Abstract
Primary hyperparathyroidism is not commonly diagnosed during pregnancy. For pregnant women with mild, asymptomatic disease, surgery can be avoided unless the degree of hypercalcemia becomes more severe or they develop complications. However, there are no evidence-based guidelines to assist clinicians regarding the management of primary hyperparathyroidism during pregnancy. When surgery is deemed necessary during pregnancy, the second trimester is generally considered to be the optimal time. We report the case of a 31-year-old female G1P0 who presented at 6 weeks gestation with symptoms of nausea, vomiting, polyuria, and corrected calcium of 14.8 mg/dL. Due to the extreme degree of hypercalcemia and refractory to medical treatment, it was decided that surgery could not be delayed until the second trimester. At 7w3d gestational age the patient had resection of a 37 gram, 5 × 4 × 3 cm right inferior parathyroid adenoma.
Keywords: hyperparathyroidism, parathyroidectomy, hypercalcemia, pregnancy, first trimester
Primary hyperparathyroidism is not commonly diagnosed during pregnancy [1–2]. For nonpregnant individuals the definitive treatment is surgery when there are significant elevations of the serum calcium or complications of the disease. For those with mild, asymptomatic disease, surgery can be avoided unless the degree of hypercalcemia becomes more severe or they develop complications [3–6]. There are published guidelines when surgery is recommended for men and nonpregnant patients with hyperparathyroidism [4]. Clearly, any decision regarding surgery for a pregnant woman with primary hyperparathyroidism is more complex than in men or nonpregnant women and there are no evidence-based guidelines to assist clinicians regarding the management of primary hyperparathyroidism during pregnancy.
Hypercalcemia during pregnancy has been associated with increased maternal and fetal morbidity and mortality. Maternal complications include nephrolithiasis, pancreatitis, hyperemesis gravidarum, preeclampsia, and hypercalcemic crises [7, 8]. Maternal hypercalcemia also increases the risk of perinatal complications primarily due to an increased frequency of miscarriages and neonatal hypocalcemia and tetany [2, 7, 9–11]. When surgery is deemed necessary during pregnancy, the second trimester is generally considered to be the optimal time [8, 11, 12].
We report the case of a 31-year-old female G1P0 who presented at 6 weeks gestation with symptomatic hypercalcemia and a corrected calcium of 14.8 mg/dL. Due to the extreme degree of hypercalcemia and refractory to medical treatment, it was decided that surgery could not be delayed until the second trimester. At 7w3d gestational age the patient underwent a parathyroidectomy.
1. Case Report
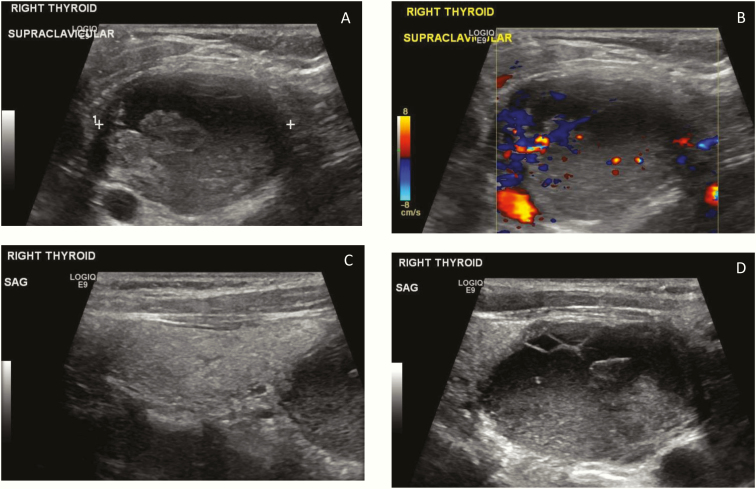
A 31-year-old female G1P0 presented at 6 weeks gestation with a 2-week history of nausea, vomiting, polyuria, constipation, and generalized weakness. Her serum calcium was 14.1 mg/dL (8.5–10.1 mg/dl), albumin was 3.2 g/dL (3.4–5.0 g/dL), corrected calcium was 14.8 mg/dL, phosphorus was 1.6 mg/dL (2.5–4.9 mg/dL), and had a PTH of 850.5 pg/mL (18.5–88 pg/mL). Additional studies included a 25-OH vitamin D <4.2 ng/mL (sufficient 30–100 ng/mL), 1,25-dihydroxyvitamin D >200 pg/mL (20.0–82.0 pg/mL), procollagen type 1 N-terminal propeptide level of 164 mcg/L (19–83 mcg/L), and serum C-telopeptide level of 4416 pg/mL (premenopausal women 34–635 pg/mL) (Table 1). Treatment was started with 1000 units of vitamin D3. An ultrasound of the neck demonstrated a large 2.9 × 3.9 × 4.7 cm complex mass at the lower pole of the right thyroid with mixed solid and cystic components that appeared to be separate from the right thyroid lobe and located posterior to the lower pole (Fig. 1A–1D). She was started on calcitonin and aggressive intravenous fluid therapy but developed tachyphylaxis to calcitonin. She remained significantly hypercalcemic with corrected calcium levels ranging between 11.1 to 13.3 mg/dL. Treatment with a bisphosphonate and cinacalcet were considered but not administered because of the lack of safety data regarding potential fetal complications when used during pregnancy, particularly in the first trimester.
Table 1.
Laboratory Test Results
| Test | 06/06/18 | 07/16/18 | 10/01/18 | 01/07/19 | 04/01/19 | Reference rangea |
|---|---|---|---|---|---|---|
| PTH | 850 | 48.0 | 91.6 | 15.7 | 62.7 | 18.5–88.0 pg/mL |
| 25-OH vitamin D | <4.2 | 13.3 | 24.2 | 20.5 | 29.3 | 30–100 ng/mL |
| 1,25 (OH)2 vitamin D | >200 | >200 | 179 | 53.8 | 71.9 | 20–82 pg/mL |
| P1NP | 164 | 241 | 124 | 39 | 53 | 19–83 mcg/L |
| BSAP | 43.2 | 34.3 | 12.2 | 10.3 | 11.6 | 4.5–16.9 mcg/L |
| CTX | 4416 | 802 | 551 | 226 | 296 | 34–635 pg/mL |
The parathyroidectomy was performed on 06/11/2018.
Abbreviations: BSAP, bone specific alkaline phosphatase; CTX, C-telopeptide; P1NP, procollogen type 1 N-terminal propeptide; PTH, Parathyroid hormone.
aReference range is for nonpregnant individuals.
Figure 1.
Ultrasound images demonstrating a large 2.9 × 3.9 × 4.7 cm complex mass at the lower pole of the right thyroid in the supraclavicular area with mixed solid and cystic components that proves to be the parathyroid adenoma. The mass on sagittal images appears to be separate from the right thyroid lobe and located posterior to the lower pole. A: Transverse image, right lower neck. B: Transverse image right lower neck with Doppler. C: Sagittal image demonstrating a normal right thyroid lobe with the complex mass at the inferior border of the thyroid. D: Sagittal image of the complex mass.
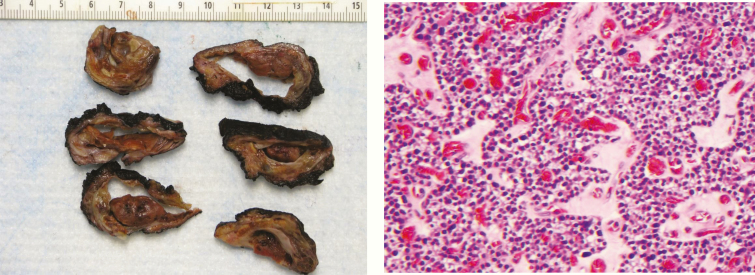
At a multidisciplinary conference that included endocrinology, maternal–fetal medicine, and otolaryngology-head and neck surgery, it was decided that due to the extreme degree of hypercalcemia that surgery could not be delayed until the second trimester. At 7w3d gestational age the patient underwent a parathyroidectomy with removal of a 37 gram right inferior parathyroid gland. The intraoperative PTH decreased from 807.1 to 35.5 pg/mL. The pathology demonstrated a parathyroid adenoma with nuclear atypia and 1 benign lymph node. The parathyroid adenoma was composed of multiple cell types with chief cell and oncocytic elements (Fig. 2). There was focal pleomorphism in tumor cells. However, increased mitotic activity was not detected. Immunohistochemical stains for BCL-1/Cyclin D1 was negative in the tumor cells. The Ki-67 proliferation index was 5% to 7%.
Figure 2.
Gross pathology and H and E stain x200.
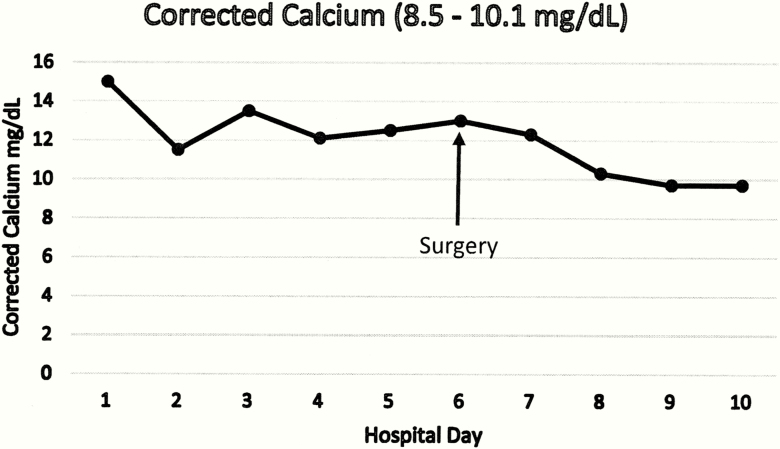
Immediately after parathyroidectomy, the patient’s calcium levels were in the reference range and there was normal fetal development and growth (Fig. 3). At the gestational age of 26w6d, the patient developed preeclampsia and a decision was made to deliver the male child by C-section. The infant’s calcium, phosphorus, and alkaline phosphatase levels were all found to be within the reference range for a newborn. He had an uneventful course in the neonatal ICU and was discharged at 2 months of age with a normal calcium.
Figure 3.
Corrected calcium (reference range 8.5–10.1 mg/dL) before and immediately after surgery
After surgery and over the next several months the patient’s calcium levels remained normal and her PTH, vitamin D levels, marker of bone resorption (CTX), and markers of bone formation (P1NP and bone specific alkaline phosphatase) returned to normal (Table 1). Genetic testing for the hyperpararthyroidism-jaw tumor syndrome did not identify a mutation of the CDC73 gene.
2. Discussion
Primary hyperparathyroidism is not an uncommon disorder, but it is rarely diagnosed during pregnancy [1, 2]. It is more common in older compared to younger women and calcium levels are not routinely measured during uncomplicated pregnancies. In addition, albumin levels are decreased during pregnancy, resulting in lower serum total but not ionized calcium. During pregnancy, identifying an increased total, albumin-corrected, or ionized calcium with a clearly elevated PTH, or one that is in the high-normal range, would be highly suspicious for the diagnosis of primary hyperparathyroidism [13].
Hypercalcemia during pregnancy is associated with an increase in maternal and fetal morbidity and mortality. Precise data concerning the complications of primary hyperparathyroidism during pregnancy are limited. Maternal morbidity rates as high as 67% have been reported and include nephrolithiasis, pancreatitis, hyperemesis gravidarum, preeclampsia, and hypercalcemic crises with nausea, vomiting, mental status changes, dehydration, uremia, and coma [7, 10, 14].
Significant maternal hypercalcemia can also increase the risk of perinatal morbidity and mortality. Perinatal mortality rates exceeding 25% have been reported [9]. Following delivery there is a high risk of neonatal hypocalcemia. Maternal hypercalcemia during pregnancy results in fetal hypercalcemia suppressing fetal parathyroid hormone secretion. Parathyroid suppression resulting in hypocalcemia may persist in the early postpartum period.
There are no randomized trials providing clinicians with information on how to optimally manage maternal primary hyperparathyroidism. The available literature is limited to case reports, small series of patients, and analytical reviews [8, 11, 15]. Medical management of hypercalcemia during pregnancy is quite limited. Maternal hypercalcemia can improve with intravenous fluids and saline diuresis combined with loop diuretics to increase urine calcium excretion. Subcutaneous calcitonin (FDA pregnancy category C) does not cross the placenta and can lower the calcium level but the benefit is typically transient since patients rapidly develop tachyphylaxis. In the past, some women were treated with phosphates but this modality should be avoided due to the risk of developing soft tissue calcifications. Intravenous bisphosphonates are commonly prescribed to lower the serum calcium in nonpregnant individuals. A few women have received intravenous bisphosphonates (FDA pregnancy category D) during pregnancy without their children having identifiable bone pathology, but there remain significant concerns about their potential toxic effects on fetal skeletal development [16, 17]. Cinacalcet is an oral calcimimetic that lowers PTH and calcium concentrations by activating the calcium sensing receptor. There are case reports of using cincalcet to treat hypercalcemia during pregnancy; however, it is an FDA class C drug for use in pregnancy and long-term safety data are lacking [18–20].
In view of the concerns and limitations of medical treatments, the major questions that emerge are whether definitive treatment with surgery during pregnancy reduces maternal and fetal complications and at what degree of hypercalcemia do the benefits of surgery outweigh the risk. The first parathyroidectomy during pregnancy was performed in 1947 [21], and since then this has proved to be a safe procedure during pregnancy when done by highly experience parathyroid surgeons [8, 11, 15]. With the selection of appropriate patients, surgery for primary hyperparathyroidism reduces the risk of fetal and maternal complications. An early series of women from 1930 to 1990 comparing those managed with and without surgery was reported by Kelly [2]. In those who did not have surgery the neonatal mortality rate was 16%, and 53% of neonates had complications. In the surgical group, 12.5% of neonates had a complication and only 2.5% died. Norman et al published data on 32 women with 77 pregnancies with primary hyperparathyroidism in 2009. All 15 women who had midtrimester parathyroidectomies delivered healthy infants, while 48% of pregnancies managed medically ended in a miscarriage. The rate of loss was directly related to the degree of hypercalcemia, exceeding 68% in those women with calcium levels greater than or equal to 11.4 mg/dL [11]
More recently, Rigg et al reported their experience managing hyperparathyroidism in 28 pregnancies in 23 women from 2000–2015 [8]. Of those managed medically, 30% had preeclampsia and 66% had a preterm delivery. Six women had surgery without complications and all carried the pregnancy to term. Only 1 newborn of a woman who did not have surgery had neonatal hypocalcemia. This data must be interpreted with caution since calcium levels were measured in the infants of only 10 of the 22 medically-managed and 2 of the 6 surgically-treated pregnancies.
Based on the available information and accumulated clinical experience, as well as balancing the risks and benefits, we agree with those who have analyzed the data and recommend surgery for primary hyperparathyroidism during pregnancy when the serum calcium exceeds 11.4 to 12.0 mg/dL [11, 22–24]. Preoperative localization of an adenoma during pregnancy remains challenging. Parathyroid scans using radioactive sestamibi and CT scans must be avoided secondary to concerns related to radiation exposure of the fetus. Ultrasound can be used safely during pregnancy; however, the sensitivity of ultrasound in localizing a parathyroid adenoma is only 57% to 89% [25]. Some lesions seen on ultrasound are quite typical of a parathyroid adenoma, while others are less convincing. One option for the latter is an ultrasound-guided aspiration of the lesion and measurement of parathyroid hormone from the needle washout [26, 27]. Surgery should only be done by those highly experienced in parathyroid surgery. If an adenoma has been localized preoperatively, minimally invasive parathyroidectomy limiting the operative field has been shown to be as effective as bilateral neck exploration in prospective trials and is associated with shorter hospital stays, smaller scars, and better short-term patient satisfaction [28]. The chance of successful surgery is aided by the use of intraoperative parathyroid hormone monitoring to confirm the removal of an adenoma [28–30].
During pregnancy, the optimal time for any surgery that is not an emergency is generally considered the second trimester. This same principle holds true for parathyroid surgery. In 1992 Carella and Gossain reviewed the available literature and identified 38 pregnant woman who had surgery for hyperparathyroidism. They reported normal fetal outcomes in all 7 woman who had surgery in the first trimester and 94% in the second trimester, but only 42% in the third trimester [31]. More recently, Tachamo et al reported a successful parathyroidectomy in the first trimester [32]. In 2005 Schnatz et al reviewed 16 patients with primary hyperparathyroidism who were treated surgically after 27 weeks of gestation. Forty-two percent of fetuses and 68.7% of mothers had postoperative complications as a direct result of the surgery. Reported complications included renal failure, premature rupture of membranes, preeclampsia, and postoperative hypocalcemia [12]. The decision to proceed with surgery during the third trimester must be individualized based on the degree of hypercalcemia, fetal maturity, and obstetrical history [8, 15, 22–24]
Our patient presented at 6 weeks gestation with symptomatic hypercalcemia and a corrected calcium of 14.8 mg/dL. Her initial PTH of 850 pg/mL was diagnostic of primary hyperparathyroidism, although vitamin D deficiency with secondary hyperparathyroidism may have contributed to this degree of elevation. Due to refractory hypercalcemia, she had resection of a 37 gram parathyroid adenoma at 7 weeks and 3 days of gestation. Following surgery our patient’s calcium, PTH, 1,25-dihydroxyvitamin D levels, and markers of bone resorption and bone formation returned to normal (Table 1). Despite the successful surgery, our patient developed preeclampsia. While this was her first pregnancy and she was obese with a BMI of 32, both of which increase the risk of preeclampsia, we cannot exclude the possibility that hyperparathyroidism in the first trimester contributed to this complication.
When a young person is diagnosed with primary hyperparathyroidism it should raise suspicion of a familial syndrome [33]. In our patient, there was no family history of hypercalcemia, and the absence of multigland parathyroid disease and a normal calcitonin level did not support a diagnosis of multiple endocrine neoplasia types 1 or 2. Genetic testing for the hyperpararthyroidism-jaw tumor syndrome did not identify a mutation of CDC73 gene.
Surgical management of primary hyperparathyroidism should be considered for pregnant women if the calcium level is significantly elevated or they are experiencing complications from the disease. Ideally, surgery is delayed until the second trimester but should be considered earlier if there is a significant degree of hypercalcemia that remains unresponsive to medical therapy.
Additional Information:
Disclosure Summary: The authors have nothing to disclose.
References
- 1. Kort KC, Schiller HJ, Numann PJ. Hyperparathyroidism and pregnancy. Am J Surg. 1999;177(1):66–68. [DOI] [PubMed] [Google Scholar]
- 2. Kelly TR. Primary hyperparathyroidism during pregnancy. Surg. 1991;110(6):1028–1033; discussion 1033. [PubMed] [Google Scholar]
- 3. Bilezikian JP. Primary Hyperparathyroidism. J Clin Endocrinol Metab. 2018;103(11):3993–4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bilezikian JP, Brandi ML, Eastell R, et al. . Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3561–3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Marcocci C, Bollerslev J, Khan AA, Shoback DM. Medical management of primary hyperparathyroidism: proceedings of the fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism. J Clin Endocrinol Metab. 2014;99(10):3607–3618. [DOI] [PubMed] [Google Scholar]
- 6. Silverberg SJ, Clarke BL, Peacock M, et al. . Current issues in the presentation of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3580–3594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schnatz PF, Curry SL. Primary hyperparathyroidism in pregnancy: evidence-based management. Obstet Gynecol Surv. 2002;57(6):365–376. [DOI] [PubMed] [Google Scholar]
- 8. Rigg J, Gilbertson E, Barrett HL, Britten FL, Lust K. Primary hyperparathyroidism in pregnancy: maternofetal outcomes at a quaternary referral obstetric hospital, 2000 through 2015. J Clin Endocrinol Metab. 2019;104(3):721–729. [DOI] [PubMed] [Google Scholar]
- 9. Shangold MM, Dor N, Welt SI, Fleischman AR, Crenshaw MC Jr. Hyperparathyroidism and pregnancy: a review. Obstet Gynecol Surv. 1982;37(4):217–228. [DOI] [PubMed] [Google Scholar]
- 10. Iqbal N, Aldasouqi S, Peacock M, Mohammed IA, Edmondson JW. Life-threatening hypercalcemia associated with primary hyperparathyroidism during pregnancy: case report and review of literature. Endocr Pract. 1999;5(6):337–342. [DOI] [PubMed] [Google Scholar]
- 11. Norman J, Politz D, Politz L. Hyperparathyroidism during pregnancy and the effect of rising calcium on pregnancy loss: a call for earlier intervention. Clin Endocrinol (Oxf). 2009;71(1):104–109. [DOI] [PubMed] [Google Scholar]
- 12. Schnatz PF, Thaxton S. Parathyroidectomy in the third trimester of pregnancy. Obstet Gynecol Surv. 2005;60(10):672–682. [DOI] [PubMed] [Google Scholar]
- 13. Levine SN Albritton M, Pothiwala P. Calcium and parathyroid disorder. In: Cohen WR, August P, eds. Obstetric Medicine, Management of Medical Disorders in Pregnancy. 6th ed. Shelton, CT: Peoples Medical Publishing House; 2013:479–495. [Google Scholar]
- 14. Kohlmeier L, Marcus R. Calcium disorders of pregnancy. Endocrinol Metab Clin North Am. 1995;24(1):15–39. [PubMed] [Google Scholar]
- 15. Hirsch D, Kopel V, Nadler V, Levy S, Toledano Y, Tsvetov G. Pregnancy outcomes in women with primary hyperparathyroidism. J Clin Endocrinol Metab. 2015;100(5):2115–2122. [DOI] [PubMed] [Google Scholar]
- 16. Sokal A, Elefant E, Leturcq T, Beghin D, Mariette X, Seror R. Pregnancy and newborn outcomes after exposure to bisphosphonates: a case-control study. Osteoporos Int. 2019;30(1):221–229. [DOI] [PubMed] [Google Scholar]
- 17. Levy S, Fayez I, Taguchi N, et al. . Pregnancy outcome following in utero exposure to bisphosphonates. Bone. 2009;44(3):428–430. [DOI] [PubMed] [Google Scholar]
- 18. Vera L, Oddo S, Di Iorgi N, Bentivoglio G, Giusti M. Primary hyperparathyroidism in pregnancy treated with cinacalcet: a case report and review of the literature. J Med Case Rep. 2016;10(1):361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. .Nadarasa K, Bailey M, Chahal H, et al. . The use of cinacalcet in pregnancy to treat a complex case of parathyroid carcinoma. Endocrinol Diabetes Metab Case Rep. 2014;2014(1):140056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Horjus C, Groot I, Telting D, et al. . Cinacalcet for hyperparathyroidism in pregnancy and puerperium. J Pediatr Endocrinol Metab. 2009;22(8):741–749. [DOI] [PubMed] [Google Scholar]
- 21. Petit DW, Clark RL. Hyperparathyroidism and pregnancy. Am J Surg. 1947;74(6):860–866. [DOI] [PubMed] [Google Scholar]
- 22. Dochez V, Ducarme G. Primary hyperparathyroidism during pregnancy. Arch Gynecol Obstet. 2015;291(2):259–263. [DOI] [PubMed] [Google Scholar]
- 23. Diaz-Soto G, Linglart A, Sénat MV, Kamenicky P, Chanson P. Primary hyperparathyroidism in pregnancy. Endocrine. 2013;44(3):591–597. [DOI] [PubMed] [Google Scholar]
- 24. DiMarco AN, Meeran K, Christakis I, et al. . Seventeen cases of primary hyperparathyroidism in pregnancy: a call for management guidelines. J Endocr Soc. 2019;3(5):1009–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Egan RJ, Scott-Coombes DM. The surgical management of sporadic primary hyperparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018;32(6):847–859. [DOI] [PubMed] [Google Scholar]
- 26. Abraham D, Sharma PK, Bentz J, Gault PM, Neumayer L, McClain DA. Utility of ultrasound-guided fine-needle aspiration of parathyroid adenomas for localization before minimally invasive parathyroidectomy. Endocr Pract. 2007;13(4):333–337. [DOI] [PubMed] [Google Scholar]
- 27. Pothiwala P, Levine SN. Parathyroid surgery in pregnancy: review of the literature and localization by aspiration for parathyroid hormone levels. J Perinatol. 2009;29(12):779–784. [DOI] [PubMed] [Google Scholar]
- 28. Udelsman R, Åkerström G, Biagini C, et al. . The surgical management of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3595–3606. [DOI] [PubMed] [Google Scholar]
- 29. Shawky M, Abdel Aziz T, Morley S, et al. . Impact of intraoperative parathyroid hormone monitoring on the management of patients with primary hyperparathyroidism. Clin Endocrinol (Oxf). 2019;90(2):277–284. [DOI] [PubMed] [Google Scholar]
- 30. Bhangu JS, Riss P. The role of intraoperative parathyroid hormone (IOPTH) determination for identification and surgical strategy of sporadic multiglandular disease in primary hyperparathyroidism (pHPT). Best Pract Res Clin Endocrinol Metab. 2019;33(5):101310. [DOI] [PubMed] [Google Scholar]
- 31. Carella MJ, Gossain VV. Hyperparathyroidism and pregnancy: case report and review. J Gen Intern Med. 1992;7(4):448–453. [DOI] [PubMed] [Google Scholar]
- 32. Tachamo N, Timilsina B, Dhital R, Lynn T, Magaji V, Gabriely I. Primary hyperparathyroidism in pregnancy: successful parathyroidectomy during first trimester. Case Rep Endocrinol. 2018;2018:5493917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Eastell R, Brandi ML, Costa AG, D’Amour P, Shoback DM, Thakker RV. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3570–3579. [DOI] [PubMed] [Google Scholar]