This randomized clinical trial examines the effect of telephonic work-focused counselling combined with integrated care vs integrated care alone among veterans with depression treated at a large Veterans Health Administration medical center.
Key Points
Question
Is a telephonic work-focused counselling program combined with the Veterans Health Administration’s mental health integrated care (IC) program superior to IC alone for improving the occupational functioning and depression symptom severity of employed veterans with depression and work limitations?
Findings
In this randomized clinical trial including 253 veterans, IC plus work-focused counseling resulted in significantly larger reductions in at-work productivity loss and depression symptom severity immediately after the intervention, and these effects were present 4 months later.
Meaning
These findings suggest that supplementing the IC program with this low-cost, work-focused intervention may help veterans with depression and work limitations achieve better occupational and clinical outcomes.
Abstract
Importance
Thousands of working-age veterans with depression experience impaired occupational functioning.
Objectives
To test whether the Veterans Health Administration (VHA) integrated care (IC) program combined with telephonic work-focused counseling, known as Be Well at Work (BWAW), is superior to IC alone for improving occupational functioning and depression, to determine whether these effects persist 4 months later, and to determine whether the return on investment is positive.
Design, Setting, and Participants
In this randomized clinical trial conducted from October 21, 2014, to December 6, 2019, patients undergoing IC at VHA facilities were screened for eligibility and randomized to IC alone or IC plus BWAW. Blinded interviewers administered questionnaires before the intervention, immediately after completion of the intervention at month 4, and at month 8. Eligibility criteria were individuals 18 years or older who were working at least 15 hours per week in a job they had occupied for at least 6 months, were experiencing work limitations, and had current major depressive disorder or persistent depressive disorder. Exclusion criteria were individuals who could not read or speak English, had planned maternity leave, or had a history of bipolar disorder or psychosis. Data analyses were conducted from January 1, 2018, to December 6, 2019.
Interventions
Integrated care is multidisciplinary depression care involving screening, clinical informatics, measurement-based care, brief behavioral interventions, and referral as needed to specialty mental health care. Be Well at Work counseling involves 8 biweekly telephone sessions and 1 telephone booster visit after 4 months. Doctoral-level psychologists helped patients to identify barriers to functioning and to adopt new work-focused cognitive-behavioral and work-modification strategies.
Main Outcomes and Measures
The primary outcome was the adjusted mean group difference in changes from before to after intervention (hereafter, adjusted effect) in the percentage of at-work productivity loss, measured with the Work Limitations Questionnaire (range, 0%-25%). The secondary outcome was adjusted effect in the Patient Health Questionnaire 9-item symptom severity score (range, 0-27, with 0 indicating no symptoms and 27, severe symptoms).
Results
Of 670 veterans referred for participation, 287 veterans (42.8%) consented and completed eligibility screening, and 253 veterans (37.8%) were randomized. Among these 253 patients (mean [SD] age, 45.7 [11.6] years; 218 [86.2%] men; 135 [53.4%] white), 114 (45.1%) were randomized to IC and 139 (54.9%) were randomized to IC plus BWAW. At the 4-month follow-up, patients who received IC plus BWAW had greater reductions in at-work productivity loss (adjusted effect, −1.7; 95% CI, −3.1 to −0.4; P = .01) and depression symptom severity (adjusted effect, −2.1; 95% CI, −3.5 to −0.7; P = .003). The improvements from IC plus BWAW persisted 4 months after intervention (at-work productivity loss mean difference, −0.5; 95% CI, −1.9 to 0.9; P = .46; depression symptom severity mean difference, 0.6; 95% CI −0.9 to 2.1; P = .44). The cost per patient participating in BWAW was $690.98, and the return on investment was 160%.
Conclusions and Relevance
These findings suggest that adding this work-focused intervention to IC improves veterans’ occupational and psychiatric outcomes, reducing obstacles to having a productive civilian life.
Trial Registration
ClinicalTrials.gov Identifier: NCT02111811
Introduction
In the largest health care system in the United States, the Veterans Health Administration (VHA), approximately 7% of patients meet criteria for major depressive disorder, and 13.5% of patients visiting VHA primary care clinics have depression symptoms.1 Major depressive disorder is a costly, frequently disabling condition.2 Depression specifically contributes to occupational disability.3 Compared with veterans without depression, veterans with depression have more unemployment,3 and those who work have more functional deficits (known as presenteeism) and work absences.4,5 A 2011 study4 among Operation Enduring Freedom and Operation Iraqi Freedom veterans who were referred by VHA primary care clinicians for psychiatric evaluation found that veterans with depression had a mean of approximately 6% to 8% less productivity than a healthy benchmark sample.
The VHA currently offers vocational rehabilitation services, which are primarily for unemployed veterans, as well as comprehensive depression care. Since 2007, the VHA has implemented evidence-based, primary care mental health integrated care (IC) for depression, which consists of screening, clinical informatics, measurement-based care, brief behavioral interventions, and referral to specialty mental health care to reduce symptom severity, delivered by multidisciplinary teams.6 A 2006 study7 of the IC program found that it improved depression detection and treatment as well as clinical outcomes. However, while studies conducted in non-VHA settings report improved occupational outcomes associated with IC,8,9 to our knowledge, the effect of IC on the occupational outcomes of veterans with depression is not known.
This study’s primary aim was to test whether the VHA’s primary care mental health IC program for depression in combination with a telephone-based work-focused intervention, known as Be Well at Work (BWAW), was more effective than IC alone. In 2 prior clinical trials involving commercially insured employees principally recruited through their employers, BWAW was superior to usual depression care for reducing presenteeism, absenteeism, and depression symptom severity.10,11 To our knowledge, this is the first study to test this program’s effectiveness in the context of a health care delivery system in which standard depression care is high quality and evidence based. We hypothesized that, compared with IC alone, the combined program would result in greater improvements in occupational functioning and depression symptom severity and that improvements would persist. We also aimed to determine whether the experimental program provided a return on investment (ROI).
Methods
From October 21, 2014, through December 6, 2019, we conducted a 2-group randomized clinical trial comparing IC alone with IC combined with BWAW at a large VHA medical center and 2 smaller satellite sites. In this single-blind study, research assistants collecting study data were blinded to treatment group assignment. The study did not restrict veterans’ use of VHA or non-VHA care. Full details on the study protocol are available in Supplement 1, and information on deviations from the protocol are listed in the eAppendix in Supplement 2. The protocol was reviewed and approved by each local institutional review board. All participants provided written informed consent. This study is reported following the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Eligible veterans were 18 years or older, worked at least 15 hours per week in jobs they had occupied for at least 6 months, and had work limitations resulting in at least 5% at-work productivity loss based on validated questionnaire assessment, as well as current major depressive disorder or persistent depressive disorder confirmed by diagnostic interview. Exclusions were inability to speak or read English, planned maternity leave, or a history of bipolar disorder or psychosis.
The IC program referred veterans to the study. Research assistants conducted the pretrial screening, involving a health record review and telephone interview. Potentially eligible, interested patients were invited to come in for informed consent and to complete a further eligibility assessment, which also served as the study baseline measurement (T0). For this initial assessment, the research assistant administered standardized questions to assess depression (Patient Health Questionnaire [PHQ-9]; range, 0-27, with 0 indicating no symptoms and 27, severe symptoms),12 work limitations (Work Limitations Questionnaire [WLQ]; range, 0%-25%),13 mean number of alcoholic drinks per week,14 generalized anxiety disorder (General Anxiety Disorder 7-item questionnaire; range, 0-21, in which 0 = no symptoms to 21 = severe anxiety),15 posttraumatic stress disorder based on a checklist (1 = present, 0 = absent),16 use of illicit substances (excluding cannabis) more than weekly in the past month,17 suicidal ideation,12 and the Veterans Rand 12-item health survey.18
Next, VHA study clinicians administered the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5)19 (SCID-5) modules to diagnose major depressive disorder and persistent depressive disorder and rule out bipolar disorder and psychosis.20 Finally, patients were asked to complete a self-report questionnaire measuring work absences (WLQ Time Loss Module), work hours, job earnings, demographic characteristics needed for descriptive purposes (eg, race/ethnicity and sex), use of non-VA care, and current and past service-connected disability claims. Physical and psychosocial job demands, job autonomy, and workplace social support were measured with a modified Job Content Questionnaire (range, 0-100, in which 0 indicates minimum and 100, maximum).21 These assessments required approximately 1 hour to complete.
If all eligibility criteria were met, the patient was assigned by simple randomization to 1 of the treatment groups. In this automated process, a random uniform number was calculated using the Math.random function in Java Math Library random function software version 8 (Oracle Technology Network) and the patient was assigned to IC plus BWAW half of the time.
Follow-up telephone interviews of randomized patients were conducted after the intervention period at month 4 (T1), and at approximately months 8 to 9 (T2). Patients who did not complete the T1 follow-up remained eligible for T2. For difficult-to-reach patients, multiple telephone and/or mail outreach attempts were made. At T2, we extracted VHA data for 2013 to 2017 on all diagnoses, health care use, and mental health or behavioral health treatments. Incentives included $25 for the baseline visit, $25 for the T1 follow-up, and $45 for the T2 follow-up (total, $95).
Interventions
Within IC, patients with mild to moderate disorders were treated in primary care in collaboration with the primary care clinician and an IC mental health care practitioner. Patients with more severe symptoms were encouraged to engage in the appropriate VHA specialty care (eg, mental health services, addiction counseling).22 Practitioners in the IC team included psychologists, nurses, and social workers, supervised by a VHA psychiatrist, who supported the use of brief evidence-based psychotherapy and pharmacotherapy. Treatment plans promoted adherence to prescribed antidepressants as well as activities to increase positive social interactions, healthy living, and self-esteem. Patients were continuously assessed to determine whether a higher level of care was needed and to facilitate transition as needed to more specialized services.
Patients assigned to IC plus BWAW also received an individualized program of eight 50-minute telephone visits occurring biweekly for 4 months, and 1 booster session approximately 4 months later. Telephone care reduces the burden of requiring in-person visits for patients who also work. Two doctoral-level psychologists who were not providing IC provided BWAW counseling under the supervision of its developers (a psychiatrist [D.A.A.] and a workplace health specialist [D.L.]). Initially, counselors received an intensive 2.5-day training session, followed by weekly telephone supervision involving in-depth case reviews. Additionally, counselor fidelity to the protocol was monitored through review of electronic health records. Patient records had mandatory data fields to document steps in the BWAW care process (eg, homework assignments, referrals to specialty care, standardized assessments, physician reporting, self-care planning). We did not audiorecord patient care visits.
The BWAW intervention is based on stress and coping theory in which successful mental health and functional outcomes are related to responding effectively to psychosocial challenges.23 Accordingly, stress occurs when coping methods are ineffective for confronting life events and experiences, such as work demands, which the person perceives as threatening or harmful. Coping may be compromised by factors such as depression symptoms, access to social supports, and adverse life experiences. Be Well at Work targets 3 areas of coping. First, counselors address issues related to coping with depression treatment using motivational enhancement and psychoeducational strategies to prepare the patient to actively engage in treatment provided in BWAW and by the person’s regular health care practitioner. To coordinate BWAW with existing depression care, counselors assess occupational functioning and depression symptom severity monthly, sharing results with health care practitioners through the VHA electronic health record. Second, counselors provide work-focused cognitive-behavioral therapy strategy training based on a self-help manual adapted from Simon and colleagues.24 This component is aimed at increasing the patient’s ability to identify maladaptive patterns of thinking, feeling, and behaving that affect work and substitute more adaptive coping behaviors. Third, the patient and counselor identify and address workplace barriers to effective functioning and potential work-appropriate coping strategies. Drawing from psychology, occupational health, and disability and rehabilitation practices,25,26 patients are guided to make small specific changes in how they perform work tasks (eg, new time management techniques), work routines (eg, collaborating vs staying isolated), and/or the work environment (eg, rearranging the workspace). Some patients may be guided to develop compensatory work strategies (eg, using memory aids).
With 2-week intervals between sessions, patients are assigned homework to test new strategies and integrate their use. The BWAW intervention culminates with the development of a customized self-care plan. At the booster session, self-care progress is reviewed, and if necessary, the plan is adjusted.
Hypotheses and Measures
We hypothesized that T1 outcomes of the IC plus BWAW group would be better than those of the IC-only group, indicated by the adjusted mean group difference in the changes in WLQ at-work productivity loss score from before the intervention to after. Secondary end points included the adjusted mean group difference in changes in depressive symptom severity and in productivity loss due to work absences from before the intervention to after. We also assessed adjusted mean differences in the change in percentage of job loss (for any reason) and new disability claims, and in mean weekly work hours. Our second hypothesis was that the improvements observed at T1 would be present at T2. Our third hypothesis was that the ROI for IC plus BWAW would be positive.
The WLQ at-work productivity loss score is computed using an empirically based algorithm reflecting the observed association between its 4 scale scores and objectively measured productivity. The WLQ assesses the amount of health-related difficulty in the past 2 weeks performing work tasks.13 The tasks are organized into work limitation scales addressing time management, physical tasks, mental and interpersonal tasks, and output tasks. Scale scores range from 0% (limited none of the time) to 100% (limited all of the time). Scale Cronbach α in this sample are 0.87 to 0.89. The at-work productivity loss score is the weighted sum of the scale scores, and quantifies the estimated percentage difference in at-work productive output between a person (or group) completing the WLQ and an external healthy worker benchmark sample (range, 0%-25%, with a higher score indicating more at-work productivity loss).27 The WLQ Time Loss Module measures the number of hours of work missed in the past 2 weeks owing to a health-related issue. The percentage of productivity loss due to absences was calculated as the number of hours missed divided by the number of hours usually spent working. Depression symptom severity was measured with the Patient Health Questionnaire, with scores ranging from 0, indicating no depressive symptoms to 27, severe depression.28 The sample Cronbach α is 0.78.
Statistical Analysis
For our first hypothesis, based on data from the primary site we estimated that a sample size of 100 enrollees per treatment group would be needed for 80% power to detect a mean group difference in the change in at-work productivity loss score of 1.2% at T1, based on an intent-to-treat analysis using analysis of covariance (ANCOVA) with a 2-sided t test and statistical significance set at P = .05. For our second hypothesis, we used mixed models testing for maintenance of outcomes from T1 to T2.
From an economic perspective, a 1–percentage point productivity improvement is meaningful at group, company, and national levels. For example, a 2% to 3% change in output nationally is regarded as an important indicator.29 On an employer level, if 6% of employees in a 10 000-person company with mean annual earnings of $45 000 were to have depression, a 1% improvement in productivity would generate productivity savings of $450 per employee with depression, or $270 000 companywide.
Prior to testing our hypothesis, we evaluated the randomization with t tests and χ2 statistics, the effect of attrition from the study, and BWAW treatment drop-out. Because the 2 low-volume satellite sites enrolled only 3 patients, their data were excluded.
For our first hypothesis, we present the mean change in the primary study outcome by group followed by hypothesis-testing of the adjusted T1 outcome with ANCOVA (adjusted mean group difference in changes from before to after intervention [hereafter, adjusted effect] and P value). All other study outcomes (ie, depression symptom severity, productivity loss due to absences, job loss, disability claims, and weekly work hours) were tested using these methods. Additionally, mixed-model results based on all available data and a last value–carry forward analysis were used to confirm that sample losses to follow-up did not bias conclusions.
For our second hypothesis, changes from T1 to T2 and intervention effects were estimated and tested using mixed models. Models included variables for time and a treatment-by-time interaction. The T2 follow-up interaction was compared with the T1 interaction using 2-sided z tests with P = .05.
For our third hypothesis evaluating ROI, we computed the ratio of benefits minus costs to costs.30 To monetize benefits, we computed the marginal benefits at T2 in at-work productivity loss and productivity loss due to absences using a mean of 4- and 8-month effects, and combined them with the formula: total productivity loss = absenteeism loss + at-work productivity loss × (1 – absenteeism). Next, total percentage loss was multiplied by the sample’s median annual job earnings, $45 000. Marginal costs were based on the mean number of counselor hours per BWAW participant. Counselor cost per clinical hour was calculated as the sum of a doctoral-level counselor salary ($105 697) plus benefits (32% of salary) and overhead (20% of salary), divided by 1260 clinical counseling hours available per year, totaling $132.88 per hour. The total cost of participating in BWAW was computed as this hourly amount multiplied by the number of per-participant treatment hours (mean [SD], 5.2 [2.9] hours). Missed appointment hours and supervision time were considered part of counselor time other than the included 1260 clinical counseling hours.
All analyses were performed with Stata statistical software version 15 (StataCorp). Data analyses were conducted from January 1, 2018, to December 6, 2019.
Results
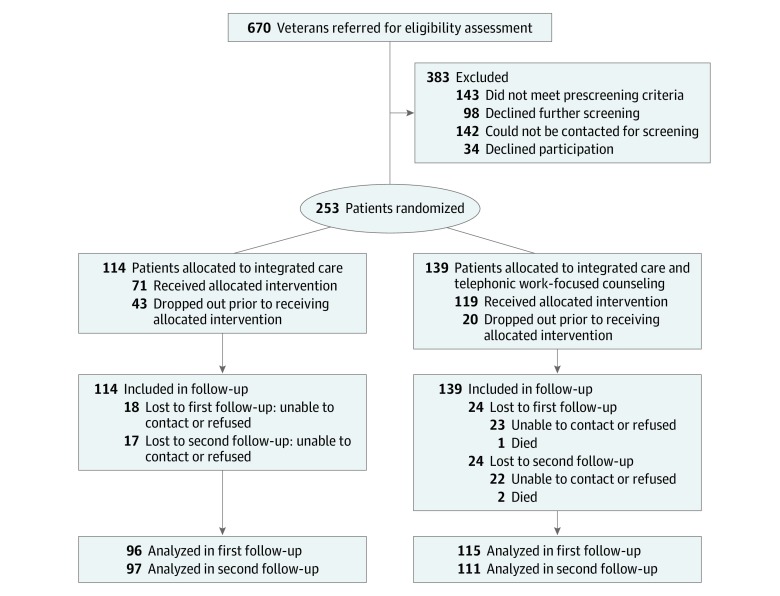
Of 670 veterans referred to the study, 143 (21.3%) were ineligible at pretrial screening, 142 (21.2%) could not be reached for eligibility screening, and 98 (14.6%) declined further assessment (Figure). Of 287 veterans (42.8%) who consented to the study, 31 (4.6%) were ineligible at T0 assessment, and 3 (0.4%) dropped out. Therefore, the starting sample included 253 patients (37.8% of those originally referred; mean [SD] age, 45.7 [11.6] years; 218 [86.2%] men) (Table 1). There were 135 white patients (53.4%), and 116 patients (46.2%) reported having attended some college. At T0, 114 patients (45.1%) were randomized to IC and 139 patients (54.9%) were randomized to IC plus BWAW. The T1 follow-up survey was completed by 96 patients (83.5%) in the IC group and 115 patients (82.7%) in the IC plus BWAW group, and the T2 follow-up survey was completed by 97 patients (84.3%) in the IC group and 111 patients (79.9%) in the IC plus BWAW group (study attrition rate, 17.8%). At baseline (Table 1 and Table 2) and after attrition (eTable 1 and eTable 2 in Supplement 2), the treatment groups were not significantly different on any variable.
Figure. CONSORT Flow Diagram.
Table 1. Baseline Sample Characteristics of IC-Only Group vs IC Plus BWAW Group.
| Characteristic | No. (%) | P Value for Difference | |||
|---|---|---|---|---|---|
| Total Respondents | Total (N = 253) | IC Only (n = 114) | IC + BWAW (n = 139) | ||
| Age, mean (SD), y | 253 | 45.7 (11.6) | 44.8 (11.6) | 46.5 (11.6) | .26 |
| Men | 253 | 218 (86.2) | 96 (84.2) | 122 (87.8) | .41 |
| White race | 253 | 135 (53.4) | 56 (49.1) | 79 (56.8) | .22 |
| Education | |||||
| <High school | 351 | 2 (0.8) | 2 (1.8) | 0 | .50 |
| High school | 251 | 44 (17.5) | 18 (15.8) | 26 (19.0) | |
| Some college | 251 | 116 (46.2) | 57 (50.0) | 59 (43.1) | |
| Associate’s degree | 251 | 19 (7.6) | 7 (6.1) | 12 (8.8) | |
| Bachelor’s degree | 251 | 40 (15.9) | 18 (15.8) | 22 (16.1) | |
| Postgraduate degree | 251 | 30 (12.0) | 12 (10.5) | 18 (13.1) | |
| Annual earnings, median, (range), $ | 243 | 45 000 (500-200 000) | 45 000 (500-140 000) | 45 000 (500-200 000) | .99 |
| Work status | |||||
| Working for pay | 251 | 237 (94.4) | 104 (91.2) | 133 (97.1) | .11 |
| Off work owing to illness | 251 | 4 (1.6) | 4 (3.5) | 0 | |
| Off work owing to injury | 251 | 2 (0.8) | 1 (0.9) | 1 (0.7) | |
| On vacation | 251 | 6 (2.4) | 3 (2.6) | 3 (2.2) | |
| Not working (other reason) | 251 | 2 (0.8) | 2 (1.8) | 0 | |
| Time at current job, y | |||||
| <1 | 251 | 52 (20.7) | 22 (19.3) | 30 (21.9) | .53 |
| 1 to <2 | 251 | 48 (19.1) | 26 (22.8) | 22 (16.1) | |
| 2 to <5 | 251 | 46 (18.3) | 19 (16.7) | 27 (19.7) | |
| 5 to 10 | 251 | 44 (17.5) | 17 (14.9) | 27 (19.7) | |
| >10 | 251 | 61 (24.3) | 30 (26.3) | 31 (22.6) | |
| Job type | |||||
| Permanent | 251 | 223 (88.8) | 102 (89.5) | 121 (88.3) | .77 |
| Temporary | 251 | 28 (11.2) | 12 (10.5) | 16 (11.7) | |
| Payment structure | |||||
| Hourly | 250 | 158 (63.2) | 70 (61.4) | 88 (64.7) | .59 |
| Salaried | 250 | 87 (34.8) | 42 (36.8) | 45 (33.1) | .54 |
| Member of labor union | 251 | 101 (40.2) | 43 (37.7) | 58 (42.3) | .46 |
| Employment type | |||||
| Self-employed | 249 | 12 (4.8) | 4 (3.6) | 8 (5.8) | .41 |
| Private company | 249 | 117 (47.0) | 59 (52.7) | 58 (42.3) | .10 |
| Government agency | 249 | 120 (48.2) | 49 (43.8) | 71 (51.8) | .21 |
| Filed disability claim, past 4 mo | 251 | 10 (4.0) | 7 (6.1) | 3 (2.2) | .11 |
| Insurance through employer | 251 | 137 (54.6) | 61 (53.5) | 76 (55.5) | .76 |
| Eligible for paid sick time | 249 | 187 (75.1) | 84 (75.0) | 103 (75.2) | .97 |
| PHQ-9 symptom severity score, mean (SD) | 14.5 (4.8) | 14.1 (4.9) | 14.8 (4.8) | .25 | |
| High suicide risk | 253 | 54 (21.3) | 25 (21.9) | 29 (20.9) | .84 |
| SCID results | |||||
| MDD and PDD | 253 | 107 (42.3) | 45 (39.5) | 62 (44.6) | .41 |
| MDD | 253 | 106 (41.9) | 50 (43.9) | 56 (40.3) | .57 |
| PDD | 253 | 40 (15.8) | 19 (16.7) | 21 (15.1) | .74 |
| GAD-7 score, mean (SD) | 252 | 13.0 (4.8) | 12.8 (4.5) | 13.1 (5.0) | .62 |
| PTSD | 253 | 151 (59.7) | 69 (60.5) | 82 (59.0) | .81 |
| Alcoholic drinks/wk, mean (SD), No. | 251 | 5.4 (8.9) | 5.1 (8.8) | 5.6 (8.9) | .64 |
| Recent substance misuse | 253 | 5 (2.0) | 3 (2.6) | 2 (1.4) | .50 |
| VR12 score, mean (SD) | |||||
| Physical component | 251 | 38.3 (12.9) | 38.2 (13.4) | 38.4 (2.4) | .94 |
| Mental component | 251 | 28.5 (10.8) | 29.0 (11.1) | 28.1 (10.6) | .49 |
| Using antidepressant medication | 253 | 68 (26.9) | 26 (22.8) | 42 (30.2) | .19 |
| Non-VHA health care, past 4 mo | |||||
| Physician visit | 251 | 95 (37.8) | 44 (38.6) | 51 (37.2) | .82 |
| Therapist visit | 251 | 23 (9.2) | 13 (11.4) | 10 (7.3) | .26 |
| Hospitalization | 251 | 7 (2.8) | 4 (3.5) | 3 (2.2) | .53 |
| Emergency department visit | 251 | 28 (11.2) | 13 (11.4) | 15 (10.9) | .91 |
Abbreviations: BWAW, Be Well at Work; GAD-7, 7-item General Anxiety Disorder questionnaire; IC, integrated care; MDD, major depressive disorder; PDD, persistent depressive disorder; PHQ-9, 9-item Patient Health Questionnaire; PTSD, posttraumatic stress disorder; SCID, Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition); VHA, Veterans Health Administration; VR12, Veterans Rand 12-item health survey.
Table 2. Baseline Self-Reported Work Issues Among IC-Only vs IC Plus BWAW Groups.
| Self-Reported Work Issue | Respondents, No. | Mean (SD) | P Value for Difference | ||
|---|---|---|---|---|---|
| Total | IC Only | IC + BWAW | |||
| Work Limitations Questionnaire scorea | |||||
| Time management | 250 | 52.0 (23.5) | 51.3 (24.5) | 52.6 (22.7) | .65 |
| Physical tasks | 248 | 41.3 (24.7) | 41.8 (24.1) | 40.9 (25.2) | .78 |
| Mental or interpersonal tasks | 251 | 46.8 (21.4) | 46.9 (21.3) | 46.8 (21.5) | .96 |
| Output tasks | 249 | 46.1 (24.3) | 46.4 (23.9) | 45.9 (24.8) | .89 |
| At-work productivity loss, %b | 245 | 12.3 (4.7) | 12.3 (4.5) | 12.4 (4.9) | .88 |
| Absenteeism | |||||
| Time missed in the past 2 wk, d | 253 | 1.8 (2.4) | 1.9 (2.4) | 1.8 (2.3) | .55 |
| Productivity loss due to absences, %c | 250 | 18.6 (22.4) | 20.7 (25.0) | 16.9 (20.1) | .19 |
| Had leave of absence in past 4 mo, No. (%) | 249 | 32 (12.9) | 16 (14.3) | 16 (11.7) | .54 |
| Modified Job Content Questionnaire scores | |||||
| Job control | 251 | 47.5 (21.2) | 48.0 (21.2) | 47.1 (21.4) | .74 |
| Physical job demands | 251 | 46.7 (31.5) | 44.2 (30.9) | 48.8 (32.0) | .25 |
| Psychosocial job demands | 251 | 61.7 (18.5) | 61.6 (18.2) | 61.8 (18.8) | .93 |
| Supervisor support | 251 | 52.8 (32.2) | 54.4 (31.9) | 51.5 (32.5) | .47 |
| Coworker support | 250 | 57.6 (29.4) | 58.8 (28.2) | 56.6 (30.5) | .57 |
| Bothered or upset by work, No. (%) | |||||
| Almost always | 251 | 43 (17.1) | 17 (14.9) | 26 (19.0) | .18 |
| Often | 251 | 102 (40.6) | 47 (41.2) | 55 (40.1) | |
| Sometimes | 251 | 88 (35.1) | 45 (39.5) | 43 (31.4) | |
| Rarely | 251 | 17 (6.8) | 4 (3.5) | 13 (9.5) | |
| Never | 251 | 1 (0.4) | 1 (0.9) | 0 (0) | |
| Job satisfaction, No. (%) | |||||
| Extremely satisfied | 251 | 14 (5.6) | 5 (4.4) | 9 (6.6) | .81 |
| Very satisfied | 251 | 50 (19.9) | 22 (19.3) | 28 (20.4) | |
| Somewhat satisfied | 251 | 107 (42.6) | 53 (46.5) | 54 (39.4) | |
| Somewhat dissatisfied | 251 | 55 (21.9) | 23 (20.2) | 32 (23.4) | |
| Very dissatisfied | 251 | 25 (10.0) | 11 (9.6) | 14 (10.2) | |
Abbreviations: BWAW, Be Well at Work; IC, integrated care.
Scores indicate the mean percentage of time in the prior 2 weeks the person was limited by health conditions.
Range, 0% to 25%.
Measured as the mean percentage of total hours missed from work in the past 2 weeks owing to health conditions or medical care divided by the number of hours usually spent working (range, 0-100).
Regarding work characteristics, 52 patients (20.7%) had their jobs less than 1 year, while job tenure exceeded 10 years for 61 patients (24.3%); 223 patients (88.8%) were permanent workers; 101 patients (40.2%) had unionized positions; and 158 patients (63.2%) were paid hourly. Most patients had access to employer-sponsored health insurance (137 patients [54.6%]) and paid sick days (187 patients [75.1%]) (Table 1). Similar proportions of patients worked in the private (117 patients [47.0%]) and public (120 patients [48.2%]) sectors. In the prior 4 months, 10 patients (4.0%) had filed for service-connected disability benefits.
At T0, the mean (SD) Patient Health Questionnaire depression symptom severity score was 14.5 (4.8), indicating moderate severity; 106 patients (41.9%) met DSM-5 criteria19 for major depressive disorder only, 40 patients (15.8%) met criteria for persistent depressive disorder only, and 107 patients (42.3%) met criteria for both. A total of 68 patients (26.9%) were using antidepressant medications at baseline. Overall mean (SD) Veterans Rand 12-item health survey scores for physical health (38.3 [12.9]) and mental health (28.5 [10.8]) components were poor (Table 1).
In the 2 weeks prior to baseline, the mean (SD) proportions of time patients had work limitations were 52.0% (23.5%) for time management, 41.3% (24.7%) for physical tasks, 46.8% (21.4%) for mental and interpersonal tasks, and 46.1% (24.3%) for output tasks (Table 2). Mean (SD) at-work productivity loss was 12.3% (4.7%). In this same period, patients missed a mean (SD) of 1.8 (2.4) workdays and had a mean (SD) absence productivity loss of 18.6% (22.4). There were no significant differences between the IC and IC plus BWAW groups in their ratings of job stress, job satisfaction, job control, job demands, or workplace support. The results from the Modified Job Content Questionnaire suggest that jobs were viewed as more demanding psychosocially (mean [SD] score, 61.7 [18.5]) than physically (mean [SD] score, 46.7 [31.5]).
During the 4-month intervention period, patients in the IC group had a mean (SD) of 3.9 (3.9) mental health office visits compared with 3.8 (5.4) mental health visits in the IC plus BWAW group (P = .20). The mean (SD) number of BWAW sessions attended was 5.2 (2.9). Twenty patients (14.2%) in the IC plus BWAW group attended no BWAW sessions or only 1. Approximately one-fifth of patients in the IC plus BWAW group (27 patients [22.1%]) completed the BWAW booster session.
For our first hypothesis, tested with ANCOVA, we found that IC plus BWAW resulted in larger reductions in at-work productivity loss by T1 (adjusted effect, −1.7; 95% CI, −3.1 to −0.4; P = .01) (Table 3). Regarding secondary outcomes, we found significantly greater reductions in depression symptom severity for the IC plus BWAW group compared with the IC-only group (adjusted effect, −2.1; 95% CI, −3.5 to −0.7; P = .003), although both groups experienced significant improvements (IC-only: mean change, −1.6; 95% CI, −2.6 to −0.7; P = .001; IC plus BWAW: mean change, −3.8; 95% CI, −4.8 to −2.7; P < .001). Although rates of productivity loss due to work absences showed a greater change in the IC plus BWAW group (mean change, −4.0%; 95% CI, −8.5% to 0.5%) than the IC-only group (mean change, −1.3%; 95% CI, −6.9% to 4.2%), the difference was not statistically significant (P = .20), but the mean changes from both follow-ups combined was significant (combined effect: at-work productivity loss, –1.94; 95% CI, –0.82 to –3.1; P < .001; productivity loss due to absences, 1.96; 95% CI, –7.5 to 3.6; P < .001). In terms of additional outcomes assessed, we found that the IC-only group had a significantly greater loss in the number of weekly work hours than the IC plus BWAW group (adjusted effect, 6.4; 95% CI, 2.8 to 10.1; P = .001). Changes in the percentages of job loss (adjusted effect, −0.02; 95% CI, −0.08 to 0.03; P = .46) and disability claims (adjusted effect, −0.7; 95% CI, −6.3 to 4.9; P = .81) were not statistically different. These results were consistent in models based on last value carried–forward analysis (eTable 4 in Supplement 2).
Table 3. Analysis of Covariance Among IC-Only vs IC Plus BWAW Groups.
| Outcome | IC Only | IC + BWAW | Adjusted Effect (95% CI)a | P Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Change, Mean (95% CI) | P Value | Mean (SD) | Change, Mean (95% CI) | P Value | |||||
| T0 (n = 96) | T1 (n = 96) | T0 (n = 115) | T1 (n = 115) | |||||||
| At-work productivity loss, %b | 11.7 (4.7) | 11.7 (4.6) | −0.1 (−1.1 to 0.9) | .86 | 12.3 (4.9) | 10.2 (6.0) | −2.1 (−3.1 to −1.0) | <.001 | −1.7 (−3.1 to −0.4) | .01 |
| Depression symptom severity scorec | 14.3 (4.8) | 12.6 (5.5) | −1.6 (−2.6 to −0.7) | .001 | 14.4 (5.3) | 10.6 (6.3) | −3.8 (−4.8 to −2.7) | <.001 | −2.1 (−3.5 to −0.7) | .003 |
| Productivity loss due to absence, %d | 19.2 (23.3) | 17.9 (21.1) | −1.3 (−6.9 to 4.2) | .64 | 17.7 (20.1) | 13.7 (20.0) | −4.0 (−8.5 to 0.5) | .09 | −3.7 (−9.3 to 1.9) | .20 |
| Had leave of absence, % | 12.0 (32.6) | 9.8 (29.9) | −2.2 (−8.2 to 3.9) | .48 | 12.6 (33.3) | 9.0 (28.8) | −3.6 (−10.7 to 3.5) | .32 | −1.0 (−8.5 to 6.4) | .79 |
| Filed disability claim, % | 7.4 (26.4) | 5.3 (22.6) | −2.1 (−8.0 to 3.8) | .48 | 1.8 (13.4) | 3.6 (18.7) | 1.8 (−2.5 to 6.1) | .42 | −0.7 (−6.3 to 4.9) | .81 |
| Experienced job loss, % | 0 | 3.1 (17.5) | 3.1 (−0.4 to 6.6) | .08 | 0 | 5.2 (22.3) | 5.2 (1.1 to 9.3) | .01 | 2.1 (−3.4 to 7.6) | .46 |
| Work hr/wk | 45.0 (19.6) | 36.6 (13.0) | −8.4 (−12.8 to −4.0) | <.001 | 43.1 (15.9) | 42.6 (14.2) | −0.5 (−3.5 to 2.5) | .73 | 6.4 (2.8 to 10.1) | .001 |
Abbreviations: BWAW, Be Well at Work; IC, integrated care; T0, baseline; T1, 4-month follow-up.
Controlled for baseline values of the outcome variable.
Measured using the Work Limitations Questionnaire (range, 0%-25%).
Measured using the Patient Health Questionnaire 9-item symptom severity score (range, 0-27).
Measured as the mean percentage of total hours missed from work in the past 2 weeks owing to health conditions or medical care divided by the number of hours usually spent working (range, 0-100).
Regarding our second hypothesis, which was tested in mixed models (Table 4; eTable 2 in Supplement 2), we found that the IC plus BWAW group advantage in at-work productivity loss at T1 did not erode at T2 (mean difference, −0.5; 95% CI, −1.9 to 0.9; P = .46). There was also no significant loss in the initial improvement in depression severity (mean difference, 0.6; 95% CI, −0.9 to 2.1; P = .44). Using mixed models, the sensitivity tests of time by group interactions (eTable 3 in Supplement 2) also supported ANCOVA results.
Table 4. Mixed Model Estimates for Analyses of Outcome Changes for IC-Only vs IC Plus BWAW Groups.
| Outcome | Estimate | Mean Difference of Changes (95% CI) | P Valuea | |||
|---|---|---|---|---|---|---|
| IC Only | IC + BWAW | |||||
| T1 (n = 96) | T2 (n = 97) | T1 (n = 115) | T2 (n = 111) | |||
| At-work productivity loss, %b | 11.9 | 11.3 | 10.2 | 9.2 | −0.5 (−1.9 to 0.9) | .46 |
| Depression symptom severity scorec | 12.6 | 12.0 | 10.7 | 10.7 | 0.6 (−0.9 to 2.1) | .44 |
| Productivity loss due to absence, %d | 18.4 | 19.4 | 13.6 | 12.6 | −2.0 (−9.0 to 5.1) | .58 |
| Had leave of absence, % | 10.4 | 11.4 | 8.8 | 11.4 | 1.5 (−8.5 to 11.5) | .76 |
| Filed disability claim, % | 5.0 | 7.3 | 3.8 | 6.7 | 0.6 (−7.0 to 8.3) | .87 |
| Experienced job loss, % | 3.0 | 9.3 | 5.1 | 5.4 | 6.0 (−0.5 to 12.5) | .07 |
| Work hr/wk | 36.9 | 39.9 | 42.8 | 41.1 | −4.8 (−10.0 to 0.5) | .07 |
Abbreviations: BWAW, Be Well at Work; IC, integrated care; T1, 4-month follow-up; T2, 8-month follow-up.
Estimated based on mixed models.
Measured using the Work Limitations Questionnaire (range, 0-25).
Measured using the Patient Health Questionnaire 9-item symptom severity score (range, 0-27).
Measured as the mean percentage of total hours missed from work in the past 2 weeks owing to health conditions or medical care divided by the number of hours usually spent working (range, 1-100).
Regarding benefits, at-work productivity loss was statistically significant with a point estimate of 2.0% (95% CI, 0.8% to 3.1%) combining effects from both follow-ups ($900 marginal benefit over a 1-year period). Similarly, the point estimate for absence-related productivity loss was approximately 2.0% (95% CI, 3.6% to 7.5%) ($900 marginal benefit). The cost per BWAW participant was $690.98. Medical costs were not included because they were similar in both groups. On this basis, the total benefit is $1800, implying an ROI of 160%. Excluding gains in productivity due to absence benefits, the ROI was 30%. If the effect lasted only until the second follow-up, benefits would be smaller and the ROI would be lower, at 95%, and after excluding gains in productivity due to absence benefits, ROI would be −2%. If benefits lasted for 2 years, the total ROI would be 421%, and the ROI excluding gains in productivity due to absence benefits would be 160%.
Discussion
This randomized clinical trial tested the benefits of adding a work-focused intervention to VHA IC for patients with depression and found that this relatively low-cost, work-focused intervention was effective and that the outcomes obtained immediately after the program ended were present 4 to 5 months later. As found in prior BWAW studies,10,11 the ROI was positive, partly reflecting the relatively low cost of BWAW and the high economic burden of depression.
The VHA recognizes the importance of employment to veterans’ mental health and quality of life, but it has not supplemented its integrated behavioral health interventions with work-focused services aimed at people currently employed.3 Currently, the Department of Veterans Affairs offers vocational supports, but these primarily serve veterans with disabilities who may need accommodations or retraining.31
In prior BWAW clinical trials in which participants were recruited from worksites,10,11 the BWAW program outperformed usual depression care, which meant any care the person elected to use. In a 2015 randomized clinical trial,10 BWAW was found to improve at-work productivity by 50%, productivity loss due to absences by 50%, and depression symptom severity by 50%. We found that improvements in at-work productivity, at 17%, and depression symptoms severity, at 26%, in IC plus BWAW were lower than these prior studies, which may reflect the greater health and social needs of veterans compared with other populations and the higher baseline quality of care provided in VHA IC compared with usual care. Furthermore, we found that the IC group also reduced their weekly work hours to a greater degree than the IC plus BWAW group, although they regained these hours by T2 so that the effect was not statistically significant. The effect on absences was also not as pronounced and not statistically significant. This may reflect the high degree of heterogeneity in workplace absence policies across the different employers, as controlling for occupation, hourly vs salaried status, unionization, paid sick days, or job tenure did not change the result. Rates of job loss and claims were similarly low. The study may have been underpowered to analyze these outcomes.
Limitations and Strengths
While the general conculsion of this study is that IC plus BWAW is superior to IC alone, this study has some limitations. This study included only 1 VHA medical center, and many eligible veterans did not participate, limiting generalizability. The sample size may have limited our power to detect some differences, and we relied on self-reported measures of outcomes, which may contribute response bias. Additionally, we could not determine the effect of the booster session, which was not highly attended. In future studies, we may wish to compare the cost vs benefits of telephonic BWAW to in-person or video versions.
This study also had some strengths, including the study design, clinical assessment of mental health, and objective measurement of VHA service use. Our intervention was manualized and had a strong emphasis on occupational functioning as the clinical goal. Additionally, we used extensively validated self-reported measures of depression and occupational outcomes, interviewer blinding, systematic efforts to follow-up with enrollees, and care was delivered in a realistic setting.
Conclusions
These findings suggest that adding a telephonic, work-focused intervention to IC for depression is more effective than IC alone. Facilitating reentry and reintegration into civilian life are high-priority goals within the Department of Veterans Affairs, and many employers want to hire veterans and be assured that they will function effectively in the workplace. Depression and difficulty functioning in occupational roles and settings pose significant barriers to achieving success. Building telephonic work-focused care into IC offers a holistic, accessible, and economical solution. As the VHA invests in telemedicine to address access barriers, BWAW’s telephone-based counseling provides a further opportunity to make higher-quality care more accessible to veterans.
Trial Protocol.
eAppendix. Deviations From the Original Protocol
eTable 1. Comparison of Baseline Characteristics of Study Participants With Study Drop-outs Within Integrated Care–Only Group and IC Plus Be Well at Work Group
eTable 2. Comparison of Baseline Characteristics of Integrated Care Plus Be Well at Work Treatment Participants vs Treatment Drop-outs
eTable 3. Model Estimates Without Baseline Data for Mixed-Model Analyses of Outcome Changes for Integrated Care–Only Group vs Integrated Care Plus Be Well at Work Group
eTable 4. Analysis of Covariance for Last Value Carry Forward Analysis
Data Sharing Statement.
References
- 1.Rubenstein L, Chaney E, Smith J. Improving treatment for depression in primary care. QUERI Quarterly. 2004;6(3):,. [Google Scholar]
- 2.US Department of Veterans Affairs, Veterans Benefits Administration Annual benefits report: fiscal year 2016. https://www.benefits.va.gov/REPORTS/abr/docs/2016_abr.pdf. Accessed January 22, 2020.
- 3.Zivin K, Yosef M, Levine DS, et al. Employment status, employment functioning, and barriers to employment among VA primary care patients. J Affect Disord. 2016;193:194-202. doi: 10.1016/j.jad.2015.12.054 [DOI] [PubMed] [Google Scholar]
- 4.Adler DA, Possemato K, Mavandadi S, et al. Psychiatric status and work performance of veterans of Operations Enduring Freedom and Iraqi Freedom. Psychiatr Serv. 2011;62(1):39-46. doi: 10.1176/appi.ps.62.1.39 [DOI] [PubMed] [Google Scholar]
- 5.Lippa SM, Fonda JR, Fortier CB, et al. Deployment-related psychiatric and behavioral conditions and their association with functional disability in OEF/OIF/OND veterans. J Trauma Stress. 2015;28(1):25-33. doi: 10.1002/jts.21979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Post EP, Van Stone WW. Veterans Health Administration primary care-mental health integration initiative. N C Med J. 2008;69(1):49-52. [PubMed] [Google Scholar]
- 7.Oslin DW, Ross J, Sayers S, Murphy J, Kane V, Katz IR; The Behavioral Health Laboratory . Screening, assessment, and management of depression in VA primary care clinics. J Gen Intern Med. 2006;21(1):46-50. doi: 10.1111/j.1525-1497.2005.0267.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schoenbaum M, Unützer J, McCaffrey D, Duan N, Sherbourne C, Wells KB. The effects of primary care depression treatment on patients’ clinical status and employment. Health Serv Res. 2002;37(5):1145-1158. doi: 10.1111/1475-6773.01086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang PS, Simon GE, Avorn J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298(12):1401-1411. doi: 10.1001/jama.298.12.1401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lerner D, Adler DA, Rogers WH, et al. A randomized clinical trial of a telephone depression intervention to reduce employee presenteeism and absenteeism. Psychiatr Serv. 2015;66(6):570-577. doi: 10.1176/appi.ps.201400350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lerner D, Adler D, Hermann RC, et al. Impact of a work-focused intervention on the productivity and symptoms of employees with depression. J Occup Environ Med. 2012;54(2):128-135. doi: 10.1097/JOM.0b013e31824409d8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lerner D, Amick BC III, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care. 2001;39(1):72-85. doi: 10.1097/00005650-200101000-00009 [DOI] [PubMed] [Google Scholar]
- 14.Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1988;83(4):393-402. doi: 10.1111/j.1360-0443.1988.tb00485.x [DOI] [PubMed] [Google Scholar]
- 15.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 16.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- 17.Humeniuk R, Ali R, Babor TF, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction. 2008;103(6):1039-1047. doi: 10.1111/j.1360-0443.2007.02114.x [DOI] [PubMed] [Google Scholar]
- 18.Kazis LE, Miller DR, Skinner KM, et al. Applications of methodologies of the Veterans Health Study in the VA healthcare system: conclusions and summary. J Ambul Care Manage. 2006;29(2):182-188. doi: 10.1097/00004479-200604000-00011 [DOI] [PubMed] [Google Scholar]
- 19.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 5th ed Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 20.First M, Williams JBW, Karg RS, Sptizer RL. Structured Clinical Interview for DSM-5 Disorders: Research Version. Washington, DC: APA Publishing; 2016. [Google Scholar]
- 21.Karasek RA. Job Content Questionnaire and User’s Guide. Amherst, MA: University of Massachusetts; 1985. [Google Scholar]
- 22.Tew J, Klaus J, Oslin DW. The Behavioral Health Laboratory: building a stronger foundation for the patient-centered medical home. Fam Syst Health. 2010;28(2):130-145. doi: 10.1037/a0020249 [DOI] [PubMed] [Google Scholar]
- 23.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publishing Co; 1984. [Google Scholar]
- 24.Simon G, Ludman EJ, Tutty D. Creating a Balance: A Step by Step Approach to Managing Stress and Lifting Your Mood. Bloomington, IN: Trafford Publishing; 2006. [Google Scholar]
- 25.Kopelowicz A, Liberman RP. Integrating treatment with rehabilitation for persons with major mental illnesses. Psychiatr Serv. 2003;54(11):1491-1498. doi: 10.1176/appi.ps.54.11.1491 [DOI] [PubMed] [Google Scholar]
- 26.Handler J, Doel K, Henry A, Lucca A. Rehab rounds: implementing supported employment services in a real-world setting. Psychiatr Serv. 2003;54(7):960-962. doi: 10.1176/appi.ps.54.7.960 [DOI] [PubMed] [Google Scholar]
- 27.Lerner D, Amick BC III, Lee JC, et al. Relationship of employee-reported work limitations to work productivity. Med Care. 2003;41(5):649-659. doi: 10.1097/01.MLR.0000062551.76504.A9 [DOI] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509-515. doi: 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- 29.The Conference Board Total economy database—key findings. https://www.conference-board.org/data/economydatabase/. Accessed December 5, 2019.
- 30.Brousselle A, Benmarhnia T, Benhadj L. What are the benefits and risks of using return on investment to defend public health programs? Prev Med Rep. 2016;3:135-138. doi: 10.1016/j.pmedr.2015.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abraham KM, Ganoczy D, Yosef M, Resnick SG, Zivin K. Receipt of employment services among Veterans Health Administration users with psychiatric diagnoses. J Rehabil Res Dev. 2014;51(3):401-414. doi: 10.1682/JRRD.2013.05.0114 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol.
eAppendix. Deviations From the Original Protocol
eTable 1. Comparison of Baseline Characteristics of Study Participants With Study Drop-outs Within Integrated Care–Only Group and IC Plus Be Well at Work Group
eTable 2. Comparison of Baseline Characteristics of Integrated Care Plus Be Well at Work Treatment Participants vs Treatment Drop-outs
eTable 3. Model Estimates Without Baseline Data for Mixed-Model Analyses of Outcome Changes for Integrated Care–Only Group vs Integrated Care Plus Be Well at Work Group
eTable 4. Analysis of Covariance for Last Value Carry Forward Analysis
Data Sharing Statement.