Abstract
Objective The purpose of the present study was to analyze the structures in the radial tunnel that can cause posterior interosseous nerve entrapment.
Methods A total of 30 members of 15 adult cadavers prepared by intra-arterial injection of a 10% solution of glycerol and formalin were dissected. All were male, belonging to the laboratory of anatomy of this institution.
Results The branch for the supinator muscle originated from the posterior interosseous nerve in all limbs. We identified the Frohse arcade with a well-developed fibrous constitution in 22 of the 30 dissected limbs (73%) and of muscular constitution in 8 (27%). The distal margin of the supinator muscle presented fibrous consistency in 7 of the 30 limbs (23.5%) and muscular appearance in 23 (76.5%). In the proximal margin of the extensor carpi radialis brevis muscle, we identified the fibrous arch in 18 limbs (60%); in 9 (30%) we noticed the arcade of muscular constitution; in 3 (10%) there was only the radial insertion, so that it did not form the arcade.
Conclusion The Frohse arcade and the arcade formed by the origins of the extensor carpi radialis brevis are normal anatomical structures in adult cadavers. However, from the clinical point of view, these structures have the potential to cause entrapment of the posterior interosseous nerve.
Keywords: radial nerve, radial neuropathy, nerve compression syndromes, cadaver
Introduction
The radial nerve (RN) is the main nerve originating from the posterior fascicle of the brachial plexus. It supplies all muscles from the posterior compartment of the arm and forearm. It passes from the posterior to the anterior compartment, contouring the RN sulcus at the humerus. It crosses the intermuscular septum between the brachialis muscle (B) medially, and the brachioradialis (BR) laterally. Traveling distally, it emerges between the BR and extensor carpi radialis longus muscle (ECRL). It is divided in a superficial branch of the RN and the posterior interosseus nerve (PIN), also called deep branch of the RN.
The radial tunnel is a muscle-aponeurotic structure extending from the humeral lateral epicondyle to the distal margin of the supinator muscle (S). 1 2 Compression of the PIN at the radial tunnel may result in two distinctive clinical presentations: PIN syndrome, leading to motor paralysis, and radial tunnel syndrome, which causes sensorial symptoms and pain at the lateral aspect of the elbow and forearm, and is occasionally misdiagnosed as lateral epicondylitis of the elbow. 1
It may seem paradoxical that nerve compression may cause pain as an initial symptom. However, in addition to motor fibers, the PIN presents sensorial afferent fibers to the wrist joint and afferent fibers to the muscles supplied by it. 3 Pain or “weight” sensations may be mediated by these factors. 3 The S muscle consists of two heads, superficial and deep, with the PIN between them. The proximal border of the S superficial head may form a fibrous arcade with variable thickness and length, also known as Frohse arcade (FA). The FA was described in 1908 by Frohse et al, 4 and it is considered the most common site for PIN compression. 2 5 6 Repetitive pronation and supination movements of the forearm may worsen this nerve compression. Other structures may be involved in this condition, such as the fibrous proximal margin of the extensor carpi radialis brevis muscle (ECRB), which has an osseous origin at the radial side and a fascial origin at the ulnar side. These two origins form an arcade, which is crossed by the PIN. This arcade has been involved in PIN compressive syndrome, being proximal or, occasionally, distal to the FA. 1 The present study aimed to identify which structures from the radial tunnel may be responsible for PIN compressive neuropathy.
Material and Methods
The present study was based on the dissection of 30 limbs from 15 cadavers, all male. The limbs were prepared by intra-arterial injection of a 10% glycerin and formalin solution. Four limbs from two full-term fetus cadavers were dissected to evaluate the composition of the S, determining if the fetal arches presented muscular or a partially fibrous composition. These four members were not included in the present study. Each forearm was dissected with the elbow in extension, wrist in neutral position and forearm in pronation. No limb showed evidence of deformities, previous surgical procedures or traumatic injuries in the study area. The skin and fascia from the anterolateral surface of the distal third of the arm, forearm, and wrist were removed.
The RN was identified between the B and BR and dissected from proximal to distal. The BR, ECRL and ECRB tendons were sectioned at their distal third and freed from the fibrous connections joining them to facilitate the identification of nervous branches. The branches to the BR, ECRL, ECRB and S muscles were dissected. Vascular structures were not preserved to facilitate nerve dissection. A 2.5x magnifying glass was occasionally used during dissection. The relation between the PIN and the fibrous tunnel formed by the proximal margin of the ECRB muscle, the FA and the distal S margin was assessed and classified as fibrous or muscular, depending on its appearance, that is, fibrous/tendinous or muscular/translucid, respectively. The present study was approved by the Ethics Committee under number 2.207.258.
Results
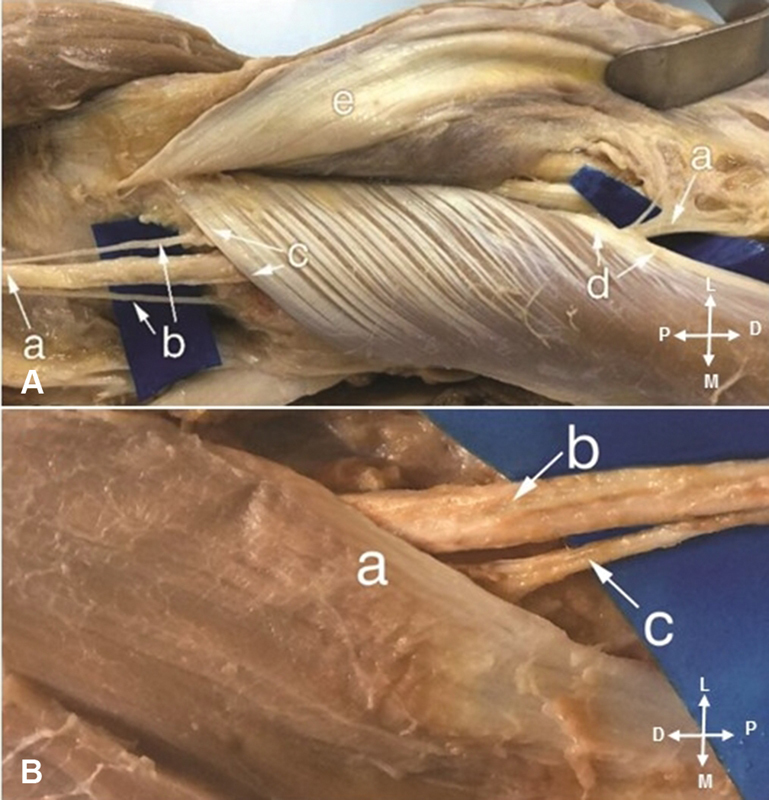
For easier understanding, proximal, distal, medial and lateral aspects are identified in the figures. The FA had a well-developed, fibrous constitution in 22 limbs (73%) ( Fig. 1A and 1B ) and a muscular constitution in 8 limbs (27%) ( Fig. 2A and 2B ). The distal S margin was fibrous in 7 out of 30 limbs (23.5%) ( Fig. 3A ) and had a muscular appearance in the remaining 23 limbs (76.5%) ( Fig. 1B ). The proximal ECRB margin presented an arcade with both bone and fascial origins at the radial and ulnar aspects, respectively; the PIN lied at the tunnel formed by these structures. This arcade was fibrous in 18 limbs (60%) ( Fig. 3B ) and muscular in 9 limbs (30%) ( Fig. 4A ); in addition, in 3 limbs (10%), only the radial attachment was present, with no arcade formation ( Fig. 4B ). The ECRB arcade was proximal to the FA in 17 limbs (57%), in direct contact with the PIN and supported by it ( Fig. 3B and 4A ); however, the arcade had visible macroscopic thickness and structure sufficient to cause PIN compression in only 6 limbs (20%). This arcade was positioned at the same level as the FA in 4 limbs (13.5%) ( Fig. 5A ); in 6 limbs (20%), it was distal to the FA, being supported by the S, not by the PIN ( Fig. 5B ).
Fig. 1.

(A) - (a) Median nerve (MN); (b) branch to brachioradialis muscle (BR); (c) branch to extensor carpi radialis longus muscle (ECRL); (d); branch to extensor carpi radialis brevis muscle (ECRB); (e) superficial branch of the radial nerve (RN); (f) posterior interosseous nerve (PIN). (B) - (a) PIN; (b) branch to supinator (S); (c) fibrous Frohse arcade (FA); (d) distal muscular margin of S.
Fig. 2.

(A) - (a) Median nerve (MN); (b) branch to brachioradialis muscle (BR); (c) branches to extensor carpi radialis longus muscle (ECRL); (d); branch to extensor carpi radialis brevis muscle (ECRB); (e) superficial branch of the radial nerve (RSRN); (f) posterior interosseous nerve (PIN); (g) branches to supinator muscle (S). (B) - (a) MN; (b) branches to BR; (c) branch to ECRL; (d); branch to ECRB; (e) PIN; (f) ECRB; (g) S.
Fig. 3.
(A) - (a) Posterior interosseous nerve (PIN); (b) branches to supinator muscle (S) proximal to the Frohse arcade (FA); (c) fibrous FA; (d) fibrous distal margin of S. (B)- (a) fibrous margin of the extensor carpi radialis brevis muscle (ECRB); (b) PIN; (c) branch to S.
Fig. 4.

(A) - (a) Muscular margin of extensor carpi radialis brevis muscle (ECRB); (b) posterior interosseous nerve (PIN); (c) branch to S. (B) - (a) fibrous Frohse arcade (FA); ECRB (only with bone attachment, no arcade formation); (c) PIN; (d) branch to S muscle; (e) radial nerve superficial branch (RNSB).
Fig. 5.

(A) - (a) Fibrous Frohse arcade (FA) and extensor carpi radialis brevis muscle (ECRB) arcade (sectioned) (b) same level; (c) PIN; (d) branches to supinator muscle (S). (B) - a) median nerve (MN); (b) branch to brachioradialis muscle (BR); (c) branch to extensor carpi radialis longus muscle (ECRL); (d); branch to ECRB; (e) superficial branch of the radial nerve (SBRN); (f) PIN; (g) S. (h) FA proximal to ECRB arcade (i).
Discussion
Kopell et al 7 first described PIN compression at the radial tunnel. Spinner 2 reports studying 25 limbs from adult cadavers and 10 limbs from term fetuses. The lack of a fibrous FA in fetuses, in contrast to the 30% incidence of a fibrous arcade in adult cadavers, suggests that the fibrous arcade component forms at the superficial part of the supinator muscle in response to the repetitive pronation and supination movements of the forearm. 2 We were curious and dissected four fetal forearms and, in fact, no vestigial fibrous tissue was identified in the S. Werner 8 found 39 (65%) fibrous arcades in 60 unselected cadavers and in 80 (89%) out of 90 surgically treated patients. Lister et al 9 identified a thick, fibrous FA in all patients from a 20 surgical cases series, all unilateral. Papadopoulos et al 10 analyzed a series with 120 cadaveric limbs and found a fibrous FA in 61 of them (51%).
Prasartritha et al, 11 dissecting 60 limbs from 30 cadavers, found that the constitution of the FA was membranous in 26 (43%) and fibrotendinous in 34 specimens (57%). Riffaud et al 12 dissected 25 cadaveric limbs and observed that the FA had a fibrous constitution in 23 of them (95%). In an anatomical study on the radial tunnel in 60 cadaveric limbs, Ozkan et al 13 identified a fibrous FA in 48 specimens (80%). Ebrahein et al 14 dissected 20 cadaveric limbs and found a fibrous FA in 14 specimens (70%). Konjengbam et al 15 reported that the FA was fibrous in 40 (87%) out of 46 cadaveric limbs. In the study by Ozturk et al, 6 the FA was tendinous in 48 (87%) cadaveric limbs. Meng et al 16 examined 21 cadaveric limbs, identifying a tendinous arcade in 16 (71%) and a membranous arcade in 5 specimens (29%). Rinker et al 3 reported operating on 79 patients, all presenting fibrous FA. For Clavert et al, 5 the FA had a semicircular shape and tendinous consistency in 26 limbs (87%) and membranous constitution in the remaining 4 specimens (13%). In our study, the FA was fibrous in 22 limbs (73%) and muscular in 8 specimens (27%), with no statistically significant difference between the right and left sides. The number discrepancies can only be explained by the different forms of interpreting the constitution of the FA.
The distal S margin represents the end of the radial tunnel and, in exceptional cases, may be the cause for PIN compression. A distal S margin of fibrous consistency was identified by Konjengbam et al 15 in 30 (65%) out of 46 dissected limbs, and by Riffaud et al 12 in only 3 (7.5%) out of 25 limbs. In our study, the distal S margin had a fibrous constitution in 7 out of 30 limbs (23.5%). As with the FA, these discrepancies can only be explained by the different forms of interpretation. In addition to the AF, other structures can cause nerve compression. Among them, the second most common is the muscular-tendinous arcade formed by both ECRB origins, that is, its osseous origin at the radial aspect and its fascial origin at the ulnar aspect, with the PIN lying between them. This arcade may be proximal or distal to the FA. Riffaud et al. 12 studied 25 cadaveric limbs, and all of them presented an ECRB arcade, always proximal to the FA. Papadopoulos et al, 10 analyzing a series of 120 cadaveric limbs, found a fibrous ECRB arcade in 90% of the specimens. Konjengbam et al 15 identified the tendinous upper medial margin of the ECRB muscle in 36 out of 46 (78%) cadaveric limbs. Clavert et al 5 examined 30 previously prepared cadaveric limbs and found a fibrous component of the ECRB muscle around the PIN in 4 specimens (13%); however, these authors did not register macroscopic evidence of PIN compression by the FA or by any other adjacent structures. Nayak et al 17 reported dissecting 72 cadaveric limbs and found that the ECRB arcade was tendinous in 21 specimens (29,1%), muscular in 8 limbs (11,1%) and absent in 43 specimens (59,7%); in addition, these authors informed that the ECRB arcade involves the PIN and may compress it. Vergara-Amador et al 1 studied 21 cadaveric limbs and identified a fibrotendinous arcade in the upper medial margin of the ECRB muscle in 20 limbs (95.2%). In 14 limbs (71.5%), the arch was positioned proximally to the FA in direct contact with the PIN. In 2 limbs (9.5%), this tendon arcade was found at the same level of the FA, and it was in a distal position, with no direct contact with the PIN, in 4 limbs (19%). Our findings are close to those reported by these authors; we identified that the arcade was fibrous in 18 limbs (60%) and muscular in 9 specimens (30%), in addition to 3 limbs (10%) presenting only a radial attachment that did not form an arcade ( Fig. 4B ). In 17 out of 30 limbs (57%), the ECRB muscle arcade was proximal to the FA, therefore in direct contact with the PIN and supported by it; however, the arcade only had macroscopically-visible thickness and structure and convincing consistency for PIN compression during pronation and supination in 5 specimens (16.5%). The arcade was distal to the FA in six limbs (20%), and, in 4 (13.5%), it was at the same level of the FA, lying over the S, not the PIN ( Fig. 5A ).
We suggest a surgical approach for radial tunnel decompression with the forearm in pronation. The incision is ∼ 10 cm long, starting at the lateral epicondyle and following the radial axis. The forearm fascia is incised and the space between the ECRB and the extensor digitorum (ED) muscles is identified. The dissection is deepened in this space, identifying the FA and the ECRB muscle arcade ( Tables 1 and 2 ).
Table 1. Literature summary on the incidence of the Frohse arcade and supinator distal margin (DM) according to authors.
| Authors | Fibrous FA | Muscular FA | Fibrous DM | Muscular DM | Study type | Number of cases | Year |
|---|---|---|---|---|---|---|---|
| Spinner 2 | 07 (30%) | 18 (70%) | – | – | anatomical | 25 | 1968 |
| Werner 8 | 80 (89%) | 10 (11%) | – | – | surgical | 90 | 1979 |
| Lister et al 9 | 20 (100)% | 0 (0%) | – | – | surgical | 20 | 1979 |
| Papadopoulos et al 10 | 61 (51%) | 59 (49%) | – | – | anatomical | 120 | 1989 |
| Prasartritha et al 11 | 34 (57%) | 26 (43%) | – | – | anatomical | 60 | 1993 |
| Riffaud et al 12 | 23 (95%) | 2 (5%) | 3 (7.5%) | 22 (92.5%) | anatomical | 25 | 1999 |
| Ozcan et al 13 | 48 (80%) | 12 (20%) | – | – | anatomical | 60 | 1999 |
| Ebraheim et al 14 | 14 70% | 6 (30%) | – | – | anatomical | 20 | 2000 |
| Konjengbam et al 15 | 40 (87%) | 6 (13%) | 30 (65%) | 16 (35%) | anatomical | 46 | 2004 |
| Rinker et al 3 | 79 (100%) | 0 (0%) | – | – | surgical | 79 | 2004 |
| Ozturk et al 6 | 48 (87%) | 07 (13%) | – | – | anatomical | 55 | 2005 |
| Clavert et al 5 | 26 (87%) | 34 (57%) | – | – | anatomical | 30 | 2009 |
| Meng et al 16 | 16 (71%) | 05 (29%) | anatomical | 21 | 2015 | ||
| Caetano et al * | 22 (73%) | 08 (17%) | 7 (23.5%) | 23 (76.5%) | anatomical | 30 | 2017 |
Abbreviations: DM, supinator distal margin; FA, Frohse arcade.
Data from this manuscript.
Table 2. Literature summary on the incidence of extensor carpi radialis brevis arcade according to authors.
| Authors | Fibrous ECRB arcade | Muscular ECRB arcade | Absence of ECRB arcade | Study type | Number of cases | Year |
|---|---|---|---|---|---|---|
| Papadopoulos et al 10 | 108 (90%) | 12 (10%) | – | anatomical | 120 | 1989 |
| Konjengbam et al 15 | 36 (78%) | 10 (22%) | – | anatomical | 46 | 2004 |
| Clavert. 5 | 04 (13%) | 26 (87%) | – | anatomical | 30 | 2009 |
| Noyak et al 17 | 21 (29.1%) | 4 (13%) | 43 (59.7%) | anatomical | 72 | 2010 |
| Vergara-Amador et al 1 | 20 (95.2%) | 01 (4.8%) | – | anatomical | 21 | 2015 |
| Caetano et al * | 18 (60%) | 9 (30%) | 3 (10%) | anatomical | 30 | 2018 |
Abbreviation: ECRB, extensor carpi radialis brevis.
Data from this manuscript.
When proximal to the FA, the PIN can be identified through palpation against the radial diaphysis. Both arcades must be decompressed.
Conclusion
The Frohse arcade and the arcade formed by the origins of the ECRB are normal anatomical structures in adult cadavers. It is important to highlight that, clinically, these structures have potential to cause PIN entrapment.
Conflito de Interesses Os autores declaram não haver conflito de interesses.
Trabalho realizado na Pontifícia Universidade Católica de São Paulo, Faculdade de Ciências Médicas e da Saúde, Sorocaba, SP, Brasil.
Work performed at the Pontifícia Universidade Católica de São Paulo, Faculdade de Ciências Médicas e da Saúde, Sorocaba, SP, Brazil.
Referências
- 1.Vergara-Amador E, Ramírez A. Anatomic study of the extensor carpi radialis brevis in its relation with the motor branch of the radial nerve. Orthop Traumatol Surg Res. 2015;101(08):909–912. doi: 10.1016/j.otsr.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 2.Spinner M. The arcade of Frohse and its relationship to posterior interosseous nerve paralysis. J Bone Joint Surg Br. 1968;50(04):809–812. [PubMed] [Google Scholar]
- 3.Rinker B, Effron C R, Beasley R W.Proximal radial compression neuropathy Ann Plast Surg 20045202174–180., discussion 181–183 [DOI] [PubMed] [Google Scholar]
- 4.Frohse F, Fränkel M. Jena: Gustav Fischer; 1908. Die muskeln des menschlichen armes; pp. 164–165. [Google Scholar]
- 5.Clavert P, Lutz J C, Adam P, Wolfram-Gabel R, Liverneaux P, Kahn J L. Frohse's arcade is not the exclusive compression site of the radial nerve in its tunnel. Orthop Traumatol Surg Res. 2009;95(02):114–118. doi: 10.1016/j.otsr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Ozturk A, Kutlu C, Taskara N, Kale A C, Bayraktar B, Cecen A. Anatomic and morphometric study of the arcade of Frohse in cadavers. Surg Radiol Anat. 2005;27(03):171–175. doi: 10.1007/s00276-005-0321-z. [DOI] [PubMed] [Google Scholar]
- 7.Kopell H P, Thompson W AL. Baltimore: William and Wilkins; 1963. Peripheral entrapment neuropathies. [Google Scholar]
- 8.Werner C O. Lateral elbow pain and posterior interosseous nerve entrapment. Acta Orthop Scand Suppl. 1979;174:1–62. doi: 10.3109/ort.1979.50.suppl-174.01. [DOI] [PubMed] [Google Scholar]
- 9.Lister G D, Belsole R B, Kleinert H E. The radial tunnel syndrome. J Hand Surg Am. 1979;4(01):52–59. doi: 10.1016/s0363-5023(79)80105-7. [DOI] [PubMed] [Google Scholar]
- 10.Papadopoulos N, Paraschos A, Pelekis P. Anatomical observations on the arcade of Frohse and other structures related to the deep radial nerve. Anatomical interpretation of deep radial nerve entrapment neuropathy. Folia Morphol (Praha) 1989;37(03):319–327. [PubMed] [Google Scholar]
- 11.Prasartritha T, Liupolvanish P, Rojanakit A. A study of the posterior interosseous nerve (PIN) and the radial tunnel in 30 Thai cadavers. J Hand Surg Am. 1993;18(01):107–112. doi: 10.1016/0363-5023(93)90253-Y. [DOI] [PubMed] [Google Scholar]
- 12.Riffaud L, Morandi X, Godey B et al. Anatomic bases for the compression and neurolysis of the deep branch of the radial nerve in the radial tunnel. Surg Radiol Anat. 1999;21(04):229–233. doi: 10.1007/BF01631390. [DOI] [PubMed] [Google Scholar]
- 13.Ozkan M, Bacakoğlu A K, Gül O, Ekin A, Mağden O. Anatomic study of posterior interosseous nerve in the arcade of Frohse. J Shoulder Elbow Surg. 1999;8(06):617–620. doi: 10.1016/s1058-2746(99)90100-3. [DOI] [PubMed] [Google Scholar]
- 14.Ebraheim N A, Jin F, Pulisetti D, Yeasting R A. Quantitative anatomical study of the posterior interosseous nerve. Am J Orthop. 2000;29(09):702–704. [PubMed] [Google Scholar]
- 15.Konjengbam M, Elangbam J. Radial nerve in the radial tunnel: anatomic sites of entrapment neuropathy. Clin Anat. 2004;17(01):21–25. doi: 10.1002/ca.10194. [DOI] [PubMed] [Google Scholar]
- 16.Meng S, Tinhofer I, Weninger W J, Grisold W. Ultrasound and anatomical correlation of the radial nerve at the arcade of Frohse. Muscle Nerve. 2015;51(06):853–858. doi: 10.1002/mus.24483. [DOI] [PubMed] [Google Scholar]
- 17.Nayak S R, Ramanathan L, Krishnamurthy A et al. Extensor carpi radialis brevis origin, nerve supply and its role in lateral epicondylitis. Surg Radiol Anat. 2010;32(03):207–211. doi: 10.1007/s00276-009-0526-7. [DOI] [PubMed] [Google Scholar]







