermore, we hypothesized that the age, sex, race, insurance status, access to health care adjusted time trends in prevalence of ideal cardiovascular health, as captured by Life’s Simple 7 metrics, varied among adults from different socioeconomic strata. We used the National Health and Nutrition Examination Survey (NHANES) from 2007 to 2016 to evaluate our hypotheses.
METHODS
Data Source and Study Population
We used the data from participants of 5 NHANES cycles spanning from 2007–2008 to 2015–2016.16 Description of NHANES data set is briefly outlined in Supplemental Method 1 (Online Appendix A). Participants prior to 2007–2008 (prerecession period) were not included in the study because of significant changes in the measurement and coding of physical activity (ie, a component of Life’s Simple 7 metrics) in NHANES from 2007–2008 onward.17 Furthermore, there is a lack of availability of NHANES data during the period of 2008–2009 as a separate data set. In an effort to keep the longitudinal assessment and coding constant while examining NHANES cycles for the impact of the economy on cardiovascular health, we performed the following steps to identify study participants: 1) we merged the data sets from 2007 to 2010 NHANES surveys into 1 period to classify these survey years as a period of economic recession; and 2) the data from the NHANES survey years 2011 to 2016 were treated as separate data sets to assess trends in the postrecession or economic recovery period. The flow chart for selection of the study population is outlined in Supplemental Figure 1 and Supplemental Method 2 (Online Appendix A). As NHANES dataset contains deidentified publicly available data, this study was exempt from IRB of the University of Alabama at Birmingham.
Age and sex were self-reported. Self-reported race and ethnicity was categorized into 4 levels: non-Hispanic whites, non-Hispanic blacks, Mexican American, and others. Health insurance status (Yes/No) and total number of health care visits in past 1 year were also self-reported. These measures were included as surrogates for health care access.
Definition of Cardiovascular Health Metrics
The cardiovascular health metrics were identified using the AHA’s Life’s Simple 7 behavioral and health factors. The Life’s Simple 7 metrics are grouped into the ideal health behaviors (ie, smoking status, BMI, physical activity, and healthy diet score) and ideal health factors are (ie, total cholesterol, blood pressure, and fasting plasma glucose). Each cardiovascular health metric was categorized into the ideal, intermediate, and poor categories and given a point score of 2, 1, and 0, respectively (Supplemental Table 1, Online Appendix A).10,11 The NHANES questionnaire list was used to identify the self-reported smoking status (ie, current, former, or non-smoker) (Supplemental Table 1). The BMI was calculated based on the anthropometric parameters that were measured by the trained health technician during the mobile examination. The manner in which we classified subjects’ physical activity levels and the healthy diet score is outlined in detail in Supplemental Method 3 (Online Appendix A). As outlined in a previous study,18 the poverty income ratio and years of education were used to categorize the socioeconomic status (Supplemental Method 4, Online Appendix A).
Statistical Analysis
SAS version 9.4 (SAS Institute Inc., Cary, NC) was used to perform all of the statistical analyses. Detailed description of all the statistical analyses including sensitivity analysis is outlined in Supplemental Method 5 (Online Appendix A).
RESULTS
Table 1 outlines the age-standardized weighted sample characteristics for each of the NHANES cycles included in our study. As shown, the demographic and socioeconomic characteristics of the study participants were similar across the NHANES survey cycles (Table 1). The mean age of study participants was 45 years, 51% were females, and ~67% were non-Hispanic whites from 2007–2010 through 2015–2016 (Table 1). The proportion of participants in the different strata of socioeconomic status (a combination of education and income status) remained similar during the study period (Table 1). There was a modest increase (~6%) in the proportion of individuals with insurance from 2007–2010 to 2015–2016 (Table 1).
Table 1.
Characteristics of American Adults From NHANES 2007–2016
| NHANES 2007–2010 | NHANES 2011–2012 | NHANES 2013–2014 | NHANES 2015–2016 | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) |
| Age, years | 4369 | 45 (32–58) | 2012 | 46 (33–59) | 2102 | 46 (32–59) | 2017 | 47 (32–60) |
| Age Group | ||||||||
| 20–29 | 707 | 20 (18–22) | 362 | 18 (15–21) | 335 | 19 (16–21) | 318 | 19 (17–21) |
| 30–39 | 709 | 18 (16–19) | 372 | 18 (15–21) | 361 | 18 (16–21) | 330 | 17 (15–19) |
| 40–49 | 790 | 20 (18–23) | 347 | 20 (16–23) | 397 | 19 (16–23) | 339 | 18 (15–21) |
| 50–59 | 730 | 19 (17–21) | 330 | 19 (16–21) | 373 | 19 (16–22) | 352 | 18 (16–21) |
| 60–69 | 692 | 12 (10–13) | 314 | 15 (12–17) | 341 | 15 (12–17) | 373 | 17 (15–20) |
| ≥70 | 741 | 11 (10–12) | 287 | 11 (10–13) | 295 | 11 (8–13) | 305 | 10 (8–12) |
| Sex | ||||||||
| Male | 2122 | 49 (47–51) | 1025 | 49 (46–52) | 1013 | 49 (47–51) | 988 | 49 (47–51) |
| Female | 2247 | 51 (49–53) | 987 | 51 (48–54) | 1089 | 51 (49–53) | 1029 | 51 (49–53) |
| Race | ||||||||
| Non-Hispanic White | 2111 | 70 (65–74) | 787 | 67 (59–75) | 947 | 67 (60–74) | 694 | 64 (55–73) |
| Non-Hispanic Black | 742 | 11 (8–13) | 445 | 11 (7–16) | 381 | 11 (8–14) | 396 | 11 (6–16) |
| Mexican American | 815 | 8 (6–11) | 221 | 8 (4–12) | 278 | 9 (6–12) | 334 | 8 (4–13) |
| Other | 701 | 11 (9–14) | 559 | 14 (10–17) | 496 | 13 (9–17) | 593 | 17 (13–20) |
| Family Poverty Income Ratio | ||||||||
| ≥3.50 | 1223 | 41 (38–44) | 559 | 38 (30–46) | 619 | 39 (31–46) | 535 | 39 (33–44) |
| 1.30–3.49 | 1541 | 34 (31–37) | 647 | 34 (29–38) | 674 | 32 (30–35) | 731 | 35 (31–39) |
| <1.30 | 1605 | 25 (23–28) | 806 | 28 (23–33) | 809 | 29 (21–37) | 751 | 27 (23–31) |
| Education | ||||||||
| ≤12 year | 2275 | 42 (38–46) | 876 | 36 (31–42) | 894 | 36 (29–43) | 910 | 37 (29–44) |
| Some College | 1166 | 29 (27–31) | 595 | 32 (29–35) | 653 | 33 (29–36) | 588 | 32 (27–36) |
| College Graduate | 922 | 29 (26–32) | 540 | 32 (25–38) | 554 | 31 (26–36) | 519 | 32 (24–40) |
| Socioeconomic Status | ||||||||
| High | 1125 | 38 (35–41) | 530 | 37 (29–44) | 592 | 37 (29–45) | 511 | 37 (32–43) |
| Middle | 2506 | 52 (49–55) | 1172 | 53 (47–60) | 1212 | 53 (48–58) | 1217 | 55 (50–59) |
| Low | 732 | 9 (8–11) | 309 | 10 (8–13) | 297 | 9 (6–13) | 289 | 8 (6–10) |
| Insurance Status | 4369 | 80 (79–82) | 2012 | 80 (77–84) | 2102 | 82 (78–85) | 2017 | 86 (82–89) |
| Number of Health Care Visits | ||||||||
| None | 752 | 16 (14–18) | 324 | 15 (12–18) | 329 | 15 (11–18) | 352 | 17 (16–19) |
| 1 to 3 | 1969 | 48 (46–51) | 934 | 47 (43–51) | 976 | 48 (44–52) | 941 | 50 (47–53) |
| ≥4 | 1647 | 36 (33–38) | 754 | 38 (35–41) | 797 | 37 (35–40) | 724 | 33 (30–36) |
CI = confidence interval; NHANES = National Health and Nutrition Examination Survey; No. = number.
Overall Trends in Cardiovascular Health
As described in Table 2, the prevalence of obesity (BMI ≥30 kg/m2) significantly increased from 2007–2010 to 2015–2016 (Plinear =0.005). Additionally, the prevalence of ideal fasting blood glucose showed a quadratic trend (P <0.001), initially increasing from 2007–2010 to 2013–2014, but then decreasing in 2015–2016. The prevalence of cardiovascular health metrics such as smoking, physical activity, healthy diet score, total cholesterol, and blood pressure remained unchanged (Plinear and Pquadratic >0.05).
Table 2.
Age Standardized Weighted Prevalence of Cardiovascular Health Metrics Among US Adults-NHANES 2007–2016
| NHANES 2007–2010* | NHANES 2011–2012* | NHANES 2013–2014* | NHANES 2015–2016* | Trend P value† | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cardiovascular Health‡ | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | Linear | Quadratic |
| Smoking | ||||||||||
| Current | 920 | 21 (19–22) | 395 | 19 (16–23) | 410 | 19 (15–23) | 392 | 19 (16–22) | 0.87 | 0.46 |
| Former | 433 | 11 (10–12) | 190 | 10 (7–12) | 206 | 10 (8–12) | 219 | 13 (10–16) | 0.12 | 0.33 |
| Never | 3016 | 68 (66–71) | 1427 | 71 (67–74) | 1486 | 71 (67–75) | 1406 | 68 (64–72) | 0.33 | 0.21 |
| Physical Activity | ||||||||||
| None | 1198 | 22 (20–24) | 460 | 21 (17–25) | 530 | 24 (23–26) | 547 | 21 (18–25) | 0.66 | 0.16 |
| Intermediate | 1002 | 25 (23–27) | 521 | 25 (21–30) | 546 | 27 (24–30) | 483 | 26 (23–30) | 0.48 | 0.29 |
| Ideal | 2169 | 53 (50–55) | 1031 | 54 (50–57) | 1026 | 49 (46–52) | 987 | 52 (50–55) | 0.19 | 0.04 |
| Body Mass Index (kg/m2) | ||||||||||
| ≥30 | 1624 | 34 (32–36) | 731 | 35 (31–39) | 782 | 37 (35–39) | 821 | 41 (36–45) | 0.005 | 0.50 |
| 25–29.9 | 1507 | 34 (32–36) | 652 | 34 (31–36) | 673 | 33 (31–36) | 654 | 32 (30–34) | 0.27 | 0.94 |
| <25 | 1238 | 32 (30–34) | 629 | 31 (27–36) | 647 | 30 (27–33) | 542 | 27 (23–31) | 0.03 | 0.62 |
| Healthy Diet Score | ||||||||||
| 0–1 components | 3353 | 78 (77–80) | 1510 | 78 (75–82) | 1649 | 79 (77–82) | 1522 | 79 (76–82) | 0.50 | 0.55 |
| ≥2 components | 1016 | 22 (20–23) | 502 | 22 (18–24) | 453 | 21 (18–23) | 495 | 21 (18–24) | ||
| Total Cholesterol (mg/dL) | ||||||||||
| >240 | 579 | 13 (12–14) | 215 | 11 (9–13) | 227 | 11 (9–13) | 248 | 13 (10–15) | 0.91 | 0.09 |
| 200–239 | 1796 | 39 (36–41) | 862 | 44 (41–47) | 852 | 40 (36–45) | 834 | 39 (36–43) | 0.27 | 0.50 |
| <200 | 1994 | 48 (46–50) | 935 | 45 (42–49) | 1023 | 48 (44–53) | 935 | 48 (44–52) | 0.24 | 0.76 |
| Blood Pressure (mm Hg) | ||||||||||
| ≥140/≥90 | 641 | 11 (10–12) | 273 | 11 (10–13) | 284 | 12 (9–14) | 338 | 13 (11–15) | 0.21 | 0.96 |
| 120–139/80–89 | 1618 | 36 (34–38) | 801 | 40 (37–43) | 751 | 34 (31–38) | 798 | 39 (36–43) | 0.64 | 0.23 |
| <120–80 | 2110 | 53 (50–56) | 938 | 49 (45–52) | 1067 | 54 (51–57) | 881 | 48 (43–52) | 0.76 | 0.15 |
| Fasting Blood Glucose (mg/dL) | ||||||||||
| ≥126 | 517 | 8 (7–9) | 240 | 9 (6–11) | 237 | 10 (8–12) | 309 | 12 (10–14) | 0.003 | 0.40 |
| 100–125 | 1867 | 42 (40–44) | 786 | 39 (37–42) | 788 | 35 (31–38) | 926 | 46 (42–51) | 0.66 | <0.001 |
| <100 | 1985 | 50 (47–53) | 986 | 52 (49–55) | 1077 | 55 (51–60) | 782 | 42 (37–46) | 0.04 | <0.001 |
| Cardiovascular Health§ | 4364 | 8.18 (8.07–8.29) | 2012 | 8.23 (8.06–8.40) | 2100 | 8.19 (8.04–8.34) | 2012 | 7.94 (7.73–8.16) | 0.02 | 0.02 |
| Number of Ideal Cardiovascular Health Metrics | ||||||||||
| 0 | 116 | 2 (1–3) | 53 | 2 (2–3) | 55 | 2 (2–3) | 59 | 3 (2–4) | 0.47 | 0.79 |
| 1 | 601 | 11 (10–13) | 290 | 15 (12–17) | 273 | 12 (11–14) | 331 | 16 (12–19) | 0.22 | 0.76 |
| 2 | 1095 | 23 (21–25) | 454 | 20 (18–23) | 483 | 22 (19–25) | 555 | 26 (22–29) | 0.13 | 0.27 |
| 3 | 1183 | 27 (25–29) | 512 | 25 (23–28) | 506 | 24 (21–27) | 501 | 24 (21–27) | 0.10 | 0.18 |
| 4 | 817 | 21 (19–23) | 382 | 20 (18–23) | 436 | 22 (19–25) | 319 | 18 (15–21) | 0.39 | 0.35 |
| 5 | 435 | 12 (10–13) | 239 | 12 (10–15) | 266 | 13 (11–15) | 198 | 11 (8–13) | 0.71 | 0.17 |
| ≥6 | 122 | 4 (3–5) | 82 | 4 (3–6) | 83 | 5 (3–6) | 54 | 3 (1–5) | 0.47 | 0.11 |
CI = confidence interval; NHANES = National Health and Nutrition Examination Survey; No. = number.
Direct method for age standardization was performed using the US 2000 census population age-groups 20–29, 30–39, 40–49, 50–59, 60–69, ≥70 years or older.
The orthogonal polynomial model including age groups, race, sex, insurance status, number of health care visits, and Bonferroni correction for multiple testing was used to assess the linear and quadratic trend P value across the survey years.
All the participants 20 years or older with available cardiovascular health metrics were included.
Age, sex, race, and insurance status-adjusted mean cardiovascular health metric with 95% CI from NAHNES 2007–2016.
From the economic recession to the economic recovery period, the age, sex, race, insurance status, and number of health care visits adjusted mean cardiovascular health score decreased marginally, albeit significantly, from 8.18 (95% confidence interval [CI] 8.07–8.29) in 2007–2010 to 7.94 (95% CI 7.73–8.16) in 2015–2016 (Plinear=0.02; Table 2). Odds of fasting blood glucose ≥126 mg/dL were 25% higher (95% CI 1.03–1.52) and obesity were 15% (95% CI 1.01–1.30) higher in the postrecession survey cycles (2011–2016) compared with the recession period (2007–2010; Table 3).
Table 3.
Adjusted Odds Ratio of Cardiovascular Health Metrics in the Post-Recession Years (2011–2016) Compared With Recession Years (2007–2010) From NHANES
| Odds Ratio (95% CI) | |
|---|---|
| Cardiovascular Health* | 2011–2016 vs 2007–2010 |
| Smoking | |
| Current | 0.95 (0.81–1.12) |
| Former | 1.04 (0.84–1.27) |
| Never | 1.03 (0.89–1.18) |
| Physical Activity | |
| None | 0.98 (0.84–1.14) |
| Intermediate | 1.05 (0.87–1.26) |
| Ideal | 0.98 (0.85–1.12) |
| Body Mass Index (kg/m2) | |
| ≥30 | 1.15 (1.01–1.30) |
| 25–29.9 | 0.96 (0.85–1.09) |
| <25 | 0.89 (0.76–1.05) |
| Healthy Diet Score | |
| 0–1 components | 1.05 (0.89–1.24) |
| ≥2 components | 0.96 (0.81–1.13) |
| Total Cholesterol (mg/dL) | |
| >240 | 0.86 (0.71–1.04) |
| 200–239 | 1.07 (0.92–1.25) |
| <200 | 1.01 (0.85–1.19) |
| Blood Pressure (mm Hg) | |
| ≥140/≥90 | 1.06 (0.86–1.32) |
| 120–139/80–89 | 1.06 (0.91–1.23) |
| <120–80 | 0.92 (0.78–1.08) |
| Fasting Blood Glucose (mg/dL) | |
| ≥126 | 1.26 (1.01–1.59) |
| 100–125 | 0.91 (0.77–1.06) |
| <100 | 1.03 (0.86–1.23) |
CI = confidence interval; NHANES, National Health and Nutrition Examination Survey.
Adjusted for age, sex, race, insurance status, and number of health care visits.
Among participants with high socioeconomic status, the mean cardiovascular health score, adjusted for age, sex, race, insurance status, and number of health care visits, decreased from 9.4 (95% CI 8.9–9.8) in 2007–2010 to 8.7 (95% CI 8.2–9.3) in 2015–2016 (Plinear =0.007) (Figure 1, Panel A). However, among lower socioeconomic strata, the adjusted mean cardiovascular health score increased from 7.4 (95% CI 6.6–8.1) in 2007–2010 to 8.4 (95% CI 7.7–9.2) in 2011–2012 and then subsequently declined to 7.0 (95% CI: 6.0–8.0) in 2015–2016 (Pquadratic =0.007). In the higher socioeconomic strata, there was a decline in the prevalence of ideal cardiovascular health from 51% in 2007–2010 to 42% in 2015–2016 (Pquadratic =0.01; Figure 1, Panel B). However, among lower socioeconomic strata, the prevalence of ideal cardiovascular health increased from 16% in 2007–2010 to 26% in 2011–2012 and then declined to 13% in 2015–2016 (Pquadratic =0.02). We did not observe any trend in the mean cardiovascular health score or the prevalence of ideal cardiovascular health among participants in the middle socioeconomic stratum (Plinear and Pquadratic >0.05; Figure 1, Panels A and B).
Figure 1.
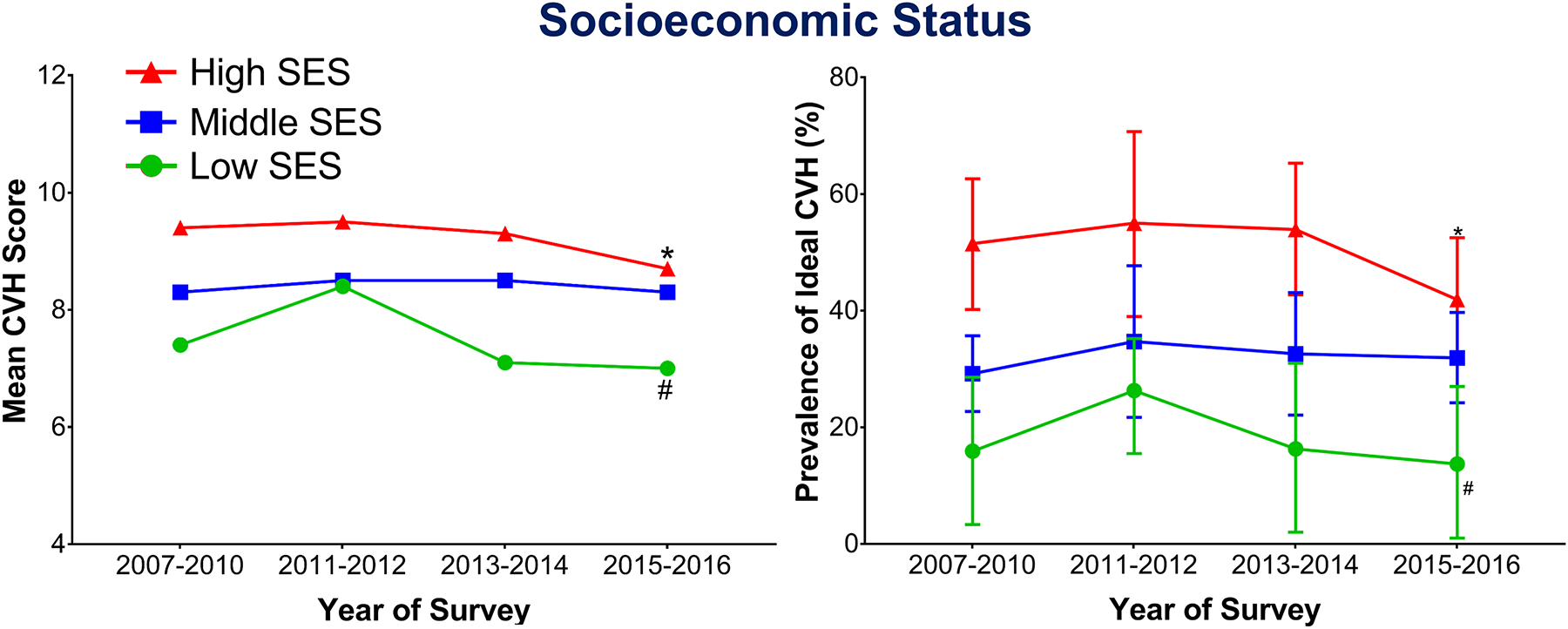
The trends in mean (A) and ideal (B) cardiovascular health according to socioeconomic status by National Health and Nutrition Examination Survey cycle. (A) The symbols indicate covariate adjusted mean cardiovascular health. The red triangle with redline represents trends of mean cardiovascular health in participants from high socioeconomic strata (Plinear =0.007). The blue square with the blue line represents trends of mean cardiovascular health in participants from middle socioeconomic strata (Plinear and Pquadratic >0.05). The green circle with the green line represents trends of mean cardiovascular health in participants from low socioeconomic strata (Pquadratic =0.007). Values were estimated from multivariable linear regression analysis including age, sex, race, insurance status, and number of health care visits. Trend P values were estimated from multivariable logistic regression analysis including age, sex, race, insurance status, number of health care visits, and Bonferroni correction for multiple testing. * denotes trend P value of 0.007; # denotes trend P value of 0.007. (B) The symbols indicate covariate adjusted percentage prevalence with 95% confidence interval (error bars). The red triangle with redline represents trends of ideal cardiovascular health in participants from high socioeconomic strata (Pquadratic =0.01). The blue square with the blue line represents trends of ideal cardiovascular health in participants from middle socioeconomic strata (Plinear and Pquadratic>0.05). The green circle with the green line represents trends of ideal cardiovascular health in participants from low-socioeconomic strata (Pquadratic =0.02). Values were estimated from multivariable linear regression analysis including age, sex, race, insurance status, and number of health care visits. Trend P values were estimated from multivariable logistic regression analysis including age, sex, race, insurance status, number of health care visits, and Bonferroni correction for multiple testing. * denotes trend P value of 0.01; # denotes trend P value of 0.02.
Cardiovascular Health Stratified by Socioeconomic Status: High Socioeconomic Status
In the highest socioeconomic stratum, the prevalence of participants with a BMI above 30 kg/m2 increased significantly from 30% (95% CI 26%–34%) in 2007–2010 to 42% (95% CI 36%–48%) in 2015–2016 (Plinear =0.003; Table 4). Similarly, the prevalence of participants with a fasting blood glucose above 126 mg/dL significantly increased from 6% (95% CI 5%–8%) in 2007–2010 to 12% (95% CI 8%–16%) in 2015–2016 (Plinear =0.04). The prevalence of participants with ideal physical activity showed a quadratic trend (P = 0.002), decreasing from 55% in 2007–2010 to 46% in 2013–2014 but then increased to 54% in 2015–2016. The prevalence of other ideal cardiovascular health metrics remained unchanged from 2007–2010 to 2015–2016 (Plinear and Pquadratic >0.05).
Table 4.
Age Standardized Weighted Prevalence of Cardiovascular Health Metrics in Higher Socioeconomic US adults-NHANES 2007–2016
| NHANES 2007–2010* | NHANES 2011–2012* | NHANES 2013–2014* | NHANES 2015–2016* | Trend P value† | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cardiovascular Health‡ | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | No. | Prevalence (95% CI) | Linear | Quadratic |
| Smoking | ||||||||||
| Current | 131 | 14 (12–16) | 56 | 9 (7–11) | 48 | 9 (5–13) | 56 | 11 (8–15) | 0.66 | 0.07 |
| Former | 105 | 10 (8–13) | 57 | 11 (8–15) | 59 | 10 (7–13) | 49 | 12 (7–17) | 0.59 | 0.74 |
| Never | 889 | 76 (73–79) | 417 | 80 (75–84) | 485 | 81 (77–86) | 406 | 77 (71–83) | 0.96 | 0.06 |
| Physical Activity None | 187 | 14 (11–17) | 78 | 15 (9–21) | 126 | 20 (17–23) | 99 | 16 (12–20) | 0.22 | 0.007 |
| Intermediate | 326 | 31 (27–35) | 183 | 33 (27–39) | 195 | 33 (29–38) | 149 | 30 (24–36) | 0.72 | 0.27 |
| Ideal | 612 | 55 (52–59) | 269 | 52 (45–58) | 271 | 46 (42–51) | 263 | 54 (50–57) | 0.42 | 0.002 |
| Body Mass Index (kg/m2) | ||||||||||
| ≥30 | 384 | 30 (26–34) | 162 | 29 (22–36) | 177 | 31 (26–35) | 198 | 42 (36–48) | 0.003 | 0.36 |
| 25–29.9 | 400 | 36 (33–39) | 182 | 37 (32 (43) | 214 | 38 (31–44) | 164 | 32 (27–37) | 0.24 | 0.43 |
| <25 | 341 | 34 (29–39) | 186 | 34 (24–43) | 201 | 32 (26–38) | 149 | 26 (20–32) | 0.06 | 0.87 |
| Healthy Diet Score | ||||||||||
| 0–1 components | 799 | 78 (74–82) | 385 | 76 (71–81) | 453 | 79 (75–82) | 369 | 77 (73–81) | 0.72 | 0.68 |
| ≥2 components | 241 | 22 (18–26) | 143 | 24 (18–29) | 138 | 21 (18–25) | 141 | 23 (19–27) | ||
| Total Cholesterol (mg/dL) | ||||||||||
| >240 | 135 | 12 (9–15) | 56 | 12 (9–16) | 75 | 13 (10–16) | 69 | 15 (10–20) | 0.33 | 0.86 |
| 200–239 | 498 | 42 (39–46) | 247 | 45 (39–51) | 254 | 42 (35–50) | 227 | 44 (36–52) | 0.48 | 0.83 |
| <200 | 492 | 45 (41–50) | 227 | 43 (37–48) | 263 | 43 (37–48) | 215 | 41 (35–47) | 0.94 | 0.85 |
| Blood Pressure (mm Hg) | ||||||||||
| ≥140/≥90 | 147 | 10 (8–12) | 68 | 12 (8–16) | 74 | 11 (9–14) | 66 | 13 (8–17) | 0.59 | 0.82 |
| 120–139/80–89 | 422 | 36 (32–40) | 211 | 39 (34–44) | 192 | 32 (28–37) | 211 | 42 (36–47) | 0.95 | 0.06 |
| <120–80 | 556 | 54 (50–58) | 251 | 49 (42–55) | 326 | 56 (51–62) | 234 | 46 (38–53) | 0.75 | 0.12 |
| Fasting Blood Glucose (mg/dL) | ||||||||||
| ≥126 | 101 | 6 (5–8) | 38 | 6 (2–10) | 52 | 7 (5–10) | 70 | 12 (8–16) | 0.04 | 0.85 |
| 100–125 | 484 | 42 (38–45) | 216 | 42 (35–49) | 222 | 35 (31–39) | 228 | 47 (41–53) | 0.96 | 0.001 |
| <100 | 540 | 52 (49–56) | 276 | 52 (45–59) | 318 | 57 (52–63) | 213 | 41 (33–49) | 0.22 | 0.002 |
CI = confidence interval; NHANES = National Health and Nutrition Examination Survey; No. = number.
Direct method for age standardization was performed using the US 2000 census population age-groups 20–29, 30–39, 40–49, 50–59, 60–69, ≥70 years or older.
The orthogonal polynomial model including age groups, race, sex, insurance status, number of health care visits, and Bonferroni correction for multiple testing was used to assess the linear and quadratic trend P value across the survey years.
All the participants 20 years or older with available cardiovascular health metrics were included.
Cardiovascular Health Stratified by Socioeconomic Status: Middle Socioeconomic Status
Among subjects in the middle socioeconomic stratum, the prevalence of fasting blood glucose above 126 mg/dL increased significantly from 8% (95%CI 7%–10%) in 2007–2010 to 12% (95%CI 9%–14%) in 2015–2016 (Plinear =0.008; Supplemental Table 2, Online Appendix A). We observed a quadratic trend (P = 0.02) in the prevalence of participants with total cholesterol >240 mg/dL, decreasing from 14% in 2007–2010 to 11% in 2011–2012 and then remained unchanged to 11% in 2015–2016.
Cardiovascular Health Stratified by Socioeconomic Status: Low Socioeconomic Status
Among participants in the low socioeconomic stratum, the prevalence of participants with an ideal blood pressure (<120/80 mm Hg) decreased significantly from 50% (95% CI 44%–56%) in 2007–2010 to 38% (95% CI 29%–47%) in 2015–2016 (Plinear =0.02; Supplemental Table 3, Online Appendix A). The prevalence of ideal fasting blood glucose less than 100 mg/dL showed a quadratic trend, increasing from 43% in 2007–2010 to 51% in 2013–2014 but then decreasing dramatically to 33% in 2015–2016 (Pquadratic =0.005). Additionally, the prevalence of ideal healthy diet (ie, ≥2 components) declined from 28% in 2007–2010 to 18% in 2013–2014 but then increased to 26% in 2015–2016 (Pquadratic =0.001).
Sensitivity Analysis
Among population in high-income status (ie, poverty income ratio >3.5), there was a stable prevalence of ideal cardiovascular health at ~50% from 2007–2010 to 2013–2014, with a decline in the prevalence to 42% in 2015–2016 (Pquadratic =0.02; Supplemental Figure 2, Online Appendix A). Additionally, the prevalence of ideal cardiovascular health among individuals with ≤12 years of education showed a linear trend (P = 0.01), increasing from 19% in 2007–2010 to 29% in 2015–2016 (Supplemental Figure 3, Online Appendix A). However, we did not observe any trends in the prevalence of ideal cardiovascular health among participants with middle income status (ie, poverty income ratio between 1.50 and 3.49) and some college attainment (Supplemental Figures 2 and 3).
DISCUSSION
In summary, we demonstrated that the ideal cardiovascular health, as measured by the AHA’s Life’s Simple 7 metrics, has continued to decline despite the economic recovery. We noted 25% higher odds of fasting blood glucose ≥126 mg/dL and 15% higher odds of obesity in the postrecession period from 2011–2016 as compared with recession period 2007–2010. The prevalence of the ideal fasting blood glucose metric was noted to decline across all socioeconomic strata, while the prevalence of obesity was noted to increase in the high socioeconomic stratum only. We demonstrated that the adverse cardiovascular health effects were present across all socioeconomic strata of US adults. Finally, we also demonstrated that the economic fluctuations had a greater impact on the participants in high and low socioeconomic stratum.
There are multiple mechanistic explanations for our findings. Economic hardship is a well-described physical, cognitive, psychological, and social stressor.19 Stressful experiences have previously been linked to both adverse behavioral mechanisms and direct pathophysiological mechanisms. The behavioral mechanisms may include maladaptive responses like binge drinking and pathophysiological mechanisms like overactivation of the sympathetic nervous system and endocrine dysregulation.20 These pathways have multiplicative effects that may lead to cardiovascular diseases. This complex pathophysiology may even begin in newborns.21 There are other important practical considerations. Unemployment rose to unprecedented levels in the United States during the economic recession. This was coupled with a 25% rise in adults that had incomes below 200% of the federal poverty levels.22 This unemployment likely contributed to an additional 5 million Americans being without health insurance, leading to a total of 50 million uninsured Americans. This was in the context of already declining health insurance coverage rates between the years 2000 and 2007.22 This economic difficulty may also partially explain the rising prevalence of obesity and diabetes over the course of the study periods via an inability to secure key medication and preventive strategies. Obesity and diabetes mellitus can be resource-intensive chronic diseases.23 The cornerstones of management include nutritious food intake, regular exercise, and for diabetes mellitus, access to hypoglycemic medications. There is clear evidence that all of these management strategies, particularly access to medications, are grossly disrupted in financial hardship.24
Our investigation adds to the existing literature base on cardiovascular health outcomes related to the economic recession. The results of longitudinal cohort from the Multi-Ethnic Study of Atherosclerosis showed a significant increase in blood pressure and fasting blood glucose among US adults posteconomic recession.3 Furthermore, younger adults, highly educated individuals, and home owners were more likely to have the deleterious effect of economic recession on blood pressure and fasting blood glucose than their counterparts.3 To the best of our knowledge, our investigation is the first to study the aggregate effect of multiple cardiovascular behaviors and risk factors after the economic depression. This offers a more nuanced view of which ill cardiovascular health effects have recovered after the economic recession. Data from Centers for Disease Control and Prevention (CDC) showed a steady decline in rates of all cardiovascular disease, heart disease, and stroke mortality between 2000 and 2011.25 However, the decline in mortality rates among all three categories slowed substantially after 2011.25 Hence, the decline in ideal cardiovascular health that we demonstrated may itself provide the mechanistic explanation for the slowed decline of cardiovascular mortality rates that have been previously described in the period after the economic depression. Study assessing data from the World Health Organization (WHO) on 26 European Union countries had previously demonstrated that a 1% rise in unemployment rates led to an increase in age-specific cardiovascular mortality among males between the years 1980 and 2007.26 Our investigation also provides a mechanistic explanation for this data. Lastly, the economic recession has also impacted the cardiovascular health in other countries, such as the United Kingdom.27 The data including 1.36 million survey responses ages 16201364 years from the Quarterly Labour Force Survey of the United Kingdom showed a ~3% rise in unemployment during the economic recession. Following the economic recession, nearly 1% increase in poor cardiovascular health was reported, despite the presence of a robustly funded public health system in the United Kingdom.27 Our results suggest that the effect may be even more dramatic in the US population.
Our study also holds public health importance. The increasing prevalence of poorly controlled fasting blood glucose especially in high socioeconomic strata is particularly disconcerting. A major increase (~12%) in the prevalence of obesity among participants from high socioeconomic strata might explain the aforementioned observation. The 2010 Global Burden of Disease report noted a rapidly rising worldwide disability-adjusted life year burden conferred by obesity and diabetes mellitus.28 Other important cardiovascular risk factors were also noted to having a rising burden between 1990 and 2010. These concepts were likely synergistic in the emergence of ischemic heart disease and stroke as the pathologies that accounted for 2 of the highest burdens of disability life-adjusted years worldwide after the economic recession.28 Needless to say, the rising prevalence of diabetes mellitus also confers a significant cost for the health system overall. The estimated cost of diabetes treatment is already thought to be well more than US$100 billion yearly based on cost-of-illness studies.29 Moreover, the lack of improvement or widening in preexisting cardiovascular health disparities and inequities as a result of the economic recession was of great concern to us. For example, we noted in our study population that participants in the lowest socioeconomic stratum had the greatest prevalence of elevated fasting blood glucose levels (~15%). Copeland et al also described that health outcomes worsened disproportionately among English women with the lowest levels of educational attainment in the period after the economic recession.30 Finally, we note that the economic recession and decline in ideal cardiovascular health measures coincided with a reduction in health care spending by the US government.31 This is of particular concern to us as cuts in health care funding in an era when ideal cardiovascular health is quantifiably worsening may yield a potential endless loop of negative health outcomes.
The decline in ideal cardiovascular health may be addressed by intervention targeting the modifiable factors such as healthy diet components and ideal physical activity levels. These are relevant to subjects of all socioeconomic strata. Ideal diet, particularly among individuals of low socioeconomic status, may be addressed via reduction of food insecurity. Food insecurity is a term that refers to the inability to afford nutritious food to sustain a healthy lifestyle.32 Food insecurity has been associated with a higher prevalence of diabetes mellitus and worsened metabolic control in prior NHANES surveys.32,33 Food insecurity may addressed via the reduction of food desserts in lower socioeconomic status neighborhoods,34 encouraging individuals to participate in underused food-assistance programs,35 and avoiding budget cuts to federal food assistance programs such as the Supplemental Nutrition Assistance Program.36 The 2018 Physical Activity Guidelines also outlined numerous useful strategies for increasing the uptake of physical activity among Americans—professional- and peer-guided groups; community-wide campaigns; and mindful community design to encourage physical activity.37
We acknowledge that our investigation has numerous limitations. Causality cannot be established from cross-sectional surveys such as the NHANES data. The cross-sectional nature of NHANES data limits our ability to study measures of disease frequency and intraindividual trends in ideal cardiovascular health over time. Furthermore, residual confounding may have influenced the trends we observed (eg, our analyses does not capture access to medications or ability to pay for medications). Because of the lack of geographic identifiers such as state or county, we cannot assess the regional trends in the prevalence of cardiovascular health from the NHANES data. However, the population-level viewpoint still offers numerous important insights into cardiovascular disease risk factors. As the physical activity questionnaires changed substantially from 2007–2008 onward,17 we are unable to compare the cardiovascular health metrics among participants prior to NHANES 2007–2008 cycle. Cardiovascular diseases such as ischemic heart disease, stroke, and peripheral arterial disease typically have long induction and latency periods. Hence, it is unlikely that we have captured the full extent of the cardiovascular disease burden that resulted from the economic depression. This will require further prospective research.
CONCLUSIONS
Despite economic recovery, we witnessed the rising prevalence of fasting hyperglycemia and obesity and declining prevalence of overall ideal cardiovascular health, especially among high and low socioeconomic strata.
Supplementary Material
CLINICAL SIGNIFICANCE.
Cardiovascular health, as measured by the American Heart Association’s Life’s Simple 7 metrics between economic recession (2007–2010) and economic recovery (2011–2016) was assessed.
From 2007–2010 to 2011–2016, US adults showed a decline in mean cardiovascular health score driven by increasing prevalence of obesity and impaired fasting glucose.
Individuals from high- and low-socioeconomic strata showed decreasing prevalence of ideal cardiovascular health.
Cardiovascular health has continued to decline despite economic recovery.
Funding:
PA is supported by National Institutes of Health Mentored Patient-Oriented Research Award 1K23HL146887-01. NP is supported by National Institutes of Health grant 5T32HL129948-02.
Footnotes
Conflicts of Interest: None of the authors have any conflicts of interest or financial relationship to disclose.
SUPPLEMENTARY DATA
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amjmed.2019.06.004.
References
- 1.Wang H, Wang C, Halliday TJ. Health and health inequality during the great recession: evidence from the PSID. Econ Hum Biol 2018;29:17–30. [DOI] [PubMed] [Google Scholar]
- 2.Jofre-Bonet M, Serra-Sastre V, Vandoros S. The impact of the great recession on health-related risk factors, behaviour and outcomes in England. Soc Sci Med 2018;197:213–25. [DOI] [PubMed] [Google Scholar]
- 3.Seeman T, Thomas D, Merkin SS, et al. The great recession worsened blood pressure and blood glucose levels in American adults. Proc Natl Acad Sci U S A 2018;115:3296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burgard SA, Ailshire JA, Kalousova L. The great recession and health: people, populations, and disparities. Ann Am Acad Pol Soc Sci 2013;650:194–213. [Google Scholar]
- 5.Riumallo-Herl C, Basu S, Stuckler D, et al. Job loss, wealth and depression during the great recession in the USA and Europe. Int J Epidemiol 2014;43:1508–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mishel L, Bivens J, Gould E, et al. The State of Working America. 12 ed Ithaca, NY: Cornell University Press; 2012. [Google Scholar]
- 7.Thomson RM, Niedzwiedz CL, Katikireddi SV. Trends in gender and socioeconomic inequalities in mental health following the great recession and subsequent austerity policies: a repeat cross-sectional analysis of the health surveys for England. BMJ Open 2018;8:e022924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reinhard E, Layte R, McCrory C, et al. The great recession and the health of young children: a fixed-effects analysis in Ireland. Am J Epidemiol 2018;187:1438–48. [DOI] [PubMed] [Google Scholar]
- 9.Miller GE, Chen E, Yu T, et al. Metabolic syndrome risks following the great recession in rural black young adults. J Am Heart Assoc 2017;6 10.1161/JAHA.117.006052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 2017;135:e146–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 12.Ogunmoroti O, Oni E, Michos ED, et al. Life’s Simple 7 and incident heart failure: the multi-ethnic study of atherosclerosis. J Am Heart Assoc 2017;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Folsom AR, Shah AM, Lutsey PL, et al. American Heart Association’s Life’s Simple 7: avoiding heart failure and preserving cardiac structure and function. Am J Med 2015;128:970–976.e972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garg PK, O’Neal WT, Chen LY, et al. American Heart Association’s Life Simple 7 and Risk of atrial fibrillation in a population without known cardiovascular disease: the ARIC (Atherosclerosis Risk in Communities) Study. J Am Heart Assoc 2018;7:e008424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mok Y, Sang Y, Ballew SH, et al. American Heart Association’s Life’s Simple 7 at middle age and prognosis after myocardial infarction in later life. J Am Heart Assoc 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zipf G, Chiappa M, Porter KS, et al. National health and nutrition examination survey: plan and operations, 1999–2010. Vital Health Stat 2013;1(56):1–37. [PubMed] [Google Scholar]
- 17.Scholes S, Bann D. Education-related disparities in reported physical activity during leisure-time, active transportation, and work among US adults: repeated cross-sectional analysis from the National Health and Nutrition Examination Surveys, 2007 to 2016. BMC Public Health 2018;18:926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang DD, Leung CW, Li Y, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med 2014;174:1587–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynch JW, Kaplan GA, Shema SJ. Cumulative Impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med 1997;337:1889–95. [DOI] [PubMed] [Google Scholar]
- 20.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999;99:2192–217. [DOI] [PubMed] [Google Scholar]
- 21.van den Berg GJ, Doblhammer-Reiter G, Christensen K. Being born under adverse economic conditions leads to a higher cardiovascular mortality rate later in life: evidence based on individuals born at different stages of the business cycle. Demography 2011;48:507–30. [DOI] [PubMed] [Google Scholar]
- 22.Holahan J. The 2007–09 recession and health insurance coverage. Health Aff 2011;30:145–52. [DOI] [PubMed] [Google Scholar]
- 23.Zhuo X, Zhang P, Barker L, et al. The lifetime cost of diabetes and its implications for diabetes prevention. Diabetes Care 2014;37:2557–64. [DOI] [PubMed] [Google Scholar]
- 24.Campbell DJT, Manns BJ, Hemmelgarn BR, et al. Understanding financial barriers to care in patients with diabetes: an exploratory qualitative study. Diabetes Educ 2016;43:78–86. [DOI] [PubMed] [Google Scholar]
- 25.Sidney S, Quesenberry CP Jr., Jaffe MG, et al. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol 2016;1:594–9. [DOI] [PubMed] [Google Scholar]
- 26.Stuckler D, Basu S, Suhrcke M, et al. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet 2009;374:315–23. [DOI] [PubMed] [Google Scholar]
- 27.Astell-Burt T, Feng X. Health and the 2008 economic recession: evidence from the United Kingdom. PLoS One 2013;8:e56674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med 2013;369:448–57. [DOI] [PubMed] [Google Scholar]
- 29.Ettaro L, Songer TJ, Zhang P, et al. Cost-of-illness studies in diabetes mellitus. PharmacoEconomics 2004;22:149–64. [DOI] [PubMed] [Google Scholar]
- 30.Copeland A, Bambra C, Nylén L, et al. All in it together? the effects of recession on population health and health inequalities in England and Sweden, 1991–2010. Int J Health Serv 2015;45:3–24. [DOI] [PubMed] [Google Scholar]
- 31.Chandra A, Holmes J, Skinner J. Is this time different? the slowdown in health care spending. Brook Pap Econ Act 2013;2013:261–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 2010;140:304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berkowitz SA, Baggett TP, Wexler DJ, et al. Food insecurity and metabolic control among u.s. adults with diabetes. Diabetes Care 2013;36:3093–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker RE, Keane CR, Burke JG. Disparities and Access to healthy food in the United States: a review of food deserts literature. Health Place 2010;16:876–84. [DOI] [PubMed] [Google Scholar]
- 35.Carney M Compounding crises of economic recession and food insecurity: a comparative study of three low-income communities in Santa Barbara County. Agric Hum Values 2012;29:185–201. [Google Scholar]
- 36.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff 2015;34:1830–9. [DOI] [PubMed] [Google Scholar]
- 37.US Dept of Health and Human Services. Physical Activity Guidelines Advisory Committee Scientific Report. Available at https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf. Accessed November 24, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


