Abstract
Importance
Although post-operative hypotony is common, many ophthalmologists argue that ocular hypotony is relatively inconsequential and question its occurrence as a surgical complication. Corneal changes related to ocular hypotony has seldom been described.
Objective
To describe corneal topographical changes and ectasia occur in patients who experienced hypotony after glaucoma filtering procedures.
Design
Prospective case series on adults who presented to the University of Illinois glaucoma service from October 2016 to September 2017 who had undergone glaucoma drainage surgeries with at least 3 months of ocular hypotony.
Setting
Single, referral center.
Participants
Adults who had undergone glaucoma drainage surgeries with at least two separate post-operative intraocular pressure readings of 5 mmHg or less measured by Goldmann applanation tonometry in one or both eyes were included. Patient with less than 3 months of persistent hypotony and/or had undergone previous corneal surgeries, had a history of corneal ectasia prior to glaucoma filtering surgeries, or had a history of uveitis were excluded.
Intervention/Exposures
Slit lamp photography, corneal topography, and anterior segment optical coherence tomography were obtained from all patients at the time of enrollment.
Main Outcomes
The development of irregular astigmatism on topography, corneal ectasia on OCT and changes in best-corrected spectacle visual acuity.
Results
A total of nine eyes of seven patients were included. Significant associations between age, thin central corneal thickness and the development of irregular corneal astigmatism were found (p<0.05). Irregular corneal astigmatism was associated with a decreased best-corrected spectacle visual acuity (p=0.02). We also report a case of bilateral corneal ectasia associated with corneal sutures in the setting of hypotony.
Conclusions and Relevance
We illustrate the development of decreased visual acuity associated with irregular corneal astigmatism and the potential for the development of irreversible corneal thinning as complications of persistent hypotony post glaucoma filtering surgeries.
Introduction
Hypotony is a relatively common complication after glaucoma filtering surgeries. In the tube versus trabeculectomy(TVT) study, five year outcome data showed that persistent hypotony accounted for 13% of treatment failures in the tube group and 31% of failures in the trabeculectomy group.1 Although post-operative hypotony is common, many ophthalmologists argue that ocular hypotony is relatively inconsequential and question its occurrence as a surgical complication. Although various negative sequelae, e.g. maculopathy, may develop in response to hypotony,1,2 corneal changes related to ocular hypotony has seldom been described.
It is known that corneal ectatic diseases, e.g. keratoconus, pellucid marginal degeneration and post-refractive ectasia, are characterized by irregular corneal astigmatism and progressive corneal thinning. Although the exact mechanism of keratoconus is unknown, mechanical pressure exerted by the eyelids may cause temporary changes in the corneal curvature, which may be accentuated by ocular hypotony2,3. Especially in eyes with hypotony, upper eyelid could be observed to linearly deforming the globe with each blink.2,4,5 The occurrence of corneal ectasia and hydrops have been described to occur in the setting of ocular hypotony associated with chronic uveitis.4 Here we present a case series describing the corneal changes in patients who experienced hypotony after glaucoma filtering procedures.
Methods
After obtaining institutional review board approval, a prospective case series was conducted on patients older than 18 year-old who presented to the University of Illinois glaucoma service from October 2016 to September 2017 who had undergone glaucoma drainage surgeries. Patients with at least two separate post-operative intraocular pressure (IOP) readings of 5 mmHg or less measured by Goldmann applanation tonometry in one or both eyes were included. Patient with less than 3 months of persistent hypotony and/or had undergone previous corneal surgeries, had a history of corneal ectasia prior to glaucoma filtering surgeries, or had a history of uveitis were excluded.
Written consent to obtain slit lamp photography (Carl Zeiss, Germany), corneal topography (Atlas, Carl Zeiss, Germany) and anterior segment optical coherence tomography (AS-OCT, Pentacam, Oculus, Germany) were obtained from all patients at the time of enrollment. These topography and AS-OCT images were reviewed by two expert reviewers (TSV, EYT). Placido discs were reviewed to ensure that ocular surface disease did not distort topographical results. Data on preoperative characteristics (demographics, primary diagnosis, indication for surgery, comorbid conditions, baseline exam findings) as well as the intraoperative (device model, complications) and postoperative course (postoperative IOP, complications, treatment) were recorded.
Descriptive analysis was performed using Excel (Microsoft, Redmond, WA) and statistical analysis was performed using StatPlus (StatPlus, Version 6, AnalystSoft Inc., Walnut, CA). Chi-square test was used to analyze categorical data. Student’s t-test was used to analyze visual acuity data. Statistical significance was set at p < 0.05.
Results
A total of nine eyes of seven patients were included in the case series. Seven of the eyes had a diagnosis of advanced primary open angle glaucoma(POAG); one neovascular glaucoma; one pigmentary glaucoma. Of the nine eyes, six eyes had undergone trabeculectomy with mitomycin C; two eyes had undergone trabeculectomy with 5-fluorouracil; one eye had undergone Ahmed glaucoma valve implantation.
Table 1 demonstrates the association of irregular corneal astigmatism with age, co-existing diabetes, sex, pre-operative central corneal thickness, preoperative LogMar visual acuity and duration of hypotony. A significant association between age and irregular corneal astigmatism were found (p=0.0007). All patients over 80-year-old with hypotony had irregular corneal astigmatism. The existence of irregular corneal astigmatism was also associated with thinner pre-operative central corneal thickness (CCT) (p=0.03). A statistically significant difference in best-corrected spectacle pre-operative and post-operative visual acuity was found in patients who developed irregular astigmatism in the setting of ocular hypotony (mean pre-operative logMAR visual acuity of 0.53 vs. mean visual acuity with development of astigmatism of 0.90, p=0.02). Macular OCT of these patients showed no macular edema.
Table 1.
Table demonstrating the association of irregular corneal astigmatism with age, co-existing diabetes, gender, pre-operative central corneal thickness, preoperative LogMar visual acuity and duration of hypotony. P-values were calculated using chi-square statistics.
| Eye | Irregular Astigmatism | Age | Diabetes | Sex | Preoperative Central cornea thickness (microns) | Preoperative LogMAR VA | Duration of Hypotony (months) |
|---|---|---|---|---|---|---|---|
| 1 | No | 64 | No | M | 547 | 0.2 | 36 |
| 2 | No | 62 | No | M | 550 | 0.4 | 96 |
| 3 | No | 60 | No | F | 558 | 2.3 | 5 |
| 4 | Yes | 82 | No | M | 492 | 0.1 | 3 |
| 5 | Yes | 82 | No | M | 491 | 0.2 | 4 |
| 6 | Yes | 85 | No | F | 514 | 0.3 | 96 |
| 7 | Yes | 85 | No | F | 519 | 0.4 | 30 |
| 8 | Yes | 82 | Yes | F | 565 | 0.4 | 25 |
| 9 | Yes | 82 | Yes | M | 475 | 1.8 | 60 |
| P-values | - | 0.0007 | 0.17 | 0.63 | 0.03 | 0.56 | 0.73 |
Representative Cases
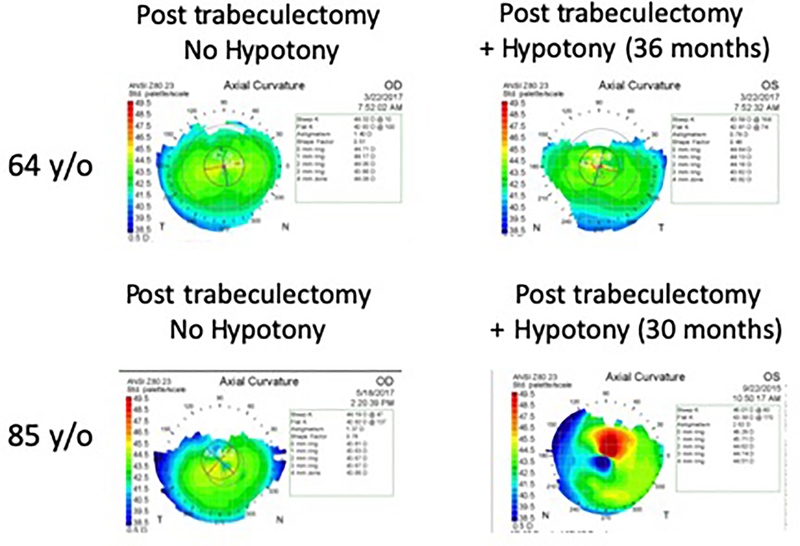
Case 1 and 7
Figure 1 illustrate the right and left eyes of two patients who had undergone trabeculectomy with mitomycin C. In both cases, the left eyes experienced ocular hypotony. Ocular hypotony in the 85-year-old patient led to the development of irregular astigmatism. In contrast, the hypotonous eye from the 64-year-old patient did not develop irregular astigmatism.
Figure 1.
Atlas topography of the right and left eyes of two patients who had undergone trabeculectomy with mitomycin C. In both cases, the left eyes experienced ocular hypotony. Ocular hypotony in the 85-year-old patient led to the development of irregular corneal astigmatism, in contrast the hypotonous eye from the 64-year-old patient did not develop irregular astigmatism.
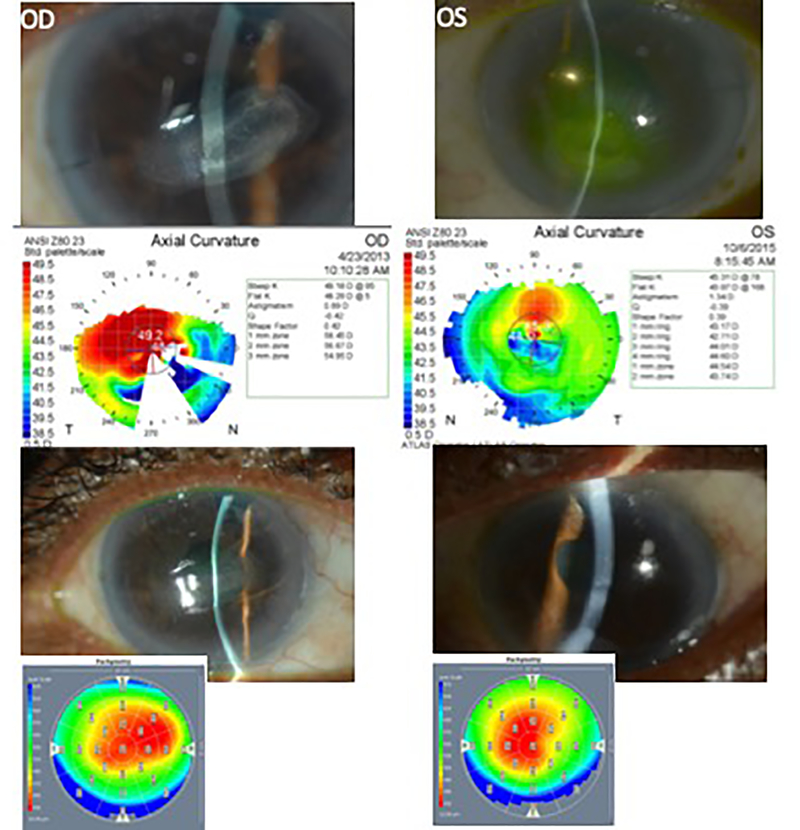
Case 4 and 5
A 82-year-old male, who had undergone trabeculectomy with 5-Fluorouracil OU with post-operative course complicated by hypotony due to over-filtration, underwent cataract surgeries. On postoperative week three through seven, central stromal thinning involving 20% of the corneal stroma in an ellipsoid pattern with the long axis in the direction of the corneal sutures was observed in both eyes (Figure 2a). Corneal topographies OU demonstrated superotemporal steepening (Figure 2b). Corneal sutures were removed and aggressive ocular lubrication was started. Subsequently, central corneal thinning stabilized over the next two months (Figure 3a). AS-OCT demonstrated central areas of corneal thinning OU (Figure 3b).
Figure 2.
A 82-year-old male with advanced primary open angle glaucoma status post trabeculectomy with 5-Fluorouracil OU had undergone cataract surgeries in OD then OS. Post operative course was complicated by hypotony. A) Both eyes developed central stromal thinning in an ellipsoid pattern with the long axis in the direction of the tight corneal sutures. Visual acuities were counting fingers in both eyes. B) Atlas topography demonstrated superotemporal steepening. 2C) Central corneal thinning stabilized over the next two months with visual acuities of 20/30 OD and 20/125 OS. D) Pentacam AS-OCT demonstrated central areas of corneal thinning OU.
Discussion
In this study, we present a case series describing corneal topographical changes in patients with post-filtering surgery hypotony. We found irregular astigmatism in 6 of 9 total eyes with hypotony. All 6 eyes of patients aged 82 to 85 developed irregular corneal astigmatism. In comparison, none of the 3 patients aged 60 to 64 developed irregular astigmatism. We also observed that 5 of 6 eyes with irregular astigmatism had pre-operative CCT less than 520 microns.
Based on our observation, older patients with thin corneas tended to develop irregular astigmatism in the setting of ocular hypotony. We hypothesize that hypotony-related irregular astigmatism may be related to age-related changes in corneal biomechanical properties for several reasons. Firstly, corneal hysteresis, which characterizes an ability to regain the original shape after an applied force, declines with age. Specifically, corneal hysteresis declines with age at a rate of 0.24 to 0.7 mmHg per decade of life.6–8 Secondly, low corneal hysteresis is observed in patients with low CCT and also in ectatic disorders such as keratoconus.9–11 It is possible that older patients with ocular hypotony and thin corneas are prone to develop irregular astigmatism and at risk for corneal ectasia due to low corneal hysteresis.
Persistent hypotony is one of the most frequent complications of glaucoma filtering surgeries. Various changes in the cornea may occur in persistent hypotony, including corneal striate opacities, Bowman’s and Descemet’s folds, and corneal edema. 13 Although post-operative hypotony is common, many ophthalmologists argue that ocular hypotony is relatively inconsequential and question its occurrence as a real complication of surgery. However, our case series demonstrates that irregular astigmatism and consequential changes in best-corrected spectacle visual acuity can develop in ocular hypotony.
We also describe a case of a patient with bilateral corneal thinning from a corneal crease induced from corneal sutures in hypotonous eyes. Notably, central corneal stromal thinning in an ellipsoid pattern with the long axis in the direction of the suture was observed, and corneal curvature was steepened superiorly. The observed corneal thinning in this patient was similar to findings in a case series of corneal ectasia and hydrops in eyes with chronic uveitic hypotony.4 Farooq et. al. described, in eyes with uveitic hypotony, the development of irregular corneal astigmatism and corneal thinning occurring in an arcuate pattern, resembling a “corneal crease” and hypothesized that repeated mechanical stress from blinking in the setting of poor ocular rigidity contributed to a narrow area of corneal flexion and consequent corneal thinning4. In this report, we illustrate the potential for the development of irreversible corneal thinning in the setting of persistent hypotony post glaucoma surgery accentuated by corneal sutures. Recognizing this potential complication and prompt suture removal may prevent permanent visual loss. Similarly, it is plausible that subclinical corneal thinning, corneal ectasia and/or irregular astigmatism could be a cause of unexplained vision loss in hypotonous eyes after glaucoma surgery, therefore evaluation with corneal topography or rigid contact lens overrefraction may be warranted.
Key Points.
Question
What corneal changes occur in patients with ocular hypotony after glaucoma filtering procedures?
Findings
In this prospective case series that included 9 eyes of 7 adults, significant associations between age, pre-operative central corneal thickness and the development of irregular corneal astigmatism were found (p < 0.05). Irregular corneal astigmatism was associated with decreased best-corrected spectacle visual acuity (p=0.02).
Meaning
We illustrate the development of irregular corneal astigmatism and the potential for the development of irreversible corneal thinning as complications of persistent hypotony post glaucoma filtering surgeries.
Bibliography
- 1.Gedde SJ et al. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am. J. Ophthalmol. 153, 804–814.e1 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins MJ et al. Factors influencing lid pressure on the cornea. Eye Contact Lens 32, 168–173 (2006). [DOI] [PubMed] [Google Scholar]
- 3.Sugar J & Macsai MS What causes keratoconus? Cornea 31, 716–719 (2012). [DOI] [PubMed] [Google Scholar]
- 4.Farooq AV et al. Corneal Ectasia and Hydrops in Ocular Hypotony: The Corneal Crease. Cornea 34, 1152–1156 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Buehren T, Collins MJ, Iskander DR, Davis B & Lingelbach B The stability of corneal topography in the post-blink interval. Cornea 20, 826–833 (2001). [DOI] [PubMed] [Google Scholar]
- 6.Kida T, Liu JHK & Weinreb RN Effects of aging on corneal biomechanical properties and their impact on 24-hour measurement of intraocular pressure. Am. J. Ophthalmol. 146, 567–572 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hussnain SA, Alsberge JB, Ehrlich JR, Shimmyo M & Radcliffe NM Change in corneal hysteresis over time in normal, glaucomatous and diabetic eyes. Acta Ophthalmol 93, e627–630 (2015). [DOI] [PubMed] [Google Scholar]
- 8.Kotecha A, Elsheikh A, Roberts CR, Zhu H & Garway-Heath DF Corneal thickness- and age-related biomechanical properties of the cornea measured with the ocular response analyzer. Invest. Ophthalmol. Vis. Sci. 47, 5337–5347 (2006). [DOI] [PubMed] [Google Scholar]
- 9.Kirwan C, O’Malley D & O’Keefe M Corneal hysteresis and corneal resistance factor in keratoectasia: findings using the Reichert ocular response analyzer. Ophthalmologica 222, 334–337 (2008). [DOI] [PubMed] [Google Scholar]
- 10.Saad A, Lteif Y, Azan E & Gatinel D Biomechanical properties of keratoconus suspect eyes. Invest. Ophthalmol. Vis. Sci. 51, 2912–2916 (2010). [DOI] [PubMed] [Google Scholar]
- 11.Mangouritsas G, Morphis G, Mourtzoukos S & Feretis E Association between corneal hysteresis and central corneal thickness in glaucomatous and non-glaucomatous eyes. Acta Ophthalmol 87, 901–905 (2009). [DOI] [PubMed] [Google Scholar]
- 12.Gedde SJ et al. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. Am. J. Ophthalmol. 153, 789–803.e2 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schubert HD Postsurgical hypotony: relationship to fistulization, inflammation, chorioretinal lesions, and the vitreous. Surv Ophthalmol 41, 97–125 (1996). [DOI] [PubMed] [Google Scholar]