Abstract
This cross-sectional study uses combined statistical areas to explore whether the availability of clinical trial seats in nonrural regions varies with population, racial and socioeconomic compositions, research activity, or the amount of health care infrastructure.
Introduction
A lack of geographically convenient clinical trial sites hinders study participation,1,2 particularly for rural residents.3 But even in more densely populated regions, where most US residents live, trial locations may not be optimized to maximize access. In this cross-sectional study, we explored whether availability of trial seats in nonrural regions varies with population, racial and socioeconomic compositions, research activity, or amount of health care infrastructure.
Methods
We downloaded all records from ClinicalTrials.gov on August 29, 2016. Using automated methods and manual curation, we identified actively recruiting, interventional, industry-supported drug trials in phase 1/2 through phase 3 with at least 1 US site and an unambiguous number of total study locations. Records were downloaded on October 12, 2017, to update the sites and projected enrollment for each trial and exclude dormant trials. This yielded 41 770 nonunique US sites for 1926 trials (median, 18 sites/trial; interquartile range [IQR], 3-64 sites/trial).
We obtained zip codes for more than 98% of sites (41 279/41 770), imputing as needed by matching city, state, or institution name. We mapped zip codes to combined statistical areas (CSAs), each of which contains adjacent metropolitan, micropolitan, or both types of areas, and surrounding counties that share social and economic linkages.4,5 Because crosswalk files from zip codes to CSAs do not exist, we used a 2-step process involving core-based statistical areas as an intermediate. Our final analysis comprised 35 149 nonunique sites in CSAs from 1888 trials. To calculate mean seats per site, we divided each trial’s target enrollment by its total number of sites.
We obtained data on population (in 2016), median household income (in 2015), and racial demographics (in 2016) from the US Census; data on funding (in 2018) from the National Institutes of Health (NIH); and data on US inpatient hospital beds (in 2014) from the American Hospital Association’s annual survey. We mapped institutions to CSAs via zip codes as indicated above.
We performed linear regression and tabulations in Stata MP version 13 (StataCorp). Underlying data are available at Open Science Framework under a CC-BY-4.0 license.
The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. This study was based on publicly available data that did not include patient contact or medical record review, and therefore did not require institutional review board approval or informed consent.
Results
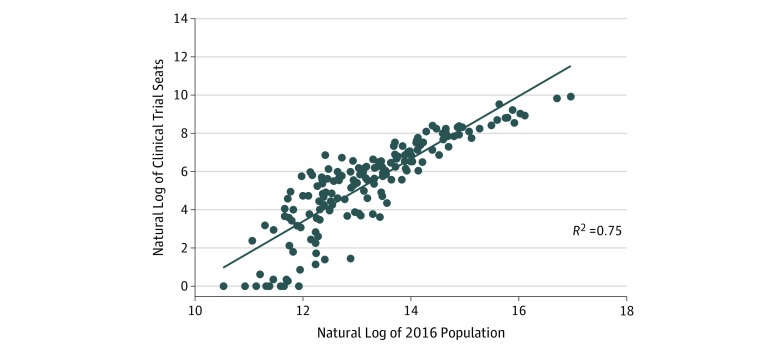
Across 171 CSAs in the United States, trial seats per 1000 residents ranged from 0 to 3.83 (median, 0.64; IQR, 0.25-1.01). In a bivariable model, population size explained 87% of the variation in seats per CSA (Figure). In a multivariable model, median income, percentage of the population identified as white, number of hospital beds, and NIH funding explained scant remaining variability and were not statistically significant (Table). We obtained similar results when we specifically focused on cancer studies (n = 1012), early-stage studies (phase 1/2 and phase 2; n = 1206), and late-stage studies (phase 2/3 and phase 3; n = 682) (data not shown).
Figure. Scatter Plot for 171 Combined Statistical Areas.
Table. Subtractive Model of Clinical Trial Seats per CSA.
| Bivariate | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|---|
| No. of CSAs | 171 | 171 | 171 | 171 | 171 | 171 | 171 |
| Population/1000 (SE) | 1 (−0.03) |
0.88 (−0.393) |
0.86 (−0.402) |
0.895 (−0.399) |
0.96 (−0.113) |
0.902 (−0.395) |
|
| Median income/$1000 (SE) | 157 (−22.2) |
−4.6 (−10.3) |
11.5 (−14.2) |
−6.13 (−8.89) |
−5.85 (−13.5) |
−0.708 (−11.2) |
|
| White, % (SE) | −78.35 (−17.44) |
−3.699 (−5.215) |
−9.167 (−7.33) |
−4.431 (−4.325) |
−3.422 (−5.902) |
−4.076 (−5.221) |
|
| Hospital beds, No. (SE) | 0.435 (−0.014) |
0.0352 (−0.202) |
0.393 (−0.072) |
0.0424 (−0.205) |
0.0318 (−0.203) |
0.0424 (−0.192) |
|
| NIH funding/$1000 (SE) | 0.03 (−0.00196) |
0.00208 (−0.00305) |
0.00299 (−0.00335) |
0.00188 (−0.00312) |
0.00213 (−0.003) |
0.00215 (−0.00281) |
|
| R2 | 0.873 | 0.855 | 0.872 | 0.872 | 0.872 | 0.872 |
Abbreviations: CSA, combined statistical area; NIH, National Institutes of Health.
Discussion
Unequal distribution of trial sites relative to population may impede patients’ participation in clinical studies and contribute to the well-documented low representation of minorities in certain studies.6 We found that population size explained 87% of the variability in the number of seats in industry-supported studies across nonrural regions throughout the United States. Accounting for racial demographic categories, income, NIH funding, and hospital beds did not substantively improve the bivariable model’s explanatory power. Thus, we conclude that the number of available seats in industry-sponsored trials across CSAs is largely explained by population size.
Our work has several limitations. Indication-specific differences in seat access and the distances patients are willing to travel to participate in trials were not examined. Although our methods minimized selection bias, our focus on industry-sponsored studies in CSAs limits the generalizability of our findings. In addition, the small number of CSAs (geographic units) limited our ability to explore other factors. Lastly, we could not explore time trends in trial access in this cross-sectional analysis.
Notwithstanding these limitations, we demonstrated that population size is the main determinant of the availability of industry-sponsored clinical trial seats in nonrural areas. Factors related to trial recruitment and retention, not site selection per se, are most likely responsible for remaining racial and socioeconomic inequities in trial access and participation in these regions.
References
- 1.English R, Lebovitz Y, Giffin R; Institute of Medicine (US) Forum on Drug Discovery, Development, and Translation . Transforming Clinical Research in the United States: Challenges and Opportunities: Workshop Summary. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 2.Unger JM, Vaidya R, Hershman DL, Minasian LM, Fleury ME. Systematic review and meta-analysis of the magnitude of structural, clinical, and physician and patient barriers to cancer clinical trial participation. J Natl Cancer Inst. 2019;111(3):-. doi: 10.1093/jnci/djy221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seidler EM, Heshaviah A, Brown C, et al. Geographic distribution of clinical trials may lead to inequities in access. Clin Investig. 2014;4(4):376-380. doi: 10.4155/cli.14.21 [DOI] [Google Scholar]
- 4.Bureau of Labor Statistics, US Department of Labor . Federal statistical area delineations. https://www.bls.gov/lau/lausmsa.htm. Accessed August 16, 2019.
- 5.US Office of Management and Budget . Revised delineations of metropolitan statistical areas, micropolitan statistical areas, and combined statistical areas, and guidance on uses of the delineations of these areas: OMB bulletin No. 17-01. https://www.bls.gov/bls/omb-bulletin-17-01-revised-delineations-of-metropolitan-statistical-areas.pdf. Accessed August 16, 2019.
- 6.Chen C, Wong R. Black patients miss out on promising cancer drugs. https://www.propublica.org/article/black-patients-miss-out-on-promising-cancer-drugs. Accessed December 16, 2019.