Abstract
BACKGROUND AND PURPOSE:
Group B Streptococcus and Escherichia coli (E coli) are the 2 most common causes of bacterial meningitis in neonates. The purpose of this study was to determine whether CSF and/or MR imaging findings differ between infants with group B streptococcal or E coli meningitis.
MATERIALS AND METHODS:
A retrospective review was performed among neonates (younger than 28 days) and infants (younger than 120 days) with proved group B streptococcal (n = 57) or E coli meningitis (n = 50). A CSF or blood culture positive for Streptococcus or E coli and an elevated CSF white blood cell count were used as the criterion standard. Independent, blinded review of brain MRIs obtained within 21 days of presentation were performed by 2 board-certified neuroradiologists. CSF laboratory values and MR imaging findings were compared between the groups.
RESULTS:
There was no statistically significant difference between the mean age at presentation for patients with group B streptococcal (40 days; range, 2–111 days) versus patients with E coli meningitis (31 days; range, 12–115 days) (P = .18). There was no statistically significant difference in the CSF white blood cell count, glucose, or protein. There was a significant difference between group B streptococcal and E coli meningitis in the frequency of hydrocephalus (0% versus 22%, P = .001) and infarct (40% versus 14%; P = .038), respectively. There was no statistically significant difference in leptomeningeal enhancement, cerebritis, ventriculitis, abscess/granuloma, subdural effusion, extra-axial purulent material, intraventricular purulent material, hemorrhage, and sinus thrombosis.
CONCLUSIONS:
Although neonates and infants with group B streptococcal or E coli meningitis had similar age and CSF laboratory values, patients with group B streptococcal meningitis more frequently demonstrated infarcts, while those with E coli meningitis more frequently had early onset of hydrocephalus.
Bacterial meningitis is an inflammation of the meninges affecting the pia, arachnoid, and subarachnoid space in response to bacteria and bacterial products. Despite an array of antibiotics, neonatal meningitis remains a devastating disease. In developed countries, the incidence of culture-proved neonatal meningitis is estimated at 0.3 per 1000 live births.1 In the modern era, the mortality is approximately 10%, and survivors remain at high risk for neurologic sequelae.2,3 In neonates, the most common pathogens are group B Streptococcus (GBS) and Escherichia coli (E coli).2,4,5 Although early-onset GBS meningitis has decreased by two-thirds following the institution of intrapartum antibiotic prophylaxis, late-onset GBS remains a major cause of bacterial meningitis in infants.6
Neonates and infants may present with a wide range of nonspecific clinical symptoms of meningitis, including fever, hypothermia, irritability, poor feeding, bulging fontanelle, and seizure. A lumbar puncture is necessary for definitive diagnosis of bacterial meningitis. Typical CSF findings in bacterial meningitis include elevated white blood cell (WBC) count, predominance of polymorphonuclear leukocytes, reduced glucose levels, and elevated protein levels.7
Neonates with bacterial meningitis will routinely have an MR imaging of the brain to assess complications, which can include abscess, empyema, infarct, and hydrocephalus. Detection of complications from meningitis is necessary in the management of these patients to assess the need for abscess or empyema drainage and ventricular shunting as well as for assessment of parenchymal injury.
A previous report on infants with meningitis indicated a potential trend for different complications depending on the pathogen.8 The purpose of this research was to determine whether CSF and/or MR imaging findings differ between neonates and infants with GBS or E coli meningitis.
Materials and Methods
Following institutional review board approval from Texas Children's Hospital and Indiana University Riley Children's Hospital, a multicenter retrospective review was performed from 2011 to 2018 among neonates (younger than 28 days) and infants (younger than 120 days) with culture-confirmed GBS (n = 57) or E coli meningitis (n = 50). Diagnosis of GBS or E coli meningitis was determined by a CSF culture positive for either Streptococcus or E coli, or a blood culture positive for Streptococcus or E coli combined with an elevated CSF WBC count (>20 WBC/μL for neonates younger than 30 days of age, >9 WBC/μL for 30–90 days of age, and >6 WBC/μL for older than 90 days of age).9
The CSF WBC count per μL, corrected WBC count per μL, red blood cell (RBC) count per μL, glucose (mg/dL), and total protein (mg/dL) obtained within 7 days of presentation were recorded. Corrected WBC count was obtained by dividing the red blood cell count by 500 and subtracting this value from the WBC count. Patients with immunodeficiency, malignancy, or intracranial shunt were excluded. The electronic medical record was reviewed to determine patient age at presentation, duration from presentation to initial CSF obtained by lumbar puncture, duration from presentation to initial MR imaging, prematurity (<37 weeks' gestation), and history of a ventriculoperitoneal shunt procedure.
MR imaging of the brain was performed in all patients on 1.5 T and 3T MR imaging scanners using precontrast axial and sagittal T1-weighted turbo spin-echo, axial FLAIR, axial and coronal T2-weighted, axial gradient-echo, axial diffusion-weighted, and postcontrast axial and coronal T1-weighted turbo spin-echo imaging.
Retrospective independent blinded reviews of brain MRIs were performed within 21 days of presentation by 2 board-certified neuroradiologists (S.F.K., M.K.K.) with 7 and 9 years of experience, respectively, for the presence of the following: leptomeningeal enhancement, cerebritis, ependymal enhancement, hydrocephalus, abscess/granuloma, subdural effusion, infarct, hemorrhage, extra-axial purulent material, intraventricular purulent material, and sinus thrombosis. The neuroradiologist reviewed the MRIs of the brain with the clinical indications of possible meningitis but was blinded to the CSF laboratory results and pathogen diagnosis.
Leptomeningeal enhancement was defined as abnormal contrast enhancement of the leptomeninges on postcontrast T1-weighted imaging. Ependymal enhancement was defined as enhancement of the ependymal surface of the ventricles on postcontrast T1-weighted imaging. Abscess was defined as a peripherally enhancing intraparenchymal lesion on postcontrast T1-weighted imaging with or without associated diffusion restriction. Granuloma was defined as a homogeneously enhancing parenchymal lesion on postcontrast T1-weighted imaging. Cerebritis was defined as superficial brain parenchymal diffusion restriction, enhancement on postcontrast T1-weighted imaging, or T2-weighted/FLAIR hyperintense signal. Infarct was defined as diffusion restriction or T2-weighted hyperintense signal in either a wedge-shaped cortical distribution or a lacunar type distribution. Hemorrhage was defined as abnormal hypointense signal on gradient-echo or T1-weighted hyperintense signal. Subdural effusion was defined as a subdural fluid collection without diffusion restriction or hemorrhage indicated by a lack of susceptibility artifacts or T1-weighted shortening. Extra-axial purulent material was defined as extra-axial (subarachnoid, subdural, or epidural space) diffusion restriction not caused by hemorrhage. Intraventricular purulent material was defined as diffusion restriction within the ventricles not caused by hemorrhage. Sinus thrombosis was defined as abnormal loss of T2-weighted flow void and loss of venous sinus contrast enhancement. Hydrocephalus was defined subjectively as disproportionate enlargement of the ventricles relative to cerebral sulci with reduced subarachnoid spaces in the sulci or cisterns.
Following determination of a statistically significant difference in hydrocephalus between groups, the reviewers subsequently reviewed all sonography, CT, and MRIs of the brain performed in the clinical care of the patients in inpatient and outpatient setttings in all patients to determine the time from presentation to development of hydrocephalus on imaging.
For all patients in whom there was a discordant MR imaging finding, the reviewers performed a combined review and reached a consensus on the MR imaging finding, and this consensus was used as the final diagnosis. Interobserver agreement for individual MR imaging findings was calculated using the κ statistic. A κ value of 0.81–1.0 indicated excellent agreement, 0.61–0.80 indicated good agreement, 0.41–0.60 indicated moderate agreement, 0.21–0.40 indicated fair agreement, and 0–0.20 indicated slight agreement.
A Fisher exact test and an unpaired t test were used when appropriate to compare differences between patients with GBS meningitis and those with E coli meningitis for patient age at presentation, prematurity, duration from presentation to initial CSF collection, duration from presentation to MR imaging, duration from presentation to development of hydrocephalus on imaging, ventriculoperitoneal shunt procedure, CSF laboratory values (corrected WBC count, glucose and protein levels), and MR imaging findings (leptomeningeal enhancement, cerebritis, ependymal enhancement, hydrocephalus, abscess/granuloma, subdural effusion, infarct, hemorrhage, extra-axial purulent material, intraventricular purulent material, and sinus thrombosis). A Bonferroni correction was used to adjust for multiple comparisons for CSF and MR imaging findings between groups (n = 14), and a final P value < .05 was considered statistically significant.
Results
A total of 57 patients with GBS meningitis and 50 with E coli meningitis were included. There was no significant difference for positive CSF culture detection of meningitis for GBS meningitis patients (46/57; 81%) compared to E Coli meningitis patients (35/50; 70%) (P = .26). There was no significant difference in the frequency of positive blood cultures between patients with GBS meningitis (46/57; 81%) and those with E coli meningitis (44/50; 88%) (P = .43).
There was no statistically significant difference between the mean age at presentation for patients with GBS meningitis (40 days; median interquartile range, 38.3 days) versus the mean age for those with E coli meningitis (31 days; median interquartile range, 34.0 days) (P = .18). There was no significant difference in the history of prematurity in patients with GBS meningitis (10/57; 18%) compared with those with E coli meningitis (15/50; 30%) (P = .17).
There was excellent interobserver agreement for all MR imaging findings as follows: leptomeningeal enhancement 0.84 (95% CI, 0.74–0.95); cerebritis 0.87 (95% CI, 0.74–0.99); ependymal enhancement 0.93 (95% CI, 0.83–1.0); hydrocephalus 0.95 (95% CI, 0.84–1.0); abscess 1.0 (95% CI, 1.0–1.0); effusion 0.83 (95% CI, 0.71–0.94); infarct 0.93 (95% CI, 0.84–1.0); hemorrhage 0.92 (95% CI, 0.84–1.0); extra-axial purulent material 0.92 (95% CI, 0.84–1.0); intraventricular purulent material 0.96 (95% CI, 0.89–1.0); and sinus thrombosis 0.93 (95% CI, 0.79–1.0).
Comparison of CSF and MR imaging findings between groups is found in the Table. There was no statistically significant difference between patients with GBS and E coli meningitis in the mean duration from presentation to the date of the initial CSF laboratory study (0.65 versus 1.57 days; P = .06). There was no statistically significant difference in the CSF corrected WBC count and glucose levels or total protein levels between groups.
Comparison of CSF and MRI findings in patients with GBS and E coli meningitisa
| Finding | GBS (n = 57) | E coli (n = 50) | P Valueb |
|---|---|---|---|
| CSF corrected WBC count (cells/μL) | 3116 ± 5058 | 4770 ± 12684 | 1.00 |
| CSF glucose (mg/dL) | 35.2 ± 21.8 | 34.0 ± 24.6 | 1.00 |
| CSF total protein (mg/dL) | 517.8 ± 867.0 | 910.7 ± 1414.2 | 1.00 |
| Leptomeningeal enhancement | 49% | 46% | 1.00 |
| Cerebritis | 21% | 7% | .77 |
| Ependymal enhancement | 7% | 28% | .063 |
| Abscess/granuloma | 2% | 2% | 1.00 |
| Subdural effusion | 49% | 26% | .24 |
| Hemorrhage | 33% | 46% | 1.00 |
| Extra-axial purulent material | 37% | 38% | 1.00 |
| Intraventricular purulent material | 9% | 22% | .84 |
| Sinus thrombosis | 11% | 4% | 1.00 |
| Hydrocephalus | 0% | 22% | .0014 |
| Infarct | 40% | 14% | .038 |
CSF values are listed as mean ± SD.
P value is adjusted for multiple comparisons (n = 14).
There was no statistically significant difference between groups for the duration from presentation to the date of MR imaging (10.1 versus 12.8 days, P = .08). There was a significant difference between GBS and E coli meningitis for acute development of hydrocephalus (0% versus 22%, P = .001). Ultimately, 7% (4/57) of patients with GBS meningitis required ventriculoperitoneal shunting compared with 18% (9/50) of patients with E coli meningitis (P = .14). There was a shorter mean time to development of hydrocephalus among patients with E coli meningitis compared with those with GBS meningitis (18 versus 92 days; P = .006). There was a significant difference between GBS and E coli meningitis for the development of infarct (40% versus 14%; P = .038). There was no statistically significant difference between GBS and E coli groups for leptomeningeal enhancement, cerebritis, ependymal enhancement, abscess/granuloma, subdural effusion, hemorrhage, extra-axial purulent material, intraventricular purulent material restriction, or sinus thrombosis. Representative examples of patients with GBS and E coli meningitis are seen in Figs 1 and 2.
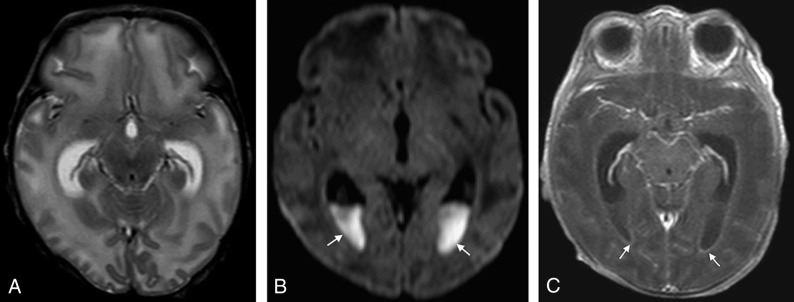
Fig 1.
A 12-day-old neonate with GBS meningitis. Axial DWI demonstrates multifocal areas of diffusion restriction (ADC not shown) in the parenchyma, consistent with infarcts and cerebritis.
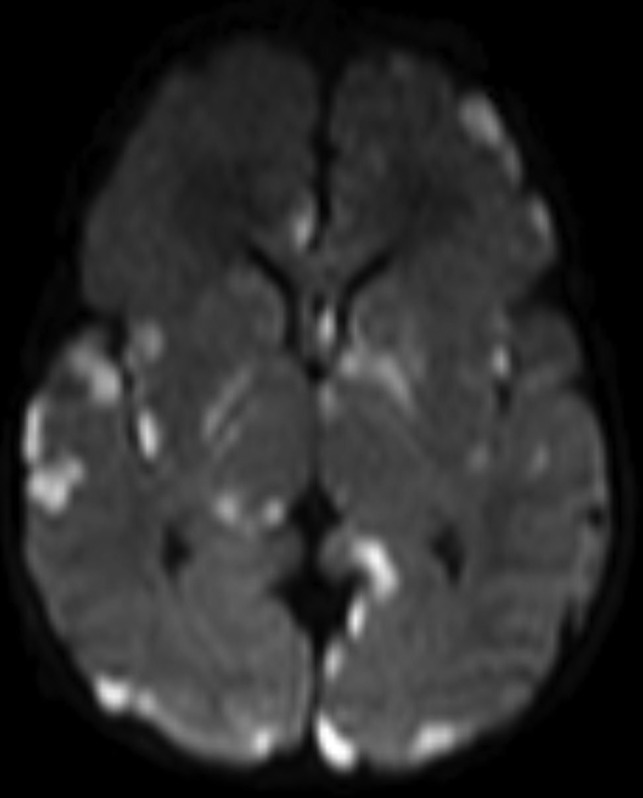
Fig 2.
A 19-day-old neonate with E coli meningitis. A, Axial T2-weighted image demonstrates disproportionate enlargement of the lateral ventricles relative to the sulci, consistent with hydrocephalus. B, Axial DWI demonstrates areas of diffusion restriction (ADC not shown) in the ventricles (arrows), consistent with intraventricular purulent material. C, Axial T1-weighted postcontrast image demonstrates abnormal ependymal enhancement along the lateral ventricles (arrows).
Discussion
The results of this study demonstrate that neonates and infants with GBS meningitis more frequently develop infarcts, while patients with E coli meningitis more frequently develop early onset of hydrocephalus. Some patients with GBS meningitis may ultimately develop hydrocephalus requiring shunting, but there was a shorter duration from presentation to the development of hydrocephalus in patients with E coli meningitis. While CSF remains necessary to obtain a definitive pathogen, no differences in corrected CSF WBC count and protein or glucose levels were detectable between groups. These findings suggest that neurologic complications of meningitis may differ by causative pathogen.
Cerebral infarcts and hydrocephalus are common complications of bacterial meningitis in neonates and infants, found in 28%–43% and 20%–25%, respectively, which is similar to our results.2,5 Despite both of these complications being relatively common, it is interesting that a significant difference in these complications in the acute setting was detected between GBS and E coli meningitis. Our results are similar to those of Jaremko et al,8 who, in a smaller series of neonates and infants with meningitis, compared all streptococcal pathogens with E coli pathogens and found that infarcts were more common with streptococcal pathogens compared with E coli meningitis (59% versus 27%), while hydrocephalus was more common with E coli compared with streptococcal pathogens (64% versus 22%). These results are different from the results of Chang et al,10 who demonstrated no difference in GBS compared with E coli meningitis for the presence of infarcts. This discrepancy may reflect methodologic differences in Chang et al, including a different definition for the diagnosis of bacterial meningitis, a different patient population (Taiwanese), patient collection during a 16-year period, and the use of CT or MR imaging to detect infarcts. The results of our study were obtained during a shorter timeframe and used the gold standard of MR imaging for the diagnosis of infarcts. A longer timeframe in the study of Chang et al may also introduce unknown factors of patient management affecting patient care.
Neonates with bacterial meningitis who develop infarcts have poor outcomes.10,11 Infarcts can occur with other pathogens, particularly Streptococcus pneumoniae so that detection of infarcts on MR imaging is not specific for GBS meningitis.11 The pathogenesis of infarcts from bacterial meningitis is likely related to vasculopathy induced by bacterial products and host inflammatory response.12 Among the bacterial factors, GBS β-hemolysin/cytolysin is directly cytotoxic to the brain endothelium, triggers the endothelium to generate an inflammatory response, and induces macrophage production of inducible nitric oxide synthetase and generation of nitric oxide.13,14 Nitric oxide plays a major role in regulating cerebral blood flow and autoregulation and plays a role in neurotoxicity in the developing brain.15 In addition to infarcts being more frequently identified with GBS compared with E coli, the frequency of cerebritis in patients with GBS meningitis was 3 times greater than in those with E coli meningitis, a finding that could reflect cytotoxicity on a microvascular level. Conversely, E coli is capable of entering the central nervous system through the cerebral vasculature without altering the microvascular endothelium or permeability; this feature may partially explain differences in development of infarcts between GBS and E coli.16
Hydrocephalus may result from purulent exudates in the subarachnoid spaces and/or ependymal surface, resulting in impaired CSF flow or impaired absorption of CSF by the arachnoid villi. Hydrocephalus has been associated with motor disability in neonates with bacterial meningitis.7 In addition to early hydrocephalus being more frequently identified with E coli, our results indicated a 4-fold increase in the frequency of ependymal enhancement and a greater than 2-fold increase in the frequency of intraventricular purulent material with E coli meningitis. These factors may account for the more rapid development of hydrocephalus with E coli compared with GBS. Therefore, differences in the inflammatory response may partially explain the differences in hydrocephalus observed in these patients. These results also provide the clinically important information that patients with GBS meningitis may develop hydrocephalus at a much longer time duration from presentation. Finally, because both infarcts and hydrocephalus can result in injury to the brain parenchyma, these findings are important for patient prognosis and indicate the need for imaging to detect these complications.
Limitations of this study include the retrospective nature of the study and the low number of patients. The small sample size may limit our ability to confirm statistically significant differences in the longer term requirement for intracranial shunt. Although there was greater than twice the frequency of patients with E coli meningitis than with GBS meningitis who ultimately required an intracranial shunt, this determination may require an even larger sample size. Despite the low number of patients, this remains the largest series comparing CSF and MR imaging findings in infants with GBS and E coli meningitis. This study was limited to patients who had MR imaging. At our institution, it has become the standard of care for these patients to undergo MR imaging of the brain, so it is unlikely to result in a selection bias. We acknowledge that CT and sonography can also be used for detection of complications of meningitis such as hydrocephalus, but they are less sensitive and specific for the other findings used in this study.17
Another potential limitation of this study is the subjectivity in the determination of individual MR imaging findings. This subjectivity was mitigated by independent imaging reviews by 2 neuroradiologists, consensus diagnosis in discordant findings, and calculation of interobserver agreement. We observed excellent interobserver agreement for all MR imaging findings. Although there are various ventricular measurements that can be performed to assess hydrocephalus, these are uncommonly required in clinical practice. Lastly, this study used a gold standard diagnosis of meningitis to be either a positive CSF culture or positive blood culture with elevated CSF WBC count. Patients with a positive blood culture and normal CSF WBC count were therefore excluded from this study.
Conclusions
Although infants with GBS and E coli meningitis may have similar ages and CSF laboratory values, MR imaging findings may differ between the groups. Patients with GBS meningitis more frequently demonstrate infarcts, while those with E coli meningitis more frequently have early onset of hydrocephalus. These findings suggest that neurologic complications of meningitis may reflect the specific causative pathogen.
ABBREVIATIONS:
- GBS
group B Streptococcus
- WBC
white blood cell
Footnotes
Disclosures: Nilesh K. Desai—UNRELATED: Expert Testimony: multiple legal firms, Comments: expert review of cases. Jesus G. Vallejo—UNRELATED: Royalties: Wolters Kluwer, Comments: UptoDate chapters.
REFERENCES
- 1. Ku LC, Boggess KA, Cohen-Wolkowiez M. Bacterial meningitis in infants. Clin Perinatol 2015;42:29–45, vii–viii 10.1016/j.clp.2014.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ouchenir L, Renaud C, Khan S, et al. . The epidemiology, management, and outcomes of bacterial meningitis in infants. Pediatrics 2017;140 10.1542/peds.2017-0476 [DOI] [PubMed] [Google Scholar]
- 3. de Louvois J, Halket S, Harvey D. Neonatal meningitis in England and Wales: sequelae at 5 years of age. Eur J Pediatr 2005;164:730–34 10.1007/s00431-005-1747-3 [DOI] [PubMed] [Google Scholar]
- 4. Chávez-Bueno S, McCracken GH. Bacterial meningitis in children. Pediatr Clin North Am 2005;52:795–810, vii 10.1016/j.pcl.2005.02.011 [DOI] [PubMed] [Google Scholar]
- 5. Oliveira CR, Morriss MC, Mistrot JG, et al. . Brain magnetic resonance imaging of infants with bacterial meningitis. J Pediatr 2014;165:134–39 10.1016/j.jpeds.2014.02.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baker CJ, Byington CL, Polin RA; Committee on Infectious Diseases, Committee on Fetus and Newborn. Policy statement: recommendations for the prevention of perinatal group B streptococcal (GBS) disease. Pediatrics 2011;128:611–16 10.1542/peds.2011-1466 [DOI] [PubMed] [Google Scholar]
- 7. Lin WL, Chi H, Huang FY, et al. . Analysis of clinical outcomes in pediatric bacterial meningitis focusing on patients without cerebrospinal fluid pleocytosis. J Microbiol Immunol Infect 2016;49:723–28 10.1016/j.jmii.2014.08.013 [DOI] [PubMed] [Google Scholar]
- 8. Jaremko JL, Moon AS, Kumbla S. Patterns of complications of neonatal and infant meningitis on MRI by organism: a 10-year review. Eur J Radiol 2011;80:821–27 10.1016/j.ejrad.2010.10.017 [DOI] [PubMed] [Google Scholar]
- 9. Kestenbaum LA, Ebberson J, Zorc JJ, et al. . Defining cerebrospinal fluid white blood cell count reference values in neonates and young infants. Pediatrics 2010;125:257–64 10.1542/peds.2009-1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chang CJ, Chang WN, Huang LT, et al. . Cerebral infarction in perinatal and childhood bacterial meningitis. QJM 2003;96:755–62 10.1093/qjmed/hcg128 [DOI] [PubMed] [Google Scholar]
- 11. Katchanov J, Heuschmann PU, Endres M, et al. . Cerebral infarction in bacterial meningitis: predictive factors and outcome. J Neurol 2010;257:716–20 10.1007/s00415-009-5395-9 [DOI] [PubMed] [Google Scholar]
- 12. Iijma S, Shirai M, Ohzeki T. Severe, widespread vasculopathy in late-onset group B streptococcal meningitis. Pediatr Int 2007;49:1000–03 10.1111/j.1442-200X.2007.02474.x [DOI] [PubMed] [Google Scholar]
- 13. Doran KS, Liu GY, Nizet V. Group B streptococcal beta-hemolysin/cytolysin activates neutrophil signaling pathways in brain endothelium and contributes to development of meningitis. J Clin Invest 2003;112:736–44 10.1172/JCI200317335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Doran KS, Nizet V. Molecular pathogenesis of neonatal group B streptococcal infection: no longer in its infancy. Mol Microbiol 2004;54:23–31 10.1111/j.1365-2958.2004.04266.x [DOI] [PubMed] [Google Scholar]
- 15. Garry PS, Ezra M, Rowland MJ, et al. . The role of the nitric oxide pathway in brain injury and its treatment: from bench to bedside. Exp Neurol 2015;263:235–43 10.1016/j.expneurol.2014.10.017 [DOI] [PubMed] [Google Scholar]
- 16. Kim KS. Current concepts on the pathogenesis of Escherichia coli meningitis: implications for therapy and prevention. Curr Opin Infect Dis 2012;25:273–78 10.1097/QCO.0b013e3283521eb0 [DOI] [PubMed] [Google Scholar]
- 17. Littwin B, Pomiećko A, Stępień-Roman M, et al. . Bacterial meningitis in neonates and infants: the sonographic picture. J Ultrason 2018;18:63–70 10.15557/JoU.2018.0010 [DOI] [PMC free article] [PubMed] [Google Scholar]