Abstract
Objective
Human oral squamous cell carcinoma (OSCC) is a major cause of mortality and morbidity worldwide. There is an urgent need to identify bioactive molecules and potential target genes that could inhibit carcinogenesis for OSCC therapy. Fisetin (3,7,3′,4′-tetrahydroxyflavone), a naturally occurring flavonoid, has been previously shown to have anti-proliferative activities in OSCC; however, its molecular mechanism is unknown.
Methods
Colony formation, cell viability, Boyden chamber, wound healing, and tumor xenograft assays were used to detect the impact of fisetin on OSCC cells in vitro and in vivo. Western blot analysis was used to examine the corresponding protein expression.
Results
Fisetin treatment significantly inhibited proliferation and promoted apoptosis by repressing PAK4 expression. Moreover, fisetin treatment attenuated cell migration by blocking PAK4 signaling pathways. In addition, the tumor xenograft showed anti-tumor growth effects of fisetin exposure in vivo.
Conclusion
Fisetin may represent a potential therapeutic strategy for human OSCC by targeting PAK4 signaling pathways.
Keywords: OSCC, fisetin, PAK4, PARP
Introduction
Oral squamous cell carcinoma (OSCC) is a common malignancy of the head and neck, with more than 354,900 newly diagnosed cases each year worldwide, arising from the mucosal epithelium of the oral cavity and oropharynx.1,2 The development of OSCC is a complex multistep process, and the main potential risk factors including smoking,3 drinking,3,4 and human papillomavirus.5–7 Cancer therapy has improved rapidly over the past decade, in particular, advanced radiotherapy with or without chemotherapy, enhanced surgical procedures, and immunotherapy. However, there is a lack of accurate and effective biomarkers and small-molecule compounds for the diagnosis and treatment of OSCC.8
The PAK (p21-activated kinase) protein family in mammals is composed of six conserved Ser/Thr protein kinases that are involved in the regulation of cell survival, cell proliferation, and the actin cytoskeleton reorganization.9,10 They can be subdivided into two groups: group I (PAK1–3) and group II (PAK4–6). PAK4 is a downstream regulator of the HGF/Met receptor tyrosine kinase signaling pathway and is associated with cell proliferation, invasion, and remodeling of the actin cytoskeleton.11,12 PAK4 is involved in tumorigenesis in vitro and in vivo, and shows overexpression, nuclear localization, and abnormal amplification in numerous cancer cell lines and tumor tissues.13 For example, downregulating PAK4 expression with the novel PAK4 inhibitor LC-0882 reduced the proliferation of human gastric cancer cells by repressing cyclin D1 expression.14 In human breast cancer cells, PAK4 can mediate cell proliferation, via the stability of p57(Kip2), through the ubiquitin-proteasome pathway.15 Furthermore, several lines of evidence show that PAK4 overexpression promotes proliferation and/or survival of OSCC cells,16 and no significantly innovative therapy way was covered about OSCC biology.
Fisetin (3,3ʹ,4ʹ,7-tetrahydroxyflavone) is a naturally occurring flavonoid found in numerous vegetables and fruits, including apple, onion, grape, cucumber, persimmon, and strawberry.17–19 It was recently reported to have anti-proliferative and apoptotic activity in various cancer cell lines, including human head and neck cancer, osteosarcoma, breast cancer, and renal cancer stem cell, suggesting that it could be used as a novel anti-cancer agent.20–23 We previously confirmed that fisetin inhibited malignant proliferation in human OSCC by blocking the Met/Src signaling pathway.24 However, no crucial downstream molecular targets for the anti-proliferation effect of fisetin in OSCC have yet been identified.
Here, our data show that fisetin significantly reduces proliferation and induces apoptosis in PAK4-overexpressing OSCC cells in vitro and in vivo. Based on these results, we conclude that targeting PAK4 with fisetin represents a potential therapeutic strategy for human OSCC.
Materials and Methods
Cell Culture
SCC9 and SCC4 human oral squamous cell carcinoma cell lines were purchased from Cobioer Biotechnology Co., Ltd. (Nanjing, China), and the Tca8113 cell line was purchased from Shanghai GeneChem Co., Ltd. (Shanghai, China). Cells were maintained in DMEM/F-12 (Life, Shanghai, China) with 400 ng/mL hydrocortisone, antibiotics (100 U/mL penicillin and 100 U/mL streptomycin), and 10% Gibco fetal bovine serum (FBS, Thermo Fisher Scientific, Shanghai, China) at 37 °C with 5% CO2 in an incubator.
Chemical Treatment
Fisetin (S2298, purity: 97.76%, Selleck & Bimake, Shanghai, China) was dissolved at a concentration of 100 mM in dimethyl sulfoxide (DMSO) as a stock solution (stored at −80°C), and at concentrations from 2 to 80 μM in DMEM/F-12 or corn oil as a working solution. Cells were plated in standard DMEM/F-12 in 24-well or six-well dishes. Twenty-four hours after plating, cells were treated for another 24 h with the indicated concentration of fisetin and then lysed for Western blot detection. Control cultures received the same volume of DMSO.
Immunoblotting
Cells were washed with cold phosphate-buffered saline (PBS) before being lysed in RIPA Lysis and Extraction Buffer (Thermo Fisher Scientific, Shanghai, China) containing protease inhibitor cocktail (Roche, Basel, Switzerland). Cell proteins were separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis and transferred to polyvinylidene fluoride membranes (Millipore, Billerica, MA, USA). Membranes were probed with specific primary antibodies and then with peroxidase-conjugated secondary antibodies. The bands were visualized by chemiluminescence (Tanon, Shanghai, China). The following antibodies were used: antibodies to PAK4 (1:2000; Cell Signaling, # 3242); PARP (1:1000; Cell Signaling, # 9542); caspase-3 (1:1000; Cell Signaling, #9662); β-actin (1:1000; Cell Signaling, #4970); GAPDH (1:10,000; Shanghai Kangchen, KC-5G4). β-actin and GAPDH were used as equal loading controls. The ImageJ software (National Institutes of Health, Bethesda, MD, USA) was used for densitometric analyses of Western blots, and the quantification results were normalized to the loading control.
Lentivirus Production and Infection
To stably overexpress PAK4, recombinant PAK4-lentivirus was purchased from Shanghai GeneChem Company (Shanghai, China). The commercial lentivirus was used to infect Tca8113, SCC4, and SCC9 cells in a 12-well plate with 3 mg/mL polybrene, followed by selection with puromycin (1.5 μg/mL). Infected Tca8113, SCC4, and SCC9 cells were identified by Western blotting.
Flat Plate Clone Formation
The complete medium was removed from culture dishes, and cells were washed with 1x PBS. Next, 1 mL 0.25% trypsin was added for 1–2 min, and cells were pipetted to form a single-cell suspension with the addition of complete medium. Cells were spun at 200 x g for 5 min and resuspended in complete medium, after which cells were counted and the concentration adjusted to 50 cells/mL. In six-well cell culture plates, 2 mL (50 cells/mL) of complete cell medium was added and mixed until homogeneous. The cells were treated with DMSO (control group) or fisetin (2 or 5 μM). After 2–3 weeks of culture, cell morphology was observed. Then, cells were fixed with absolute ethanol and stained with crystal violet. The numbers of cell colonies were counted using the ImageJ software.
Cell Cycle
Cells were incubated with the indicated concentrations of fisetin (10 or 20 μM) for 24 h. After incubation, cells were collected, washed with PBS, and then suspended in propidium iodide (PI) staining solution with RNase (BD Biosciences, San Jose, CA, USA). The cells were analyzed using a Becton-Dickinson FACS Vantage flow cytometer (Becton Dickinson, San Jose, CA, USA).
Migration Assay
For the migration assays, 1 × 105 cells with 200 μL DMEM/F-12 medium (1% FBS) were seeded onto transwell upper chambers (Corning Costar, USA) with a pore size of 8.0 μm, and 600 μL DMEM/F-12 medium (20% FBS) was added to the lower chamber. After 24 h incubation at 37 °C, cells were fixed with 4% paraformaldehyde and stained with 0.4% trypan blue. Cells in the upper chambers were gently removed with cotton swabs, then numbers of cells were counted. Three independent experiments were performed, and the data are presented as mean ± standard deviation.
Scratch Assay
Tca8113-PAK4-overexpressing cells were seeded into 24-well tissue culture plates at a density such that after 24 h of growth, they reached ~70–80% confluence as a monolayer. A wound was created by gently and slowly scratching the monolayer with a sterile 200 μL pipette tip across the center of the well. After scratching, the well was gently washed twice with medium to remove detached cells. Images were acquired immediately after scratching at 0 h and after 24 h incubation at 37 °C.
Xenograft Mouse Model
For the in vivo study, 4-week-old athymic nude mice (BALB/c) were randomly divided into two groups with oral gavage administration: a corn oil control group and fisetin treatment groups. All the experiments with mice were conducted strictly in accordance with the Animal Welfare Act approved by the Ethics Committee of China Medical University. For subcutaneous xenografts, 1 × 105 PAK4-overexpressing SCC9 cells were injected into the right flank area of nude mice. Tumor weights were measured for 30 days.
Statistical Analysis
All experiments included at least three independent biological assays (n ≥ 3), and the results are presented as mean ± standard deviation. Statistical analyses were performed using GraphPad Prism v6.0 (GraphPad Software, Inc. San Diego, CA, USA) or SPSS 17.0. To assess the statistical significance of the differences in protein expression of PAK4 and other related proteins between DMSO-treated and fisetin-treated SCC-4/9 cells, the Student’s t-test (two-tailed) was performed. For clone formation, transwell, and wound healing assays, statistical differences between groups treated with DMSO or fisetin (2 or 5μM) were determined using one-way analysis of variance. The results were considered to be significant when the P-value was less than 0.05 (*< 0.05, **< 0.01, ***< 0.001). Corresponding significance levels are indicated in the figures.
Results
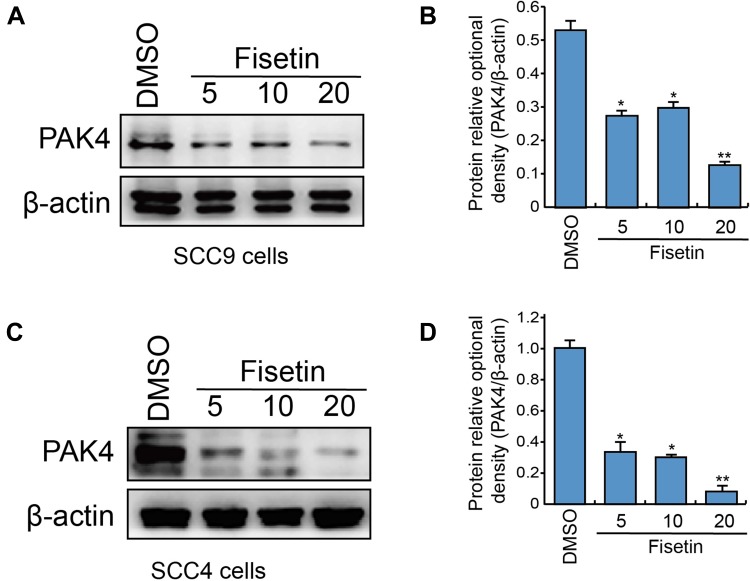
Fisetin Downregulates PAK4 Expression in OSCC Cell Lines
Our results showed a marked inhibition of hepatocyte growth factor receptor (c-Met)/Src signaling by fisetin treatment;24 however, whether this affected the c-Met/Src downstream effector PAK4 remained unclear. For this purpose, SCC9 and SCC4 cells were treated with 5, 10, and 20 μM fisetin for 24 h using Western blot analysis (Figure 1A and C and Supplementary Figure 1). The gray value ratios of PAK4/β-actin are shown in Figure 1B and D, respectively. Fisetin strongly suppressed the expression of PAK4 protein in both SCC9 and SCC4 cells, with decreases of 76% and 92%, respectively, in the 20 μM fisetin treatment group compared with the control DMSO group. These results suggest that fisetin inhibits PAK4 expression in OSCC.
Figure 1.
Fisetin reduced PAK4 protein expression in SCC9 and SCC4 cells.
Notes: (A and C) SCC9 and SCC4 cells were treated with fisetin (5, 10, and 20 μM) for 24 h. Western blotting was carried out to detect PAK4 protein expression, with β-actin used as a loading control. The gray value ratios of PAK4/β-actin protein are shown in (B and D), respectively. *P < 0.05, **P < 0.01 vs DMSO (Student’s t-test, n=3).
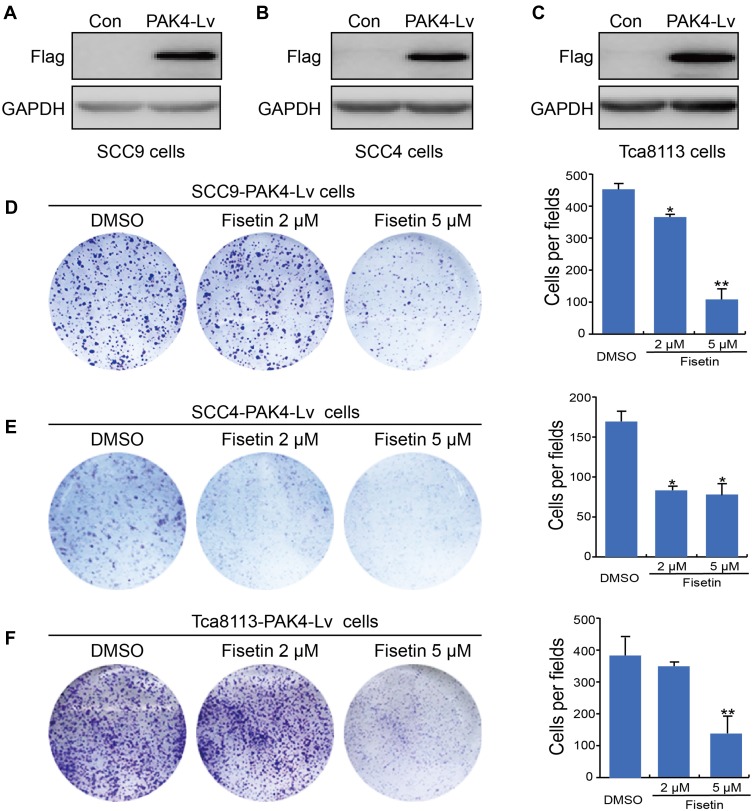
Fisetin Inhibits Colony Formation of PAK4-Overexpressing OSCC Cells
We confirmed that the expression of PAK4 protein was downregulated by fisetin in two OSCC cell lines (SCC4 and SCC9). It has been reported that high levels of PAK4 protein promote the proliferation and/or survival of OSCC cells.16 To conform that fisetin is a novel downregulator of PAK4, we screened OSCCs stably overexpressing PAK4. Flag-PAK4-Lv was ectopically expressed in SCC9, SCC4, and Tca8113 cell lines, which showed increased malignancy (Figure 2A–C). By use of colony formation assays, we found that fisetin significantly suppressed the colony formation of PAK4-overexpressing OSCC cells: in SCC9 cells, the number of clones decreased by 19% and 76%, respectively; in SCC4 cells, the number of clones decreased by 50% and 53%, respectively; and in the Tca8113 cell line, the number of clones decreased by 19% and 76%, respectively (Figure 2D–F and Supplementary Figure 2).
Figure 2.
Fisetin inhibits the proliferation of PAK4-overexpressing OSCC cells.
Notes: Western blot results showing that PAK4-lentivirus (PAK4-Lv) infection markedly increases protein levels in (A) SCC9, (B) SCC4, and (C) Tca8113. (D) SCC9-PAK4-Lv, (E) SCC4-PAK4-Lv, and (F) Tca8113-PAK4-Lv cells stably expressing PAK4 protein were treated with fisetin (2 and 5 µM) for 7 days. The numbers of cell colonies were counted with ImageJ. Data are presented in the histogram as mean ± standard deviation (n=3). *P < 0.05, **P < 0.01 vs. DMSO.
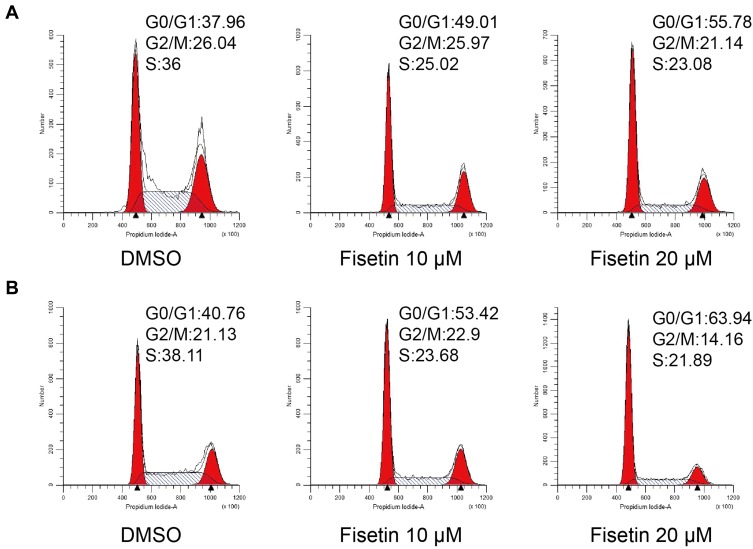
Fisetin Inhibits the Cell Cycle in PAK4-Overexpressing OSCC Cells
To assess the cell cycle status of PAK4-overexpressing OSCC cells, we analyzed their DNA content using FACS (Figure 3A and B). PI staining was performed after treatment of SCC9-PAK4-Lv and SCC4-PAK4-Lv cells with different concentrations of fisetin for 24 h. The percentage of cells with a 2C compliment appeared to increase in the G0/G1-phase, with fewer cells having a full 4C compliment in G2/M-phase and S-phase. These data indicate that fisetin inhibits the cell cycle in PAK4-overexpressing cells, possibly via delayed progression through the G2/M and S-phase.
Figure 3.
Fisetin inhibits the cell cycle of PAK4-overexpressing OSCC cells.
Notes: (A) SCC9-PAK4-Lv and (B) SCC4-PAK4-Lv cells treated with fisetin were subjected to flow cytometry analysis. SCC9 and SCC4 cells were treated with 10 and 20 μM of fisetin, respectively, for 24 h. The percentages of cells in the G0/G1, S, and G2/M phases are shown in the graphs.
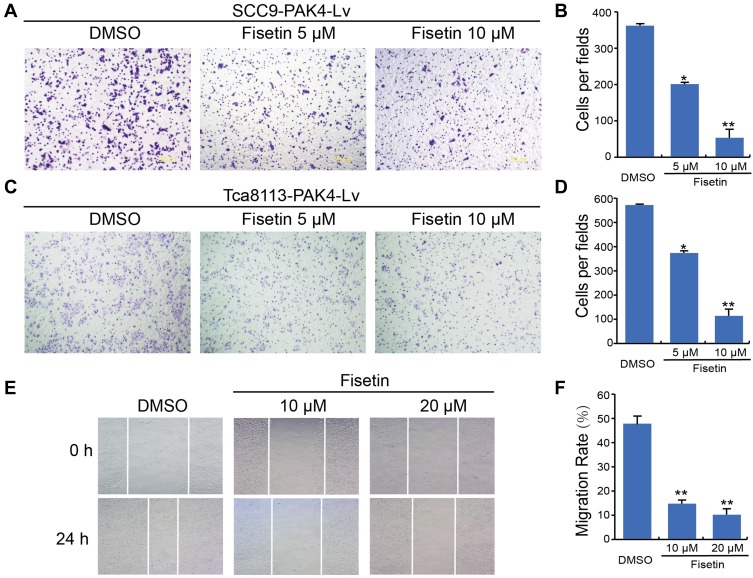
Fisetin Inhibits Migration of PAK4-Overexpressing OSCC Cells
To evaluate the effects of fisetin on the migratory properties of PAK4-overexpressing OSCC cells, we performed transwell migration assays and wound healing assays. In the transwell migration assay without Matrigel, the SCC9-PAK4-Lv and Tca8113-PAK4-Lv cells treated with fisetin (5 μM and 10 μM) displayed reduced migration ability compared with DMSO control cells (Figure 4A–D). The results of the wound healing assays indicated that the migration rate of Tca8113-PAK4-Lv cells with DMSO control was 48.37 ± 2.01%, higher than the rates observed for cells treated with 10 μM fisetin (16.33 ± 1.23%) and 20 μM fisetin (12.01 ± 1.31%). This suggested that fisetin inhibited the migration of Tca8113-PAK4-Lv cells (Figure 4E and F).
Figure 4.
Fisetin inhibits the migration of PAK4-overexpressing OSCC cells.
Notes: (A and C) Migration abilities of SCC9-PAK4-Lv and Tca8113-PAK4-Lv cells treated with fisetin were evaluated using the transwell system. (B and D) The numbers of migrating cells were counted and analyzed. *P < 0.05, **P < 0.01 vs. control. (E) Wound-healing assay performed with DMSO control and fisetin-treated Tca8113-PAK4-Lv cells. Scale bar = 200μm. Representative images were obtained at the indicated concentrates for 24 h. (F) The statistical graphs in the right panel indicate the average number of cells per field (**P < 0.01, compared with DMSO).
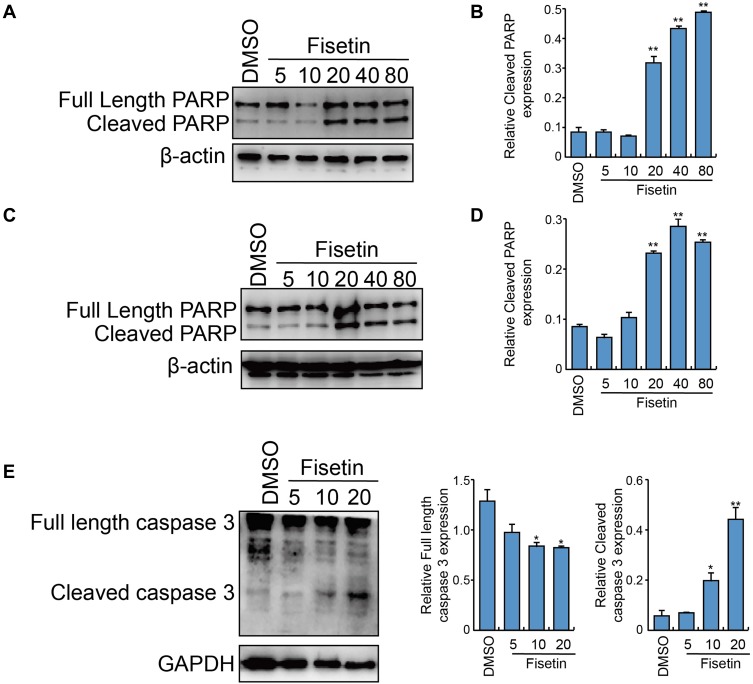
Fisetin Induces Cleavage of Caspase 3 and PARP in PAK4-Overexpressing OSCC Cells
Next, we investigated whether fisetin treatment induced apoptosis in PAK4-overexpressing OSCC cells, by examining activation of cleavage of PARP and caspase 3, which are hallmarks of apoptosis. SCC9-PAK4-Lv (Figure 5A and B and Supplementary Figure 3) and SCC4-PAK4-Lv cells (Figure 5C and D and Supplementary Figure 3) were treated with increasing concentrations of fisetin for 24 h. Western blot analysis demonstrated increased cleavage of PARP. In addition, as shown in Figure 5E and Supplementary Figure 3, fisetin treatment of SCC9-PAK4-Lv cells increased the cleavage of caspase 3 fragments.
Figure 5.
Effect of fisetin treatment on cleavage of caspase 3 and PARP in PAK4-overexpressing OSCC cells.
Notes: After treatment with the indicated concentration of fisetin for 24 h, (A) SCC9-PAK4-Lv and (C) SCC4-PAK4-Lv cells were harvested, whole cells were lysed, and the expression of full-length and cleaved PARP was determined. β-actin was used as a loading control. Expression of cleaved PARP was measured with ImageJ; the relative cleaved PARP/β-actin ratios are shown in (B and D). **P < 0.01 vs. DMSO. (E) In SCC9-PAK4-Lv cells, the expression of full-length and cleaved caspase 3 was detected. GAPDH was used as a loading control protein. The statistical graphs are shown in the right panel (*P < 0.05 and **P < 0.01, compared with DMSO).
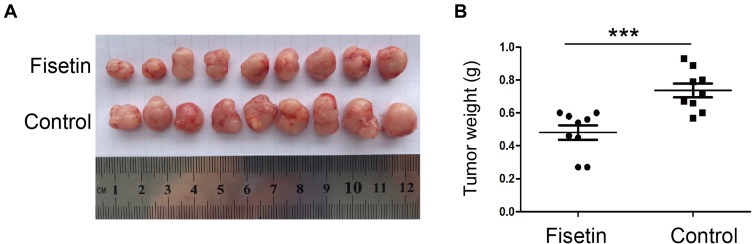
Fisetin Inhibits Growth of OSCC in vivo
To evaluate the anti-proliferation potential of fisetin in vivo, we used a xenograft tumor model bearing SCC9-PAK4-Lv cells. The primary tumors isolated from fisetin-treated mice exhibited a dramatic decrease in tumor growth (Figure 6A and B) compared with the control group.
Figure 6.
Fisetin retarded tumor formation in vivo.
Notes: (A) Nude mice were subcutaneously inoculated with 1×105 SCC9-PAK4-Lv cells, and tumor formation was monitored. Beginning on day 5, mice received oral gavage with the control (corn oil) or fisetin at a dose of 10 mg/kg/d. (B) Tumor weights were calculated at day 30 (***P < 0.001, fisetin group: n = 9, control group: n = 9).
Discussion
In this study, we showed that fisetin negatively regulates the expression of PAK4 in OSCC cell lines. This implied a significant role for fisetin in OSCC interventions. Then, we constructed three OSCC cell lines stably expressing PAK4, using lentivirus infection of SCC9, SCC4, and Tca8113 cells. Fisetin restrained proliferation and migration and prompted apoptosis of PAK4-overexpressing OSCC. In addition, experiments in vivo showed that fisetin reduced tumor size in nude mice. Furthermore, the PAK4 pathway may be blocked by fisetin in OSCC.
In the present study, we sought to investigate the function and underlying mechanisms of fisetin in OSCC. PAK4 was upregulated in OSCC tissues and cell lines and was significantly associated with a poorer prognosis.16 Downregulation of PAK4 inhibited the proliferation, migration, and invasion of cells.14,25 PAK4 is recruited to and activated by c-Met, which is associated with cancer cell motility and invasiveness;12 thus, it represents a good diagnostic and therapeutic target for OSCC. Fisetin, a dietary flavonoid, has been shown to function as a novel anti-cancer agent in several types of cancer cells.26 Our previous studies demonstrated that fisetin could be used in potential therapeutic strategies for human OSCC by blocking the Met/Src signaling pathway.24 Most importantly, oral administration of fisetin reduces tumorigenesis in mouse models of human OSCC with overexpression of PAK4.
The oncogene PAK4 shows elevated expression in various cancer cell lines and tumor tissues, making it a promising drug target.27 Several small molecules have been developed to inhibit PAK4 kinase activity, including PF-3758309,28,29 LCH-7749944,30,31 GNE-2861,32 GL-1196,25 and LC-0882.14 Only KPT-9274, a unique small-molecule inhibitor, can reduce the level of PAK4 protein expression.33 Studies have shown that PAK4 has functions that are independent of its kinase activity. Therefore, inhibition of PAK4 protein affects various biological processes of cancer cells, including cell survival, proliferation, invasion, and metastasis. Fisetin, like KPT-9274, can reduce levels of PAK4 protein, possibly through the C-Met/Src signaling pathway in OSCC.
Despite advances in diagnostic and treatment methods, OSCC remains a disease with high morbidity and mortality.34 In consequence, therapies targeting OSCC-related biomarkers have become a research hotspot.35,36 Our previous work indicated that fisetin could play an important part in such therapeutic strategies. However, the results of clinical trial design for therapy of patients with OSCC remains unclear. Therefore, further studies are needed to validate our findings in a patient-derived xenograft model. Functional investigations are also required to explore the molecular mechanisms of fisetin in OSCC cancer progression, so as to provide a precise understanding of fisetin function in the clinical therapeutics of OSCC.
In conclusion, our study highlights the role of fisetin in suppressing the malignant proliferation and migration of OSCC cells by targeting PAK4. Our results provide insight into the therapeutic value of fisetin in reducing OSCC differentiation and inducing OSCC cell apoptosis, possibly through PAK4 signaling pathways.
Funding
This work was supported by the Project of Natural Science Foundation of Liaoning Province (2015020528, 20180530037), and by grants from the National Natural Science Foundation of China (No. 81902701) and College Students’ Innovation and Entrepreneurship Training Projects (201910159001 and 201910159084).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–1953. doi: 10.1002/ijc.v144.8 [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 3.Mello FW, Melo G, Pasetto JJ, Silva CAB, Warnakulasuriya S, Rivero ERC. The synergistic effect of tobacco and alcohol consumption on oral squamous cell carcinoma: a systematic review and meta-analysis. Clin Oral Investig. 2019;23(7):2849–2859. doi: 10.1007/s00784-019-02958-1 [DOI] [PubMed] [Google Scholar]
- 4.Vucicevic Boras V, Fucic A, Virag M, et al. Significance of stroma in biology of oral squamous cell carcinoma. Tumori. 2018;104(1):9–14. doi: 10.5301/tj.5000673 [DOI] [PubMed] [Google Scholar]
- 5.Jiang S, Dong Y. Human papillomavirus and oral squamous cell carcinoma: a review of HPV-positive oral squamous cell carcinoma and possible strategies for future. Curr Probl Cancer. 2017;41(5):323–327. doi: 10.1016/j.currproblcancer.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 6.Hubbers CU, Akgul B. HPV and cancer of the oral cavity. Virulence. 2015;6(3):244–248. doi: 10.1080/21505594.2014.999570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gharat SA, Momin M, Bhavsar C. Oral squamous cell carcinoma: current treatment strategies and nanotechnology-based approaches for prevention and therapy. Crit Rev Ther Drug Carrier Syst. 2016;33(4):363–400. doi: 10.1615/CritRevTherDrugCarrierSyst.2016016272 [DOI] [PubMed] [Google Scholar]
- 8.Sparger EE, Murphy BG, Kamal FM, et al. Investigation of immune cell markers in feline oral squamous cell carcinoma. Vet Immunol Immunopathol. 2018;202:52–62. doi: 10.1016/j.vetimm.2018.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eswaran J, Li DQ, Shah A, Kumar R. Molecular pathways: targeting p21-activated kinase 1 signaling in cancer–opportunities, challenges, and limitations. Clin Cancer Res. 2012;18(14):3743–3749. doi: 10.1158/1078-0432.CCR-11-1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Y, Zhang H, Zhao Y, et al. A mandatory role of nuclear PAK4-LIFR axis in breast-to-bone metastasis of ERalpha-positive breast cancer cells. Oncogene. 2019;38(6):808–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paliouras GN, Naujokas MA, Park M. Pak4, a novel Gab1 binding partner, modulates cell migration and invasion by the Met receptor. Mol Cell Biol. 2009;29(11):3018–3032. doi: 10.1128/MCB.01286-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whale AD, Dart A, Holt M, Jones GE, Wells CM. PAK4 kinase activity and somatic mutation promote carcinoma cell motility and influence inhibitor sensitivity. Oncogene. 2013;32(16):2114–2120. doi: 10.1038/onc.2012.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang C, Li Y, Zhang H, et al. Oncogenic PAK4 regulates Smad2/3 axis involving gastric tumorigenesis. Oncogene. 2014;33(26):3473–3484. doi: 10.1038/onc.2013.300 [DOI] [PubMed] [Google Scholar]
- 14.Zhang HY, Zhang J, Hao CZ, et al. LC-0882 targets PAK4 and inhibits PAK4-related signaling pathways to suppress the proliferation and invasion of gastric cancer cells. Am J Transl Res. 2017;9(6):2736–2747. [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y, Wang D, Zhang H, et al. P21-activated kinase 4 regulates the cyclin-dependent kinase inhibitor p57(kip2) in human breast cancer. Anat Rec. 2013;296(10):1561–1567. doi: 10.1002/ar.22754 [DOI] [PubMed] [Google Scholar]
- 16.Begum A, Imoto I, Kozaki K, et al. Identification of PAK4 as a putative target gene for amplification within 19q13.12-q13.2 in oral squamous-cell carcinoma. Cancer Sci. 2009;100(10):1908–1916. doi: 10.1111/cas.2009.100.issue-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sundarraj K, Raghunath A, Perumal E. A review on the chemotherapeutic potential of fisetin: in vitro evidences. Biomed Pharmacother. 2018;97:928–940. doi: 10.1016/j.biopha.2017.10.164 [DOI] [PubMed] [Google Scholar]
- 18.Rengarajan T, Yaacob NS. The flavonoid fisetin as an anticancer agent targeting the growth signaling pathways. Eur J Pharmacol. 2016;789:8–16. doi: 10.1016/j.ejphar.2016.07.001 [DOI] [PubMed] [Google Scholar]
- 19.Maher P. Protective effects of fisetin and other berry flavonoids in parkinson’s disease. Food Funct. 2017;8(9):3033–3042. doi: 10.1039/C7FO00809K [DOI] [PubMed] [Google Scholar]
- 20.Won DH, Chung SH, Shin JA, et al. Induction of sestrin 2 is associated with fisetin-mediated apoptosis in human head and neck cancer cell lines. J Clin Biochem Nutr. 2019;64(2):97–105. doi: 10.3164/jcbn.18-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fu CY, Chen MC, Tseng YS, et al. Fisetin activates hippo pathway and JNK/ERK/AP-1 signaling to inhibit proliferation and induce apoptosis of human osteosarcoma cells via ZAK overexpression. Environ Toxicol. 2019;34(8):902–911. doi: 10.1002/tox.22761 [DOI] [PubMed] [Google Scholar]
- 22.Guo G, Zhang W, Dang M, Yan M, Chen Z. Fisetin induces apoptosis in breast cancer MDA-MB-453 cells through degradation of HER2/neu and via the PI3K/Akt pathway. J Biochem Mol Toxicol. 2019;33(4):e22268. doi: 10.1002/jbt.2019.33.issue-4 [DOI] [PubMed] [Google Scholar]
- 23.Si Y, Liu J, Shen H, et al. Fisetin decreases TET1 activity and CCNY/CDK16 promoter 5hmC levels to inhibit the proliferation and invasion of renal cancer stem cell. J Cell Mol Med. 2019;23(2):1095–1105. doi: 10.1111/jcmm.2019.23.issue-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li YS, Qin XJ, Dai W. Fisetin suppresses malignant proliferation in human oral squamous cell carcinoma through inhibition of Met/Src signaling pathways. Am J Transl Res. 2017;9(12):5678–5683. [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang J, Zhang HY, Wang J, et al. GL-1196 suppresses the proliferation and invasion of gastric cancer cells via targeting PAK4 and inhibiting PAK4-mediated signaling pathways. Int J Mol Sci. 2016;17(4):470. doi: 10.3390/ijms17040470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sabarwal A, Agarwal R, Singh RP. Fisetin inhibits cellular proliferation and induces mitochondria-dependent apoptosis in human gastric cancer cells. Mol Carcinog. 2017;56(2):499–514. doi: 10.1002/mc.v56.2 [DOI] [PubMed] [Google Scholar]
- 27.Rane C, Senapedis W, Baloglu E, et al. A novel orally bioavailable compound KPT-9274 inhibits PAK4, and blocks triple negative breast cancer tumor growth. Sci Rep. 2017;7:42555. doi: 10.1038/srep42555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang K, Huynh N, Wang X, et al. PAK inhibition by PF-3758309 enhanced the sensitivity of multiple chemotherapeutic reagents in patient-derived pancreatic cancer cell lines. Am J Transl Res. 2019;11(6):3353–3364. [PMC free article] [PubMed] [Google Scholar]
- 29.Murray BW, Guo C, Piraino J, et al. Small-molecule p21-activated kinase inhibitor PF-3758309 is a potent inhibitor of oncogenic signaling and tumor growth. Proc Natl Acad Sci U S A. 2010;107(20):9446–9451. doi: 10.1073/pnas.0911863107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang J, Wang J, Guo Q, et al. LCH-7749944, a novel and potent p21-activated kinase 4 inhibitor, suppresses proliferation and invasion in human gastric cancer cells. Cancer Lett. 2012;317(1):24–32. doi: 10.1016/j.canlet.2011.11.007 [DOI] [PubMed] [Google Scholar]
- 31.Guo Q, Su N, Zhang J, et al. PAK4 kinase-mediated SCG10 phosphorylation involved in gastric cancer metastasis. Oncogene. 2014;33(25):3277–3287. doi: 10.1038/onc.2013.296 [DOI] [PubMed] [Google Scholar]
- 32.Zhuang T, Zhu J, Li Z, et al. p21-activated kinase group II small compound inhibitor GNE-2861 perturbs estrogen receptor alpha signaling and restores tamoxifen-sensitivity in breast cancer cells. Oncotarget. 2015;6(41):43853–43868. doi: 10.18632/oncotarget.v6i41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abu Aboud O, Chen CH, Senapedis W, Baloglu E, Argueta C, Weiss RH. Dual and specific inhibition of NAMPT and PAK4 by KPT-9274 decreases kidney cancer growth. Mol Cancer Ther. 2016;15(9):2119–2129. doi: 10.1158/1535-7163.MCT-16-0197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lauritano D, Lucchese A, Contaldo M, et al. Oral squamous cell carcinoma: diagnostic markers and prognostic indicators. J Biol Regul Homeost Agents. 2016;30(2 Suppl 1):169–176. [PubMed] [Google Scholar]
- 35.Rivera C, Oliveira AK, Costa RAP, De Rossi T, Paes Leme AF. Prognostic biomarkers in oral squamous cell carcinoma: a systematic review. Oral Oncol. 2017;72:38–47. doi: 10.1016/j.oraloncology.2017.07.003 [DOI] [PubMed] [Google Scholar]
- 36.Cuevas-Nunez MC, Gomes CBF, Woo SB, et al. Biological significance of 5-hydroxymethylcytosine in oral epithelial dysplasia and oral squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(1):59–73.e52. doi: 10.1016/j.oooo.2017.06.006 [DOI] [PubMed] [Google Scholar]