Abstract
Plantar fibromatosis (PF) is a rare benign disease. Here we report bilateral PF accompanied by Dupuytren’s contracture in the right palm. Magnetic resonance imaging was useful in diagnosing PF, although biopsy was needed to rule out hemangioma. As the patient had been receiving female hormone therapy since orchiectomy, there may be a possibility that estrogen accelerated the growth of PF. Local excision with a 1-cm margin was performed, followed by primary wound closure. Neither complication nor recurrence had occurred 6 months after the surgery.
Keywords: plantar fibromatosis, Dupuytren’s contracture, Magnetic resonance imaging, local excision, LGBT, estrogen
INTRODUCTION
Plantar fibromatosis (PF) is a rare and benign thickening of the plantar aponeurosis. The exact pathogenesis of PF remains elusive, while the development of PF has been linked to hereditary, trauma, diabetes or epilepsy [1]. Here, we treated a 50-year-old lesbian, gay, bisexual and transgender (LGBT) person with bilateral PF as well as Dupuytren’s contracture. The detailed case report is described in the next section.
CASE REPORT
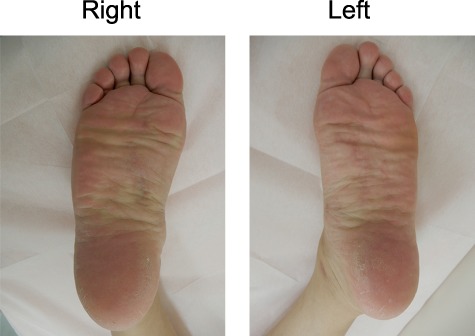
A 50-year-old male came to our department with walking difficulties because of painful bilateral plantar nodules. Visual inspection revealed solid nodules with 4 cm in diameter bilaterally in the medial plantar regions (Fig. 1a). About 15 years ago, the asymptomatic nodules were simultaneously noticed being the size of a grain of rice, although the growing nodules caused difficulties and pain with footwear. Additionally, he also had Dupuytren’s contracture in his right palm (Fig. 1b). Conversely, Doppler auscultation revealed arteriosus vascular sound on the mass in the bilateral plantar.
Figure 1.
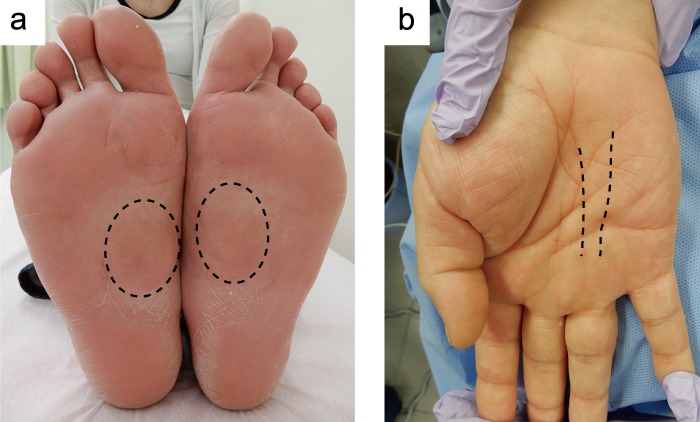
Gross appearance of the bilateral plantar (a) and the right palmar (b). Dot circles and lines indicate the mass or the thick chord.
A plain magnetic resonance imaging (MRI) scan revealed soft subcutaneous mass in the bilateral plantar with a dark signal on T1-weighted images, while a brighter signal than muscles on T2-weighted images (Fig. 2a). In turn, MR angiography visualized symmetrical mass bilaterally as a high density area (Fig. 2b). In contrast, MRI scan of his right palm showed a thick cord with a dark signal on both T1- and T2- weighted images (Fig. 3). To rule out the possibility of hemangioma, a biopsy was performed, resulting in the diagnosis that PF was strongly suspected.
Figure 2.
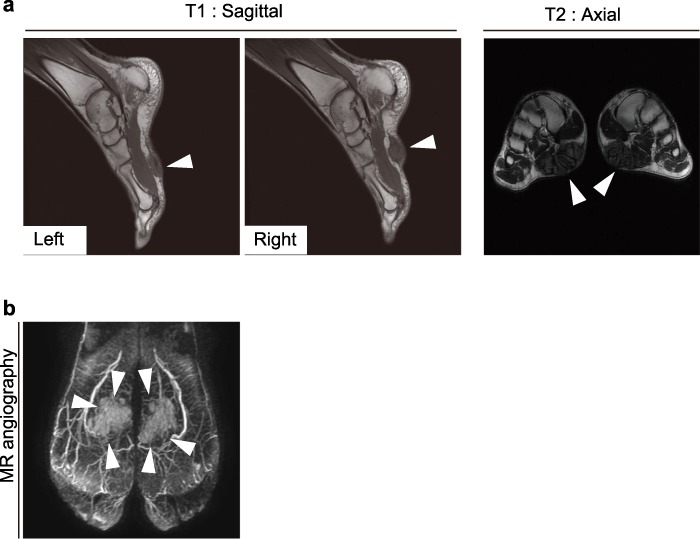
MRI (a) and MR angiographic imaging of the foot (b). White arrowheads indicate the mass.
Figure 3.
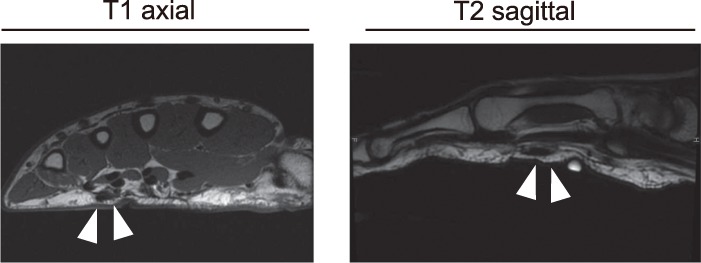
MRI images of the right palmar. White arrowheads indicate the chord.
He had neither family history of PF nor history of diabetes/epilepsy. He is a LGBT person and orchiectomy was performed 7 years ago. Instead of lost androgenic hormone, female hormone therapy had been prescribed with 1 mg of norgestrel and 0.1 mg of ethinyl estradiol per day.
Since the patient wanted surgical treatment, operation under general anesthesia was performed (Fig. 4). Skin incision enabled the observation that the medial plantar neurovascular bundles were involved in the mass in the right foot. Therefore, it was necessary to dissect the medial plantar neurovascular bundles from the mass before excising the mass en bloc with a 1 cm safety margin. In contrast, there was no such finding in the left plantar. The primary wound closure was performed and suction drains were left. The patient was instructed to prevent the operation sites from bearing weight for 2 weeks. The skin wound healed uneventfully and he was released from the hospital 15 days after his operation. The final pathological diagnosis was PF. After 6 months, the patient is free of pain and is able to wear his shoes without any trouble (Fig. 5).
Figure 4.
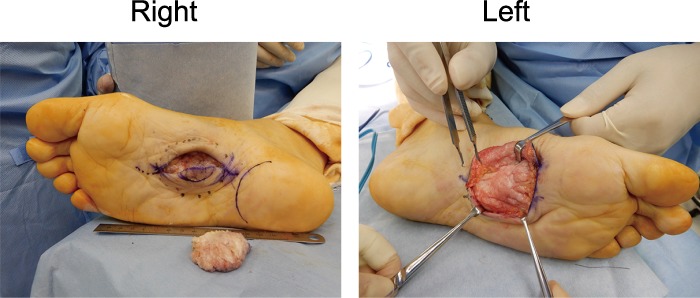
Intraoperative findings.
Figure 5.
Postoperative findings 6 months after the operation.
DISCUSSION
Three stages are described as PF progresses [1]. Namely, the first (proliferative) stage is characterized by increased fibroblasts activity and cellular proliferation, followed by the second (active) stage where nodules are formed and the third (maturation) stage where fibroblasts are replaced with the deposition of type III collagen, which resembles scar contracture. Although PF is easily diagnosed in most cases, Masadeh et al. [1] suggested that the diseases to be differentially diagnosed include rheumatoid nodule, gout, pyogenic granuloma or inclusion cyst. Conversely, malignant diseases to be differentially diagnosed are fibrous histiocytoma, giant cell tumor, synovial cell sarcoma and leiomyosarcoma [1,2]. Regularly, MRI is a useful tool in diagnosing PF with a dark signal on T1-weighted images, while a low-to-intermediate signal on T2-weighed images. Ultrasound is also useful in confirming clinical diagnosis [2].
There are conservative and surgical treatments for PF. Conservative treatments involve steroid injections or radiation. Since a single-dose injection can cause a recurrence of the mass within the several years, a protocol of intralesional steroid injections is recommended [3]. In such a case, informed consent including possible adverse effects such as fat atrophy, infection or rupture of the plantar fascia should be obtained from a patient.
Radiation therapy is frequently reported effective for PF patients with the first stage [3]. In turn, adjuvant radiotherapy after surgical treatment has been proposed to prevent recurrence [3]. However, in spite of no recurrence after adjuvant radiotherapy, it could lead to dystrophic foot with impaired foot function [4].
Antiestrogen therapy appears effective for PF, taking into account that it is effective for patients with Dupuytren’s contracture, which is histologically similar to PF [3]. It is intriguing to note that our patient recognized the mass growth in his plantar regions after starting estrogen therapy. Thus, there may be a possibility that estrogen accelerated the growth of PF in our case.
Careful observation is needed because of the high rate of recurrence after surgery [5]. Mainly, there are three methods in surgical management, which include local excision, wide excision and complete fasciectomy. The excision of mass with a 2–3 cm margin is regarded as wide excision. We avoided wide excision/total fasciectomy for the reason that wide excision including weight-bearing region could cause pain in the standing position, considering he was a chef who worked in the standing position for a long time.
In conclusion, we treated a patient with bilateral PF, which was extremely rare [2,6]. Further investigation should be needed for elucidating pathogenesis and pursuing treatments with no recurrence as well as no adverse effects.
FINANCIAL DISCLOSURES
None of the authors has a financial interest in any of the products, devices or drugs mentioned in this manuscript.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1. Masadeh SB, Lynos MC, Terol C, Manning S. PLANTAR FIBROMATOSIS: Treatment Considerations. Orthopedics 2018; Chapter 29.
- 2. Akdag O, Yildiran G, Karamese M, Tosun Z. Dupuytren-like contracture of the foot: Ledderhose disease. Surg J 2016;02:e102–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Young JR, Sternbach S, Willinger M, Hutchinson ID, Rosenbaum AJ. The etiology, evaluation, and management of plantar fibromatosis. Orthop Res Rev 2018;11:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. De Bree E, Zoetmulder FAN, Keus RB, Peterse HL, Van Coevorden F. Incidence and treatment of recurrent plantar fibromatosis by surgery and postoperative radiotherapy. Am J Surg 2004;187:33–8. [DOI] [PubMed] [Google Scholar]
- 5. Carroll P, Henshaw RM, Garwood C, Raspovic K, Kumar D. Plantar fibromatosis: pathophysiology, surgical and nonsurgical therapies: an evidence-based review. Foot Ankle Spec 2018;11:168–76. [DOI] [PubMed] [Google Scholar]
- 6. Newman C, McQuaid SE. Bilateral plantar fibromatosis. Ir Med J 2019;112:919. [PubMed] [Google Scholar]


