Abstract
Background
Many older people live at home, often with complex and chronic health and social care needs. Integrated care programs are increasingly being implemented as a way to better address these needs. To support older people living at home, it is also essential to maintain their safety. Integrated care programs have the potential to address a wide range of risks and problems that could undermine older people’s ability to live independently at home. The aim of this scoping review is to provide insight into how integrated care programs address safety risks faced by older people living at home - an area that is rather underexplored.
Methods
Safety was conceptualised as preventing or reducing the risk of problems, associated with individual functioning and behaviour, social and physical environments, and health and social care management, which could undermine older people’s ability to live independently at home. For this scoping review a systematic literature search was performed to identify papers describing integrated care programs where at least one intervention component addressed safety risks. Data were extracted on the programs’ characteristics, safety risks addressed, and the activities and interventions used to address them.
Results
None of the 11 programs included in this review explicitly mentioned safety in their goals. Nevertheless, following the principles of our conceptual framework, the programs appeared to address risks in multiple domains. Most attention was paid to risks related to older people’s functioning, behaviour, and the health and social care they receive. Risks related to people’s physical and social environments received less attention.
Conclusion
Even though prevention of safety risks is not an explicit goal of integrated care programs, the programs address a wide range of risks on multiple domains. The need to address social and environmental risks is becoming increasingly important given the growing number of people receiving care and support at home. Prioritising a multidimensional approach to safety in integrated care programs could enhance the ability of health and social care systems to support older people to live safely at home.
Keywords: Integrated care, Safety, Risks, Prevention, Elderly, Older people living at home, Primary care, Community care, Scoping review
Introduction
All over the world, countries are facing aging populations. Old age is associated with an increased prevalence of chronic conditions, functional decline and frailty, which often results in chronic and complex health and social care needs [1–3]. As a result, the demand for health and social care services is increasing [4]. In response to the growing pressures on the health and social care systems, older people are being stimulated to live independently at home for as long as possible. The majority of older people do indeed ‘age in place’ [5–7], often with support from a range of formal and informal care providers.
In an effort to better address older people’s chronic health and social care needs, integrated care programs for older people living at home are increasingly being implemented in primary and community care settings [8–11]. Although different definitions and models of integrated care exist [12–14], integrated care is generally characterised as a proactive and person-centred approach to care and support that is seamlessly coordinated across multiple professional disciplines and care interfaces, and responsive to the risks and needs older people may face on various domains of life [10, 11]. Integrated care programs come in many shapes and forms, and can pursue different aims ranging from improving functional outcomes, quality of life, quality of care and efficiency [15]. The organisation of integrated primary and community care in considered an essential step towards supporting older people to live independently at home for as long as possible [16].
In order for older people to successfully age in place, it is also important to maintain their safety. Research on patient safety has traditionally focused on the “prevention of errors and adverse effects associated with health care” ( [17], par. 1). However, older people encounter limitations in multiple domains of life, which could also pose risks to their ability to live safely and independently at home [18–25]. This implies a need to look at older people’s safety at home from a broader perspective. Lau et al. (2007) [23] proposed a model for health-related safety that extends beyond the institutional settings and includes a wide range of risk factors in multiple domains of life. Following the principles of this model, risks relate to older people’s health and functioning (e.g., physical or cognitive decline), their lifestyle and behaviour (e.g., dietary intake, self-care, medication adherence), their social or physical environments (e.g., social isolation, caregiver burden, hazards in the home) and the health and social care they receive (e.g., medication errors, communication failures, fragmentation of care) [18–27]. This wide range of risks could lead to a multitude of problems that challenges people’s ability to live safely at home, and could ultimately result in emergency department visits, (re) hospitalisation, institutionalisation and mortality [23]. It is therefore deemed important to address such risks and focus efforts on preventing problems.
Given its proactive, interdisciplinary and comprehensive character, integrated care may provide opportunities to address this range of risks to older people’s safety at home [28]. However, the extent to which integrated care programs currently do this is unclear. There is limited evidence for the effectiveness of preventative integrated care for older people [8, 29], and integrated care programs throughout Europe have been shown to lack a focus on preventative aspects [30]. This suggests a need to increase our awareness of types of risks that are currently considered in integrated care programs, and the scope of activities and interventions that are employed to tackle these risks. Such insights will help researchers and policy makers to identify knowledge gaps, and promote their understanding of what might additionally be needed to properly support older people to live safely at home [31, 32].
To address this knowledge gap in the literature, this study aims to provide insight into how integrated care programs currently address safety risks for older people living at home. This will be done by reviewing integrated care programs published in the scientific literature, which may have various approaches and aims. We will use the principles of Lau et al.’s broad perspective on safety to examine how these programs address safety risks on multiple domains of people’s lives. This review will answer two questions: 1) which safety risks are addressed in integrated care programs for older people living at home, and 2) which activities and interventions are used to address these risks?
Methods
The research questions in this study can be addressed appropriately by carrying out a scoping review [33]. As such, this paper follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for scoping reviews [34].
Search strategy
We conducted a systematic literature search in the Embase and Medline electronic databases with support from a librarian. We searched for papers that described integrated care programs for older people living at home, and that included intervention components that addressed safety. We limited our search to papers published in English, Dutch and Norwegian given our language abilities as authors; and searched for papers published between January 2007 and February 2018. The search combined terms to identify: 1) the target group (e.g., older people, elderly people, frail, aging, geriatric), 2) the care setting (e.g., living in the community, living at home, community-dwelling, home dwelling, independent living, home care, home nursing), 3) integrated care programs (e.g., integrated care, care coordination, case management, comprehensive care, managed care, interdisciplinary care, person-centred care), and 4) safety (e.g., home care safety, patient safety, preventable harm, risk reduction, prevention of adverse events/death/hospitalisations, prevention of risk/medication error/malnutrition/deterioration/social isolation). The detailed search terms and steps are available in Additional file 1. In addition to searching the electronic databases, we identified other relevant papers through reference tracking and manual searches.
Inclusion criteria and definitions
Studies that met the following criteria were eligible for inclusion:
Population: the program in the study targets older people (≥65 years of age) living at home with multiple health and social care needs.
Setting: the program in the study is delivered in older peoples’ homes or in the primary or community care setting.
Integrated care: the program in the study is an integrated care program. For the purpose of this review, integrated care programs were defined as programs that complied with the following three principles of integrated care drawn from the Chronic Care Model and related models [12, 35–38]: 1) interdisciplinarity, meaning that the program aimed to involve professionals from at least two different health and social care professions, 2) comprehensiveness, that is, the program aimed to focus on participants needs in multiple domains of life (i.e., physical, cognitive, psychological, social and environmental), and 3) person-centeredness, meaning that the program aimed to centre care around older people’s needs and wishes, and/or aimed to actively involve older people in the care process.
Design: the study addressed the evaluation of an integrated care program, meaning that we included studies that published program protocols and descriptions, as well as process and outcome evaluations of programs.
Safety: the program in the study contained explicit intervention components that address older people’s safety at home. For this review, safety was conceptualised as preventing or reducing the risk of problems that could undermine older people’s ability to live independently at home. Following the principles of Lau et al.’s framework for health-related safety [23], risks could be associated with individual functioning and behaviour (e.g., physical or cognitive decline, medication adherence, dietary intake), social and physical environments (e.g., caregiver burden, social isolation, in-home hazards), and health and social care management (e.g., polypharmacy, care transitions, over- or under treatment) [18, 23].
Studies were excluded when: 1) they described programs addressing populations with specific diseases (e.g., patients with diabetes or chronic obstructive pulmonary disorder), 2) they described programs delivered in the hospital or nursing home, or 3) they were not published in peer-reviewed scientific journals.
Study selection
After performing the literature search, two reviewers (ML and EA) independently screened the titles and abstracts of the identified papers to assess their relevance based on the first four criteria. Full text papers were retrieved for the studies that both reviewers considered relevant. The reviewers then assessed the studies for eligibility based on their full text using all five inclusion criteria. Any disagreements between the reviewers were resolved by consulting a third reviewer (SdB) and then reaching a consensus.
Data extraction and analyses
Two reviewers (ML and EA) independently extracted relevant data from the included studies using a predefined template. Data were extracted on the general characteristics of the integrated care program (i.e., country, setting and target group, goals, and how programs address the elements of integrated care), and on the safety-related intervention components of the program (i.e., the risks addressed, and the interventions and activities used to address them). These safety-related components were categorised into five domains of safety risks, which were defined based on the principles of Lau et al.’s framework for health-related safety and additional literature [18–24]. The domains included client functioning, client behaviour, social environment, physical environment, and health and social care management (see Fig. 1; also see inclusion criteria 5). This conceptualisation of safety was used as a ‘new’ lens to look at existing information. Therefore, the extracted safety-related data consisted of both information that was labelled as safety-related in the included studies, as well as information that was interpreted as safety-related by the two reviewers, based on this conceptualisation. Data on the activities and interventions used to address risks were limited to the descriptions and reasoning provided in the included studies. An examination of intervention mechanisms of the identified activities and interventions was beyond the scope of this review. Program components not related to any of the five safety domains were not reported.
Fig. 1.

Domains of safety risks (based on the principles of Lau et al.’s framework for health-related safety and additional literature [18–24]). This figure presents the five domains that were used to categorise the safety risks and interventions identified in the included studies
Results
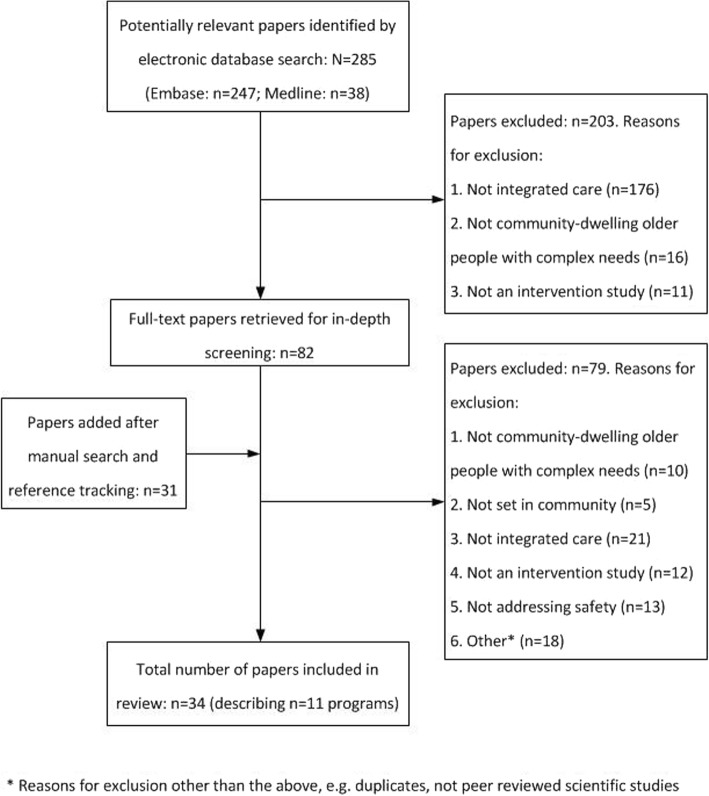
A flowchart of the study selection process is presented in Fig. 2. A total of 285 papers were identified through the systematic search of the electronic databases. After their titles and abstracts were screened, 82 publications were selected for full text screening. An additional 31 papers were selected for full-text screening after reference tracking. Full-text screening resulted in a total of eleven integrated care programs, described across 34 publications, that were included in this review.
Fig. 2.
Flowchart of study selection process. This figure provides an overview of the different steps taken during the study selection process
Characteristics of included programs
The eleven programs included in this review are presented in Tables 1-3. As shown in Table 1, the programs were from the United States (n = 4), the Netherlands (n = 4), Sweden (n = 2) and Switzerland (n = 1). Consistent with our inclusion criteria, included programs targeted people with complex health and social care needs. Some programs explicitly stated that they screened for participants who were cognitively unimpaired (n = 6 programs), or who were at risk of (or experiencing) functional limitations (n = 5). None of the included programs explicitly mentioned safety or improvements in safety as the program’s goal. Generally, programs could be categorised into those that aimed to: 1) prevent or delay functional decline or improve health outcomes (n = 9); 2) reduce service use or costs (n = 6); 3) improve quality of life (n = 4); and 4) improve quality of care (n = 2).
Table 1.
Characteristics of included integrated care programs (abbreviation definitions below)
| Country | Program name | Setting + target group | Goal of program | Elements of integrated care addressed in program | ||
|---|---|---|---|---|---|---|
| Interdisciplinary | Comprehensive | Person-centred | ||||
| United States | ABLE [39, 40] | People aged ≥70 years from an urban community who were cognitively unimpaired and reported some functional difficulties. | Reduce functional difficulties by modifying behavioural and environmental contributors to functional decline. | OT and PT performed home visits and telephone consultations, and together coordinated their activities. | Program targeted participants’ physical functioning, behaviour and physical environment. | Intervention focused on problems identified and prioritised by older people. |
| United States | CAPABLE [41–43] | Low-income people aged ≥65 years from an urban community who were cognitively unimpaired, and who reported some functional difficulties. | Reduce the impact of disability among low income adults by addressing individual abilities and the home environment. | OT and RN performed home visits, and licensed handyman performed home modifications. | Program targeted participants’ physical health and functioning, psychological health, behaviour and physical environment. | Older people were involved in identifying and prioritising problem areas, and developing action plans. |
| United States | Guided Care [44–47] | Older people aged ≥65 years from an urban community who were enrolled in participating primary care practices, and who were at high risk of heavily using health services during the following year. | To first improve patients’ quality of care and physicians’ satisfaction with the quality of care, which would later improve patients’ quality of life and efficiency in the use of resources for older adults with multimorbidity. | RN collaborated with the GP and primary care office staff, and coordinated the activities of all care providers involved. | Program included a CGA of the medical, functional, cognitive, affective, psychosocial, nutritional, and environmental status of older people. | Older people were involved in prioritizing care needs, and care plans were adjusted according to their priorities and preferences. |
| United States | Restorative Home Care [48, 49] | Older people aged ≥65 years who were cognitively unimpaired and at risk for functional decline after acute illness or hospitalization, but who had the potential for maintaining or improving their functioning. | Improve participants’ health outcomes, functional status and service use; and increase their likelihood of remaining at home. | Home care agency reorganized staff into multidisciplinary teams consisting of an RN, OT, PT and HHAs. | Reorientation of home care teams’ focus from primarily treating diseases and “taking care of” patients to that of working together to maximize functioning and comfort. | Goals and the process of reaching them was established based on input from and agreement between the patient, the family and home care staff. |
| The Netherlands | Carewell [50–52] | Frail older people ≥70 years from an urban community who were registered with participating general practices. | Improve quality of life and reduce functional decline, institutionalization, and hospitalization among frail older people living in the community. | Multidisciplinary team consisted of a GP, CCRN, gerontological social worker, elderly care physician, and a pharmacist. CCRN or social worker functioned as case managers. | Program targeted participants’ goals and needs on the domains of health and wellbeing | Case manager supported participants with goal setting and self-management by means of home-visits and telephone contacts. |
| The Netherlands | Embrace [53–55] | People aged ≥75 years from a semi-rural community who were registered with participating general practices. | Support older adults to age in place and improve health outcomes. Also improve quality of care and reduce service use and costs. | Multidisciplinary team consisted of GP, CCRN, social worker and elderly care physician. For complex and frail participants, the nurse or social worker acted as case manager. | Program took into account all aspects of participants’ functioning and disability, along with social and environmental aspects of their lives. | Older people were involved in identifying and prioritizing care needs, and the case manager helped navigate them through the processes of organizing the appropriate care and support. |
| The Netherlands | FIT [56, 57] | People aged ≥70 years at increased risk of functional decline who were registered with participating general practices. | Prevent or delay functional decline and disability. | Intervention was delivered by CCRN and GP. CCRN collaborated with other professionals when necessary. | Program included a CGA that addressed the somatic, psychological, functional and social domains of participants’ lives. | Older people were involved in prioritizing care needs and developing their care plans. |
| The Netherlands | U-Profit [58–60] | Potentially frail people aged ≥60 years who were enrolled in participating general practices. | Improve daily functioning of older people receiving primary care. | Program was delivered by an RN and GP. The RN collaborated with other professionals when necessary. | Program addressed biopsychosocial care needs. | During home visits, the RN focused on participants’ perceived care needs and preferences. |
| Sweden | Elderly Persons in the Risk Zone [61–65] | People aged ≥80 years from an urban community who were cognitively unimpaired and not dependent on help with ADLs. | Delay the progression of frailty in older adults, preserve their health and quality of life, and minimize their need for health care. | Nurse, PT, OT and social worker collaborated to perform preventive home visits or facilitate group meetings for older people. | Preventive home visits and group meetings focused on the physical, psychological, social and environmental domains of participants’ lives. | Participants’ experiences formed the basis of the group meetings; they were the experts, whereas the professionals functioned as enablers. |
| Sweden | Home-based Case Management [66–71] | Older people ≥65 years living in one municipality containing both urban and rural areas, and who were cognitively unimpaired and had at least two ADL dependencies. | Decrease participants’ healthcare use and improve their life satisfaction and other outcomes. | RN delivered case management in collaboration with PT, municipal health and social care services, GPs and the university hospital. | Comprehensive assessment addressed multiple key domains such as function, health, social support, and services. | Older people were consulted regarding the goals and needs that are important to them, and the care activities implemented for them. |
| Switzerland | SpitexPlus [72] | People aged ≥80 years from an urban community who were cognitively unimpaired. | Promote self-care ability and skills for a home-based population aged 80 years and older. | The program was delivered by advance practice nurses who were trained by geriatric specialists. | Program identified health problems as well as social problems. | Program targeted the problems older people chose to focus on. |
Abbreviations: ABLE Advancing Better Living for Elders, OT Occupational Therapist, PT Physical Therapist, CAPABLE Community Aging in Place—Advancing Better Living for Elders, RN Registered Nurse, (I) ADL (Instrumental) Activities of Daily Living, ED Emergency Department, GP General Practitioner, HHA Home Health Aides, CGA Comprehensive Geriatric Assessment, CCRN Community Care Registered Nurse, FIT Functioning in Transition
Table 3.
Activities, interventions and tools used in integrated care programs to address risks on different domains of safety
| ABLE | CAPABLE | Guided Care | Restorative Home Care | Carewell | Embrace | FIT | U-Profit | Elderly Persons in the Risk Zone | Home-Based Case Management | SpitexPlus | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Activities targeting client functioning | |||||||||||
| Assessment of risks and needs | X | X | X | X | X | X | X | X | X | ||
| Evidence based guidelines and protocols to address risks and needs | X | X | X | X | X | X | X | ||||
| Proactive risk management | X | X | X | X | X | X | |||||
| Activities targeting client behaviour | |||||||||||
| Training in disease and symptom management | X | X | X | ||||||||
| Training in medication management | X | X | |||||||||
| Training in functional performance | X | X | X | X | |||||||
| Education about potential problems and risks | X | X | X | X | X | X | |||||
| Counselling in how to cope with problems and risks | X | X | X | X | X | ||||||
| Activities targeting the social environment | |||||||||||
| Education and counselling for caregivers | X | X | |||||||||
| Access to community resources | X | X | X | ||||||||
| Activities targeting the physical environment | |||||||||||
| Aids and assistive devices | X | X | X | ||||||||
| Adjustments and repairs in the home | X | X | X | X | |||||||
| Activities targeting health and social care management | |||||||||||
| Medication reviews | X | X | X | X | |||||||
| Coordination activities within care teams | X | X | X | X | X | ||||||
| Case management during care transitions | X | X | X | X | X | ||||||
| Training on specific aspects of safety | X | X | X | X | X | X | X | X | |||
Abbreviations: ABLE Advancing Better Living for Elders, CAPABLE Community Aging in Place—Advancing Better Living for Elders, FIT Functioning in Transition
Note: empty cells indicate that this type of activity was not reported in the identified literature as being part of the integrated care program
With regard to the components of integrated care, interdisciplinarity of the programs varied. Programs included staff from two to five different health and/or social care professions. Nurses (n = 10) were the most commonly represented, followed by physicians (n = 6) and physical or occupational therapists (n = 5). Social workers were only included in three programs. As pertains to the principle of comprehensiveness, the included programs paid attention to participants’ needs across multiple domains of life. These included, amongst others, physical health and functioning (n = 11), social needs and well-being (n = 8), psychological and cognitive health (n = 5), and the physical environment (n = 5). All eleven programs observed the principle of person-centeredness by focusing on the problems, needs, or goals identified and/or prioritised by participants. Some programs also involved participants in developing or providing input on their care plans, and on the intervention-related activities (n = 5); and promoted participants’ involvement in managing their care (n = 1) and organising appropriate care and support for themselves (n = 1).
Domains of safety risks addressed in included programs
Table 2 provides an overview of the risks that were addressed on the five different domains of safety risks, namely: client functioning, client behaviour, social environment, physical environment, and health and social care management. We considered a risk to have been addressed in some way or form if it was described in the study. Generally, the safety risks identified in this review were interpreted as safety risks by the reviewers—the risks were not labelled as safety risks in the included studies themselves. Even though the findings show that a variety of safety risks were addressed, overall, we found no clear patterns related to the stated program goals and the safety domains or types of risks they addressed.
Table 2.
Safety risks addressed in integrated care programs for older people living at home
| Client functioning | Client behaviour | Social environment | Physical environment | Health and social care management | |
|---|---|---|---|---|---|
| ABLE | Fall risk | Self-management | Obstacles and hazards in the home | ||
| CAPABLE | Fall risk, functional impairments, depressive symptoms | Self-management | Obstacles and hazards in the home | Polypharmacy, patient-provider communication | |
| Guided Care | Fall risk, functional impairments | Self-management, dietary intake, substance abuse | Caregiver burden, elder abuse | Care continuity and transitions, access to care | |
| Restorative Home Care | Functional impairments | Self-management | Caregiver burden | Obstacles and hazards in the home | Polypharmacy, care continuity and transitions |
| Carewell | Fall risk, functional impairments, cognitive impairments, depressive symptoms | Dietary intake | Polypharmacy, care continuity and transitions, over- and under treatment | ||
| Embrace | Functional impairments | Self-management | Caregiver burden | Polypharmacy | |
| FIT | Fall risk, functional impairments, cognitive impairments, depressive symptoms | Medication management, dietary intake, substance abuse | Social isolation, caregiver burden, elder abuse | Obstacles and hazards in the home | Polypharmacy, care continuity and transitions |
| U-Profit | Fall risk, functional impairments, cognitive impairments, depressive symptoms | Dietary intake | Social isolation, caregiver burden | Polypharmacy | |
| Elderly Persons in the Risk Zone | Fall risk, functional impairments | Self-management, medication management, dietary intake | Social isolation | Obstacles and hazards in the home | |
| Home-Based Case Management | Fall risk, functional impairments | Medication management, dietary intake | Social isolation | Obstacles and hazards in the home | Polypharmacy, care continuity and transitions, access to care |
| SpitexPlus | Functional impairments, cognitive impairment | Dietary intake | Social isolation | Care continuity and transitions |
Abbreviations: ABLE Advancing Better Living for Elders, CAPABLE Community Aging in Place—Advancing Better Living for Elders, FIT Functioning in Transition
Note: empty cells indicate that identified literature provided no indication of risks in these domains being addressed
We found that all eleven programs addressed at least three domains of safety risks; nine programs addressed four out of five domains, and three addressed all five domains of safety risks. All programs addressed risks related to client functioning and client behaviour, whereas risks related to people’s social environment (n = 8) and physical environment (n = 6) were addressed in about two-thirds of the programs. Finally, nine programs addressed risks related to health and social care management. We found the programs to be rather uniform in the types of risks they addressed within each domain. For example, the risks related to client functioning that were addressed generally pertained to either functional impairments, fall risk or both. Cognitive impairments and depressive symptoms were addressed less often. For client behaviour, there was somewhat more variation across the programs in the types of risks addressed. Whereas risks related to self-management and dietary intake were addressed in more than half of the programs, risks related to substance abuse and medication management were addressed in only two and three programs, respectively. Risks related to people’s social environment mainly included social isolation or caregiver burden, and risks related to peoples’ physical environment that were addressed always consisted of obstacles and hazards in the home. Care continuity and transitions, and polypharmacy, were most often addressed in the health and social care management domain, whereas safety aspects such as access to care, patient-provider communication, and over- and under treatment were only targeted sporadically.
Activities and interventions used to address safety risks
Table 3 provides an overview of the activities and interventions used within the eleven programs to address safety risks on different domains. We considered an activity to be a part of the given integrated care program if it was described as so in the study. We note again that safety-related activities and interventions were mainly identified and interpreted as being safety-related activities and interventions by the reviewers because the programs themselves did not label the activities as safety-related. Activities targeting risks related to client functioning were quite uniform across the programs. They included comprehensive assessments of participants’ health risks and needs (n = 9), evidence-based guidelines and protocols for planning for care (n = 7), and proactive monitoring of participants’ functioning on the identified risks and needs (n = 6). Although all programs addressed risks related to client functioning (see also Table 2), for the programs Community Aging in Place—Advancing Better Living for Elders (CAPABLE) and Elderly Persons in the Risk Zone, no activities targeting these risks were described. Similar findings were observed regarding risks related to client behaviour. While all programs addressed risks in this domain, the programs Functioning in Transition (FIT) and U-Profit did not describe any associated activities or interventions. Overall, activities and interventions targeting risks related to client behaviour showed more variation across the programs compared to those targeting risks related to client functioning. Approximately half of the programs (n = 6) included written or verbal education for participants about potential problems and risks, whereas five programs provided participants with counselling on how to cope with behaviour problems and risks. In three cases, counselling was provided by registered nurses who acted as case managers. Furthermore, seven programs provided participants with various forms of training, such as in disease and symptom management (n = 3), functional performance (n = 4) and medication management (n = 2).
Activities targeting risks related to participants’ social environment were less frequently reported across the eleven programs. Of the eight programs that addressed such risks, only four described the associated activities. The programs Guided Care, Elderly Persons in the Risk Zone, and Home-Based Case Management addressed risks such as social isolation and elder abuse by helping people get access to community resources; and Restorative Home Care and Guided Care addressed caregiver burden by training and counselling caregivers. As for risks related to participants’ physical environment, four programs described activities that included the installation of adaptive equipment and/or adjustments and repairs in the home. In the programs Advancing Better Living for Elders (ABLE) and CAPABLE, a handyman was part of the comprehensive intervention; whereas in the programs Home-Based Case Management and Restorative Home Care the home safety activities (e.g., adjustments, repairs) were outsourced. Finally, activities aimed at risks related to health and social care management included, for example, taking action to improve coordination between different professionals. Programs did this by providing case management across care transitions (n = 5) or by implementing shared records or multidisciplinary team meetings (n = 5). Additionally, most programs (n = 8) trained the professionals involved. Training targeted, for example, how to deal with polypharmacy, provide counselling, and comprehensively assess risks and needs. Even so, only four out of seven programs that addressed polypharmacy included an activity related to medication review.
Discussion
This scoping review aimed to provide insight into how integrated care programs for older people living at home address a broad range of safety risks. After examining the programs according to a predefined conceptual framework, our findings suggest that all included programs addressed risks related to client functioning and behaviour, and several programs addressed risks related to health and social care management. Fewer programs addressed risks related to people’s social and physical environments as evidenced by program activities and interventions. However, as the number of people receiving care and support at home keeps rising, risks related to, for example, people’s socio-economic conditions, their home environments, and increasing caregiver responsibilities, are becoming more prominent [24]. Addressing such risks is especially important since older people themselves also express that such concerns influence their ability to age in place [20, 25].
Our findings show that integrated care programs vary in the extent to which they addressed safety risks in a multidimensional way. Programs were quite heterogeneous in terms of their activities and interventions for addressing safety risks, but overall, the activities and interventions fell into two broad categories. Some activities and interventions were relevant for preventing harm that may arise from health care interventions, for example, through the organisation of medication reviews or training for professionals. Other activities were pertinent for improving safety by preventing (unnecessary) health decline and supporting people to manage risks in their daily lives. While both types of interventions are necessary in order to address safety, we found that few programs were as comprehensive as to include activities and interventions targeted at all domains of safety risks. Incorporating additional interventions targeting specific risks such as social isolation [73], caregiver burden [74] or environmental hazards [75] might improve the programs’ ability to support older people to live safely at home.
Methodological considerations
Scoping reviews differ from systematic reviews in that they are used to answer questions related to the identification and mapping of certain characteristics or concepts, rather than answering a strictly defined clinical question. Nevertheless, the systematic approach to executing the research and reporting the study results is similar between the two types of reviews [33]. However, this review has some methodological limitations that should be considered when interpreting the findings. Although we performed a broad literature search to identify as many relevant papers as possible, our search strategy was constrained to a specific timeframe and three languages. Consequently, we may have missed studies published before 2007 or in languages other than English, Dutch, and Norwegian. Nevertheless, considering that research on both integrated care programs for older people [76, 77] and safety in primary and community care [23, 24, 32] became increasingly prevalent from 2007 onwards, we expected to find most of the relevant papers within this review’s timeframe.
We acknowledge the limitation that the selection process depended on relevant information being reported in the identified publications. Since we searched for content rather than outcomes of integrated care programs, we purposefully included program protocols and descriptions, as well as process evaluations, in addition to outcome evaluations. Still, several integrated care programs were excluded because information on one or more of the selection criteria was not available in the papers written about the programs. This was especially the case for the criteria of person-centeredness and safety. Given that space in scientific publications is often limited, we cannot rule out the possibility that some excluded programs did in fact address but did not report the inclusion criteria in question. Furthermore, both ‘safety’ and ‘integrated care’ are elastic concepts that can be conceptualised and defined in different ways. Variations in definitions may result in slightly different subsets of the literature being included for review.
When interpreting the findings of this review, it is important to realise that the programs we identified did not necessarily aim to address older people’s safety at home. We used a predefined conceptual framework, based on Lau et al.’s framework for health-related safety and other literature, to review how existing integrated care programs addressed the safety of older people living at home. This approach enabled us to look at existing data from a new perspective. Nevertheless, a limitation of our framework is that it only encompasses an objective approach to safety. It brings together all the different risks and problems that could potentially undermine people’s safety at home. However, older people’s feelings about their safety are not included in the framework. There are possibly significant discrepancies between older people’s objective and subjective safety [20, 29, 78]. Based on this review, it is not possible to indicate the extent to which integrated care programs address the subjective safety of older people living at home.
Implications for research and practice
The findings of this review suggest that addressing safety is currently an implicit aspect rather than explicit objective of integrated care programs for older people living at home. This is not necessarily a negative observation, considering that many professional disciplines have their own safety priorities and protocols that they observe. Nevertheless, in light of our reflections on the results of this scoping review, more explicit consideration of safety in the context of integrated care programs for older people living at home could have several advantages. For example, explicit consideration of the multidimensional nature of safety risks might reduce unintentional oversight among professionals delivering primary and community care, and as such increase the chances that risks are comprehensively addressed. Additionally, explicitly addressing safety risks in an interdisciplinary and multidimensional way could enhance professionals’ understanding of how multiple risks are interrelated and accumulate to undermine older people’s safety. Such work would require that an interdisciplinary team of professionals collaborate and look within and beyond their individual areas of expertise to identify and address safety needs and priorities. Multidimensional risk assessments and innovative ways of involving social care and tapping into community resources would broaden the capacity of integrated care programs to promote older people’s safety in an interdisciplinary and comprehensive way.
However, it is important to acknowledge that safety is not the only aspect to consider in primary and community care for older people. While safety is an important precondition for good quality care and support [28], a strong focus on safety may have adverse effects on older people’s quality of life [79]. Safety should not be considered in isolation from other things that older people value, such as autonomy and the ability to live their lives as they wish [20, 79]. As such, many safety risks cannot be addressed independently of older people’s perspectives [80], which implies a need for open communication and trust between professionals and older people. Professionals should strive for a person-centred way of working, creating an environment where both they and the older people they serve can successfully collaborate to identify safety needs and solutions that take into consideration older people’s priorities and what is appropriate and sustainable for them [28].
This scoping review aimed to provide insight into how integrated care programs address safety risks for older people living at home. Assessing the programs’ effects on safety was not within the scope of this review. Even though some studies did include assessments of program effects on specific risks such as physical functioning or fall risk, comprehensive evaluations of programs’ impact on older people’s safety, from a multidimensional perspective, are necessary to gain insight into the programs’ ability to support older people to live independently at home. The complexity of integrated care programs do pose challenges for such evaluations, as programs often vary in terms of the type of program, the frequency and duration of activities implemented, and the dynamic contexts in which they are implemented. Therefore, in addition to the traditional intervention studies, future research might also consider alternative methods for evaluation [28] such as case study designs [81] or realist evaluation approaches [82]. Such designs, which often employ mixed methods, would facilitate investigation of complex phenomena as they occur in everyday contexts, and bring researchers closer to answering questions as to whether integrated care programs improve older people’s safety, and how.
Conclusion
This review showed that integrated care programs included in the study addressed a broad range of safety risks for older people. Most attention was paid to risks related to older people’s functioning, behaviour, and health and social care management. However, risks related to older people’s social and physical environments are becoming increasingly important and need more attention. Prioritising a multidimensional approach to safety in integrated care programs could add value to the ability of primary and community care providers to support older people to live safely at home. Integrated care provides a platform and tools that could be harnessed further to address safety for older people living at home—in a manner that balances safety with other values important to older people, and that compliments and fills the gaps in discipline-specific safety measures and approaches.
Supplementary information
Additional file 1. Detailed search terms and steps. This file presents the search terms used and steps taken during the literature search.
Acknowledgements
This paper was published on behalf of the SUSTAIN consortium. Furthermore, the authors would like to thank librarian Wim ten Have for his support regarding the development and execution of the literature search in different databases.
Abbreviations
- ABLE
Advancing Better Living for Elders
- CAPABLE
Community Aging in Place—Advancing Better Living for Elders
- FIT
Functioning in Transition
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Authors’ contributions
All authors contributed to the study concept and design. ML and EA contributed to study selection, data extraction and analyses, and consulted SdB in case of any disagreement during study selection. ML and EA drafted the manuscript and TH, GN, CB and SdB critically revised the manuscript. All authors read and approved the final version.
Funding
This study was part of the SUSTAIN project which was funded under Horizon 2020 – the Framework Programme for Research and Innovation (2014–2020) from the European Commission under grant agreement No. 634144. The funder had no role in the design of the study, the collection, analysis, and interpretation of data, or preparation of the manuscript. The content of this paper reflects only the authors’ views. The European Union is not liable for any use that may be made of the information contained herein.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12877-020-1482-7.
References
- 1.Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–439. doi: 10.1016/j.arr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Ryan A, Wallace E, O'Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13:168. doi: 10.1186/s12955-015-0355-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375. doi: 10.1016/S0140-6736(19)31786-6. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . World report on ageing and health. Luxembourg: World Health Organisation; 2015. [Google Scholar]
- 5.Eurostat. People in the EU: who are we and how do we live? Luxembourg: European Union; 2015.
- 6.United States Census Bureau . 65+ in the United States: 2010. Washington, DC: U.S. Government Printing Office; 2014. [Google Scholar]
- 7.Canada S. Living arrangements of seniors. Ottawa, ON: Minister of Industry; 2012. [Google Scholar]
- 8.Looman WM, Huijsman R, Fabbricotti IN. The (cost-)effectiveness of preventive, integrated care for community-dwelling frail older people: a systematic review. Health Soc Care Community. 2018. [DOI] [PMC free article] [PubMed]
- 9.Martinez-Gonzalez NA, Berchtold P, Ullman K, Busato A, Egger M. Integrated care programmes for adults with chronic conditions: a meta-review. Int J Qual Health Care. 2014;26(5):561–570. doi: 10.1093/intqhc/mzu071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Bruin SR, Stoop A, Billings J, Leichsenring K, Ruppe G, Tram N, et al. The SUSTAIN project: a European study on improving integrated Care for Older People Living at home. Int J Integr Care. 2018;18(1):6. doi: 10.5334/ijic.3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Framework on integrated, people-centred health services. Report by the Secretariat for the sixty-ninth world health assembly - Provisional agenda item 16.1. 2016. Report No.: A69/39.
- 12.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Jama. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 13.Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care. 2013;13:e010. doi: 10.5334/ijic.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, et al. The expanded chronic care model: an integration of concepts and strategies from population health promotion and the chronic care model. Healthcare Quarterly. 2003;7(1):73–82. doi: 10.12927/hcq.2003.16763. [DOI] [PubMed] [Google Scholar]
- 15.Kodner DL, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications--a discussion paper. Int J Integrated Care. 2002;2:e12–e1e. doi: 10.5334/ijic.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Commissie Toekomst zorg thuiswonende ouderen. Oud en zelfstandig in 2030. Een reisadvies Den Haag; 2020.
- 17.World Health Organization. Patient Safety. Copenhagen: WHO Regional Office for Europe; [Available from: http://www.euro.who.int/en/health-topics/Health-systems/patient-safety/patient-safety.
- 18.Doran DM, Hirdes J, Blais R, Ross Baker G, Pickard J, Jantzi M. The nature of safety problems among Canadian homecare clients: evidence from the RAI-HC reporting system. J Nurs Manag. 2009;17(2):165–174. doi: 10.1111/j.1365-2834.2009.00974.x. [DOI] [PubMed] [Google Scholar]
- 19.Lang A, Edwards N, Fleiszer A. Safety in home care: a broadened perspective of patient safety. Int J Qual Health Care. 2008;20(2):130–135. doi: 10.1093/intqhc/mzm068. [DOI] [PubMed] [Google Scholar]
- 20.Lette M, Stoop A, Lemmens LC, Buist Y, Baan CA, de Bruin SR. Improving early detection initiatives: a qualitative study exploring perspectives of older people and professionals. BMC Geriatr. 2017;17(1):132. doi: 10.1186/s12877-017-0521-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Macdonald M, Lang A, Storch J, Stevenson L, Donaldson S, Barber T, et al. Home care safety markers: a scoping review. Home Health Care Services Quarterly. 2013;32(2):126–148. doi: 10.1080/01621424.2013.783523. [DOI] [PubMed] [Google Scholar]
- 22.Verver D, Merten H, Robben P, Wagner C. Perspectives on the risks for older adults living independently. British J Community Nursing. 2017;22(7):338–345. doi: 10.12968/bjcn.2017.22.7.338. [DOI] [PubMed] [Google Scholar]
- 23.Lau DT, Scandrett KG, Jarzebowski M, Holman K, Emanuel L. Health-related safety: a framework to address barriers to aging in place. Gerontologist. 2007;47(6):830–837. doi: 10.1093/geront/47.6.830. [DOI] [PubMed] [Google Scholar]
- 24.Vincent C, Amalberti R. Safety strategies for Care in the Home. In: Vincent C, Amalberti R, editors. Safer healthcare: strategies for the real world. Cham: Springer International Publishing; 2016. pp. 93–111. [Google Scholar]
- 25.Tong CE, Sims-Gould J, Martin-Matthews A. Types and patterns of safety concerns in home care: client and family caregiver perspectives. Int J Qual Health Care. 2016;28(2):214–220. doi: 10.1093/intqhc/mzw006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooper A, Edwards A, Williams H, Evans HP, Avery A, Hibbert P, et al. Sources of unsafe primary care for older adults: a mixed-methods analysis of patient safety incident reports. Age Ageing. 2017;46(5):833–839. doi: 10.1093/ageing/afx044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desmedt M, Petrovic M, Bergs J, Vandijck D, Vrijhoef H, Hellings J, et al. Seen through the patients' eyes: safety of chronic illness care. Int J Qual Health Care. 2017;29(7):916–921. doi: 10.1093/intqhc/mzx137. [DOI] [PubMed] [Google Scholar]
- 28.Leape L, Berwick D, Clancy C, Conway J, Gluck P, Guest J, et al. Transforming healthcare: a safety imperative. Qual Saf Health Care. 2009;18(6):424–8. [DOI] [PubMed]
- 29.Lette M, Baan CA, van den Berg M, de Bruin SR. Initiatives on early detection and intervention to proactively identify health and social problems in older people: experiences from the Netherlands. BMC Geriatr. 2015;15:143. doi: 10.1186/s12877-015-0131-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stoop A, de Bruin SR, Wistow G, Billings J, Ruppe G, Leichsenring K, et al. Exploring improvement plans of fourteen European integrated care sites for older people with complex needs. Health Policy. 2019;123(12):1135–1154. doi: 10.1016/j.healthpol.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 31.Cooper A, Chuter A. Patient safety research in primary care: where are we now? British J General Pract: the journal of the Royal College of General Practitioners. 2015;65(641):622–623. doi: 10.3399/bjgp15X687709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lang A. There's no place like home: research, practice and policy perspectives regarding safety in homecare. Int J Qual Health Care. 2010;22(2):75–77. doi: 10.1093/intqhc/mzq007. [DOI] [PubMed] [Google Scholar]
- 33.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed]
- 34.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and ExplanationThe PRISMA-ScR statement. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 35.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. Jama. 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 36.Wagner EH, Bennett SM, Austin BT, Greene SM, Schaefer JK, Vonkorff M. Finding Common Ground: Patient-Centeredness and Evidence-Based Chronic Illness Care. J Alternative Complementary Med. 2005;11(supplement 1):s-7–s-15. doi: 10.1089/acm.2005.11.s-7. [DOI] [PubMed] [Google Scholar]
- 37.Boult C, Green AF, Boult LB, Pacala JT, Snyder C, Leff B. Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's "retooling for an aging America" report. J Am Geriatr Soc. 2009;57(12):2328–2337. doi: 10.1111/j.1532-5415.2009.02571.x. [DOI] [PubMed] [Google Scholar]
- 38.Singer SJ, Burgers J, Friedberg M, Rosenthal MB, Leape L, Schneider E. Defining and measuring integrated patient care: promoting the next frontier in health care delivery. Med Care Res Rev. 2011;68(1):112–127. doi: 10.1177/1077558710371485. [DOI] [PubMed] [Google Scholar]
- 39.Gitlin LN, Hauck WW, Dennis MP, Winter L, Hodgson N, Schinfeld S. Long-term effect on mortality of a home intervention that reduces functional difficulties in older adults: results from a randomized trial. J Am Geriatr Soc. 2009;57(3):476–481. doi: 10.1111/j.1532-5415.2008.02147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54(5):809–816. doi: 10.1111/j.1532-5415.2006.00703.x. [DOI] [PubMed] [Google Scholar]
- 41.Szanton SL, Leff B, Wolff JL, Roberts L, Gitlin LN. Home-based care program reduces disability and promotes aging in place. Health Aff (Millwood) 2016;35(9):1558–1563. doi: 10.1377/hlthaff.2016.0140. [DOI] [PubMed] [Google Scholar]
- 42.Szanton SL, Wolff JL, Leff B, Roberts L, Thorpe RJ, Tanner EK, et al. Preliminary data from community aging in place, advancing better living for elders, a patient-directed, team-based intervention to improve physical function and decrease nursing home utilization: the first 100 individuals to complete a Centers for Medicare and Medicaid Services innovation project. J Am Geriatr Soc. 2015;63(2):371–374. doi: 10.1111/jgs.13245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Szanton SL, Wolff JW, Leff B, Thorpe RJ, Tanner EK, Boyd C, et al. CAPABLE trial: a randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: rationale and design. Contemporary Clin Trials. 2014;38(1):102–112. doi: 10.1016/j.cct.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boult C, Reider L, Frey K, Leff B, Boyd CM, Wolff JL, et al. Early effects of "guided care" on the quality of health care for multimorbid older persons: a cluster-randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2008;63(3):321–327. doi: 10.1093/gerona/63.3.321. [DOI] [PubMed] [Google Scholar]
- 45.Boult C, Reider L, Leff B, Frick KD, Boyd CM, Wolff JL, et al. The effect of guided care teams on the use of health services: results from a cluster-randomized controlled trial. Arch Intern Med. 2011;171(5):460–466. doi: 10.1001/archinternmed.2010.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boyd CM, Boult C, Shadmi E, Leff B, Brager R, Dunbar L, et al. Guided care for multimorbid older adults. Gerontologist. 2007;47(5):697–704. doi: 10.1093/geront/47.5.697. [DOI] [PubMed] [Google Scholar]
- 47.Boyd CM, Reider L, Frey K, Scharfstein D, Leff B, Wolff J, et al. The Effects of Guided Care on the Perceived Quality of Health Care for Multi-morbid Older Persons: 18-Month Outcomes from a Cluster-Randomized Controlled Trial. J Gen Intern Med. 2010;25(3):235–42. [DOI] [PMC free article] [PubMed]
- 48.Tinetti ME, Baker D, Gallo WT, Nanda A, Charpentier P, O'Leary J. Evaluation of restorative care vs usual care for older adults receiving an acute episode of home care. Jama. 2002;287(16):2098–2105. doi: 10.1001/jama.287.16.2098. [DOI] [PubMed] [Google Scholar]
- 49.Tinetti ME, Charpentier P, Gottschalk M, Baker DI. Effect of a restorative model of posthospital home care on hospital readmissions. J Am Geriatr Soc. 2012;60(8):1521–1526. doi: 10.1111/j.1532-5415.2012.04060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ruikes FG, Meys AR, van de Wetering G, Akkermans RP, van Gaal BG, Zuidema SU, et al. The CareWell-primary care program: design of a cluster controlled trial and process evaluation of a complex intervention targeting community-dwelling frail elderly. BMC Fam Pract. 2012;13:115. doi: 10.1186/1471-2296-13-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ruikes FGH, Zuidema SU, Akkermans RP, Assendelft WJJ, Schers HJ, Koopmans RTCM. Multicomponent program to reduce functional decline in frail elderly people: a cluster controlled trial. J Am Board Fam Med. 2016;29(2):209–217. doi: 10.3122/jabfm.2016.02.150214. [DOI] [PubMed] [Google Scholar]
- 52.Ruikes FGH, Adang EM, Assendelft WJJ, Schers HJ, Koopmans R, Zuidema SU. Cost-effectiveness of a multicomponent primary care program targeting frail elderly people. BMC Fam Pract. 2018;19(1):62. doi: 10.1186/s12875-018-0735-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Uittenbroek RJ, Kremer HPH, Spoorenberg SLW, Reijneveld SA, Wynia K. Integrated Care for Older Adults Improves Perceived Quality of care: results of a randomized controlled trial of embrace. J Gen Intern Med. 2017;32(5):516–523. doi: 10.1007/s11606-016-3742-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spoorenberg SL, Uittenbroek RJ, Middel B, Kremer BP, Reijneveld SA, Wynia K. Embrace, a model for integrated elderly care: study protocol of a randomized controlled trial on the effectiveness regarding patient outcomes, service use, costs, and quality of care. BMC Geriatr. 2013;13(1):1–11. doi: 10.1186/1471-2318-13-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spoorenberg SLW, Wynia K, Uittenbroek RJ, Kremer HPH, Reijneveld SA. Effects of a population-based, person-centred and integrated care service on health, wellbeing and self-management of community-living older adults: A randomised controlled trial on Embrace. PLoS One. 2018;13(1):e0190751. 10.1371/journal.pone.0190751. [DOI] [PMC free article] [PubMed]
- 56.Suijker JJ, Buurman BM, ter Riet G, van Rijn M, de Haan RJ, de Rooij SE, et al. Comprehensive geriatric assessment, multifactorial interventions and nurse-led care coordination to prevent functional decline in community-dwelling older persons: protocol of a cluster randomized trial. BMC Health Serv Res. 2012;12:85. doi: 10.1186/1472-6963-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Suijker JJ, Van Rijn M, Buurman BM, ter Riet G, Moll van Charante EP, de Rooij SE. Effects of nurse-led multifactorial care to prevent disability in community-living older people: Cluster randomized trial. PLoS One. 2016; 11(7):e0158714. 10.1371/journal.pone.0158714. [DOI] [PMC free article] [PubMed]
- 58.Bleijenberg N, Drubbel I, Schuurmans MJ, Dam HT, Zuithoff NPA, Numans ME, et al. Effectiveness of a proactive primary care program on preserving daily functioning of older people: a cluster randomized controlled trial. J Am Geriatr Soc. 2016;64(9):1779–1788. doi: 10.1111/jgs.14325. [DOI] [PubMed] [Google Scholar]
- 59.Bleijenberg N, Drubbel I, ten Dam VH, Numans ME, Schuurmans MJ, de Wit NJ. Proactive and integrated primary care for frail older people: design and methodological challenges of the Utrecht primary care PROactive frailty intervention trial (U-PROFIT) BMC Geriatr. 2012;12(1):16. doi: 10.1186/1471-2318-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bleijenberg N, ten Dam VH, Drubbel I, Numans ME, de Wit NJ, Schuurmans MJ. Development of a proactive care program (U-CARE) to preserve physical functioning of frail older people in primary care. J Nursing Scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2013;45(3):230–237. doi: 10.1111/jnu.12023. [DOI] [PubMed] [Google Scholar]
- 61.Behm L, Wilhelmson K, Falk K, Eklund K, Zidén L, Dahlin-Ivanoff S. Positive health outcomes following health-promoting and disease-preventive interventions for independent very old persons: long-term results of the three-armed RCT elderly persons in the risk zone. Arch Gerontol Geriatr. 2014;58(3):376–383. doi: 10.1016/j.archger.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 62.Dahlin-Ivanoff S, Gosman--Hedström G, Edberg A-K, Wilhelmson K, Eklund K, Duner A, et al. Elderly persons in the risk zone. Design of a multidimensional, health-promoting, randomised three-armed controlled trial for "prefrail" people of 80+ years living at home. BMC Geriatrics. 2010;10(1):27. doi: 10.1186/1471-2318-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gustafsson S, Eklund K, Wilhelmson K, Edberg A-K, Johansson B, Häggblom Kronlöf G, et al. Long-term outcome for ADL following the health-promoting RCT--elderly persons in the risk zone. The Gerontologist. 2012;53(4):654–663. doi: 10.1093/geront/gns121. [DOI] [PubMed] [Google Scholar]
- 64.Gustafsson S, Wilhelmson K, Eklund K, Gosman-Hedström G, Ziden L, Kronlöf GH, et al. Health-Promoting Interventions for Persons Aged 80 and Older Are Successful in the Short Term—Results from the Randomized and Three-Armed Elderly Persons in the Risk Zone Study. J Am Geriatr Soc. 2012;60:447–454. doi: 10.1111/j.1532-5415.2011.03861.x. [DOI] [PubMed] [Google Scholar]
- 65.Ziden L, Häggblom-Kronlöf G, Gustafsson S, Lundin-Olsson L, Dahlin-Ivanoff S. Physical function and fear of falling 2 years after the health-promoting randomized controlled trial: elderly persons in the risk zone. The Gerontologist. 2013;54(3):387–397. doi: 10.1093/geront/gnt078. [DOI] [PubMed] [Google Scholar]
- 66.Granbom M, Kristensson J, Sandberg M. Effects on leisure activities and social participation of a case management intervention for frail older people living at home: a randomised controlled trial. Health Social Care Community. 2017;25(4):1416–1429. doi: 10.1111/hsc.12442. [DOI] [PubMed] [Google Scholar]
- 67.Kristensson J, Ekwall AK, Jakobsson U, Midlov P, Hallberg IR. Case managers for frail older people: a randomised controlled pilot study. Scand J Caring Sci. 2010;24(4):755–763. doi: 10.1111/j.1471-6712.2010.00773.x. [DOI] [PubMed] [Google Scholar]
- 68.Möller UO, Kristensson J, Midlöv P, Ekdahl C, Jakobsson U. Effects of a one-year home-based case management intervention on falls in older people: a randomized controlled trial. J Aging Phys Act. 2014;22(4):457–464. doi: 10.1123/japa.2013-0101. [DOI] [PubMed] [Google Scholar]
- 69.Sandberg M, Jakobsson U, Midlöv P, Kristensson J. Cost-utility analysis of case management for frail older people: effects of a randomised controlled trial. Heal Econ Rev. 2015;5(1):12. doi: 10.1186/s13561-015-0051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sandberg M, Kristensson J, Midlöv P, Jakobsson U. Effects on healthcare utilization of case management for frail older people: a randomized controlled trial (RCT) Arch Gerontol Geriatr. 2015;60(1):71–81. doi: 10.1016/j.archger.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 71.Taube E, Kristensson J, Midlöv P, Jakobsson U. The use of case management for community-dwelling older people: the effects on loneliness, symptoms of depression and life satisfaction in a randomised controlled trial. Scand J Caring Sci. 2018;32(2):889–901. [DOI] [PubMed]
- 72.Imhof L, Naef R, Wallhagen MI, Schwarz J, Mahrer-Imhof R. Effects of an advanced practice nurse in-home health consultation program for community-dwelling persons aged 80 and older. J Am Geriatr Soc. 2012;60(12):2223–2231. doi: 10.1111/jgs.12026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health and Social Care in the Community. 2018;26(2):147–57. [DOI] [PubMed]
- 74.Parker D, Mills S, Abbey J. Effectiveness of interventions that assist caregivers to support people with dementia living in the community: a systematic review. Int J Evid Based Healthc. 2008;6(2):137–172. doi: 10.1111/j.1744-1609.2008.00090.x. [DOI] [PubMed] [Google Scholar]
- 75.Clemson L, Mackenzie L, Ballinger C, Close JCT, Cumming RG. Environmental interventions to prevent falls in community-dwelling older people: a meta-analysis of randomized trials. J Aging Health. 2008;20(8):954–71. [DOI] [PubMed]
- 76.de Bruin SR, Versnel N, Lemmens LC, Molema CC, Schellevis FG, Nijpels G, et al. Comprehensive care programs for patients with multiple chronic conditions: a systematic literature review. Health Policy. 2012;107(2–3):108–145. doi: 10.1016/j.healthpol.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 77.Hopman P, de Bruin SR, Forjaz MJ, Rodriguez-Blazquez C, Tonnara G, Lemmens LC, et al. Effectiveness of comprehensive care programs for patients with multiple chronic conditions or frailty: a systematic literature review. Health Policy. 2016;120(7):818–832. doi: 10.1016/j.healthpol.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 78.De Bruin SR, Stoop A, Baan CA, Nijpels G, Billings J. Sustainable tailored integrated care foro lder people in Europe (SUSTAIN-project): lessons learned from improving integrated care in Europe. Bilthoven, Amsterdam, Canterbury: National Institute for Public Health and the Environment (RIVM), VU University Medical Center (VUmc), University of Kent; 2018.
- 79.The Netherlands Centre for Ethics and Health. Safe care, good care? [in Dutch]. The Hague: The Netherlands Centre for Ethics and Health; 2019.
- 80.Lang A, Macdonald M, Storch J, Elliott K, Stevenson L, Lacroix H, et al. Home care safety perspectives from clients, family members, caregivers and paid providers. Healthc Q. 2009;12:97–101. doi: 10.12927/hcq.2009.20720. [DOI] [PubMed] [Google Scholar]
- 81.Yin RK. Case study research: design and methods. 4th edition ed. Los Angeles, California: SAGE Publications, Inc.; 2009. [Google Scholar]
- 82.Pawson R, Tilley N. An Introduction to Scientific Realist Evaluation. 1997. In: evaluation for the 21st century: a handbook [internet]. Thousand Oaks, California: SAGE Publications, Inc.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Detailed search terms and steps. This file presents the search terms used and steps taken during the literature search.
Data Availability Statement
Not applicable.