A major priority for the National Institutes of Health (NIH, 2018) pain consortium is to create sustainable practices for enhanced pain management. Related patient-centered priorities for the National Cancer Institute (NCI) include addressing patient’s physical and emotional needs throughout cancer diagnosis, treatment, and prognosis (Epstein & Street, 2007). Understanding how pain gets expressed by cancer patients, and responded to by doctors in the cancer clinic, falls squarely within NIH and NCI’s commitments to expand pain research and improve communication and quality of care for patients.
Yet only minimal attention has been given to the interactional organization of pain expressions during patient-doctor clinical encounters. A primary focus has been on general consultations in Great Britain (Heath, 1986, 1989, 2002), and more recently primary care encounters in the United States (McArthur, 2018). Important progress has been made identifying how patients’ reports about unpleasant physical experiences, and doctors’ responses, are constrained by diagnostic environments of medical care. Despite the predominance of pain and discomfort as primary patient complaints (Bresler, 1979; Kam, 2011; Gaskin & Richard, 2012), “diagnostic practice largely precludes the actual expression of suffering by patients” (Heath, 1989, p.114). Situated within diagnostic and physical examination interview phases, and regulated by doctors’ pursuits of biomedical agendas (Byrne & Long, 1976; Heritage & Maynard, 2006; Beach, 2013a, b), patients’ problem presentations are “normally boundaried by physicians’ questions” (Heritage & Robinson, 2006, p. 89).
Questions raised by doctors, in pursuit of biomedical agendas, can limit patients’ contributions. For example, yes/no prefaced questions can discourage elaboration beyond a yes or no answer (Raymond, 2003, 2006; Heritage & Robinson, 2006; Beach, 2013b). When patients do answer more than the question asked they attempt to elaborate their concerns and life-world experiences (Stivers & Heritage, 2001). Explanations can be sought for diagnostic statements (Peräkylä, 1998), or cancer wellness can be justified (Beach, 2013c). In response it has been shown that doctor’s assessments are missing or minimal (Jones, 2001), and closing down patients’ psychosocial concerns are not uncommon (Beach & Mandelbaum 2005). These and related actions contradict advancements in patient-centered care (Epstein & Street, 2007).
Within constrained medical interviews, patients have been shown to display cautiousness and downplay their knowledge and experiences when presenting problems to doctors (Gill, 1998). A wide variety of sequential environments have been identified where patients’ cautious behaviors are evident, including making requests (Robinson, 2001; Gill, Halkowski, & Roberts, 2001), offering lay diagnoses about illness (Beach, 2001; Drew, 2013), disclosing and responding to cancer fears (Beach, Easter, Good, & Pigeron, 2005), and pursuing responses to hopeful health outcomes (Beach, 2014). These findings suggest that talk about presently experienced, or reported painful events in the past, can also be influenced by a host of competing demands. Patients’ constraints include determining how to describe and raise their pain expressions in a timely fashion, while avoiding emotional impulses to “flood out” (Goffman, 1961, p. 55) by displaying strong affect and even crying (Hepburn, 2004). A related problem involves how to provide reasonable grounds for offering pain reports that may or may not be solicited by doctors. When talk about pain does get initiated by patients, demonstrations of pain experiences and suffering are made available to doctors as medical authorities who may discount or directly avoid addressing patients’ concerns (see Heath, 1989, 2002; Heritage, 2005; Beach, 2015; Beach, Gutzmer, & Chapman, 2017). Assessing and responding to the topical relevance of volunteered information about pain and related topics has been shown to be a critical issue, particularly during moments when patients take diagnostic positions about their pain and doctors treat these contributions as encroaching on medical authority (Heath, 2002; McArthur, 2018).
Delicate relationships thus exist “between the “objective” description and “subjective” experience of pain.” (Heath, 1989, p.113) during medical interviews. Clinical encounters are replete with tensions between patients’ epistemic and thus personal knowledge about experienced pain, how these claims get asserted, and the need to manage how doctors respond to patients’ contributions in empathic, sympathetic, or withholding ways (Ruusuvuori, 2005). Considerable evidence exists revealing inherent asymmetries between patients and doctors (Robinson, 2003; Tate, 2018), especially during moments when patients invite doctors to consider and respond to their explanations and life-world experiences (e.g., see Gill, 1998; Peräkylä, 1998, 2002). When patients advance diagnostic reasoning, or threaten medical authority (Heritage, 2005), doctors routinely decline to elaborate on patients’ complaints about everyday circumstances (Drew & Heritage, 1992). Priority is given instead to retrieving medical details and advancing agendas resulting in minimal affiliation with lifeworld disclosures (Maynard & Heritage, 2005). Throughout cancer care, the tendency has been identified “for doctors to provide neither reassurance nor commentary on patients’ contributions, essentially working to close down and move away from patients’ emotional concerns” (Beach, Easter, Good, & Pigeron, 2005, p. 906).
Doctors involved in cancer care are medical authorities who can use their expertise to shape how care progresses. For example, Tate (2018) has recently examined how oncologists produce nuanced treatment recommendations during oncology visits. Doctors initially invite patients to consider their recommendations by using proposals seeking “buy in” to facilitate patients’ alignment and trust. The context in which a recommendations are made shape the way physicians used their expertise. For example, when treatment adjustments need to be altered mid-course, doctors pronounce and tell patients what changes will be made and consequently “there is less interactional room for patients to put their own preferences on the table.” (p.10). These findings confirm speculations that pronouncements are employed when patients are not expected to be resistant (see Stivers, Heritage, Barnes, McCabe, & Thompson et al., 2018).
The inherent complexities and impacts of cancer are noticeable, including disruptions of normal lifestyles, threats to quality and length of life, financial and relational challenges, toxicity and impacts of treatments (e.g., chemotherapy, radiation, surgery, medications), and inherent troubles managing fears, uncertainties, and hopes (Beach & Dozier, 2015). This study focuses specifically on the interactional organization of pain expressions during oncology interviews, and reveals a recurrent tendency for doctors to minimally acknowledge pain that can be common, recurring, yet at times nebulous for patients. First, data are drawn from video recorded oncology interviews, extending prior work on general consultations and primary care by analyzing moments when patients report pain during cancer care. A comparative base can then be provided for assessing whether, and how, the interactional management of pain is more similar or different across diverse modes of medical care. Second, specific attention is drawn to how pain descriptions are not static but malleable as cancer patients upgrade, downgrade, and produce combined orientations when making their experiences available to oncologists. Third, three interactional environments are closely examined: 1) Reporting and responding to past pain/hurt incidents; 2) Doctors’ missing assessments in response to good news announcements about patients’ minimal pain; and 3) Patient-initiated pain responses to doctors’ questions. Fourth, across these environments it is shown how doctors respond to cancer patients’ descriptions by acknowledging, but overwhelmingly not elaborating on or affiliating with, what patients treat as important pain disclosures. An empirical basis for interactional asymmetries between cancer patients and oncologists is thus established. These empirical findings both confirm prior identified patterns comprising pain events in UK consultations and USA primary care, and reveal contingencies tailored to diagnosing and treating cancer as a unique illness and disease.
An overview is first provided of historical orientations including the omnipresent burdens of pain, impacts on societal wellness, economic costs, and inherent problems with measuring and managing pain. This background helps to situate the fundamental importance of understanding how pain gets interactionally managed during medical encounters, key relationships between communication and health, and implications for quality care.
Primal and Problematic Issues: Pain, Measurement, and Management
Pain arises from and creates medical conditions with unpleasant sensory experiences causing considerable individual, emotional, social, and economic consequences. Fluctuating in intensity, location, and duration pain and is an inevitable dimension of being human physically and emotionally. Most often unasked for and undesirable, aversion to pain is instinctual and inherent not just to being alive but living well (Goldstein, 1980): “we pity pain’s victims, condemn its perpetrators, complain about it, combat it in any way we can; ‘pain’ is rooted in ‘poena’—punishment” (Goldstein, 1989, p. 255).
Considerable attention and research has been given to understanding and treating pain as omnipresent in societies worldwide, and thus one of the most pervasive reported and experienced medical symptoms motivating the need for medical care (Institute of Medicine Committee on Advancing Pain Research & Education, 2011; Kam, 2011). Quality of life is most often associated with minimal suffering or pain-free existence (Koskinen, Aho, & Nyholm, 2016), whereas chronic and recurring acute pain are conducive to depressive symptoms and outcomes (Bair, Robinson, Katon, & Kroenke, 2003). The comorbidity of pain and depression leads to lower quality of life, relationship difficulties, decreased work function, and increased burdens on the healthcare system (Gallagher & Verma, 1999; Outcalt et al., 2015).
The total economic burden of medical care for pain in the United States alone is striking (Gaskin & Richard, 2012). At a cost exceeding $600 billion annually, pain care expenditures more than double the costs of heart disease ($309 billion), cancer, ($243 billion) and diabetes ($188 billion). In addition to direct medical costs, pain is also a powerful contributor to loss of productivity at work, culminating in over $300 billion in lost productivity, and a primary cause of both temporary and permanent work disability (Smith et al., 2001).
Faced with the growing opioid crisis, the NIH has launched initiatives such as the HEAL initiative (Helping to End Addiction Long Term) to investigate and promote behavioral interventions for pain management as an alternative to opioids (NIH, 2018). Research focused on pain communication, a common yet little understood behavioral medium for improving pain experiences, aligns with NIH initiatives for multimodal and non-pharmacological approaches to pain management. Understanding how pain is expressed and responded to in the cancer clinic is closely aligned with NIH research priorities and the need to create sustainable practices for enhanced pain management.
Limitations to Measuring and Conceptualizing Pain
Across the medical sciences, there are many objective measurements for evaluating components of health. Blood pressure can be precisely and accurately measured with a sphygmomanometer. Cholesterol, which can affect risk for coronary heart disease, is measured via lipid panel. Most cancers can be diagnosed with certainty through a biopsy. Despite the prevalence and ominous burdens of pain, however, considerable problems exist with measuring and assessing pain experiences and impacts. Tools for measuring pain focus on individuals, including the cold pressor task which involves having individuals hold their hand in water that is approximately 10 degrees Celsius (+/− 1 degree Celsius) for as long as the participant can tolerate (Baeyer, Piira, Chambers, Trapanotto, & Zeltzer, 2005). However, this procedure does not measure pain itself but rather pain tolerance. Similarly, technologies such as computerized cuff pressures (Jerpersen, et al., 2013) are employed to assess how variations in individuals’ pain thresholds require alternative pain management strategies.
Considerable attention has been given to phenomena such as individuals’ abilities to tolerate pain, experiences with and emotional impacts of pain (DeWall & Baumeister, 2006; Twigg, 1970; Woodrow, Friedman, Siegelaub, & Collen, 1972), and the neuromusculoskeletal transmission of pain stimuli. Pain caused by cancer, for example, is typically associated with consequences of metastasis causing somatic (e.g., pain receptors triggered as cancer spreads to the bone), neuropathic (e.g., injuries to nervous system resulting in burning or tingling), and visceral pain (e.g., throbbing arising from tumor pressure sensations on organs).
Figure 1 (below) provides a visual model for conceptualizing a wide array of pain dimensions:
Figure 1.
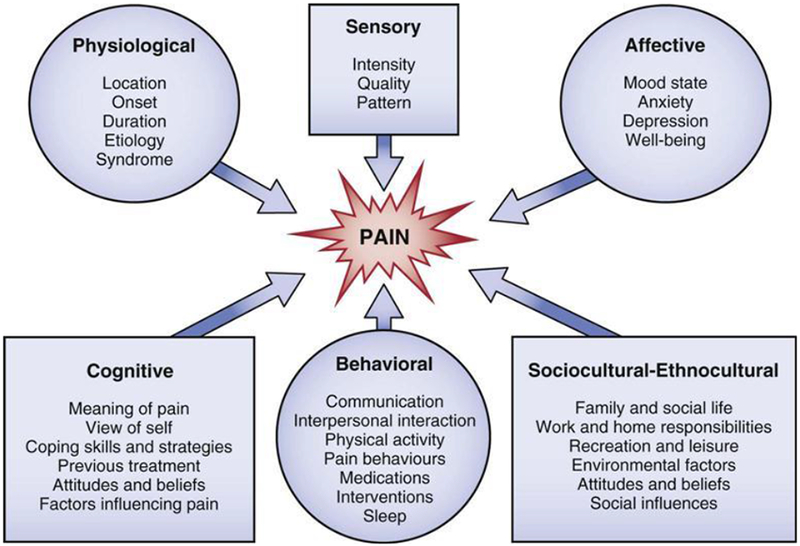
The Dimensions of Pain (Petty & Moore, 1998)
Though obvious relationships exist across these related categories, it is useful to note that activities such as ‘Communication, and ‘Interpersonal interaction’, are listed within the ‘Behavioral’ designation. However, when investigating how pain communication is embedded in social actions, co-constructed by patients and doctors when addressing numerous pain issues, analysis will reveal that topics listed in separate categories in Figure 1 are overlapping and get routinely enacted through talk and bodily actions (e.g., intensity, locations, meanings of and factors influencing pain, attitudes and beliefs). As discussed below, however, existing literature on communication and pain management communication has focused on self-reported survey research.
Communication Approaches to Pain and Cancer
Patients are routinely surveyed about their pain communication to determine barriers to reporting, and associations between communication and clinical pain outcomes, such as pain intensity or analgesic use (Ovayolu, Ovayolu, & Aytac et al., 2014; Potter, Wiseman, Dunn, & Boyle, 2003). Differences in pain management have been examined, such as patients more frequently citing financial burdens, whereas caregivers are often more concerned with fatigue (Ovayolu et al., (2014). Doctors’ strategies for improving pain management communication have also been identified, such as expressing concern for patient’s feelings, using “I” statements, and partnering with patients amidst difficult news by reassuring patients that medical problems will be faced together (Gupta, 2015). Relying on focus groups and interviews, problems with communication about cancer pain have revealed a wide variety of communication problems including general information exchange errors, medication confusion, lack of shared decision making, stigma, and addiction worries (Kimberlin, Brushwood, Allen, Radson, & Wilson, 2004). Taken together, however, these approaches inherently focus on the patients’ and caregivers’ perspectives without assessing communication occurring during recorded clinical encounters. So doing can reveal how pain expressions get initiated, co-constructed, and addressed as meaningful or bypassed by doctors.
One notable exception is Street et al.’s (2010) randomized control study on how tailored education-coaching (TEC) might enhance cancer patients’ abilities to more effectively raise and address their pain concerns with physicians. Patients receiving the TEC intervention more frequently addressed their pain concerns and rated their physicians as being more informative about pain management. Patients’ questions, assertiveness, and expressed concerns were identified and attention was drawn to selected patients’ actions and less to physicians’ responses. Implications of this study include the need to investigate not only a broader range of social actions, but more directly how patient-initiated and physician-responsive behaviors co-occur during ordinary clinical encounters. This study addresses both of these concerns.
Situating Pain Interactionally
By attending closely to recorded and transcribed pain interactions, the focus extends beyond individuals and bodily functions to the interactional organization of how patients display their experiential knowledge and ways doctors respond by relying on their medical expertise and authority. It becomes possible to identify specific interactional practices and communication patterns comprising clinical encounters as verifiable documentations of intersubjectively produced social actions. Consider, for example, Heath’s (1989) descriptions of occasions during physical examinations (e.g., rotating a painful foot) where doctors must inflict pain in order to assess, diagnose, and treat patients’ complaints. The vocal ‘pain cries’ patients utter (e.g., “arghh*hhh(*hm)” ), aspirated and affective (see also Hepburn, 2004; Hepburn & Potter, 2007, 2012), demonstrate their authentic subjective experiences of being hurt as a foot gets manipulated. Doctors can directly observe how and when these reactions occur as a primary basis for their diagnosis. The patient’s painful cry is heard as responsive to a doctor’s inspecting actions, and not as an unsolicited or independent attempt by patient to offer pain information or to diagnose a medical condition. These actions function to preserve the interactional asymmetry between doctor and patient. The doctor’s response to patient’s painful utterances provides additional evidence for these asymmetries:
The cry of pain does not occasion sympathy or appreciation from the practitioner, or is the actual experience of suffering by the patient addressed as a topic in its own right. Rather the pain is managed within the framework of the diagnostic activity in which the doctor is engaged… the doctor delicately side-steps appreciation of the suffering and discourages further cries of pain from the patient. In this way he is able to pursue the diagnostic enquiries at hand. (pp 115, 116)
During primary care (McArthur, 2018), painful displays by patients avoid offering diagnostic reasoning in two primary environments: Delivering painful information because doctors have asked for it; and (as with Heath, 1989) during doctor’s physical examination, when attempting to locate the site and intensity of pain, patients display a triggered response exuding pain indicating a hurting body (e.g., grimacing when a doctor twists a patient’s foot to determine pain location). Both environments provide evidence of how patients withhold offering diagnoses and respond to doctors’ medical agendas and procedures.
Data and Method
Interactions between patients and doctors were video recorded at an urban clinic and academic research facility that is an NCI designated comprehensive cancer center. Full institutional review board (IRB) approvals were granted and consent was obtained from patients and oncologists included in this observational study. Small digital cameras on tripods recorded medical interviews without the presence of researchers.
Conversation analysis (CA) was used to identify and analyze a total collection of 146 pain and other references (e.g., painful, hurt) across 65 video recorded oncology interviews. Visual and embodied displays of pain (e.g., grimaces, gestures, bodily touches) were not analyzed for this study. Initial data instances were identified in the talk by word searches (e.g., pain, painful, hurt, discomfort). Subsequent and more detailed analyses identified a subsample of 27 instances when patients initiated and doctors responded to pain/hurt expressions. For closer examination, this article examines 9/27 selected excerpts reflecting alternative contexts in which pain/hurt get raised, and how doctors responded to patient-initiated pain expressions. Three selection criteria were employed: 1) Patients initiating reconstructions of past incidents involving pain, and the suffering they have incurred; 2) Both intense and minimal pain descriptions; and 3) Patients’ references to pain when responding to doctors’ questions.
Video recordings were carefully transcribed and repeatedly examined to investigate how pain was raised in oncology encounters (see Drew & Heritage, 2006; Maynard & Heritage, 2005; Beach, 2013a). The empirical rigor of CA extends traditional patient-provider communication, relying on generalized coding schemes not grounded in close examinations of how participants make available their understandings to one another in the natural course of evolving interactions (Sidnell & Stivers, 2013; Beach, Gutzmer, & Chapman, 2017). Specific practices and patterns of social action are shown to be evident within intricate details and nuances of interaction, including seemingly unimportant yet consequential utterances such as “oh” (Heritage, 1984, 2002), “mm” (Gardner, 1997), or “okay” (Beach, 1993). By extending analysis to interactions when pain gets raised and responded to, it becomes possible to discover co-produced patterns involving pain communication. Based on these empirical findings, recommendations for future research inquiries and improving medical care are described.
Reporting and Responding to Past Pain/Hurt Incidents
Analysis begins with three case studies reflecting how different cancer patients initiate tellings by using dramatic and vivid language to portray past pain/hurt experiences. In turn, different doctors produce minimal responses not directly addressing, commiserating with, nor seeking further elaboration of prior sufferings reported by patients. Priority is given instead to soliciting and pursuing diagnostic information.
“I would be screaming!”
The first example involves a patient who had previously been diagnosed with multiple myeloma, an uncommon blood cancer negatively impacting plasma cells and reducing antibodies in the bone marrow. He is seeking a second opinion and alternative treatment options from an oncologist. Prior discussion focused on symptoms of his current medications, including leg swelling and blood clots. This excerpt begins by patient volunteering that he does not consistently follow recommendations for wearing his “pressure sock” (lines 1-2):
1) OC D1P10:(19-20)
| 1 | Patient: | I’m not going to be the best guy to put on the pressure sock on it | |
| 2 | every:day? | ||
| 3 | Doctor: | Were there any inciting events for your leg?= | |
| 4 | Patient: | =Oh yeah?= | |
| 5 | Doctor: | Did you get on an airplane or something?= | |
| 6 | Patient: | =Oh yeah yeah? | |
| 7 | Doctor: | [What was it?] | |
| 8 | Patient: | [I’m your typ]ical guy. Who could be like- like yo:u kno:w be- be the | |
| 9 | head- beat in the head? | ||
| 10 | Doctor: | Uh huh. | |
| 11 | Patient | And until someone would te- bu:t I still wouldn’t listen still. (.) | |
| 12 | → | No, there was pain (.) in the leg? | |
| 13 | Doctor: | Uh huh. | |
| 14 | Patient | → | If you just touched it?= |
| 15 | Doctor: | =Yeah? | |
| 16 | Patient: | → | I would be screaming! = |
| 17 | Doctor: | → | =Bu:t I mean did anything- is there any reason why you got [(it then)]. |
| 18 | Patient: | [ I was ] | |
| 19 | driving a lot. >Every other day to LA (with each event) and between | ||
| 20 | every other day I was flying to Pittsburg?< |
In response doctor does not address patient’s non-compliance disclosure. But with three contiguous questions (lines 3, 5, 7), ending with an assertive “What was it?”, he seeks information useful for diagnosis by inquiring about whether there were “inciting events” that may have contributed to leg swelling. Patient repeatedly confirms (lines 4, 6) but does not immediately address these activities. Instead and in overlap, he produces two disjointed and non-sensical utterances (lines 8-9, 11) elaborating his reported lack of adherence to medical advice. (Roughly translated, “I’m a typical guy who gets beat in the head by others to follow advice, but still wouldn’t listen.”). On occasions when patients produce explanations to doctors talk is not uncommonly dysfluent, in part because patients can be heard as deferring to medical authority and cautious about the actions they initiate (Gill, 1998). In Excerpt 2 (above), patient not only resists direct response to doctor’s prior questions, but extends talk about non-compliance which doctor had previously disattended.
The patient then offers an apparent shift in footing (Goffman, 1961; Clayman, 1992) by announcing “No, there was pain (.) in the leg?” (line 12). Raising “pain” further delays answering doctor’s prior questions, focused on “inciting events”, in lieu of reporting his past and subjective experience. Patient continues by providing dramatic evidence that “pain” does indeed qualify as an “inciting event” deserving consideration: “If you just touched it?...I would be screaming!” (lines 14,16). These exclaimed utterances vividly describe patient’s previous unpleasant experiences. Offered as reported past experiences, patient is not presenting current complaints and inviting doctor to witness and respond to here-and-now suffering he is enduring.
When patient states “If you just touched it?”, doctor does display close monitoring by providing a “Yeah?” response. Yet this distinction, between patient’s past events vs. present conditions, creates an opportunity for the doctor to employ a latched “=Bu:t I mean” (line 17) as a self-repair preface (see, e.g., Schegloff, 1989; Litzinger, 2013) designed to fix incorrect understandings by patient. Doctor makes clear that no empathic or sympathetic response will be provided (e.g., “It sounds like you’ve been suffering”, or “That must have been difficult, I’m sorry to hear that”), and that patient’s upgraded yet past description needn’t even be acknowledged. Instead, doctor re-asserts his pursuit of diagnostic information with “is there any reason you got (it then).” (line 17), giving priority not to patient’s prior pain and suffering but to events that may have caused current leg swelling. This persistence does finally elicit a more direct answer from patient that he was driving and flying a lot (lines 19-20), both responsive to doctor’s earlier “Did you get on an airplane or something?” (line 5).
Several prominent features are apparent in Excerpt 1 (above), moments drawn from a routine oncology interview when symptomatic “leg swelling” gets addressed. Competing agendas emerge and get interactionally managed, revealing asymmetries evident in different priorities pursued by patient and doctor. Patient treats issues with non-compliance and severe past pain as meaningful life-world topics. In contrast, doctor does not attend to what patient treats as significant, but is unremitting in pursuit of obtaining background information necessary for rendering a diagnosis and eventual treatment recommendations for current leg swelling conditions. At the completion of this excerpt, doctor does obtain a responsive answer (lines 18-20) to his initial questions. En route to this outcome, however, patient-initiated actions are passed-by in favor of doctor’s medical agenda. Patient does have epistemic access to prior “pain” experiences and the right to report them. But in this constrained interview environment, pain expressions remain encapsulated in a brief and dramatized reconstruction having minimal or no apparent impacts on a doctor’s persistent efforts to solicit and receive medically relevant information.
“doubled over in pa:in”
A similar instance appears below as patient expresses past dramatic pain experiences, which get acknowledged by doctor, but not further addressed. During this encounter, a leukemia patient has changed locations and meets with a new doctor to review her medical records, treatment progress, and various health problems (e.g., blood thinning, dehydration, headaches). Near the end of medical history-taking, doctor summarizes surgeries patient had undergone and patient briefly describes her most recent surgery (lines 1-6):
2) OC D4 P2: (11)
| 1 | Doctor: | Um (1.0) um (0.5) gastric bypass, gall bladder surgery and- | |
| 2 | Patient: | Exploratory surgery. | |
| 3 | Doctor: | Yeah, when was that one? | |
| 4 | Patient: | That one was the most recent I believe that was last year. (1.0) I think it | |
| 5 | was in November or so, and I did most of these at um St. Joseph’s | ||
| 6 | Hospital up in Burbank? | ||
| 7 | Doctor: | And what was that for. | |
| 8 | Patient: | → | That was uh because I was having so::: much pain.= I was like doubled over |
| 9 | → | in pa:in? (0.3) And they said you know kind of how a hose is bent and it’s on- = | |
| 10 | Doctor: | → | =Uh huh.= |
| 11 | Patient: | =and your blood is being (0.7) >basically he said my blood is being cut off< | |
| 12 | right there- there was like scar tissue that they had to kinda remo::ve. (0.7) | ||
| 13 | And they had to take me off of the Coumadin and put me on ( ), put | ||
| 14 | me on Heparin and keep me in the hospital for three to four days. And he- | ||
| 15 | he was an amazing surgeon, his name was, Dr. Kaleb? | ||
| 16 | Doctor: | Uh huh. | |
| 17 | Patient: | And um he’s done all those surgeries. | |
| 18 | Doctor: | → | Did that work. |
| 19 | Patient: | Yes. (0.3) Yeah. | |
| 20 | Doctor: | → | Um (0.5) any other surgeries? |
| 21 | Patient: | No. |
In response to doctor’s question about what her last surgery was for (line 7), patient begins her response with an animated description of “having so::: much pain.= I was like doubled over in pa:in?”. An additional upgrade is provided by comparing herself to being like a ‘bent hose’. Analogies can be viewed as “an invaluable but imperfect tool for communicating pain” (Schott, 2004, p. 211), raising images familiar to the imagination, and patient’s description does receive “Uh huh.” acknowledgment from doctor (line 10). This minimal response facilitates a continued and extended telling by patient (lines 11-15) that includes reporting what a prior doctor had stated (her blood being cut off, and scar tissue requiring removal), the medications she was prescribed, and how long she was hospitalized. She completes her telling with a positive assessment of the surgeon (line 15), which is also acknowledged with “Uh huh.” by the doctor.
At the outset of patient’s telling, there are several possible reasons why her animated pain descriptions were not treated by doctor as deserving or requiring empathic nor sympathetic responses. First, asking what a surgery was “for” was designed to receive a biomedical response, which was eventually provided (i.e., blood constriction and to remove scar tissue). In this context patient’s pain-preface, though dramatic and upgraded, was heard as preliminary to receiving what doctor prioritized as essential information. Second, as patient’s pain reporting was about a past time period which patient was en route to providing a more extended telling about, and not displaying pain at this moment, doctor was placed in a position of monitoring patient’s story without having to address pain directly. And third, as evident in doctor’s “Did that work?” and “any other surgeries? questions (lines 18-19), priorities are given to soliciting surgical information relevant for current care. These options are enacted rather than entering into and coming alongside difficulties with patient’s prior pain experiences and incurred suffering, however troubling these occurrences might have been.
“it ac::tually hurt to tou:ch”
A third example of patient reporting prior difficulties occurs in Excerpt 3 (below), but in this instance rather than explicitly invoking “pain” she twice invokes a related term – “hurt”. These moments are drawn from a routine return visit to discuss tests and images for patient’s non-Hodgkins lymphoma, a disease of the lymph nodes resulting in possible weakening of the lymphatic system including infections. Before this excerpt, doctor has announced that “your scans look good.”, which patient treats with surprise and queries whether that includes the swollen node on her neck. In line 1 (below) patient describes that node as a “ma:rble”:
3) OC D1P1:(10)
| 1 | Patient: | It was this th:ing that wa:s like a ma:rble. | |
| 2 | (0.5) | ||
| 3 | Patient: | → | But I did have a terrible cold. |
| 4 | Doctor: | But actually what- what, okay. | |
| 5 | Patient: | → | I had a terr:ible cold. |
| 6 | Doctor: | → | You had a terrible cold. |
| 7 | Patient: | → | But it hu::rt. |
| 8 | Doctor: | → | Mm hm. |
| 9 | Patient: | → | But it ac::tually hurt to to:uch. |
| 10 | (1.3) | ||
| 11 | Doctor: | .hhh It may be that they are more reacti:ve, you know, just because of | |
| 12 | the l:ow grade lymphoma. |
In line 1 patient begins to characterize her symptoms with an analogy by comparing the swollen lymph node near her throat to a “ma:rble.”, a description that may embody features of size and density. Following a slight pause, she then offers a lay diagnosis (Beach, 2001; Ten Have, 2001) for her symptoms: “But I did have a terrible cold.” (line 3). As a cold can trigger the immune system to produce additional white blood cells to ward off illness, patient may be taking the position that the node is swollen and harder due to additional cells. Her doctor next displays some confusion with her previous utterance (line 4), however, prompting patient not to reveal her lay reasoning but to restate with a more extreme “I had a terr:ible cold.” (line 5). Within repetition sequences, a second saying allows for speakers to clarify and emphasize their initial reportings and positions (Wong, 2000). This is evident with patient’s upgraded prosodic construction and extreme case formulation (Pomerantz, 1986), actions which can be designed to legitimize a claim or position. And it is the doctor that now repeats with a nearly verbatim “You had a terr:ible cold” (line 6), which displays having heard patient encouraging continuation (Pomerantz, 1984).
With patient’s following “But it hu::rt” (line 7) she doesn’t just describe the node and offer a possible diagnosis, but discloses her subjective experience with “hurt”. This expansion responds to doctor’s prior verbatim repeat by bolstering her position that her “terr:ible cold” had other negative symptoms, and by specifically addressing that her node was painful. While these actions further justify that the woes she withstood were unpleasant, doctor’s “Mm hm.” (line 8) provides only minimal acknowledgment. In pursuit of response (Pomerantz, 1984), a more vivid description demonstration of her suffering follows: “But it ac::tually hurt to to:uch” (line 9). With added descriptive force, patient’s “ac::tually” evidences the authenticity of her reporting, and “to:uch” establishes her epistemic claim as grounded in direct personal experience.
Nevertheless, following an extended (1.3) pause (line 10), doctor responds with a diagnostic evaluation absent of any recognition for, or commiseration with, patient’s depictions of being sick and experiencing “hurt”. With “It may be that they are more react:ive, you know, just because of the l:ow grade lymphoma” (lines 11-12), doctor’s response confirms how and why patient raised “terr:ible cold” as a lay diagnosis in the first instance (line 4). However, it is offered by doctor not as an agreement or confirmation of patient’s lay reasoning, but as an independent assessment. Doctor also draws attention away from patient’s repeated and concerted efforts to make clear, and receive support or understanding, for the suffering she incurred that was repeatedly constructed as real and consequential.
Empirical Basis for Interactional Asymmetries
These initial three excerpts reveal several distinct features of interactional asymmetries between cancer patients and their doctors when pain/hurt gets invoked. Each of the references to pain/hurt are not triggered by doctors physically manipulating patients to locate and assess pain intensity, or patients’ volunteering offerings about present pain/hurt sensations. Rather, patients initiate talk about past pain/hurt events, and other life-world experiences (e.g., non-compliance), and make these available for doctors’ consideration. In all cases, patients invest considerable efforts to produce progressive descriptions: In Excerpt 1, “pain → touched it → screaming!”; In Excerpt 2, “pain → doubled over in pa::in”, → “hose is bent”; and Excerpt 3, “terrible cold → terr:ible cold, → hu:rt → hurt to to:uch”. If doctors do respond within these sequential environments, they do so with minimal acknowledgments (e.g., “Mm hm”, “Uh huh”). Patients orient to these minimal responses by expanding their pain/hurt descriptions and upgrading with more extreme and vivid language. In Excerpts 1 & 3, patients’ expansions appear to be in pursuit of noticeably absent or minimal responses. Patients upgrade to legitimize their pain, solicit explanation or evaluation, express extreme pain intensity, and/or solicit empathic or sympathetic responses. In Excerpt 2 patient conveys the seriousness of her past condition, qualifying her as having a doctorable condition worthy of surgical intervention (Heritage & Robinson, 2006). Together, these progressive characterizations exemplify how pain/hurt expressions are dynamic and malleable, recruited and tailored to achieve particular social actions such as pursuing responses and recruiting extreme case formulations (Pomerantz, 1986) to legitimize prior sickness.
Across these examples, doctors overwhelmingly monitor but do not explicitly address patient-initiated actions about subjective pain experiences. Patients gain access to talking, and exploit opportunities to draw doctors into their past pain/hurt sensations, to gain appreciation and understandings for trying and at times intense medical challenges they have faced. When residual symptoms and impacts are brought into play by patients, they remain encapsulated as brief and often dramatic past reconstructions treated as central to their medical history but not presently experienced. These attempts may not go unnoticed by doctors, but vocal and elaborated expressions are repeatedly not provided. Priority is given instead to seeking diagnostic information for current medical conditions. A gap thus exists between reported unpleasant sensations patients may have experienced in the past, and doctors’ pursuits of information relevant to present circumstances. Patients’ disclosures about past pain experiences seem to have little bearing on doctors’ pursuits of present information as relevant for diagnosis, treatment, and ongoing care.
Missing Assessments in Response to Patients’ Minimal Pain
Physicians also provide minimal responses even when pain is referenced in the midst of good news announcements. On occasions when cancer patients do initiate talk about current pain, the malleable nature of pain presentations persist. But rather than upgrading the intensity of pain experienced as evident in Excerpts 1-3 (above), in Excerpt 4 patient uses three different resources to explicitly downgrade her pain condition:
4) OCD1P1:(15)
| 1 | Patient: | → | Cause occasionally I do feel some pain. I mean it’s more like itching. |
| 2 | Doctor: | Mm hm. |
With “occasionally” and “some” patient minimizes the reported pain, then further downgrades with “more like itching”. While itching and pain have been found to target different neural mechanisms, there are perceptual contrasts between the two sensations and itching is typically a less severe symptom than pain (Mochizuki et al., 2007). In this instance, patient’s “I mean” is a self-initiated repair amending a previous stance in the same turn to clarify symptoms to her doctor (Schegloff, Jefferson, & Sacks, 1977; see also Kitzinger, 2013). This repair is not necessarily an attempt by the patient to fix a problem, since “repair/correction is sometimes found where there is no hearable error, mistake, or fault” (Schegloff, 1996, p. 363). What is being presented to doctor is the minimal presence of pain, actions providing another clear example of how patients construct dynamic and shifting pain descriptions to clarify their experiences to doctors.
Patient also displays efforts to ‘justify wellness’ involving “attempts to talk health and healing into being” (Beach, 2013c, p. 579). Justifying wellness is a common resource used by cancer patients to promote hope, and minimize fears and uncertainties, occasioned by the threat of cancer. When patients justify wellness, such as announcing that pain is minimal rather than increasing and difficult to cope with, patients make available to doctors prima facie evidence that their condition is tolerable, perhaps even improving, when making the case for wellness in the face of sickness. Such efforts lay healing grounds for doctors’ consideration and response. Receipted with “Mm hm.” (line 2), however, doctor minimally acknowledges while withholding further assessment (see Jones, 2001) of what is designed as a good news announcement provided by patient.
Consider also Excerpt 5 (below), involving a leukemia patient facing terminal cancer. Patient attempts to progressively build a case for improved health and wellness by repeatedly nominating good news (lines 1-2, 4, 6, & 12), actions designed in pursuit of marked recognition or reassurance from doctor which are not forthcoming. Patient begins by describing frequent but not excessive bowel movements and a “very good” appetite (lines 1-2):
5) OCD1P4:(3)
| 1 | Patient: | → | And that now now I’m going to the toilet about three times a day or the |
| 2 | most and the, it’s feeling better. My appetite is very good. | ||
| 3 | Doctor: | Uh hm. | |
| 4 | Patient: | → | The- the pain that I feel I think is normal for the surgery. |
| 5 | Doctor: | Um hm. | |
| 6 | Patient: | → | And uh (.) everything seems to be fine. |
| 7 | Doctor: | Okay. | |
| 8 | Patient: | Except for insurance u:h my doctor told me to have uh (.) have uh | |
| 9 | uh chemotherapy. | ||
| 10 | Doctor: | Um hm. | |
| 11 | (3.0) | ||
| 12 | Patient: | → | Nobody in my family ever had cancer. |
| 13 | Doctor: | → | Uh hm, m:ka:y. (.) And you’re not allergic to any medicine? |
| 14 | Patient: | No uh, I have been very healthy. | |
| 15 | Doctor: | Uh huh. |
Following doctor’s minimal “Uh hm.” acknowledgment (line 3), his pain is described as “normal for the surgery” (line 4), which also receives an “Um hm.” (line 5). Anchored in their knowledge and past experiences, patients have been shown to invoke ‘normal’ as a resource to maintain a stance of resilience, justify their wellness, and mitigate the threat of serious disease (Bauman, Cameron, Zimmermarn, & Leventhal, 1989; Gutzmer & Beach, 2015).
With “everything seems to be fine” (line 6), patient provides a third-part and generalized list completer (Jefferson, 1990), an action further soliciting doctor’s affirmation of the good news being presented. While doctor’s “Okay.” (line 7) acknowledges, it also moves toward closure which eventuates in doctor’s shift-implicative return to the medical agenda (line 13). This shift, away from patient’s good new descriptions in favor of medical history-taking, follows a long (3.0) pause (line 11) regarding patient’s insurance and chemotherapy. By next stating “Nobody in my family ever had cancer.” (line 12) patient then provides an even stronger bid to explain his medical history and seek doctor’s elaboration. Doctor does not respond directly to patient’s reference to family cancer history, a reporting with potential diagnostic implications. This lack of response adds further evidence to previously stated findings: Patients who take diagnostic positions may encroach on doctors’ medical authority or, at minimum, be treated as formulating stances claiming lay vs. biomedical knowledge (Heath, 2002; McArthur, 2018). By raising “allergic to any medicine” (line 15) as a more important option, doctor leaves hanging serial attempts by patient to document wellness and offer a diagnostic stance toward family history. Both are unsuccessful bids to elicit affirmation and elaboration by doctor.
Overwhelmingly, then, patients who report past intense pain experiences, or current minimal symptoms revealing good health news, are receiving only minimal responses from doctors. At times these minimal responses are shift-implicative, employed to set-up doctors’ next-positioned pursuits of medical agendas (e.g., allergies, Excerpt 10, below). During other activities, including physical examinations, patient’s repeated references to pain may also not elicit direct responses. In Excerpt 6 (below), a lymphoma patient has complained about persistent pain and discomfort in his gums and mouth. As the doctor begins to look into his mouth, patient queries with “No blood?”, which doctor repeats and confirms (lines 1-2). Patient then continues with “Just swollen. Very painful.” (line 3), which goes unaddressed as doctor looks inside patient’s mouth for 23 seconds:
6) OC D4P6:(3-4)
| 1 | Patient: | No blood? | |
| 2 | Doctor: | No blood. | |
| 3 | Patient: | → | Just swollen. Very painful. |
| 4 | ((23 seconds pass as doctor checks inside patient’s mouth)) | ||
| 5 | Doctor: | There is like u:hm (0.8) like a like an installation (0.2) band (.) | |
| 6 | around the teeth? I don’t know if you have seen that, but both | ||
| 7 | (interiorly and posteriorly) you have this kind of thickening of the | ||
| 8 | (cosa) that is kind of rubbing the edge- the edge of the teeth? Uhm | ||
| 9 | sometimes we can see this in a- in lymphomas and leukemia’s, build | ||
| 10 | up of by products in this case it’s rubbing. U::m? | ||
| 11 | Patient: | → | Very painful. |
| 12 | Doctor: | Um hm. |
Doctor’s summary of what he observed (lines 5-10) describes a “band” and “thickening” of lining which may cause “rubbing” and inflammation. But he does not display understanding or appreciation for why those symptoms might be painful. In response, patient again asserts “Very painful.” (line 11), which doctor only minimally acknowledges.
Patient-Initiated Pain Responses to Doctors’ Questions
This analysis concludes with three additional case studies examining how cancer patients respond to doctors’ questions about current and prior pain and related symptoms. The patterns documented throughout Excerpts 1-9 (above) are further evident as doctors display minimal or absent responses to patients’ pain descriptions.
“just a sharp pain (0.2) in my bra::in”
In Excerpt 7, doctor’s query (lines 1-2) does not specifically address pain, but patient moves next to describe his “mi:gra:ine” as painful:
7) OCD1P10:(16-17)
| 1 | Doctor: | Currently the:n do you have a:ny proble:ms with (.) blurred vision, | |
| 2 | headaches, anything like that.= | ||
| 3 | Patient: | =Headaches uhm I think, I mean some people say it’s a mi:gra:ine? | |
| 4 | → | It’s like a- a- a just a sharp pain (0.2) in my bra::in.=Someone’s taking | |
| 5 | → | (like a knife) and going like this a::hh £to it.£ | |
| 6 | Doctor: | Heh heh. | |
| 7 | Patient: | → | You know uh it will go away if I take you know (.) uhm uh- uh- |
| 8 | → | uhm you know uh- ((snapping fingers)) £I am s:o lost for words I | |
| 9 | know all these words!£ | ||
| 10 | Doctor: | £Some kind of pain medicine.£ | |
| 11 | Patient: | £Some kind of pain medicine.£ Yeah uh- uhm some kind of anti- | |
| 12 | inflammatory? | ||
| 13 | Doctor: | Yeah like ibuprofen? | |
| 14 | Patient: | Ibuprofen. I even took vicodine as an (absolute). | |
| 15 | Doctor: | Okay. | |
| 16 | Patient: | Yeah. | |
| 17 | Doctor: | → | Okay, alright. You mentioned you had th:e heartburn kind of symptoms |
| 18 | that se:ems to be a little bit better now. | ||
| 19 | Patient: | Yeah. |
The patient gives an uncertain response, claiming insufficient knowledge (Beach & Metzger, 1997) by stating that “some people say” rather than personally claiming a “mi:gra:ine” (lines 3-5). Patients’ lay diagnoses are often surrounded by insufficient knowledge claims and a general downplaying of knowledge in deference to doctors’ authority (Gill, 1998). This excerpt is a clear example of a patient exercising caution, hesitancy, and uncertainty when presenting pain to a doctor. He continues to characterize pain as, “It’s like a- a- a just a sharp pain (0.2) in my bra::in.=Someone’s taking (like a knife) and going like this a::hh £to it.£” (lines 4-5). Pain is characterized dramatically through analogy: Her migraine is compared to being stabbed in her head with a knife, a gory mental imagery conveying intensity and sensation. The patient ends this utterance with laughter marking the delicacy of this matter. Patients “rely on laughter and humor when attempting to remedy, cope with, and buffer a wide range of awkward, sensitive, embarrassing, fearful, anxious, atypical, strange, or abnormal situations” (Beach & Prickett, 2016, p. 1). In short, the patient’s laughter displays a recognition and sensitivity to having produced an utterance (lines 3-5) filled with extreme language.
In lines 6 doctor laughs in response to patient’s dramatic pain description, and then assists patient’s search to name a pain medication (lines 7-17). But the pain patient has so vividly animated goes unaddressed. Instead, doctor moves forward by closing the sequence to address “heartburn” (lines 17-18).
“I did suffer a bit”
When doctor repeatedly asks about pains in Excerpt 11 (lines 1-3), patient simply states “No.” (line 4). Doctor’s “No. Okay.” response (line 5) acknowledges, but given the inclusiveness of prior question (“↑anywhere”, “anything”), provides a nominal reaction that does not assess nor elaborate on the good news patient’s “No.” represents:
8) OCD1P10:(6)
| 1 | Doctor: | Do you have any pain (.) ↑anywhere else in your body. Bone | |
| 2 | → | pain of any ki:nd? Just pains anything? Aches, pain, complaints, | |
| 3 | anything? | ||
| 4 | Patient: | → | No. |
| 5 | Doctor: | → | No. Okay. |
| 6 | Patient: | → | Just stiffness that’s because (.) you know I do need to go out and |
| 7 | exerci:se and you know stretch. And my primary physician told me | ||
| 8 | to do that and like I try to so. (.) U:hm (0.2) no, I don’t have any of | ||
| 9 | → | that? U:hm the only thing that I can maybe say is tha:t I did suffer a | |
| 10 | bit. | ||
| 11 | Doctor: | Mm hm. | |
| 12 | Patient: | → | A:nd u:hm as you can see (0.2) my leg is s::wollen still. This is six |
| 13 | years ago.= | ||
| 14 | Doctor: | =Six years ago! | |
| 15 | Patient: | Yeah. Yeah. |
After stating no pain, and elaborating on “stiffness” yet the need to “exerci:se” as instructed by another physician, patient discloses that “the only thing that I can maybe say is tha:t I did suffer a bit.” (lines 9-10). Her use of “suffer” is an upgrade from stiffness, aches, or pain. Suffering insinuates longer term agony that imposes a physical and emotional toll on the sufferer. In this instance, patient’s “suffer” offering insures doctor’s realization that despite patient stating the absence of pain, she did face challenging health issues including problems with a leg that is still swollen (line 12) after six years had passed. With “Six years ago!” (line 14) doctor treats patient’s reporting as surprising and even remarkable. Subsequent interaction (not on transcription) focuses on this duration of time, but without doctor directly addressing the patient’s experiences with pains and impacts comprising longer term suffering.
“No pain at all and that worried me”
With cancer care, even the absence of pain and suffering can be worrying. What is striking about the following example is not just that doctor assumed patient was experiencing abdominal pains (lines 1-2), which patient repeatedly denies (line 3, 8, 10, 12-13). In addition, the patient noticed blood while using the toilet (lines 4-7), and states “No pain at all and that worried me.” (line 10):
9) OCD1P4:(1)
| 1 | Doctor: | Now what I uh understand is you have had some intensive abdominal | |
| 2 | → | pains uh and problems that led to (being off) work last fall. | |
| 3 | Patient: | → | Well not- not- not pain. I just, it’s- to start with uh (.) I was in the gym |
| 4 | and then I went to the toilet. | ||
| 5 | Doctor: | Um hm. | |
| 6 | Patient: | And I saw some blood. | |
| 7 | Doctor: | And you saw some blood. | |
| 8 | Patient: | → | No pain. |
| 9 | Doctor: | Uh huh. | |
| 10 | Patient: | → | No pain at all and that worried me. |
| 11 | Doctor: | → | Okay so [no pain.] |
| 12 | Patient: | → | [(Right, )] no pain, zero pain. I- I- the person that I talked to, I |
| 13 | → | didn’t tell her any pain. | |
| 14 | Doctor: | Okay. | |
| 15 | Patient: | And then uh (.) I went to see the doctor and she- and he recommended a | |
| 16 | colon endoscopy. | ||
| 17 | Doctor: | Uh huh. |
Worry is an emotion that can be experienced by patients, with and without the presence of pain, further highlighting the complexity of pain as an interactional phenomenon. An empathic opportunity (Suchman, Marakis, Beckman, & Frankel, 1997) about patient’s emotional concerns and worry is passed by with doctor’s “Okay so [no pain.]” (line 11), which is further reiterated by patient (lines 12-13). Even in the absence of pain patients can experience trauma triggered by other symptoms (e.g., blood in stools), and those worries can be addressed by doctors who recognize just how troublesome such experiences might be.
Discussion
Pain is primal for the human social condition and experienced throughout all persons’ life spans. Given the prevalence of pain, research has suggested that patients frequently raise pain during clinical encounters as a significant complaint when facing diverse maladies. Yet for this study focusing on communication about cancer during oncology interviews, it is curious that out of 146 initially identified references to pain (and related terms) only 27 instances were identified that were patient-initiated actions. There is a noticeable absence of ‘pain talk’ raised by cancer patients for their doctors’ hearing, consideration, and response. And for the 9/27 moments analyzed herein, pain actions initiated by patients received little more than minimal acknowledgments from doctors. Patients’ reported or current pain expressions did not receive a range of affiliative responses (e.g., requests for elaboration, sensitive understandings, appreciation, reassurance, empathy, sympathy, compassion). This pattern holds across environments whether patients reported past (and often dramatic) pain experiences, described current pain as minimal, or raised pain events when elaborating on doctors’ questions.
These findings strongly confirm prior research on the interactional organization of pain expressions during general consultations and primary care. Further empirical support is provided for interactional asymmetries enacted through the recurrent tendency of doctors not to actively align with patients’ lifeworld disclosures. In the midst of giving basic priorities to diagnostic pursuits of medical agenda, doctors acknowledge patients’ pain expressions and thus do not overlook them entirely. But it is also evident that doctors treat patients’ varied pain expressions as subordinate concerns not meriting further discussion. Personalized attention is not designed to more fully align with or assuage patients’ problems, nor to explicitly partner with them to elevate comfort over pain. Given the highly personal knowledge available to patients about their pain experiences, it is also apparent that very few opportunities are pursued in contexts where interview protocols constrain patients’ timing and detailing of these events in appropriate affective ways. In addition, when patients orient to doctors as witnesses to their disclosures, and display being wary of encroaching upon doctors’ medical authority, the expression of suffering is minimized as are active solicitations of responses to altogether human problems.
Unique opportunities exist to translate these research findings into innovative and impactful interventions for medical education. Poor communication has been described as one of the most significant barriers to effective pain management (Yates et al., 2002). Alternatively, doctors trained broadly in effective communication are able to increase treatment adherence in patients during pain management of fibromyalgia (Butow & Sharpe, 2013). Patients express that the best practice approaches for effectively managing pain include communication that improves information exchange, encourages active participation, improves the relationship between patient and provider, and addresses fears regarding pain management (Kimberlin et al., 2004).
Addressing pains and discomfort are essential for quality medical care, and doctors could benefit by better understanding how and why patients raise pain expressions, the tendency for doctors to not attend directly to patients’ pain disclosures when pursuing diagnostic medical agendas, and the need to improve communication skills throughout medical interviewing whenever patients make available their emotions as diagnosis and treatment evolve. During workshops digitized audio and video clips, with transcriptions, could be made available when inviting doctors to participate in analyzing similar pain patterns across different medical circumstances and diverse clinical encounters. Best and less effective practices for managing and responding to pain expressions could be identified, and doctors could be encouraged to practice selected practices during routine oncology interviews. These encounters could also be video recorded and examined for review by doctors, other medical staff, and researchers. Over time, doctors receiving communication skills training could be compared with others who have not undergone interactional workshops, and multi-methodological comparisons could be utilized to assess outcomes on critically important matters such as patient and communication satisfaction, perceived compassion, compliance, and sustained healing. Additional and ongoing research collaborations could foster constructive and interdisciplinary team approaches to improving how pain gets raised and responded to during oncology interviews.
The basic importance of analyzing the detailed organization of naturally occurring interactions would become self-evident as attempts are made to improve communication during cancer care. This analysis has repeatedly shown that pain is not just experienced individually, and internally, but made available through talk and embodied actions (e.g., gesture, touch, facial grimaces, eye gaze). Although non-vocal behaviors have not been examined directly in this investigation, considerable potential exists to extend previous research on “demonstrable suffering” (Heath, 1989, 2002; McArthur, 2018) into what has recently been described as behaviors displayed when “making cancer visible” (Beach, in press a, b). Attending closely to how pain gets interactionally constructed, and responded to, creates a visual tapestry that transforms patients’ experienced (e.g., somatic, neuropathic, visceral) pain sensations into communicative behaviors as social actions revealing key indicators such as pain location and intensity. Importantly, as this analysis has also made clear, pain itself also needs to be understood not as single or isolated events, but as constructed in dynamic ways through an array of upgrades, downgrades, and even neutralizing efforts initiated by patients to inform doctors of their conditions. Pain is also situated in other courses of action, such as attempts by patients to show that they are doctorable and, at times, working to justify their wellness by minimizing their pain reports and demonstrations. Drawing attention to these complex, and often sensitive interactional environments, contributes in substantive ways to merging communication pain research with sustained efforts to enhance more personalized clinical practices.
Contributor Information
Chelsea R. Chapman, UCSD School of Medicine, Department of Family and Preventive Medicine, SDSU Graduate School of Public Health.
Wayne A. Beach, School of Communication, Center for Communication, Health, & the Public Good, SDSU/UCSD Joint Doctoral Program in Public Health, San Diego State University, Department of Surgery, Moores Cancer Center, University of California, San Diego.
References
- Baeyer CL, Piira T, Chambers CT, Trapanotto M, & Zeltzer LK (2005). Guidelines for the cold pressor task as an experimental pain stimulus for use with children. The Journal of Pain, 6, 218–227. [DOI] [PubMed] [Google Scholar]
- Bair MJ, Robinson RL, Katon W, & Kroenke K (2003). Depression and pain comorbidity: a literature review. Archives of Internal Medicine, 163, 2433–2445. [DOI] [PubMed] [Google Scholar]
- Bauman L, Cameron L, Zimmermarn R, & Leventhal H (1989). Illness representations and matching labels with symptoms. Health Psychology, 8, 449–469. [DOI] [PubMed] [Google Scholar]
- Beach WA (1993). Transitional regularities for ‘casual’ “Okay” usages. Journal of Pragmatics, 19, 325–352. [Google Scholar]
- Beach WA (2001). Lay diagnosis [Special issue]. Text, 21, 213–268. [Google Scholar]
- Beach WA (2013a). Conversation analysis and communication In Sidnell J & Stivers T (Eds.), Handbook of conversation analysis (pp. 674–687). Cambridge, England: Blackwell-Wiley. [Google Scholar]
- Beach WA (2013b). Handbook of patient-provider interactions: Raising and responding to concerns about health, illness, and disease. New York, NY: Hampton Press. [Google Scholar]
- Beach WA (2013c). Patients’ efforts to justify wellness in a comprehensive cancer clinic Health Communication, 28, 577–591. [DOI] [PubMed] [Google Scholar]
- Beach WA (2014). Managing hopeful moments: Initiating and responding to delicate concerns about illness and health In Hamilton HE & Chou WS (Eds.), Handbook of language and health communication (459–476). Routledge. [Google Scholar]
- Beach WA & Dozier D (2015). Fears, uncertainties, and hopes: Patient-initiated actions and doctors’ responses during oncology interviews. Journal of Health Communication, 20, 1243–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach WA, Easter DW, Good JS, & Pigeron E (2005). Disclosing and responding to cancer “fears” during oncology interviews. Social Science & Medicine, 60, 893–910. [DOI] [PubMed] [Google Scholar]
- Beach WA (2015). Doctor-patient interaction In Tracy K (Ed.), Encyclopedia of Language and Social Interaction (pp.476–493). John Wiley & Sons, Inc. [Google Scholar]
- Beach WA, Gutzmer K, & Chapman CR (2017). Conversation analysis and medicine In Nussbaum J & Robinson JD (Eds.), International encyclopedia of communication. New York, NY: Oxford University Press. [Google Scholar]
- Beach WA, & Metzger TR (1997). Claiming insufficient knowledge. Human Communication Research, 23, 562–588. [Google Scholar]
- Beach WA, & Prickett E (2016). Laughter, humor, and cancer: Delicate moments and poignant interactional circumstances. Health Communication, 32, 791–802. [DOI] [PubMed] [Google Scholar]
- Beach WA (in press, a). Making cancer visible: Unmasking patients’ subjective experiences. Health Communication. 10.1080/10410236.2018.1536941 [DOI] [PubMed]
- Beach WA (in press, b). “tiny tiny little nothings”: Minimization and reassurance in the face of cancer. Health Communication. 10.1080/10410236.2018.1536945 [DOI] [PubMed]
- Bresler DE (1979). Free yourself from pain. New York, NY: Simon and Schuster. [Google Scholar]
- Butow P, & Sharpe LJP (2013). The impact of communication on adherence in pain management. Pain, 154, S101–S107. [DOI] [PubMed] [Google Scholar]
- Byrne PS & Long BE (1976). Doctors talking to patients. Psychological Medicine, 7, 735–742. [Google Scholar]
- DeWall C, & Baumeister R (2006). Alone but feeling no pain: Effects of social exclusion on physical pain tolerance and pain threshold, affective forecasting, and interpersonal empathy. Journal of Personality and Social Psychology, 91, 1–15. [DOI] [PubMed] [Google Scholar]
- Drew P (2013). The voice of the patient: Non-alignment between patient and doctors in the consultation In Beach W (Ed.), Handbook of patient-provider interactions: Raising and responding to concerns about health, illness, and disease (299–306). New York, NY: Hampton Press. [Google Scholar]
- Drew P & Heritage J (1992). Analyzing talk at work: An introduction In Drew P and Heritage J (Eds.), Talk at work: Interaction in institutional settings (pp. 3–65). Cambridge, England: Cambridge University Press. [Google Scholar]
- Epstein RM, Street RL Jr. (2007). Patient-centered communication in cancer care: Promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07–6225; Bethesda, MD, [Google Scholar]
- Gallagher R, & Verma S (1999). Managing pain and comorbid depression: A public health challenge. Paper presented at the Seminars in Clinical Neuropsychiatry. [DOI] [PubMed] [Google Scholar]
- Gardner R (1997). The conversation object mm: A weak and variable acknowledging token. Research on Language and Social Interaction, 30, 131–156. [Google Scholar]
- Gaskin DJ, & Richard P (2012). The economic costs of pain in the United States. The Journal of Pain, 13, 715–724. [DOI] [PubMed] [Google Scholar]
- Gill VT (1998). Doing attributions in medical interaction: Patients’ explanations for illness and doctors’ responses. Social Psychology Quarterly, 61, 342–360. [Google Scholar]
- Gill VT, Halkowski T, & Roberts F (2001). Accomplishing a request without making one: A single case analysis of a primary care visit. Text, 21, 55–82. [Google Scholar]
- Goffman E (1961). Encounters. Indianapolis, IN: Bobbs-Merrill. [Google Scholar]
- Goldstein I (1980). Why people prefer pleasure to pain. Philosophy, 55, 349–362. [Google Scholar]
- Goldstein I (1989). Pleasure and pain: Unconditional, intrinsic values. Philosophy and Phenomenological Research, 1, 255–276. [Google Scholar]
- Gupta A (2015). The importance of good communication in treating patients’ pain. AMA journal of Ethics, 17, 265–267. [DOI] [PubMed] [Google Scholar]
- Gutzmer K, & Beach WA (2015). “Having an ovary this big is not normal”: Physicians’ use of normal to assess wellness and sickness during oncology interviews. Health Communication, 30, 8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath C (1989). Pain talk: The expression of suffering in the medical consultation. Social Psychology Quarterly, 52, 113–125. [Google Scholar]
- Heath C (2002). Demonstrative suffering: The gestural (re) embodiment of symptoms. Journal of Communication, 52, 597–616. [Google Scholar]
- Hepburn A (2004). Crying: Notes on description, transcription, and interaction. Research on Language and Social Interaction, 37, 251–290. [Google Scholar]
- Hepburn A, & Potter J (2007). Crying receipts: Time, empathy, and institutional practice. Research on Language and Social Interaction, 40, 89–116. [Google Scholar]
- Hepburn A, & Potter J (2012). Crying and crying responses In Peräkylä A & Sorjonen ML, (Eds.), Emotion in interaction (pp.195–211). Oxford, England: Oxford University Press. [Google Scholar]
- Heritage J (1984). A change-of-state token and aspects of its sequential placement In Atkinson JM & Heritage J (Eds.), Structures of social action: Studies in conversation analysis (pp. 299–345). Cambridge, England: Cambridge University Press. [Google Scholar]
- Heritage J (2002). Oh-prefaced responses to assessments: A method of modifying agreement/disagreement In Ford CE, Fox B, & Thompson S (Eds.), The language of turn and sequence (pp. 196–234). Oxford, England: Oxford University Press. [Google Scholar]
- Heritage J (2005). Revisiting authority in physician-patient interaction In Duchan JF & Kovarsky D (Eds.), Diagnosis as cultural practice (pp. 83–102). New York: Mouton De Gruyter. [Google Scholar]
- Heritage J, & Atkinson JM (1984). Introduction In Heritage J & Atkinson JM (Eds.), Structures of social action: Studies in conversation analysis (pp. 1–27). Cambridge, England: Cambridge University Press. [Google Scholar]
- Heritage J, & Maynard DW (2006). Problems and prospects in the study of physician-patient interaction: 30 Years of research. Annual Review of Sociology, 32, 351–374. [Google Scholar]
- Heritage J & Robinson JD (2006). Accounting for the visit: Giving reasons for seeking medical care In Heritage J & Maynard DW (Eds.), Communication in medical care: Interaction between primary care physicians and patients (pp. 45–85). Cambridge, England: Cambridge University Press. [Google Scholar]
- Institute of Medicine Committee on Advancing Pain Research, C., & Education. (2011). The National Academies Collection: Reports funded by National Institutes of Health In Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US) [PubMed] [Google Scholar]
- Jefferson G (1988). On the sequential organization of troubles-talk in ordinary conversation. Social Problems, 35, 418–441. [Google Scholar]
- Jefferson G (1990). List construction as a task and resource In Psathas G (Ed.), Interaction competence (pp. 63–92). London, England: International Institute for Ethnomethodology and Conversation Analysis & University Press of America. [Google Scholar]
- Kam K (2011, February 18). Is your pain acute or chronic. Retrieved from http://www.webmd.com/pain-management/features/types-pain?page=1
- Kitzinger C (2013). Repair In Sidnell J & Stivers T (Eds.), The handbook of conversation analysis (pp. 229–256). West Sussex, United Kingdom: Blackwell Publishing. [Google Scholar]
- Kimberlin C, Brushwood D, Allen W, Radson E, & Wilson D (2004). Cancer patient and caregiver experiences: communication and pain management issues. Journal of Pain and Symptom Management, 28, 566–578. [DOI] [PubMed] [Google Scholar]
- Koskinen C, Aho S, & Nyholm L (2016). Life with an unwelcome guest–caring in a context of protracted bodily pain. Scandinavian Journal of Caring Sciences, 30, 774–781. [DOI] [PubMed] [Google Scholar]
- Maynard DW, & Heritage J (2005). Conversation analysis, doctor–patient interaction and medical communication. Medical Education, 39, 428–435. [DOI] [PubMed] [Google Scholar]
- Mochizuki H, Sadato N, Saito DN, Toyoda H, Tashiro M, Okamura N, & Yanai K (2007). Neural correlates of perceptual difference between itching and pain: A human fMRI study. Neuroimage, 36, 706–717. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. NIH launches HEAL Initiative, doubles funding to accelerate scientific solutions to stem national opioid epidemic [news release]. April 4, 2018. Accessed April 4, 2018. [Google Scholar]
- Outcalt SD, Kroenke K, Krebs EE, Chumbler NR, Wu J, Yu Z, & Bair MJ (2015). Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. Journal of Behavioral Medicine, 38, 535–543. [DOI] [PubMed] [Google Scholar]
- Ovayolu Ö, Ovayolu N, Aytaç S, Serçe S, & Sevinc A (2015). Pain in cancer patients: pain assessment by patients and family caregivers and problems experienced by caregivers. Supportive Care in Cancer, 23, 1857–1864. [DOI] [PubMed] [Google Scholar]
- Peräkylä A (1997). Conversation analysis: A new model of research in doctor-patient communication. Journal of the Royal Society of Medicine, 90, 205–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peräkylä A (1998). Authority and accountability: The delivery of diagnosis in primary health care. Social Psychology Quarterly, 6, 301–320. [Google Scholar]
- Peräkylä A (2002). Agency and authority: Extended responses to diagnostic statements in primary care encounters. Research on Language and Social Interaction, 35, 219–247. [Google Scholar]
- Petty NJ, & Moore AP (1998). Neuromusculoskeletal examination and assessment: A handbook for therapists. London, United Kingdom: Churchill-Livingstone. [Google Scholar]
- Pomerantz AM (1984). Giving a source or basis: The practice in conversation of telling ‘how I know’. Journal of Pragmatics, 8, 607–625. [Google Scholar]
- Pomerantz A (1986). Extreme case formulations: A way of legitimizing claims. Human Studies, 9, 219–229. [Google Scholar]
- Potter VT, Wiseman CE, Dunn SM, & Boyle FM (2003). Patient barriers to optimal cancer pain control. Psycho‐Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer, 12, 153–160. [DOI] [PubMed] [Google Scholar]
- Raymond G (2003). Grammar and social organization: Yes/no interrogatives and the structure of responding. American Sociological Review, 14, 939–967. [Google Scholar]
- Raymond G (2006). Questions at work: Yes/no type interrogatives in institutional contexts In Drew P, Raymond G, & Weinberg D (Eds.), Talk and interaction in social research methods (pp. 115–134). London, United Kingdom: Sage. [Google Scholar]
- Robinson JD (2001). Asymmetry in action: Sequential resources in the negotiation of a prescription request. Text, 21, 19–54. [Google Scholar]
- Robinson JD (2003). An interactional structure of medical activities during acute visits and its implications for patients’ participation. Health Communication, 15, 27–57. [DOI] [PubMed] [Google Scholar]
- Ruusuvuori J (2005). “Empathy” and “sympathy” in action. Social Psychology Quarterly, 68, 204–222. [Google Scholar]
- Schegloff EA (1989). Harvey Sacks—Lectures 1964–1965 an introduction/memoir In Harvey Sacks Lectures 1964–1965 (pp. 3–27). Dordrecht, Netherlands: Springer Netherlands. [Google Scholar]
- Schegloff EA (1996). Confirming allusions: Toward an empirical account of action. American Journal of Sociology, 102, 161–216. [Google Scholar]
- Schegloff EA, Jefferson G, & Sacks H (1977). The preference for self-correction in the organization of repair in conversation. Language, 53, 361–382. [Google Scholar]
- Schott GD (2004). Communicating the experience of pain: The role of analogy. Pain, 108, 209–212. [DOI] [PubMed] [Google Scholar]
- Sidnell J, & Stivers T (Eds.). (2013).Handbook of conversation analysis. Cambridge, England: Blackwell-Wiley. [Google Scholar]
- Smith BH, Elliott AM, Chambers WA, Smith WC, Hannaford PC, & Penny K (2001). The impact of chronic pain in the community. Family Practice, 18, 292–299. [DOI] [PubMed] [Google Scholar]
- Stivers T & Heritage J (2001). Breaking the sequential mold: Answering ‘more than the question’ during comprehensive history taking. Text, 21, 151–186. [Google Scholar]
- Stivers T, Heritage J, Barnes R, McCabe R, Thompson L, & Toerien M (2018). Treatment recommendations as actions. Health Communication, 33, 1335–1344. [DOI] [PubMed] [Google Scholar]
- Street RL Jr, Slee C, Kalauokalani DK, Dean DE, Tancredi DJ, & Kravitz RL (2010). Improving physician–patient communication about cancer pain with a tailored education-coaching intervention. Patient Education and Counseling, 80, 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman AL, Markakis K, Beckman HB, & Frankel R (1997). A model of empathetic communication in the medical interview. Journal of the American Medical Association, 277, 678–682. [PubMed] [Google Scholar]
- Tate A (2018). Treatment recommendations in oncology visits: Implications for patient agency and physician authority. Health Communication. 10.1080/10410236.2018.1514683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ten Have PT (2001). Lay diagnosis in interaction. Text, 21, 251–260. [Google Scholar]
- Wong J (2000). Repetition in conversation: A look at “first and second sayings”. Research on Language and Social Interaction, 33, 407–424. [Google Scholar]
- Woodrow KM, Friedman GD, Siegelaub AB, & Collen MF (1972). Pain tolerance: differences according to age, sex and race. Psychosomatic Medicine, 34, 548–556. [DOI] [PubMed] [Google Scholar]
- Yates PM, Edwards HE, Nash RE, Walsh AM, Fentiman BJ, Skerman HM, & Najman JM (2002). Barriers to effective cancer pain management: A survey of hospitalized cancer patients in Australia. Journal of Pain and Symptom Management, 23, 393–405. [DOI] [PubMed] [Google Scholar]


