Abstract
STUDY QUESTION
Is Ongoing Pregnancy Rate (OPR) operator-dependent, and can experience improve embryo transfer efficiency?
SUMMARY ANSWER
OPR is influenced by the operators who perform the embryo transfer (ET), and experience does not assure proficiency for everyone.
WHAT IS KNOWN ALREADY
ET remains the critical step in assisted reproduction. Although many other factors such as embryo quality and uterine receptivity impact embryo implantation, the proper ET technique is clearly an operator-dependent variable and as such it should be objectively standardized.
STUDY DESIGN, SIZE, DURATION
Retrospective comparative analysis including all fresh ETs performed between January 1996 and December 2016 at the Humanitas Fertility Center after IVF—ICSI cycles.
PARTICIPANTS/MATERIALS, SETTING, METHODS
IVF/ICSI fresh ETs performed by 32 operators, 19 824 cycles in all, were analyzed. All transfers consisting of freehand insertion of a preloaded soft catheter into the uterine cavity under transabdominal ultrasound guidance were considered. Two different statistical analyses were performed. First, a logistic regression model with a random intercept for the operator was used to estimate the heterogeneity of the rate of success among operators, accounting for woman age, FSH, number of oocytes retrieved, fertilization rate, year of the procedure, number and stage of transferred embryos and operator’s experience. Second, the relationship between experience and pregnancy rate was estimated separately for each operator by logistic regression, and operator-specific results were combined and compared in a random-effects meta-analysis. In both analyses, the operator’s experience at time t was measured in terms of number of embryo transfers performed before t.
MAIN RESULTS AND THE ROLE OF CHANCE
The heterogeneity among operators was highly significant (P value <0.001) and explained 44.5% of the total variability. The odds ratio of success of the worst operator in respect to the mean was equal to 0.84. For the best operator, the odds ratio of success was equal to 1.13 in respect to the mean. Based on the meta-analysis of the relationship between operator’s experience and success rate, it resulted that, on average, the operators’ performance did not improve with additional transfers.
LIMITATIONS, REASONS FOR CAUTION
At our center, operators become independent for ET’s after performing between 30 and 50 transfers under supervision. It is also possible that other relevant factors, such as embryologists on duty for the ET, have not been included in the present analysis and this may represent a potential bias. Among these, it should be mentioned that the embryologists on duty for the ET were not taken into consideration.
WIDER IMPLICATIONS OF THE FINDINGS
Continued performance analysis and the use of a digital simulator could help operators to test their expertise over time and either correct poor performance or avoid doing transfers.
STUDY FUNDING/COMPETING INTEREST(S)
None.
TRIAL REGISTRATION NUMBER
Keywords: operator, embryo transfer, learning curve, experience, IVF success rate
Introduction
Most patients undergoing IVF or ICSI reach embryo transfer (ET), but less than half achieve pregnancy and live birth. Despite several improvements in ovulation stimulation protocols, embryo culture media and laboratory procedures, ET remains an important and limiting step for the success of ART. Although many other factors such as embryo quality and uterine receptivity impact embryo implantation, the proper ET technique is clearly an operator-dependent crucial variable (Karande et al., 1999; Hearns-Stokes et al., 2000; Yao et al., 2009) and as such it should be objectively standardized.
The study aim was 2-fold: firstly, to analyze the impact of individual operator, independent of all confounding factors including surgeon’s experience, on cycle success rate, defined as Ongoing Pregnancy Rate (OPR), and secondly, to assess whether operators improve their performance as their experience increases.
Materials and Methods
Study population
This is a retrospective comparative analysis including all fresh ETs performed between January 1996 and December 2016 at the Humanitas Fertility Center after IVF-ICSI cycles.
All data were collected using exclusively an internal web-based database. Such database allows storing, organizing and easily retrieving information on each patient. It also manages the entire cycle of patient care processes, from outpatient services to follow-up treatments, and includes tracking all details of any surgery or hospitalization. Patients’ data protection is safeguarded by an advanced threat prevention, enterprise-class encryption, and authentication procedures for each user with periodical need for password renewal. Patients signed an informed consent allowing the use of their medical records for research purposes, provided that their anonymity was protected. The study qualified for expedited review and approval by the Humanitas Center Institutional Review Board (IRB). The study protocol was registered in ClinicalTrials.gov prior to variables extraction and statistical analysis.
Only ETs performed by the operator on duty that day (‘Gynecologist of the Day’) were included. We excluded all the cycles in which patients asked for a specific private practitioner. A similar yet larger database was used for a previous research (Levi-Setti et al., 2018).
Any operator who performed less than 20 fresh embryo transfers was excluded from the analysis. Operators with previous experience in other institutions were asked to report the number of transfers performed before entering the study and such number was considered as their entry threshold. Since it is possible that the operators improve during their training period and that by the time they begin to work independently they are already quite experienced, we opted for including even the 30–50 supervised ETs done during training in each operator’s experience in order to better assess their learning curve.
A total of 32 operators were eligible to participate in the study.
In Italy, only medical doctors already specialized in Obstetrics and Gynecology or senior residents, i.e. residents attending the fourth or the fifth year of their educational program in Obstetrics and Gynecology are allowed to perform embryo transfers after a proper training and after at least 50 IUI (intrauterine insemination) procedures. The length of such training period and the goals that must be achieved by each operator are judged by senior attending staff of the Fertility Center and candidates do not have to pass an exam or to get a specific certification. Since 2015, Humanitas Fertility Center has become part of the subspecialist training program in Reproductive Medicine accredited by the European Society of Human Reproduction and Embryology (ESHRE) that provides a tailored 3-year period of fellowship, so that every trainee must perform at least a certain number of procedures to pass to the following year and to graduate.
As a standardized ET technique, we considered all transfers consisting in freehand insertion of a preloaded soft catheter into the uterine cavity under transabdominal ultrasound (US) guidance. No mock transfer was carried out routinely before the actual ET. Most patients had either a hysteroscopy or a sonohysterogram performed before starting the IVF treatment, and all had a transvaginal US to record the length and position of the cervical canal and of the endometrial cavity (Frankfurter et al., 2003).
The ETs were performed either at the cleavage or at the blastocyst stage.
On the day of ET, patients were asked to have a full bladder to facilitate transabdominal US view of the uterine cavity; none of the transfers required anesthesia or analgesia.
In preparation for the ET, the physician cleansed the vagina and external ostium with 100 mL of sterile warm water using sterile gauzes and removed the cervical mucus using warmed sterile cotton swabs as needed. The outer guide catheter was molded prior to insertion according to the angle between the cervix and the uterine cavity (Sallam et al., 2002), and then the inner catheter cannula with the loaded embryos was inserted until it passed through the internal cervical OS.
The vast majority of procedures (94.97%) was performed with a Cook K-Soft-5000 (Cook Medical, Limerick, Ireland), although no differences were found in a previous study comparing different soft catheters (Levi Setti et al., 2003). This catheter system consists of an outer firm and an inner soft catheter. The outer guiding catheter is straight and made of flexible material, while the inner catheter is made of soft and flexible polyurethane. The standardized ET technique with this catheter consisted in straightforward advancement of the preloaded inner catheter through the cervix, the internal OS and the uterine cavity up to the site of embryo release, about 1 to 1.5 cm from the uterine fundus under US visualization. The operator then gently released the embryos from the catheter (van Weering et al., 2005).
If the standard preload technique using the Cook catheter failed, the operator could opt for using an inner stiffer guide or a stiffer hard catheter (Wallace Catheter, Cooper Surgical, Målov, Denmark) with or without the use of a tenaculum.
A stiffer catheter was used in 737 procedures (3.72% of the entire sample), as for first or second choice.
Variable definition
The OPR was considered as the primary outcome and defined as the number of viable pregnancies that had completed at least 12 weeks of gestation divided by the total number of transfers.
We chose OPR as primary outcome because it is less prone to bias as compared to live birth rate (LBR) which is more influenced by individual patient history and obstetric risks. We opted for OPR as main outcome also because it is potentially less influenced by losses to follow-up and late pregnancy complications which are surely not related to the transfer, but to higher individual obstetrical risk. However, it should be noticed that OPR, as shown in Table I, differs from LBR only in 3.21% of cases; thus, OPR and LBR can be considered largely overlapping.
Table I. Characteristic of all cycles and their outcomes.
| Variable | All |
|---|---|
| Number | 19 824 |
| Female age (years) | 36.30 ± 4.00 |
| Male age (years) | 38.08 ± 7.66 |
| Female BMI (kg/m 2 ) | 22.26 ± 3.33 |
| Active smoking | 4430 (22.35%) |
| Basal FSH (mUI/mL) | 7.57 ± 2.89 |
| Oocytes retrieved (n) | 9.60 ± 5.51 |
| Fertilization rate (%) | 73.58 ± 23.80 |
| Embryos transferred (n) | 2.25 ± 0.73 |
| 1 | 2798 (14.11%) |
| 2 | 9741 (49.14%) |
| 3 | 6736 (33.98%) |
| >3 | 549 (2.77%) |
| Stage of transfer | |
| Cleavage stage | 18 947 (95.58%) |
| Blastocyst stage | 877 (4.42%) |
| Pregnancy rate (PR) | 5334 (26.91%) |
| Miscarriage (before 12 weeks) | 981 (18.39%) |
| Ectopic pregnancy | 118 (2.21%) |
| Ongoing pregnancy rate (OPR) | 4235 (21.36%) |
| Miscarriage (after 12 weeks) | 77 (1.82%) |
| Therapeutic abortion | 59 (1.39%) |
| Births | 4099 (96.79%) |
Data are mean ± SD or number (percentage).
The operator’s experience was assessed in terms of number of previous interventions performed prior to the day of ET. In addition, for each ET the following variables, which are considered as possible determinants of pregnancy, were collected: age of the woman, follicle-stimulating hormone (FSH) value, number of oocytes retrieved, fertilization rate, time factor defined as the year of the procedure and number and stage of transferred embryos (cleavage or blastocyst stage).
Statistical analysis
We performed two different analyses to answer two different research questions: did the performance differ among operators? Did the operator’s experience influence his/her performance?
To answer the first question, a logistic regression model with a random intercept for the surgeon was specified on the indicator of success of each single intervention (ongoing pregnancy = 1, no ongoing pregnancy = 0). Introducing the random intercept, we accounted for the heterogeneity among surgeons: in the presence of strong heterogeneity among operators, we could conclude that the ET was an operator-dependent procedure.
We built such model to correct for potential confounders, so that the heterogeneity was estimated ceteris paribus, i.e. as the relevant variables potentially related to OPR were fixed. We included in the model ovarian reserve, woman age and the response to stimulation in terms of number of retrieved oocytes and fertilization rate. We did not include in the model the seminal test values due to their high heterogeneity.
The model accounted also for the year in which the procedure was performed for two main reasons: during a 20-year study, laboratory and medical techniques have greatly improved, and on the other hand, important legislative changes have occurred in our country in terms of ART (Levi Setti et al., 2013, Levi Setti et al., 2008). In Italy, from 2004 to 2009 fertility centers were not allowed to inseminate more than three oocytes and cryopreserve supernumerary embryos. Therefore, during that time period it was mandatory to transfer all the viable embryos per patient.
The embryo stage at transfer (cleavage vs blastocyst) and the operator’s experience, measured in terms of previously performed procedures, were also considered.
The answer to the second question, the impact of the operator’s surgical experience on the outcome, was investigated by implementing a two-step procedure. First, a logistic regression on the success indicator was carried out for each operator to estimate a linear term expressing the relationship between surgical experience, modeled as a continuous variable, and OPR. In the logistic regression, we accounted for woman age, FSH value, number of oocytes retrieved, fertilization rate, the year of the procedure and number and stage of transferred embryos.
Then the estimated slopes, one for each operator, were compared and combined in a random effect meta-analysis: each line represents, similarly to independent studies in classical meta-analysis papers, a single operator.
Data were analyzed by Stata 15.0 (2013, Stata Corp., Texas, USA).
Ethical approval
Humanitas Ethical Committee approved the study protocol on 26 June 2018, and the protocol was registered in ClinicalTrials.gov (registration number: NCT03561129).
Patients who underwent ART cycles had consented in writing that their medical records could be used for research purposes, as long as the patients’ anonymity was protected, and no other specific consent was required.
Results
During the present 20-year study, 43 operators performed embryo transfers at the Humanitas Fertility Center, 11 of whom were excluded from the dataset because they had performed less than 20 procedures or because it was not possible to quantify their previous experience. Similarly, to reduce possible bias 1037 interventions were not included in the final data set, since they were not performed by the surgeon on duty that day, but by the patient’s private doctor. During the study period, 21 patients (0.11%) were lost at follow-up and since it was not possible to define their outcome, they were excluded from the analysis.
As a result, a total of 19 824 transfers, performed by 32 operators, were included in the final analysis.
Baseline characteristic of ART cycles and their outcomes are reported in Table I.
Operators were anonymized with a unique ID. Operators 11, 16 and 23 had an entry level of more than 500 procedures, due to their previous experience in other institutions, while for the others, the initial experience in terms of ETs was 0 threshold.
Data on operators’ performance are shown in Table II: number of procedures, inclusion period, number of ongoing pregnancies and unadjusted OPR are reported for each operator.
Table II. Operators performance: number of procedures, inclusion period, number of ongoing pregnancies (OPs) and unadjusted ongoing pregnancy rate (OPR).
| Operator ID | Number of procedures | Date of entry (mm/yyyy) | Date of exit (mm/yyyy) | Number of OPs | OPR % (unadjusted) |
|---|---|---|---|---|---|
| 01 | 270 | 10/2000 | 11/2004 | 73 | 27 |
| 02 | 2996 | 3/1997 | 12/2016 | 672 | 22.4 |
| 03 | 25 | 4/2009 | 10/2010 | 4 | 16 |
| 04 | 433 | 4/2013 | 12/2016 | 107 | 24.7 |
| 05 | 58 | 4/2013 | 9/2013 | 10 | 17 |
| 06 | 344 | 9/2013 | 11/2016 | 55 | 16.0 |
| 07 | 25 | 9/2015 | 12/2015 | 2 | 8 |
| 08 | 284 | 2/2014 | 12/2016 | 53 | 18.7 |
| 09 | 417 | 1/2000 | 4/2006 | 107 | 25.7 |
| 10 | 67 | 1/2005 | 6/2006 | 12 | 18 |
| 11 | 1579 | 5/2005 | 12/2016 | 333 | 21.1 |
| 12 | 210 | 3/2005 | 5/2007 | 41 | 19.5 |
| 13 | 56 | 10/2011 | 3/2012 | 14 | 25 |
| 14 | 1852 | 10/2003 | 12/2016 | 376 | 20.3 |
| 15 | 20 | 1/2014 | 10/2015 | 3 | 15 |
| 16 | 996 | 10/1996 | 9/2016 | 221 | 22.2 |
| 17 | 1871 | 11/2000 | 7/2015 | 440 | 23.5 |
| 18 | 26 | 4/2013 | 6/2013 | 9 | 25 |
| 19 | 114 | 10/2013 | 11/2016 | 32 | 28.1 |
| 20 | 100 | 4/2011 | 1/2012 | 13 | 13.0 |
| 21 | 74 | 9/2013 | 4/2014 | 13 | 18 |
| 22 | 780 | 4/2011 | 12/2016 | 140 | 18.0 |
| 23 | 92 | 11/2015 | 12/2016 | 25 | 27 |
| 24 | 52 | 5/2007 | 10/2007 | 15 | 29 |
| 25 | 1855 | 10/1998 | 12/2016 | 394 | 21.2 |
| 26 | 155 | 10/2014 | 12/2016 | 33 | 21.3 |
| 27 | 832 | 7/2008 | 11/2016 | 135 | 16.2 |
| 28 | 162 | 9/2012 | 9/2013 | 35 | 21.6 |
| 29 | 86 | 11/2005 | 9/2006 | 13 | 15 |
| 30 | 3367 | 11/1998 | 12/2016 | 739 | 22.0 |
| 31 | 603 | 1/2012 | 11/2016 | 112 | 18.6 |
| 32 | 23 | 8/2014 | 12/2014 | 4 | 17 |
| Total | 19 824 | 4235 | 21.36 |
In general, the 32 operators worked for a mean of 162 months, performing a mean of 620 ± 887 ETs, and their overall unadjusted OPR was 21.36%, ranging from 8 to 29%.
The results of the random-effects logistic model are reported in Table III. The likelihood ratio (LR) test for the heterogeneity among operators was highly significant (P value = 0.0098). In other terms, controlling for all the other variables that could influence the outcome, including the previous experience, the operator impacted significantly on the OPR.
Table III. Results of the logistic model with random intercept: estimated coefficients, their exponential (odds ratios), standard errors and P values.
| Variable | Coefficient | OR | OR 95% CI | P |
|---|---|---|---|---|
| Operator experience | 0.0021 | 1.0021 | 0.995–1.009 | 0.501 |
| Female age (years) | −0.1211 | 0.886 | 0.877–0.895 | <0.001 |
| Oocytes retrieved (number) | 0.0346 | 1.035 | 1.028–1.042 | <0.001 |
| Embryos transferred (number) | 0.4445 | 1.560 | 1.461–1.668 | <0.001 |
| Year of the procedure | 0.0399 | 1.041 | 1.027–1.055 | <0.001 |
| Blastocyst versus cleavage stage transfer | 0.1548 | 1.167 | 0.989–1.380 | 0.069 |
| Fertilization rate (%) | 0.7054 | 2.025 | 1.687–2.403 | <0.001 |
| Basal FSH (mUI/mL) | −0.0119 | 0.988 | 0.975–1.002 | 0. 089 |
(1)Per 100 interventions.
Table IV reports the exponential of the random intercepts estimated for each operator, from the worst to the best performer. Each value expresses, in terms of odds ratio (OR), how much the performance of the single operator deviated from the average OPR.
Table IV. Estimates of the odds ratio (OR) by operator ordered from the worst to the best performer.
| Operator ID | OR | OR 95% CI |
|---|---|---|
| 27 | 0.8626 | 0.7304–0.9677 |
| 6 | 0.9069 | 0.7549–1.0668 |
| 22 | 0.9093 | 0.7818–1.0366 |
| 31 | 0.9314 | 0.7969–1.0769 |
| 8 | 0.9444 | 0.7882–1.1237 |
| 20 | 0.9477 | 0.7710–1.1576 |
| 21 | 0.9477 | 0.7920–1.1956 |
| 7 | 0.9644 | 0.7767–1.1942 |
| 5 | 0.9670 | 0.7844–1.1895 |
| 15 | 0.9738 | 0.7846–1.2069 |
| 29 | 0.9755 | 0.7938–1.1975 |
| 10 | 0.9768 | 0.7929–1.2018 |
| 14 | 0.9779 | 0.8812–1.0842 |
| 16 | 0.9811 | 0.8624–1.1152 |
| 3 | 0.9837 | 0.7931–1.2195 |
| 32 | 0.9863 | 0.7953–1.2227 |
| 12 | 0.9950 | 0.8251–1.1998 |
| 30 | 0.9971 | 0.9209–1.0796 |
| 2 | 1.0148 | 0.9341–1.1024 |
| 13 | 1.0169 | 0.8250–1.2534 |
| 26 | 1.0204 | 0.8412–1.2378 |
| 28 | 1.0312 | 0.8509–1.2497 |
| 18 | 1.0335 | 0.8342–1.2804 |
| 25 | 1.0340 | 0.9334–1.1453 |
| 11 | 1.0342 | 0.9269–1.1538 |
| 24 | 1.0422 | 0.8453–1.2849 |
| 23 | 1.0884 | 0.8883–1.3337 |
| 9 | 1.0897 | 0.9274–1.2804 |
| 19 | 1.0984 | 0.9006–1.3396 |
| 4 | 1.1159 | 0.9512–1.3091 |
| 17 | 1.1276 | 1.0201–1.2464 |
| 1 | 1.1278 | 0.9455–1.3453 |
The OR expresses the ratio between the odds of success of the single operator and the average odds of success.
From the worst to the best operator, the OR varied between 0.84 and 1.13. This means that the odds of success of the worst operator was almost 16% lower than the mean and that the odds of success of the best one was 13% higher than the mean. This discrepancy between operators can represent an important problem within an assisted reproductive program.
From the logistic regression, the surgeon’s experience did not appear to affect her/his probability of success (Table III). To better explore this point, we thus performed a two-stage analysis, as described in the ‘Statistical analysis’ section.
The estimated slopes arising from the operator-specific logistic models, which express the relationship between operator experience and OPR, are reported in the forest plot in Figure 1. Each row (from operator 1 to operator 32) corresponds to the confidence interval of the slope for an operator, with the central dot representing the point estimate. The position of the segment with respect to the vertical line at 1.0 indicates if the outcome improved or not as the operator experience increased. Operator 15 is not shown in the graphic because in multivariable analysis, the small number of procedures performed does not allow the slope estimation.
Figure 1. Meta-analysis of the surgeon-specific slope expressing the role of the experience on the ongoing pregnancy rate (OPR). The dot position expresses the relation of the growing experience in terms of better or worse outcomes. Each line represents a single operator. OR = odds ratio; CI = confidence interval.
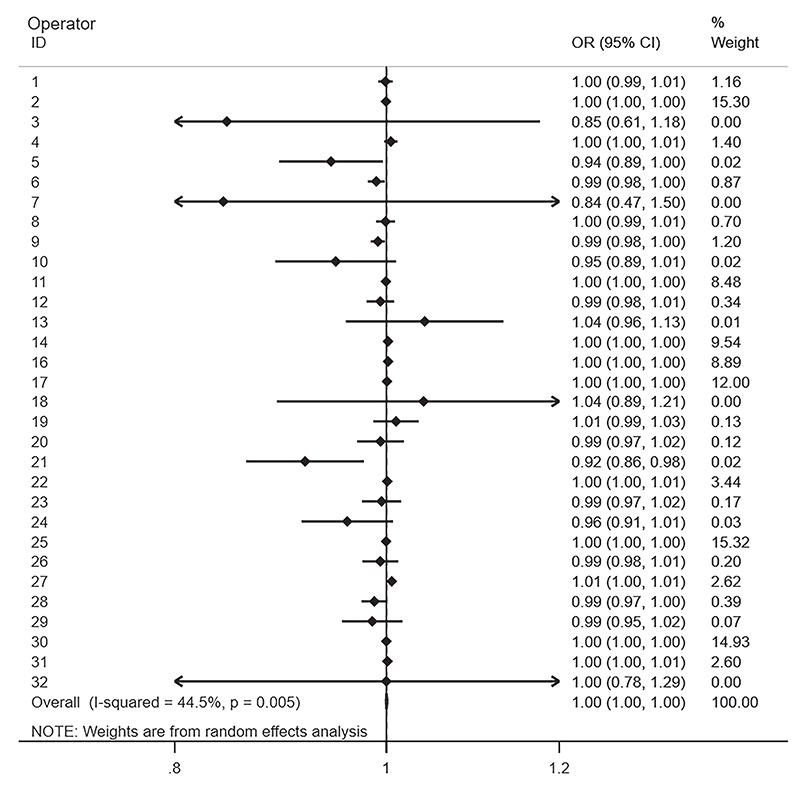
Performing a random effects meta-analysis on these operator-specific results, it appeared that the overall meta-analytic estimate, which is a weighted mean of the estimated slopes, was close to zero, with a confidence interval including the null hypothesis of no surgery experience effect (overall effect = 0.000; CI: −0.001 to 0.001). The I2 index, which measures the percentage of total variability explained by the heterogeneity among operators, was moderately high (44.5%), indicating that the effect of the surgery experience could vary among operators.
Discussion
This retrospective study shows that the operator performing embryo transfer is a crucial factor affecting the outcome of the ART cycle and, furthermore, shows that, on average, there is no significant increase in OPR as the experience of the operator (measured in terms of number of embryo transfers) increases.
The strength of the current study hinges on the completeness of the preoperative factors and follow-up and on one of the largest dataset so far reported in literature, which permitted to adjust the analysis for multiple confounders and to assess a wide range of outcomes.
Concerning possible biases and limitations, it should be noted that at our center ETs are included in the trainees’ program. An operator must perform at least 30–50 embryo transfers under supervision by an expert colleague before becoming autonomous.
It is also possible that other parameters have not been included in the present analysis, and this may represent a potential bias. Among these, it should be mentioned that the biologists on duty for the ET, were not taken into consideration. However, the biologist, unlike the gynecologist, usually has a weekly and not a daily shift, so that a single biologist usually performs all ETs during a given week. Therefore, we expect that in our data there was no relevant association between biologist of the week and gynecologist of the day.
It could also happen that a gynecologist was recurrently on shift on a specific day of the week, e.g. on Monday. This, coupled with the fact that time in which the procedure was performed, i.e. season, month, day of the week and time of the day, may have influenced the OPR, could have produced a bias in our results. However, we reasonably expect that this possible bias was negligible and not able to affect our conclusions.
Anyway, even if we used a large data set and appropriate statistical methods, due to the presence of possible residual bias related to unobserved or unknown confounders, our results should be considered with caution before any application in clinical practice.
In literature, many factors are reported to influence the pregnancy rate (PR) such as patient’s characteristics, type of catheter, i.e. soft vs firm (Abou-Setta et al., 2005; Buckett, 2006; Yao et al., 2009), number and quality of the embryos transferred (Pandian et al., 2009, Papanikolaou et al., 2009, Weitzman et al., 2010), skill of the clinician performing the ET (Dessolle et al., 2010), use of standardized embryo transfer techniques (van de Pas et al., 2003), use of ultrasound guidance during embryo transfer vs clinical touch, level of difficulty of the transfer (Tomas et al., 2002), presence of blood in the transfer catheter (Alvero et al., 2003) or presence of uterine contractions at the time of transfer (Fanchin et al., 1998; Fanchin et al., 2001).
Although PR is a more intelligible concept, it is scarcely indicative of a positive ART outcome. Considering the other two main indicators, OPR and LBR, in the present study OPR was chosen as the primary outcome since the operator may influence not only the pregnancy probability but also possible unfavorable outcomes during the first trimester, e.g. miscarriages or ectopic pregnancies. On the other hand, LBR could be potentially influenced by too many other variables.
Crucial for the outcome of a transfer is the operator ability to deposit the embryos where the chances of implantation are highest, without traumatizing the endometrium (Coroleu et al., 2002), and to avoid the induction of uterine contractions (Fanchin et al., 1998) and any iatrogenic damage to the embryos, avoiding negative pressure when removing the catheter while maintaining a controlled velocity when depressing the plunger has also been associated with successful results.
Several studies carried out so far have analyzed the correlation between operator’s ET experience and clinical PR. Until now, evidences are mixed (van Weering et al., 2005; Uyar et al., 2011) and very inconclusive largely because of insufficient sample sizes.
Beside few exceptions, such as the findings reported by van Weering et al. of no significant difference in individual PR among equally experienced gynecologists (van Weering et al., 2005), most of the published studies report large differences in OPR among physicians, with a variation from 17.0 to 54.0% (Hearns-Stokes et al., 2000) and from 13.2 to 37.4% (Karande et al., 1999).
In 2016, Morin et al. reported that, even when controlling for embryonic factors by utilizing euploid blastocyst transfers, LBR was still strongly influenced by the physician performing the ET (Morin et al., 2016). The inclusion of euploid blastocysts only reduced most of the possible biases and confounder factors, but the strength of that study was limited by the facts that the operator’s experience factor was not analyzed and that they only compared the worse and the best performer.
The observation by van de Pas et al. that the use of a fixed distance to expel embryos during the ET procedure can equalize the success rates among physicians opened a debate on the importance of a standardized technique to decrease individual variations (van de Pas et al., 2003).
To confirm the importance of the operator’s influence on ET outcome, Papageorgiou et al. studied the results of the fellows in training at their center and showed a lower success rate during their first 25 cycles and a subsequent improvement only after 50 cycles, with PRs comparable to those of experienced staff (Papageorgiou et al., 2001).
Based on similar conclusions, namely the relevance of the level of experience among operators, Karande et al. also considered the option of excluding gynecologists with lower PRs from the ET shifts (Karande et al., 1999).
On the other hand, Bjuresten et al. compared OPR from ETs performed by physicians vs midwives and found no statistically significant difference between the two groups (Bjuresten et al., 2003).
Moreover, van Weering et al. (2005) concluded that, because of the presence of many confounding variables potentially impacting the success of ET and embryo implantation, it is very difficult to identify a single relevant factor and that conclusions based on non-randomized, uncontrolled studies are highly questionable (van Weering et al., 2005).
In our study, the population of operators was very heterogeneous in terms of number of procedures, years of inclusion and unadjusted OPR (Table II), but through appropriate statistical analyses, it was possible to assess the operator’s influence on OPR, accounting for the main factors which affect the success of the ET. We found that the surgeon performing the ET significantly impacted the OPR, even after adjusting for the most relevant confounders, including experience. These findings agree with the literature that reports that the PR is influenced by the individual operator who performs the ET procedure, independently of his/her expertise. In our population, the operators from 27 to 12, as shown in Table IV, underperformed in respect to the mean, while the rest of surgeons had better odds of pregnancy.
The standard preload technique used in our Center can be affected by the operator’s manual ability since the catheter approaches directly the cervix by free hand. US guidance has always been performed throughout the study period, even prior to the NICE indications (O'Flynn, 2014).
Dual transfer technique can be a suitable alternative since it does not put into direct contact the embryo and the cervix, and possibly the outcome could be less operator-dependent.
From the meta-analysis shown in Figure 1, regarding the effect of the operator’s experience, there is no evidence of an increase in OPR depending on the number of previously performed procedures. However, this result could be interpreted with caution, because a quite large variability (44.5%) was estimated for the experience effect among the 32 operators. This could indicate that with experience the performance improves, but only for a subset of operators. It would be interesting, in future studies, to better describe this subgroup and carry out analyses, which focus on the shape of the relationship between experience and OPR to detect possible non-linearities.
In particular, it is worth noticing that some operators performed worse than the average and did not improve with experience and this result confirms the no association between success rates and number of ETs performed by provider during the study period or number of years elapsed since completion of training (Morin et al., 2016). This counterintuitive statement can be explained because ET is one of the few procedures in gynecology that is performed by a single operator on his own. After an initial training period, surgeons have scarce opportunity to compare themselves with other colleagues to avoid mistakes and correct improper maneuvers.
To improve performance and achieve proficiency, there are few options such as periodical re-training, reassessing proper standardization of the ET technique, use of the digital simulator, which could help operators to increase and confirm their own expertise over time without practicing on real patients.
However, if despite these corrective measures the OPR remains suboptimal, some operators should not be scheduled for ET procedures.
Acknowledgements
This study was the final project of the post-graduation course of Humanitas University in ‘Epidemiology for Clinical Research’ of Federico Cirillo, MD. The authors acknowledge and sincerely thank all the Humanitas Fertility Center staff for their support in conducting this study.
Authors’ roles
F.C. and P.E.L.S. were involved in the study concept and design. C.R., L.C., E.Z., A.B., F.C. and E.M. contributed to the acquisition of data. F.C. and E.M. analyzed the data. M.B. supervised the statistical analyses. P.E.L.S. and F.C. wrote the manuscript and had primary responsibility for its final content. E.M. and P.E.L.S. supervised the analysis. C.R. and L.C. contributed to bibliography updating. P.P. critically revised the manuscript and helped for data analysis. All authors read and approved the final manuscript.
Funding
No specific funding was sought for the present study.
Conflict of interest
None. All authors reported no conflict of interest regarding the present manuscript.
References
- Abou-Setta AM, Al-Inany HG, Mansour RT, Serour GI, Aboulghar MA. Soft versus firm embryo transfer catheters for assisted reproduction: a systematic review and meta-analysis. Hum Reprod 2005;20:3114–3121. [DOI] [PubMed] [Google Scholar]
- Alvero R, Hearns-Stokes RM, Catherino WH, Leondires MP, Segars JH. The presence of blood in the transfer catheter negatively influences outcome at embryo transfer. Hum Reprod 2003;18:1848–1852. [DOI] [PubMed] [Google Scholar]
- Bjuresten K, Hreinsson JG, Fridstrom M, Rosenlund B, Ek I, Hovatta O. Embryo transfer by midwife or gynecologist: a prospective randomized study. Acta Obstet Gynecol Scand 2003;82:462–466. [DOI] [PubMed] [Google Scholar]
- Buckett WM. A review and meta-analysis of prospective trials comparing different catheters used for embryo transfer. Fertil Steril 2006;85:728–734. [DOI] [PubMed] [Google Scholar]
- Coroleu B, Barri PN, Carreras O, Martinez F, Veiga A, Balasch J. The usefulness of ultrasound guidance in frozen-thawed embryo transfer: a prospective randomized clinical trial. Hum Reprod 2002;17:2885–2890. [DOI] [PubMed] [Google Scholar]
- Dessolle L, Freour T, Barriere P, Jean M, Ravel C, Darai E, Biau DJ. How soon can I be proficient in embryo transfer? Lessons from the cumulative summation test for learning curve (LC-CUSUM). Hum Reprod 2010;25:380–386. [DOI] [PubMed] [Google Scholar]
- Fanchin R, Righini C, de Ziegler D, Olivennes F, Ledee N, Frydman R. Effects of vaginal progesterone administration on uterine contractility at the time of embryo transfer. Fertil Steril 2001;75:1136–1140. [DOI] [PubMed] [Google Scholar]
- Fanchin R, Righini C, Olivennes F, Taylor S, de Ziegler D, Frydman R. Uterine contractions at the time of embryo transfer alter pregnancy rates after in-vitro fertilization. Hum Reprod 1998;13:1968–1974. [DOI] [PubMed] [Google Scholar]
- Frankfurter D, Silva CP, Mota F, Trimarchi JB, Keefe DL. The transfer point is a novel measure of embryo placement. Fertil Steril 2003;79:1416–1421. [DOI] [PubMed] [Google Scholar]
- Hearns-Stokes RM, Miller BT, Scott L, Creuss D, Chakraborty PK, Segars JH. Pregnancy rates after embryo transfer depend on the provider at embryo transfer. Fertil Steril 2000;74:80–86. [DOI] [PubMed] [Google Scholar]
- Karande VC, Morris R, Chapman C, Rinehart J, Gleicher N. Impact of the “physician factor” on pregnancy rates in a large assisted reproductive technology program: do too many cooks spoil the broth? Fertil Steril 1999;71:1001–1009. [DOI] [PubMed] [Google Scholar]
- Levi Setti PE, Albani E, Cavagna M, Bulletti C, Colombo GV, Negri L. The impact of embryo transfer on implantation--a review. Placenta 2003;24Suppl B:S20–S26. [DOI] [PubMed] [Google Scholar]
- Levi Setti PE, Albani E, Matteo M, Morenghi E, Zannoni E, Baggiani AM, Arfuso V, Patrizio P. Five years (2004-2009) of a restrictive law-regulating ART in Italy significantly reduced delivery rate: analysis of 10,706 cycles. Hum Reprod 2013;28:343–349. [DOI] [PubMed] [Google Scholar]
- Levi Setti PE, Albani E, Novara P, Cesana A, Negri L. Results of in vitro fertilization in Italy after the introduction of a new law. Fertil Steril 2008;90:1081–1086. [DOI] [PubMed] [Google Scholar]
- Levi-Setti PE, Cirillo F, Scolaro V, Morenghi E, Heilbron F, Girardello D, Zannoni E, Patrizio P. Appraisal of clinical complications after 23,827 oocyte retrievals in a large assisted reproductive technology program. Fertil Steril 2018;109:1038–1043e1031. [DOI] [PubMed] [Google Scholar]
- Morin S, Franasiak JM, Juneau CR, Scott RT. Live birth rate following embryo transfer is significantly influenced by the physician performing the transfer: data from 2707 euploid blastocyst transfers by 11 physicians. Fertil Steril 2016;e25:106. [Google Scholar]
- O'Flynn N. Assessment and treatment for people with fertility problems: NICE guideline. Br J Gen Pract 2014;64:50–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandian Z, Bhattacharya S, Ozturk O, Serour G, Templeton A. Number of embryos for transfer following in-vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database Syst Rev 2009;CD003416. [DOI] [PubMed] [Google Scholar]
- Papageorgiou TC, Hearns-Stokes RM, Leondires MP, Miller BT, Chakraborty P, Cruess D, Segars J. Training of providers in embryo transfer: what is the minimum number of transfers required for proficiency? Hum Reprod 2001;16:1415–1419. [DOI] [PubMed] [Google Scholar]
- Papanikolaou EG, Kolibianakis EM, Pozzobon C, Tank P, Tournaye H, Bourgain C, Van Steirteghem A, Devroey P. Progesterone rise on the day of human chorionic gonadotropin administration impairs pregnancy outcome in day 3 single-embryo transfer, while has no effect on day 5 single blastocyst transfer. Fertil Steril 2009;91:949–952. [DOI] [PubMed] [Google Scholar]
- Sallam HN, Agameya AF, Rahman AF, Ezzeldin F, Sallam AN. Ultrasound measurement of the uterocervical angle before embryo transfer: a prospective controlled study. Hum Reprod 2002;17:1767–1772. [DOI] [PubMed] [Google Scholar]
- Tomas C, Tikkinen K, Tuomivaara L, Tapanainen JS, Martikainen H. The degree of difficulty of embryo transfer is an independent factor for predicting pregnancy. Hum Reprod 2002;17:2632–2635. [DOI] [PubMed] [Google Scholar]
- Uyar A, Bener A, Ciray HN, Bahceci M. Physician experience in performing embryo transfers may affect outcome. Fertil Steril 2011;95:1860–1862. [DOI] [PubMed] [Google Scholar]
- van de Pas MM, Weima S, Looman CW, Broekmans FJ. The use of fixed distance embryo transfer after IVF/ICSI equalizes the success rates among physicians. Hum Reprod 2003;18:774–780. [DOI] [PubMed] [Google Scholar]
- van Weering HG, Schats R, McDonnell J, Hompes PG. Ongoing pregnancy rates in in vitro fertilization are not dependent on the physician performing the embryo transfer. Fertil Steril 2005;83:316–320. [DOI] [PubMed] [Google Scholar]
- Weitzman VN, Schnee-Riesz J, Benadiva C, Nulsen J, Siano L, Maier D. Predictive value of embryo grading for embryos with known outcomes. Fertil Steril 2010;93:658–662. [DOI] [PubMed] [Google Scholar]
- Yao Z, Vansteelandt S, Van der Elst J, Coetsier T, Dhont M, De Sutter P. The efficacy of the embryo transfer catheter in IVF and ICSI is operator-dependent: a randomized clinical trial. Hum Reprod 2009;24:880–887. [DOI] [PubMed] [Google Scholar]


