Abstract
Aim
The primary objective was to assess set-up errors (SE) and secondary objective was to determine optimal safety margin (SM)
Background
To evaluate the SE and its impact on the SM utilizing electronic portal imaging (EPI) for pelvic conformal radiotherapy.
Material and methods
20 cervical cancer patients were enrolled in this prospective study. Supine position with ankle and knee rest was used during CT simulation. The contouring was done using consensus guideline for intact uterus. 50 Gy in 25 fractions were delivered at the isocenter with ≥95% PTV coverage. Two orthogonal (Anterior and Lateral) digitally reconstructed radiograph (DRR) was constructed as a reference image. The pair of orthogonal [Anterior-Posterior and Right Lateral] single exposure EPIs during radiation was taken. The reference DRR and EPIs were compared for shifts, and SE was calculated in the X-axis, Y-axis, and Z-axis directions.
Results
320 images (40 DRRs and 280 EPIs) were assessed. The systematic error in the Z-axis (AP EPI), X-axis (AP EPI), and Y-axis (Lat EPI) ranged from -12.0 to 11.8 mm, -10.3 to 7.5 mm, and -8.50 to 9.70 mm, while the random error ranged from 1.60 to 6.15 mm, 0.59 to 4.93 mm, and 1.02 to –4.35 mm. The SM computed were 7.07, 6.36, and 7.79 mm in the Y-axis, X-axis, and Z-axis by Van Herk’s equation, and 6.0, 5.51, and 6.74 mm by Stroom’s equation.
Conclusion
The computed SE helps defining SM, and it may differ between institutions. In our study, the calculated SM was approximately 8 mm in the Z-axis, 7 mm in X and Y axis for pelvic conformal radiotherapy.
Keywords: Set-up errors, Set-up margin, Pelvic conformal radiotherapy
1. Background
The principal of radiotherapy in the 2D-3D era is to eradicate tumor cells contained in the gross tumor volume (GTV) with a margin for subclinical disease in the clinical target volume (CTV) while sparing surrounding organs at risks (OARs). It is achieved by conforming the treatment portals to the target volume and using appropriate margins to rationalize for uncertainties in organ shape and motion, beam geometry and patient set-up. The notion of the planning target volume (PTV) margin was introduced to establish the margins between the CTV and field borders. The radiation portal size is reliant on the width of SM around the CTV that ascertain that the target volume is actually or likely irradiated.1,2 Reducing the CTV to PTV margins by hampering the internal tumor motion and maximizing the patient set-up reproducibility will lead to better conformity and decrease dose to OARs. However, a too small CTV to PTV SM will result in geometrical misses at some fractions or even all fractions of radiation treatment. It is, therefore, essential to evaluate, and possibly reduce the setup errors, tumor and organ motion during radiation.3
The patient’s position reproducibility and its accuracy are essential for precise delivery of radiation therapy. Despite that, uncertainty occurs because of daily patient SE which leads to the dissimilarity between the planned and delivered dose. A significant error in the patient’s positioning during conformal pelvic radiation has been established in many studies.4, 5, 6, 7, 8
The SE can be calibrated using an EPI and megavoltage (MV) or kilovoltage (KV) cone-beam computed tomography (CBCT). The shift that occurs in a similar direction and is of similar extent for every fraction throughout treatment is defined as a systematic error. This could be a result of a target contour delineation error due to a shift in target location, change in shape between delineation and treatment due to tumor regression, and change due to bladder and bowel filling. The random error is the shift that can differ in direction and its extent for each treatment fraction, and this could result from changes in target position and shape between fractions or during fractions because of breathing. The random error is affected by patient comfort, immobilization technique used.3
The increased capacity to compute the SE, along with the requirement to shrink SEs to decrease CTV to PTV SM, has led to a growing number of studies reporting the site-specific SM for conformal radiotherapy. We conducted this study to assess SE in a cervical cancer patient undergoing 3-dimensional conformal radiotherapy (3D-CRT) and to observe its impact on SM.
1.1. Aim
The primary endpoint is to assess the SE, and the secondary objective was to determine an optimal safety CTV to PTV margin.
2. Material and methods
This single institutional study was conducted from February 2018 till December 2018. The ethical committee of the hospital approved the research study (856/Ethics/KGMU/R.cell-18). Information regarding the study protocol was given to the enrolled patient, and they signed the informed consent. 20 patients were enrolled with pathologically confirmed cervical squamous cell carcinoma. The inclusion basis was the age of ≥25 and <75 years, Kernofsky performance score of ≥80, International Federation of Gynaecology and Obstetrics Federation (FIGO) 2009 stage IIB-IIIB, adequate blood differential count and complete blood count with hemoglobin ≥12 mg/dl, creatinine clearance ≥50 ml/minute and normal liver function. An investigation like cystoscopy and contrast-enhanced computed tomography (CECT) of the whole abdomen and pelvis was done to rule out urinary bladder and para-aortic lymph node involvement, and in clinically suspicious case magnetic resonance imaging (MRI) of the abdomen and pelvis were done.
2.1. Positioning and simulation
Patients were positioned in a supine posture using the knee support and ankle rest on carbon baseplate with both arms on the chest. The knee support was used to decrease pelvic rotations, and the legs were slightly externally rotated to ensure decreased muscle tension in the legs and the buttocks.3,9,10 Patients were briefed to void their bladder and empty rectum before CT simulation and then drink 500 ml of water 30 min before simulation and daily before treatment to achieve full bladder.11 The markers were placed at the introitus, the lower extent of disease, and at the anal verge. Intravenous contrast was injected before scanning. Planning images (both plain and contrast) of 3 mm were generated by scanning the patient on Phillips 16 slice CT simulator. Three orthogonal lasers established the patient coordinate system. The crosshair points in the X, Y, and Z-axis were marked on the patient with lead beads serving as external fiducial markers that were then replaced by markings on the skin surface. The information was then transmitted to the treatment planning system (TPS- Monaco Sim Integrated Planning System Version. 10).
2.2. Contouring and treatment planning
The CT image dataset thus obtained was then registered and saved in TPS. These set of images formed the basis for the contouring of the CTV, PTV, and OARs based on consensus guideline atlas for an intact uterus.12 CTV to PTV margin was defined as 1 cm because of geometric inaccuracies, such as delineation uncertainty and internal organ motion. Shielding of normal structures external to PTV was done using Multi-leaf collimators (MLC). A 3DCRT plan consisting of four fields; Anterior-posterior (AP), Posterior-anterior (PA), and two laterals portals was generated. 50 Gy in 25 fractions was prescribed to the isocenter with the objective of ≥ 95% PTV coverage, whereas limiting the maximum dose to 107%. An orthogonal pair (Antero-posterior and right lateral) of DRR was created. The DRR images worked as a reference image and were transferred from TPS to the treatment console (iView-GT system), together with the approved treatment plan.
2.3. Portal imaging and displacement
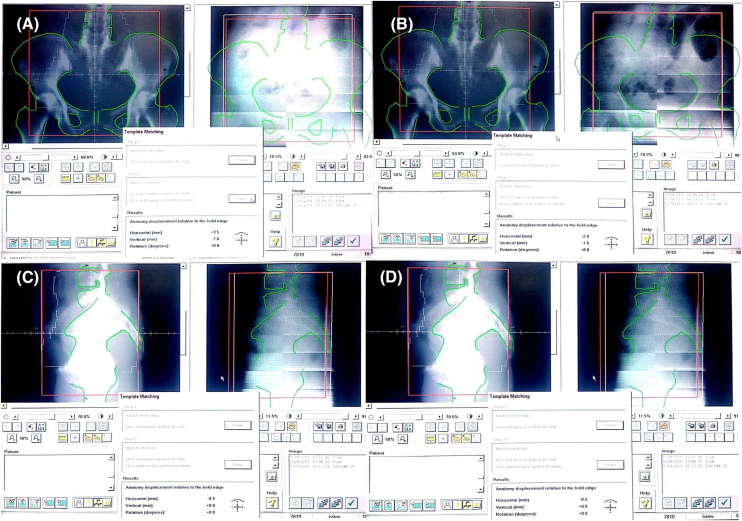
The orthogonal pair (Antero-posterior (AP) and right-lateral (Lat)) of single exposure EPIs were obtained using Elekta Perkin Elmer AL type panel EPI device (Elekta Medical System) after positioning the patient as shown in Fig. 1. For every patient, Day1, Day2, Day3 of week1 and the first day of Week2, Week3, Week4, Week5 EPI were obtained using one monitoring unit (MU), and a total of 280 EPIs were acquired. The reference DRRs images were compared with EPIs.
Fig. 1.
Assessment of set-up error using EPI before (A and C) and after correction (B and D) in Antero-posterior view EPI (A and B) and lateral view EPI (C and D).
For patients SE assessment, bony landmarks were determined as per the Royal College of Radiologists (RCR).13 The bony landmarks established were the pelvic rim for the X-axis, the symphysis pubis for the Z-axis in AP EPI, and the S1 vertebra anterior border for the Y-axis displacement in lateral EPI. The right, anterior, and superior shift were defined as positive shifts, whereas the left, posterior, and inferior shift were interpreted as negative shifts for assessment. The bony landmark displacements were calculated with reference to the isocenter. During the first fraction, the patient was positioned on the couch, and EPI is obtained using one MU of treatment dose, after which the irradiation stops automatically. Similar bony landmarks as per reference image must be defined in a portal image. The patient position is determined by calculation of the difference between landmarks in the portal and a reference image. If the 2D set-up deviation is >4 mm, the couch is moved. For offline determination of the final set-up position, the image is made using the remaining dose of 5 MU. The accuracy of on-line bony landmark match for all one MU and final 5 MU images were retrospectively analyzed by a contour match. All the calculations were performed by one medical physicist, to prevent inter-observer variation.
2.4. Calculation of systematic, random errors, and SM
The individual and population-based systematic and random errors were computed along the X-axis, Y-axis, and Z-axis directions using Cartesian coordinates, and were calculated as per the report by the RCR.13,14 The RCR report defined the individual patient mean SE (Mindividual), and overall population group mean SE (Mpop). The systematic error of population (Σ2setup) was described as the standard deviation (SD) of MIndividual around the Mpop. The individual random (σindividual) SE was expressed as the SD of the SE around the Mindividual, and the random error of population (σ2setup) was defined as the mean of all σindividual.13 Following the result of systematic and random error, the population-based SM (CTV to PTV) were computed using the Van Herk's, and Stroom's equation.4,15
2.5. Statistical analysis
The SE data analytics and safety (CTV to PTV) margin were calculated using SPSS software (Version 22, Chicago, USA).
3. Results
The median age of the study group was 55 years (range 37–64 years). 16 patients (80%) had stage IIB, and 2 patients had stage IIIA and IIIB. 320 images (40 DRRs and 280 EPIs) were acquired and evaluated through point locations in the X, Y, and Z-axis directions.
The displacement for 20 patients in the Z-axis (AP EPI), X-axis (AP EPI), Y-axis (Lat EPI) directions was inspected. The mean displacement was 4.51 mm (range −4.64 to 3.57 mm); 3.12 mm (range −2.25 to 3.40 mm); and -0.07 mm (range −3.53 to 6.00 mm) in the Z-axis (AP EPI), X-axis (AP EPI), and Y-axis (Lat EPI) as shown in Table 1. The majority (55.1%) of the displacements in the Z-axis (AP EPI) were ≤3 mm while only 3.4% of the images had deviation >10 mm. A similar result was observed in the X-axis (57.6%) and the Y-axis (67.0%) directions, where the majority had ≤3 mm displacement as shown in Table 2.
Table 1.
The range of displacement, and the range of individual systematic (MIndividual) and random error (σIndividual).
| Deviation | Z (AP EPI) | X (AP EPI) | Y (Lat EPI) |
|---|---|---|---|
|
Setup error- range (mm) |
−4.64 to 3.57 |
2.25 to 3.30 |
3.53 to 6.00 |
| Systematic error-range (mm) | −12.00 to 11.80 | −10.3 to 7.5 | −8.50 to 9.70 |
| Random error (1SD in mm) | 1.60 to 6.15 | 0.59 to 4.93 | 1.02 to 4.35 |
Z = Z-axis (Supero-inferior displacement; X = X-axis (Left-right displacement; Y = Y-axis (Antero-posterior displacement; AP = antero-posterior view EPI; Lat = Lateral view EPI.
Table 2.
Displacements in X, Y, and Z axis direction in Antero-posterior and lateral view EPI (N = 140).
| Displacements | Z (AP EPI) N (%) |
X (AP EPI) N (%) |
Y (Lat EPI) N (%) |
|---|---|---|---|
|
≤3 mm |
87 (55.1%) |
90 (57.6%) |
101 (67.0%) |
| >3 mm to ≤5 mm | 27 (22.9%) | 35 (29.7%) | 26 (22.0%) |
| >5 mm to ≤7 mm | 13 (11.0%) | 10 (8.5%) | 5 (4.2%) |
| >7 mm to ≤10 mm | 9 (7.6%) | 4 (3.4%) | 8 (6.8%) |
| >10 mm | 4 (3.4%) | 1 (0.8%) | 0 (0.0%) |
Note: Data are number (%); Abbreviation: Z = Z-axis (Supero-inferior displacement); X = X-axis (Left-right displacement); Y = Y-axis (Antero-posterior displacement); AP = antero-posterior view EPI; Lat = Lateral view EPI.
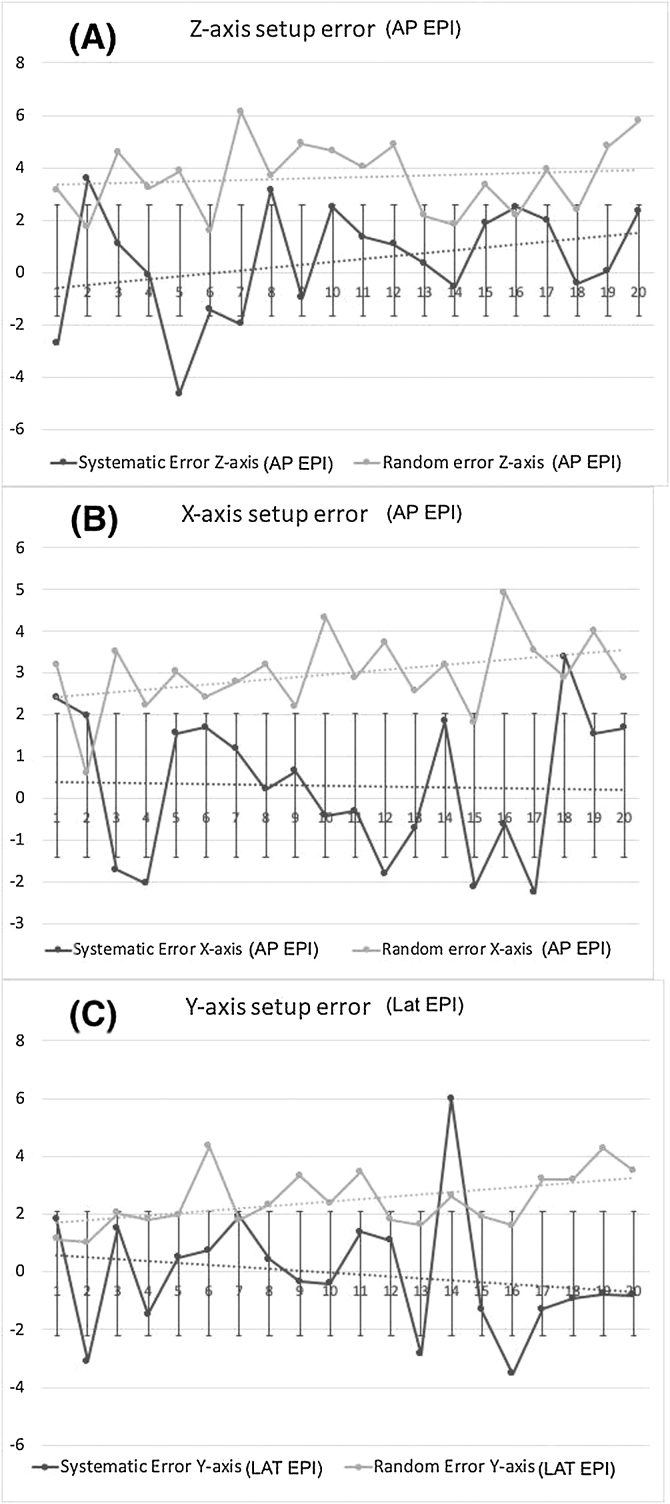
The computed systematic error was small in comparison to the random error. The calculated random error for the Z-axis (AP EPI) direction was larger in comparison to the X-axis (AP EPI), and the Y-axis (Lat EPI) as shown in Fig. 2.
Fig. 2.
(A, B, C): Systematic and random error (1SD) of 20 patients along Z-axis (AP view EPI, X-axis (AP view EPI), and Y-axis (Lat view EPI) in patient positioning. (Graph: On x-axis is patient number from 1-20, and on y-axis is displacement in millimeters).
The calculated range of MIndividual and σIndividual for 20 patients are stated in Table 1. The Mpop was computed to be 0.31, −0.07, and 0.45 in X (AP EPI), Y (Lat EPI), and Z-axis (AP EPI) directions respectively. The computed Σ2pop was 2.10 mm, 1.71 mm, 2.14 mm for the Z-axis (AP EPI), X-axis (AP EPI), and Y-axis (Lat EPI) directions. The computed σ2pop was 3.63 mm, 2.99 mm, and 2.46 mm in the Z-axis (AP EPI), X-axis (AP EPI), and Y-axis (Lat EPI) directions, respectively, as shown in Table 3.
Table 3.
Population systematic and random error, and SM depending on set-up errors.
| Direction | Systematic error (∑2pop) mm | Random error (σ2pop) mm | SM mm (Van Herk’s equation) | SM mm (Stroom’s equation) |
|---|---|---|---|---|
|
Z (AP EPI) |
2.10 |
3.63 |
7.79 |
6.74 |
| X (AP EPI) | 1.71 | 2.99 | 6.36 | 5.51 |
| Y (Lat EPI) | 2.14 | 2.46 | 7.07 | 6.00 |
∑2pop = systematic error of population; σ2pop = random error of population; Z = Z-axis (Supero-inferior displacement); X = X-axis (Left-right displacement); Y = Y-axis (Antero-posterior displacement); AP = antero-posterior view EPI; Lat = Lateral view EPI; SM = Safety margin.
The CTV to PTV population-based SM were computed using the Van Herk’s and Stroom’s equation. The CTV-PTV margin in Z-axis (AP EPI), X-axis (AP EPI), and Y-axis (Lat EPI) direction was 7.8 mm, 6.4 mm, 7.1 mm using Van Herk’s equation and 6.7 mm, 5.5 mm, and 6.0 mm by Stroom’s equation as shown in Table 3.
4. Discussion
The objective of this research was to estimate the SE and, based on it, to observe its impact on adequate CTV to PTV SM that would lead to adequate dose coverage of a target volume. The difficulties while treating a cervical cancer patient with 3DCRT or Intensity-modulated radiotherapy (IMRT) is the variability of the tumor position, internal organ variability, and inaccuracy in reproducing the similar patient position as in the initial CT simulation pose.4,5,11,16 So, the SM is reliant on the precision to reproduce the same patient position as during the initial CT simulation and irradiation.
The significant improvement in set-up accuracy was reported by the application of an off-line verification protocol, on-line verification protocol, and the combination of both off-line and on-line to minimize treatment time.4,17, 18, 19, 20 This combination of an off-line and on-line verification protocol was used in our research. The major drawback in many set-up error studies for pelvic radiotherapy is a large inter-observer variation, as it decreases the statistical significance of any difference in set-up error.3 Hence, to prevent this inter-observer variability in our study, all recording and calculations of set-up errors was performed by one medical physicist
The study by Stroom et al. reported the random errors in the X and Z-axis directions as 2.30 mm, and 3.0 mm.4 The Van Herk et al. identified the random errors along the X, Y, and Z-axis directions as 2.0 mm, 1.7 mm, and 1.8 mm.15 The random error noticed in our study along the X, Y, and Z-axis directions were 2.99 mm, 2.46 mm, and 3.63 mm. The systematic and random errors observed in our study are in accord with the studies for gynecological patients as shown in Table 4, and it can be concluded that our reproducibility precision was reasonably satisfactory.3, 4, 5, 6,21,22
Table 4.
Comparative studies for systematic and random error in X, Y, and Z-axis direction in pelvic radiotherapy.
| Systematic error (mm) |
Random error (mm) |
|||||
|---|---|---|---|---|---|---|
| X | Y | Z | X | Y | Z | |
|
JJ Haslam et al.5 |
1.90 |
2.60 |
2.40 |
2.60 |
3.70 |
2.80 |
| Hurkmanas et al.3 | _ | _ | 4.80 | 3.0 | _ | 4.90 |
| Olofsen vanAcht et al.17 | _ | 3.70 | 3.60 | 1.90 | 2.60 | 2.30 |
| Strooms et al.4 | 2.0 | _ | 2.80 | 2.30 | _ | 3.0 |
| Weiss et al.18 | 1.50 | 3.0 | 2.10 | 2.60 | 3.40 | 3.50 |
| M. Kasabasic et al.6 | 1.90 | 2.50 | 2.60 | 2.70 | 4.10 | 3.30 |
| Our Study | 1.71 | 2.14 | 2.10 | 2.99 | 2.46 | 3.63 |
Abbreviations: X = X-axis (Left-right displacement); Y = Y-axis (Antero-posterior displacement); Z = Z-axis (Supero-inferior displacement); AP = antero-posterior view EPI; LAT = Lateral view EPI.
The SE may differ based on the technique of patient positioning and immobilization, patient comfort, treatment machine uncertainties, and strategy followed for quality assurance protocols.2,7,11,23 The study by Song et al., observed that the displacement >5 mm in 40% of patient positioning is affiliated with satisfactory precision in positioning of the patient during the treatment.24 Our study observed displacement of >5 mm in Z-axis (AP EPI), X-axis (AP EPI), and Y-axis (Lat EPI) was 22%, 12.7%, and 11.0% which was in accord with better patient positioning.
The systematic error and random errors were greater in the Z-axis direction than in the X and Y-axis which might be a result of the difference in bladder filling resulting in a drift of the skin mark (anterior) above or below with reference to the true isocenter. As during simulation and radiation treatment, patient repositioning was performed in reference to the alignment of lateral lasers with lateral tattoo mark and anteriorly placed skin marks. In the study by Rudat et al., for pelvic radiotherapy a similar result was observed with the most substantial error in the Z-axis direction.25
Stroom et al., computed the CTV-PTV SM (2∑ + 0.7σ) to assure that V99% of CTV received ≥95% of the prescribed dose.26 The study by Van Herk et al., computed the SM (2.5∑ + 0.7σ) to warrant a minimum dose to CTV of 95% for 90% of the patients.15 The SM was computed from the measurement of SE using Van Herk’s and Stroom’s equation published on position variability in pelvic radiotherapy.15,26 Our calculated CTV to PTV SM was nearly 1 cm in all directions and was similar to the margin reported by various authors for pelvic radiation as shown in Table 4.
Our study has certain limitations, firstly that the sample size was limited and the number of the EPIs was small. Second, we did not assess the intra-fraction errors as a result of breathing or organ motion. Third, the predominance of systematic errors in the Y-axis because of the use of skin marks for determination of isocenter height, as the skin mark movement is influenced by weight loss, bladder filling, respiration, or patient relaxation. That warrants further evaluation in a larger cohort with the inclusion of intra-fractional error, and using a marker on the thermoplastic mask. Regardless of the above mentioned limitation, ; the observed systematic error in our study was lesser than in the published six studies for pelvic radiotherapy as shown in Table 4, as by eliminating or decreasing the systematic error, the probability of CTV involvement into the radiation portal may increase.3,13,23,27 The patient set-up error predictive factors like age, body mass index (BMI), lumbopelvic balance and pelvic rotation, weight loss, performance status was not taken into account, because of organ motion variation, the prediction of set-up error pattern according to this predictive risk factors might be far-off and need more experience with IGRT using CT, MRI, or radiopaque markers.28
The promising research will need to incorporate the intra-fractional errors by organ motion and breathing, rotational SE and its impact on the CTV to PTV SM for the pelvic radiotherapy for better patient position reproducibility, radiation treatment delivery and to achieve the objective of conformal radiotherapy by better tumor coverage and lesser treatment-related toxicity.
5. Conclusions
The SE may differ in different institutions depending on patient simulation and radiation treatment strategy directly affecting the systemic and random errors. Assessment of SE helps in precise defining the CTV to PTV SM. In our research study, we found the CTV to PTV SM of approximately 8 mm in the Z-axis, 7 mm in the X and Y axis to be appropriate for the cervical cancer patients treated with pelvic conformal radiotherapy for better dose coverage.
Finance and Funding/Grant disclosure
No fund or grant declared
Conflict of Interest
All the author(s) declare(s) that there is no conflict of interest
Acknowledgement
None.
References
- 1.Landberg T., Chavaudra J., Dobbs J. Report 50. J Int Comm Radiat Units Meas. 1993;os26(1) NP-NP. [Google Scholar]
- 2.Landberg T., Chavaudra J., Dobbs J. Report 62. J Int Comm Radiat Units Meas. 1999;os32(1) NP-NP. [Google Scholar]
- 3.Hurkmans C.W., Remeijer P., Lebesque J.V., Mijnheer B.J. Set-up verification using portal imaging; review of current clinical practice. Radiother Oncol. 2001;58:105–120. doi: 10.1016/s0167-8140(00)00260-7. [DOI] [PubMed] [Google Scholar]
- 4.Stroom J.C., Olofsen-Van Acht M.J.J., Quint S. On-line set-up corrections during radiotherapy of patients with gynecologic tumors. Int J Radiat Oncol Biol Phys. 2000;46(2):499–506. doi: 10.1016/s0360-3016(99)00386-7. [DOI] [PubMed] [Google Scholar]
- 5.Haslam J.J., Lujan A.E., Mundt A.J., Bonta D.V., Roeske J.C. Setup errors in patients treated with intensity-modulated whole pelvic radiation therapy for gynecological malignancies. Med Dosim. 2005;30(1):36–42. doi: 10.1016/j.meddos.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Kasabašić M., Faj D., Belaj N., Faj Z., Tomaš I. Implementing of the offline setup correction protocol in pelvic radiotherapy: Safety margins and number of images. Radiol Oncol. 2007;41(1):48–55. [Google Scholar]
- 7.Kneebone A., Gebski V., Hogendoorn N., Turner S. A randomized trial evaluating rigid immobilization for pelvic irradiation. Int J Radiat Oncol Biol Phys. 2003;56(4):1105–1111. doi: 10.1016/s0360-3016(03)00222-0. [DOI] [PubMed] [Google Scholar]
- 8.Hunt M.A., Schultheiss T.E., Desobry G.E., Hakki M., Hanks G.E. An evaluation of setup uncertainties for patients treated to pelvic sites. Int J Radiat Oncol Biol Phys. 1995;32(1):227–233. doi: 10.1016/0360-3016(94)00409-E. [DOI] [PubMed] [Google Scholar]
- 9.Catton C., Lebar L., Warde P. Improvement in total positioning error for lateral prostatic fields using a soft immobilization device. Radiother Oncol. 1997;44(3):265–270. doi: 10.1016/s0167-8140(97)00061-3. http://www.ncbi.nlm.nih.gov/pubmed/9380826 Accessed March 22, 2019. [DOI] [PubMed] [Google Scholar]
- 10.van Herk M., Bruce A., Kroes A.P., Shouman T., Touw A., Lebesque J.V. Quantification of organ motion during conformal radiotherapy of the prostate by three dimensional image registration. Int J Radiat Oncol Biol Phys. 1995;33(5):1311–1320. doi: 10.1016/0360-3016(95)00116-6. http://www.ncbi.nlm.nih.gov/pubmed/7493856 Accessed March 22, 2019. [DOI] [PubMed] [Google Scholar]
- 11.Buchali A., Koswig S., Dinges S. Impact of the filling status of the bladder and rectum on their integral dose distribution and the movement of the uterus in the treatment planning of gynaecological cancer. Radiother Oncol. 1999;52(1):29–34. doi: 10.1016/s0167-8140(99)00068-7. http://www.ncbi.nlm.nih.gov/pubmed/10577683 Accessed March 20, 2019. [DOI] [PubMed] [Google Scholar]
- 12.Toita T., Ohno T., Kaneyasu Y. A Consensus-based guideline defining clinical target volume for primary disease in external beam radiotherapy for intact uterine cervical cancer. Jpn J Clin Oncol. 2011;41(9):1119–1126. doi: 10.1093/jjco/hyr096. [DOI] [PubMed] [Google Scholar]
- 13.Barrett J. On target : Ensuring geometric accuracy in radiotherapy. R Coll Radiol. 2008:1–76. doi:BFCO(08)5. [Google Scholar]
- 14.Möller T.R., Rosenow U., Bentley R.E. Report 42. J Int Comm Radiat Units Meas. 1987;os22(1) NP-NP. [Google Scholar]
- 15.ven Hark M., Remeijer P., Rasch C., Lebesque J.V. The probability of correct target dosage : dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys. 2000;47(4):1121–1135. doi: 10.1016/s0360-3016(00)00518-6. [DOI] [PubMed] [Google Scholar]
- 16.Osei E.K., Jiang R., Barnett R., Fleming K., Panjwani D. Evaluation of daily online set-up errors and organ displacement uncertainty during conformal radiation treatment of the prostate. Br J Radiol. 2009;82(973):49–61. doi: 10.1259/bjr/58088207. [DOI] [PubMed] [Google Scholar]
- 17.Bel A., Vos P.H., Rodrigus P.T. High-precision prostate cancer irradiation by clinical application of an offline patient setup verification procedure, using portal imaging. Int J Radiat Oncol Biol Phys. 1996;35(2):321–332. doi: 10.1016/0360-3016(95)02395-x. [DOI] [PubMed] [Google Scholar]
- 18.Bijhold J., Lebesque J.V., Hart A.A.M., Vijlbrief R.E. Maximizing setup accuracy using portal images as applied to a conformal boost technique for prostatic cancer. Radiother Oncol. 1992;24(4):261–271. doi: 10.1016/0167-8140(92)90233-k. [DOI] [PubMed] [Google Scholar]
- 19.Van den Heuvel F., De Neve W., Verellen D., Coghe M., Coen V., Storme G. Clinical implementation of an objective computer-aided protocol for intervention in intra-treatment correction using electronic portal imaging. Radiother Oncol. 1995;35(3):232–239. doi: 10.1016/0167-8140(95)01569-3. [DOI] [PubMed] [Google Scholar]
- 20.Luchka K., Shalev S. Pelvic irradiation of the obese patient: A treatment strategy involving megavoltage simulation and intratreatment setup corrections. Med Phys. 1996;23(11):1897–1902. doi: 10.1118/1.597752. [DOI] [PubMed] [Google Scholar]
- 21.Olofsen-van Acht M., van den Berg H., Quint S. Reduction of irradiated small bowel volume and accurate patient positioning by use of a bellyboard device in pelvic radiotherapy of gynecological cancer patients. Radiother Oncol. 2001;59(1):87–93. doi: 10.1016/s0167-8140(00)00279-6. http://www.ncbi.nlm.nih.gov/pubmed/11295211 Accessed March 22, 2019. [DOI] [PubMed] [Google Scholar]
- 22.Weiss E., Richter S., Hess C.F. Radiation therapy of the pelvic and paraaortic lymph nodes in cervical carcinoma: A prospective three-dimensional analysis of patient positioning and treatment technique. Radiother Oncol. 2003;68(1):41–49. doi: 10.1016/s0167-8140(03)00080-x. http://www.ncbi.nlm.nih.gov/pubmed/12885451 Accessed March 22, 2019. [DOI] [PubMed] [Google Scholar]
- 23.Kragelj B. Setup error and its effect on safety margin in conformal radiotherapy of the prostate. Radiol Oncol. 2005;39(3):211–217. http://ojs.szd.si/index.php/ro/article/view/1292 [Google Scholar]
- 24.Song P.Y., Washington M., Vaida F. A comparison of four patient immobilization devices in the treatment of prostate cancer patients with three dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys. 1996;34(1):213–219. doi: 10.1016/0360-3016(95)02094-2. http://www.ncbi.nlm.nih.gov/pubmed/12118554 Accessed March 20, 2019. [DOI] [PubMed] [Google Scholar]
- 25.Rudat V., Hammoud M., Pillay Y., Alaradi A.A., Mohamed A., Altuwaijri S. Impact of the frequency of online verifications on the patient set-up accuracy and set-up margins. Radiat Oncol. 2011;6:101. doi: 10.1186/1748-717X-6-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stroom J.C., Heijmen B.J.M. Geometrical uncertainties, radiotherapy planning margins, and the ICRU-62 report. Radiother Oncol. 2002;64(1):75–83. doi: 10.1016/s0167-8140(02)00140-8. [DOI] [PubMed] [Google Scholar]
- 27.Gordon J.J., Siebers J.V. 2009. Coverage-based treatment planning: Optimizing the IMRT PTV to meet a CTV coverage criterion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoon W.S., Yang D.S., Lee J.A., Lee S., Park Y.J., Kim C.Y. Risk factors related to interfractional variation in whole pelvic irradiation for locally advanced pelvic malignancies. Strahlenther Onkol. 2012;188(5):395–403. doi: 10.1007/s00066-011-0049-0. [DOI] [PubMed] [Google Scholar]