Abstract
Purpose
Osteochondral lesion of talus (OLT) is one of the common causes of ankle pain. This disorder is common in young athletes after ankle injury. There are various therapeutic options. One of the options is mosaic plasticizer. The purpose of this study was to investigate the effect of mosaicplasty on improvement of symptoms of patients with osteochondral lesions of talus.
Methods
Nineteen patients with osteochondral lesions of talus participated in this study, who were treated with mosaicplasty. Before and after treatment, pain (visual analogue scale), function (American Orthopaedic Foot and Ankle Society), range of motion and radiographic signs were evaluated.
Results
The results of this study showed that mosaicplasty could significantly reduce pain, increase function and improve radiographic symptoms. The range of motion increased after treatment, which was not significant.
Conclusion
We can confirm the effect of mosaicplasty on the improvement of patients with osteochondral lesions of the ankle, suggesting it as a treatment option.
Keywords: Autografts, Talus, Osteochondral lesions
Introduction
Osteochondral lesion of talus (OLT) is one of the common causes of ankle pain.1, 2, 3 Some of patients remember a kind of traumatic event which is one of the most common causes of this disorder. Other causes include genetic factors, osteonecrosis and endocrine disease.4,5 This disorder is common in young athletes after ankle injury.6 5% of people who have ankle sprain in sports will later experience osteochondral lesions of the talus.7 Another study reported 6.5% prevalence of this complication in ankle sprains.8 Diagnosis is done based on history, clinical examinations, radiology, and magnetic resonance imaging (MRI).9 Symptoms of this disorder include pain, tenderness and swelling and in chronic phase, it can cause movement constraints.10
Selective surgical procedures for these patients are usually based on their age, location and size of the lesion.11,12 Common treatments for this disorder include non-surgical and surgical treatments. Non-surgical treatments include immobilization with cast and rest. Surgical techniques may also be referred to chondroabrasion, antegrade drilling, retrograde drilling and cancellous bone graft, autologus chondrocyte implantation, osteochonderal autograft transfer (mosaicplasty).10
For the first time, Hangody et al13 reported in 1997 the successful results of mosaicplasty. In another study in 2001, they reported good-to-excellent results for patients with osteochondral lesions of the ankle treated with mosaicplasty.14 Further studies have been done on the effect of this technique. In another study, the usefulness and effectiveness of this surgical procedure have been reported.10,15 In this study we aimed to assess the efficacy of mosaicplasty on patients with osteochondral lesions of the talar dome.
Methods
Nineteen patients with osteochondral lesion of the talus including 11 males and 8 females were treated with osteochondral autograft transfer between 2009 and 2015. Some of them experienced trauma and others had a history of recurrent ankle sprains. Clinical examination of these patients revealed tenderness and limitation of mobility of the ankle joint. All patients complained of pain. Mosaicplasty is usually used for lesions more than 15 mm in diameter and those with underlying cyst with more than 7 mm depth. Lesions were classified by preoperative MRI according to Dipaola classification (Table 1). In general inclusion criteria in this study were osteochondral lesions of the ankle grade 2 and above (Berndt/Harty) and size more than 15 mm or depth of more than 7 mm and having a painful ankle. Patients were excluded from the study if they had ankle osteoarthritis because osteoarthritis is a contraindication for mosaicplasty. Other exclusion criteria included diabetes mellitus and neurological diseases, age more than 60 years, previous ankle surgery and knee osteoarthritis.
Table 1.
Classification of lesions by preoperative MRI according to Dipaola classification.
| Dipaola classification | Description | Number of patients |
|---|---|---|
| I | Thickening of cartilage and low signal change | 0 |
| II | Articular cartilage breached with low signal rim behind | 4 |
| III | Articular cartilage breached with high signal rim behind | 14 |
| IV | Loose body | 1 |
Surgical technique
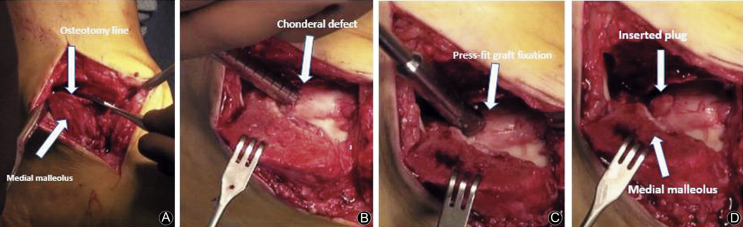
Surgery was performed in the supine position. All patients received spinal anesthesia. The affected lower extremity was prepared to allow access to the ipsilateral knee in addition to the ankle. Ankle orthoscopy was done prior to surgery to further evaluate the chondral lesion. Through a lateral knee arthrotomy, grafts were taken with a donor cutting tube from the non-weight bearing surface of the lateral femoral condyle by use of Arthrex osteochondral autograft transfer system set (6 mm). Osteochondral lesion of the talus was then approached through an anterolateral incision for lateral lesions or medial malleolar osteotomy (Fig. 1A) for medial lesions. The lesion was then excised and the crater was debrided. A recipient socket, sized to the proper depth was created in the chondral defect to accept the donor graft (Fig. 1B). The bone cylinder was inserted with a collared pin delivery system for press-fit fixation (Fig. 1C and D). In the usual way, the osteotomies were fixed with cannulated screws and incision was closed.
Fig. 1.
Medial malleolar osteotomy line (A). Recipient socket sized to the proper depth was created (B). The bone cylinder was inserted with a collared pin delivery system for press-fit fixation (C). Press-fit fixation of the osteochonderal graft (D).
A compressive dressing and posterior splinting was done after surgery. Posterior splint was changed to a brace (ankle foot orthosis) 2 weeks after surgery and passive range of motion exercises of the ankle and knee started. Patients were kept non-weight bearing for 12 weeks. After radiographs showed evidence of bone healing, full weight bearing started. Patients were allowed to return to sports after 6 months.
Assessment was done by another surgeon and a researcher before operation and 12 month after. Pain was measured by the visual analogue scale (VAS) with 0 indicating no pain and 10 indicating the worst possible pain. The patients' function was assessed by an American Orthopaedic Foot and Ankle Society (AOFAS) scoring system. Range of motion (plantar flexion, dorsiflexion, inversion, and eversion) was measured. In this study paired t-test was used. Statistical analysis was managed with SPSS software (version 16.0). Differences were considered to be statistically significant if p < 0.05.
Results
The average age of the patients was (43 ± 12) years. Almost at the end of follow-up most patients were satisfied with their treatment. The results of this study showed that the pain level of patients assessed by the VAS decreased from 7.4 before treatment to 3.2 after mosaicplasty (p < 0.001).
After the operation, the AOFAS scores increased from 42.1 to 78.6, and this increase was significant (p < 0.001). All patients were satisfied with the operation, and 14 (73%) patients reported good to excellent results. Before surgery, most patients complained of swelling, tenderness and joint locking symptoms. After treatment, these symptoms showed a significant improvement in 72.72% of patients (p < 0.001).
Following the disease, the range of motion is usually reduced in the affected side compared to the healthy side, while the change in ankle range of motion (dorsiflexion, plantar flexion, inversion and eversion) after surgery was not significant (p = 0.33). Physical therapy exercises also seemed to be beneficial for further improvement. At the end of the follow-up, none of radiographic images showed arthritic change in ankle joint.
Three patients had complications. One of the patients had superficial wound infection, and two patients had hardware irritation (due to screws for fixation of medial side). The superficial wound infection treated with oral antibiotics and dressing changes. Two patients with hardware irritation required hardware removal.
Discussion
There are several surgical procedures for the treatment of osteochondral lesions of the talus, based on cartilage repair, cartilage regeneration, and cartilage replacement strategies.16,17 Mosaicplasty is one of the therapeutic options for this disorder.18 The present study demonstrated significant improvement in pain and function of patients at 1 year after treatment with mosaicplasty. The results of this study were similar to those of some other studies, which reported improved symptoms in subjects with osteochondritis lesions of the ankle after mosaicplasty. Hangody et al19 indicated that this technique is one of the methods that has good results in long term. Improvement of symptoms after mosaicplasty has also been reported in the study by Scranton et al.20 Other studies have shown a modest to excellent improvement in the symptoms of patients with osteochondral lesions of the talus treated with mosaicplasty.21,22
Sexton et al in a study showed that mosaicplasty has a greater morbidity than some other methods, such as curettage, but it also has important advantages like removal of the necrotic subchondral tissue in the defect site.23 The disadvantages and other problems of this technique are the severe donor site morbidity on the ipsilateral knee joint that Reddy and colleagues have mentioned in a study.24 Also McGahan et al25 and Sammarco et al26 stated that donor site morbidity remains the most significant disadvantage of this technique. While Gautier et al27 reported inconsistent results in their study and did not report donor site morbidity.
Overall, increasing lesion size often requires more advanced regenerative or replacement techniques rather than reparative ones.16 More comparative studies and randomized controlled trials are needed to illustrate which treatment options are more effective for certain types of lesions.
In general, we can confirm the effect of mosaicplasty on the improvement of patients with osteochondral lesions of the ankle according to the data obtained from this study, and suggest it as a treatment option.
Funding
Nil.
Ethical Statement
This study has been approved by the local ethics committee.
Declaration of Competing Interest
The author has declared no conflicts of interest.
Acknowledgments
Research performed at Sport Medicine and Knee Research Center, Milad Hospital, Tehran, Iran. But, this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.O'loughlin P.F., Heyworth B.E., Kennedy J.G. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38:392–404. doi: 10.1177/0363546509336336. [DOI] [PubMed] [Google Scholar]
- 2.Natsuhara K.M., Sarcon A., Kreulen C. Treatment of osteochondral lesions of talus with extracellular matrix cartilage allografts. Tech Foot Ankle Surg. 2019;18:61–67. [Google Scholar]
- 3.Kim T.Y., Song S.H., Baek J.H. Analysis of the changes in the clinical outcomes according to time after arthroscopic microfracture of osteochondral lesions of the talus. Foot Ankle Int. 2019;40:74–79. doi: 10.1177/1071100718794944. [DOI] [PubMed] [Google Scholar]
- 4.Schachter A.K., Chen A.L., Reddy P.D. Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2005;13:152–158. doi: 10.5435/00124635-200505000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Sadlik B., Kolodziej L., Puszkarz M. Surgical repair of osteochondral lesions of the talus using biologic inlay osteochondral reconstruction: clinical outcomes after treatment using a medial malleolar osteotomy approach compared to an arthroscopically-assisted approach. Foot Ankle Surg. 2019;25:449–456. doi: 10.1016/j.fas.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Verhagen R.A., Struijs P.A., Bossuyt P.M. Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003;8:233–242. doi: 10.1016/s1083-7515(02)00064-5. [DOI] [PubMed] [Google Scholar]
- 7.Seil R., Kohn D. Approach to open treatment of osteochondral lesions of the talus. Orthopade. 2001;30:1–2. doi: 10.1007/s001320050572. [DOI] [PubMed] [Google Scholar]
- 8.Bosien W.R., Staples O.S., Russell S.W. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37:1237–1243. [PubMed] [Google Scholar]
- 9.Giannini S., Buda R., Faldini C. Surgical treatment of osteochondral lesions of the talus in young active patients. J Bone Joint Surg Am. 2005;87(suppl. 2):28–41. doi: 10.2106/JBJS.E.00516. [DOI] [PubMed] [Google Scholar]
- 10.Emre T.Y., Ege T., Çift H.T. Open mosaicplasty in osteochondral lesions of the talus: a prospective study. J Foot Ankle Surg. 2012;51:556–560. doi: 10.1053/j.jfas.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Berndt A.L., Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 2004;86:1336. doi: 10.2106/00004623-200406000-00032. [DOI] [PubMed] [Google Scholar]
- 12.Ove P.N., Bosse M.J., Reinert C.M. Excision of posterolateral talar dome lesions through a medial transmalleolar approach. Foot Ankle. 1989;9:171–175. doi: 10.1177/107110078900900404. [DOI] [PubMed] [Google Scholar]
- 13.Hangody L., Kish G., Karpati Z. Treatment of osteochondritis dissecans of the talus: use of the mosaicplasty technique—a preliminary report. Foot Ankle Int. 1997;18:628–634. doi: 10.1177/107110079701801005. [DOI] [PubMed] [Google Scholar]
- 14.Hangody L., Kish G., Módis L. Mosaicplasty for the treatment of osteochondritis dissecans of the talus: two to seven year results in 36 patients. Foot Ankle Int. 2001;22:552–558. doi: 10.1177/107110070102200704. [DOI] [PubMed] [Google Scholar]
- 15.Kodama N., Honjo M., Maki J. Osteochondritis dissecans of the talus treated with the mosaicplasty technique: a case report. J Foot Ankle Surg. 2004;43:195–198. doi: 10.1053/j.jfas.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Steele J.R., Dekker T.J., Federer A.E. Osteochondral lesions of the talus: current concepts in diagnosis and treatment. Foot Ankle Orthop. 2018;3:1–9. doi: 10.1177/24730114231192961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeSandis B.A., Haleem A.M., Sofka C.M. Arthroscopic treatment of osteochondral lesions of the talus using juvenile articular cartilage allograft and autologous bone marrow aspirate concentration. J Foot Ankle Surg. 2018;57:273–280. doi: 10.1053/j.jfas.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Buda R., Pilla F., Ruffilli A. Arthroscopic bone marrow–derived cell transplantation in osteochondral lesions of the talus: surgical procedure, technical tips, and results-award winner. J Am Acad Orthop Surg. 2018;26:e467. [Google Scholar]
- 19.Hangody L., Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003;85(suppl. 2):25–32. doi: 10.2106/00004623-200300002-00004. [DOI] [PubMed] [Google Scholar]
- 20.Scranton P.E., Jr., Frey C.C., Feder K.S. Outcome of osteochondral autograft transplantation for type-V cystic osteochondral lesions of the talus. J Bone Joint Surg Br. 2006;88:614–619. doi: 10.1302/0301-620X.88B5.17306. [DOI] [PubMed] [Google Scholar]
- 21.Assenmacher J.A., Kelikian A.S., Gottlob C. Arthroscopically assisted autologous osteochondral transplantation for osteochondral lesions of the talar dome: an MRI and clinical follow-up study. Foot Ankle Int. 2001;22:544–551. doi: 10.1177/107110070102200703. [DOI] [PubMed] [Google Scholar]
- 22.Valderrabano V., Leumann A., Rasch H. Knee-to-ankle mosaicplasty for the treatment of osteochondral lesions of the ankle joint. Am J Sports Med. 2009;37(1 suppl):105S–111S. doi: 10.1177/0363546509351481. [DOI] [PubMed] [Google Scholar]
- 23.Sexton A.T., Labib S.A. Osteochondral lesions of the talus: current opinions on diagnosis and management. Cur Opin Orthop. 2007;18:166–171. [Google Scholar]
- 24.Reddy S., Pedowitz D.I., Parekh S.G. The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med. 2007;35:80–85. doi: 10.1177/0363546506290986. [DOI] [PubMed] [Google Scholar]
- 25.Sammarco G.J., Makwana N.K. Treatment of talar osteochondral lesions using local osteochondral graft. Foot Ankle Int. 2002;23:693–698. doi: 10.1177/107110070202300803. [DOI] [PubMed] [Google Scholar]
- 26.McGahan P.J., Pinney S.J. Current concept review: osteochondral lesions of the talus. Foot Ankle Int. 2010;31:90–101. doi: 10.3113/FAI.2010.0090. [DOI] [PubMed] [Google Scholar]
- 27.Gautier E., Kolker D., Jakob R. Treatment of cartilage defects of the talus by autologous osteochondral grafts. J Bone Joint Surg Br. 2002;84:237–244. doi: 10.1302/0301-620x.84b2.11735. [DOI] [PubMed] [Google Scholar]