Abstract
A bone stress injury (BSI) means that the bones cannot tolerate repeated mechanical loads, resulting in structural fatigue and local bone pain. A delay in BSI diagnosis can lead to more serious injuries, such as stress fractures that require longer treatment periods. Therefore, early detection of BSI is an essential part of management. Risk factors for BSI development include biological and biomechanical factors. Medical history and physical examination are the basics for a BSI diagnosis, and magnetic resonance imaging is helpful for confirming and grading. In this paper, the authors review the overall content of BSI and stress fractures which are common in runners. Through this review, we hope that interest in stress fractures will be raised in Korea and that active researches will be conducted.
Keywords: Stress, Injury, Fractures
Graphical Abstract
INTRODUCTION
A BSI refers to a phenomenon in which bones cannot tolerate repeated mechanical loads, resulting in structural fatigue, local bone pain and tenderness.1,2 BSI varies in severity, with initial findings of periosteal edema and marrow edema. In more severe cases, stress fractures with distinct fracture lines are present.3 Stress fractures account for more than 10% of all sport-related injuries, and can be as high as 30% in running. It also represent up to 20% of the injuries treated in sports medicine clinics.4,5
In runners, BSIs come from the failure of bones to overcome the repetitive, submaximal forces from running.3 BSI is a very common cause of injury in track and field athletes, with an annual incidence of BSI more than 20% in runners.6,7 However, there has been no report on the incidence of BSIs or stress fractures among athletes in Korea. Early diagnosis of BSIs is most important for treatment, because delayed diagnosis and continued running can lead to higher-grades of BSI requiring longer healing time.3,8
The purpose of this review is to broaden the understanding of stress fractures, as well as to assist in the treatment and prevention of stress fractures by providing information about the epidemiology, risk factors, diagnosis and classification of BSI. In addition, we look forward to seeing a lot of interest and follow-up studies in Korea, a barren area of research on stress fractures.
EPIDEMIOLOGY
More than a third of cross-country and long-distance runners experience BSIs,1 and the 1-year prospective incidence of BSI in track and field athletes is reported up to about 21%.6,9 It is important to keep in mind that BSI also recurs well. About 50% of track and field athletes report 1 or more histories of BSI, and up to 12% of cross-country and track athletes with a BSI history are reported to have continued BSI for the next 1–2 years.6,10 Of all sports-related injuries encountered in sports medicine clinics, BSIs account for up to 20%.4 Unfortunately, there have been no epidemiological investigations or related studies on BSIs or stress fractures among athletes in Korea.
In long distance runners, half of the BSI occurs in the tibia and the majority of the other BSI occurs in the femur, fibula, calcaneus and metatarsal bones.9,10,11 Individual weight-bearing patterns and various running biomechanics determine the exact location of BSI.1 For example, long distance runners usually use a rear foot strike method to place weight load on the long bones such as tibia and femur, whereas short distance runners use a forefoot strike, which puts greater loads to the foot bones. Because of this difference in weight-bearing styles, long distance runners are more likely to develop BSIs in their long bones, while short distance runners are more vulnerable to BSIs in the tarsal and metatarsal bones.6
RISK FACTORS
To prevent BSI in runners or establish appropriate treatment strategies when it does occur, it is necessary to recognize the contributing risk factors. The risk factors for BSI are usually divided into biological and biomechanical factors (Table 1).
Table 1. Risk factors for bone stress injury.
| Biologic factors | Biomechanical factors | ||
|---|---|---|---|
| Female, sex | Training pattern | ||
| Genetics | Duration and frequency or intensity/speed changes | ||
| Medications | Bone characteristics | ||
| Anticonvulsants, steroids, antidepressants, antacids | Thinner cortex | ||
| Female athlete triad | Anatomic consideration | ||
| Diet and nutrition | Lean body mass, foot type, smaller calf CSA, LLD | ||
| Insufficient calcium and vitamin D | |||
CSA = cross-sectional area, LLD = leg length discrepancy.
Biological factors
Genetic factors are known to be associated with fracture risk. Drugs like antacids, steroids, and antidepressants can also adversely affect bone health. Lack of calcium and vitamin D increase BSI risk.3 Women who consume less than 800 mg of calcium a day are known to have a nearly six times higher risk of BSI than those who consume more than 1,500 mg.12 A study of BSI risks in female navies with low daily calcium intake reported a 20% decrease in BSI incidence when they took 2,000 mg of calcium and 800 IU of vitamin D per day.13
In a study of male runners, low bone mineral density (BMD) was also found to be an independent risk factor for prolonged BSI healing time.8 In both gender, previous fractures as well as lower BMD have been known to be a risk factor for BSI in runners.9 BMDs of athletes with fracture at the trabecular sites are lower than those with fractures at the cortical site.3
Female athlete triad
The risk of BSI is higher in female athletes than in male athletes.14 This is due to the gender-specific differences called the female athlete triad, which defines the interrelationship of energy availability, menstrual function, and BMD.15 The most serious form of the female athlete triad are low energy availability due to eating disorder, amenorrhea, and osteoporosis.3,15 For female runners, the more components of the triad, the higher the risk of BSI.7
Biomechanical factors
Biomechanical factors are also involved in BSI development, and faulty biomechanics can increase BSI risk. Misalignment or anatomic problems such as leg length discrepancy, small calf circumference, pes cavus and pes planus may contribute.6,16 Dynamic loading patterns and biomechanical factors are also associated with BSI. Average vertical loading rates, peak hip adduction and rear foot eversion during running were increased in runners with a previous tibial stress fracture.17,18,19
External factors, such as running surface, also affect the occurrence of BSI. Rigid running surfaces have been known to increase loads more than smooth surfaces.1 In addition, the amount of running is important, so running greater than 32 km a week increase chances of developing BSI.9
EVALUATION AND DIAGNOSIS
History taking and physical examination
BSIs often appear as gradual activity-related pain and can be confused with simple overuse injuries.1 Therefore, clinician must perform a complete medical history taking and physical examination of the runners present for the BSI assessment. A thorough history taking is the first step in diagnosing a BSI. In most cases, BSI patients have a consistent and predictable history of pain.1 It is especially important to get a complete running history. In female runners, evaluation of female athlete triads is vital, and dietary restriction behaviors, daily intake of calcium and vitamin D, and menstrual irregularities should be investigated. The previous fractures, and family history of low BMD should also be checked.3 Hormornal use, like oral contraceptives, and use of drugs, such as steroids and antacids, which may affect bone health, should be recorded.3
On physical examination, the most obvious feature of a BSI is local bony tenderness and pain during percussion.1,3 Because direct palpation of deep areas is impossible at deeper sites, single-leg hop test or fulcrum test of the femur shaft can be used to cause pain.20 In more severe cases, changes in skin color and local edema may occur.3
Assessment of bone health
For runners with diagnosed BSIs, clinicians should measure BMD and perform an endocrine function assessment.3 According to the definition of the American College of Sports Medicine, Z-score less than −1 are considered to be low bone mass in female athletes who take part in weight-bearing sports.15 For male athletes, no criteria have yet been set. Z-scores less than −2 in both gender are defined as low bone density by the International Society for Clinical Densitometry.21
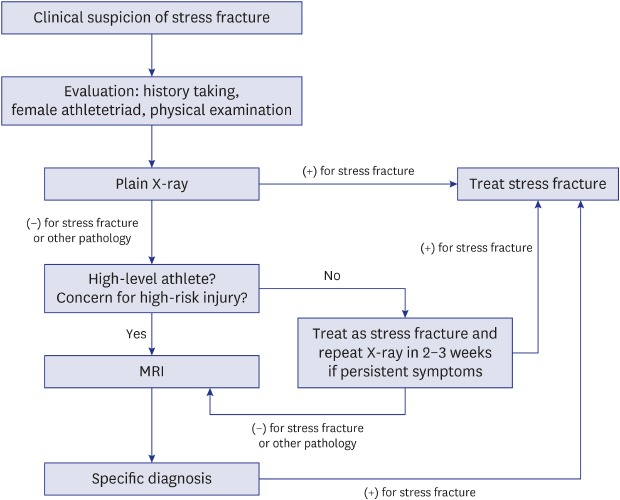
Imaging
For runners with symptoms or signs of BSIs, imaging studies are necessary to make a definitive diagnosis. Simple radiographs are still the first imaging test for BSIs in most clinical situations, but have very low sensitivity due to low resolution and planar characteristics. Computed tomography is also a less sensitive test, but can be used in some cases where fracture identification is needed.22 On the other hand, bone scan test has high sensitivity but the disadvantages are low specificity and high ionizing radiation doses.23 Among the currently available imaging tests, magnetic resonance imaging (MRI) is the test of choice due to its high resolution, no radiation exposure, and combined high sensitivity and specificity.22,24 Two MRI grading scales for BSIs are shown in Table 2.8,25 Recently, the use of diagnostic ultrasound is increasing in sports medicine center. It can be used in the field, enabling early detection of BSIs and continued use in follow-up.2
Table 2. MRI grading scales for bone stress injury.
| MRI grade | Nattiv et al.8 | Fredericson et al.25 |
|---|---|---|
| 1 | Mild marrow or periosteal edema on T2; T1 normal | Mild to moderate periosteal edema on T2; normal marrow on T2 and T1 |
| 2 | Moderate marrow or periosteal edema plus positive T2 | Moderate to severe periosteal edema on T2; marrow edema on T2 but not T1 |
| 3 | Severe marrow or periosteal edema on T2 and T1 | Moderate to severe periosteal edema on T2; marrow edema on T2 and T1 |
| 4 | Severe marrow or periosteal edema on T2 and T1 plus fracture line on T2 or T1 | Moderate to severe periosteal edema on T2; marrow edema on T2 and T1; fracture line present |
MRI = magnetic resonance imaging.
CLASSIFICATION
Injury classification systems can help grading severity, choose treatment options, and determine prognosis.1 In runners who show imaging changes compatible with the symptoms of BSIs, the anatomical location and imaging findings of the lesion are important factors. BSIs can be classified into either low- or high-risk groups, depending on the site of occurrence (Table 3).26,27 Low-risk BSIs are susceptible to compressive forces and usually heal well with activity modification, in which case normal weight-bearing is also possible. High-risk BSIs, on the other hand, are vulnerable to tensile forces and occur in regions with reduced blood flow.28 They are susceptible to delayed union or nonunion and are more likely to progress to complete fractures.1
Table 3. Bone stress injury classification by location.
| Low-risk | High-risk |
|---|---|
| Posteromedial tibia | Anterior cortex of tibia |
| Fibula/lateral malleolus | Medial malleolus |
| Femoral shaft | Femoral neck |
| Pelvis | Navicular |
| Calcaneus | Talus |
| Diaphysis of second to fourth metatarsals | Proximal diaphysis of the fifth metatarsal |
| - | Great-toe sesamoid |
In addition to risk classification by anatomical location, BSIs can be graded according to imaging findings (Table 2). In the grading system, grades 1 and 2 are low-grade BSIs, whereas grades 3 and 4 can be classified as high-grade BSIs.29 After low- and high-grade BSIs, return-to-sport time was reported to be 13.1 and 23.6 weeks, respectively.8
To sum it up, low-grade BSIs at low-risk sites with have the best prognosis and the shortest return time to running. High-grade BSIs at low-risk sites must be identified, as they will require more time to return to running. Because BSIs at high-risk sites take longer time to recover, careful treatment is required regardless of grade.1
TREATMENT
The cornerstone of treatment involves understanding and correcting the factors that caused the injury, and a 2-phase approach consisting of modifying activities and resuming gradual running is used.1,30
General principles
Phase 1 begins with pain control by cold massage, physiotherapy, and analgesics. Nonsteroidal anti-inflammatory drugs should not be used due to its potential negative effect on bone healing.31 Tolerable weight bearing is possible for daily activities, but temporary discontinuation of running and modification of activities are needed in the initial management of low-risk BSIs to allow for tissue healing and to prevent pathological progression.1 Walking boots or assistive gait devices such as cane and crutch can be supplied to athletes who can't walk without pain.1,29 Rigid-soled shoes can be used to reduce the bending forces in athletes with a BSI in the forefoot or midfoot, while cushioned shoes or insoles may provide help athletes with a BSI in the leg or rearfoot.32,33,34
Maintaining conditioning while recovering from a BSI is important for a smooth return to running. Since endurance training athletes experience cardiovascular insufficiency within two weeks after the cessation of training, conditioning exercises should be introduced early.35 There are many ways to maintain cardiovascular fitness while recovering from a BSI, such as swimming, cycling, deep-water running, and antigravity treadmill training. The latter two exercises may be most effective for runners.1
Phase 2 begins if the injured athletes have no pain for 10–14 days. Progressive running programs are applied to the treatment of low-risk BSIs. One week after the loss of bony tenderness, running can be resumed at the half of original speed and distance. Athletes with a healing fracture should run only every other day for the first 2 weeks after the pain is resolved, and gradually increase to the pre-injury levels over 3 to 6 weeks with supervision.29
High-risk BSIs require different management. It can range from prolongation of activity modification to non-weight bearing, with or without a cast and/or surgical fixation.1 Complete healing should be confirmed prior to return to play in order to prevent full fracture and complications.36
Antigravity treadmill training (ATT)
An antigravity treadmill can be used initially at over-ground running, if available. Because ATT allows athletes to run with lower bone load at higher intensity early in recovery.1 Antigravity treadmills consist of a treadmill with a pressure-controlled chamber filled with air that wraps around the lower the body (Fig. 1). They allow for adjustable body weight support and fitness enhancement for exercise while protecting the BSI site.37,38
Fig. 1. Antigravity treadmill. Reproduced with permission from AlterG, Inc.
PREVENTION
Ball sports participation during adolescence
Engaging in ball sports like soccer and basketball during adolescence for 2 years has been reported to reduce the risk of BSI.39
Sufficient intake of calcium and vitamin D
Getting enough calcium and vitamin D may reduce risk for BSIs. Female runners consuming 800 mg of calcium daily are six times more likely to develop stress fractures than those who consume 1,500 mg daily.12
Identification and prevention of female athlete triad
In female athletes, identifying and correction of energy imbalance, and recovery of menstrual function may be the best way to maintain proper bone health during adolescence.29
Preparticipation screening
Some behavior and activity patterns should be examined for all athletes at preparticipation screening.29 They include drinking more than 10 bottles per week, smoking, participation in excessive physical activity with insufficient rest time, sudden increase in physical activity, and running mainly on hard surfaces.40,41
CONCLUSION
BSIs are common form of overuse injuries encountered by athletes, particularly in runners. Therefore, clinicians should keep in mind the possibility of such injury in differential diagnosis of musculoskeletal pain in running athletes. Early effective treatment can promote return to sports, and eliminating underlying risk factors may help prevent future injuries.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Koo JH.
- Writing - original draft: Song SH.
- Writing - review & editing: Koo JH.
References
- 1.Warden SJ, Davis IS, Fredericson M. Management and prevention of bone stress injuries in long-distance runners. J Orthop Sports Phys Ther. 2014;44(10):749–765. doi: 10.2519/jospt.2014.5334. [DOI] [PubMed] [Google Scholar]
- 2.Fukushima Y, Ray J, Kraus E, Syrop IP, Fredericson M. A review and proposed rationale for the use of ultrasonography as a diagnostic modality in the identification of bone stress injuries. J Ultrasound Med. 2018;37(10):2297–2307. doi: 10.1002/jum.14588. [DOI] [PubMed] [Google Scholar]
- 3.Tenforde AS, Kraus E, Fredericson M. Bone stress injuries in runners. Phys Med Rehabil Clin N Am. 2016;27(1):139–149. doi: 10.1016/j.pmr.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Fredericson M, Jennings F, Beaulieu C, Matheson GO. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17(5):309–325. doi: 10.1097/RMR.0b013e3180421c8c. [DOI] [PubMed] [Google Scholar]
- 5.Robertson GA, Wood AM. Lower limb stress fractures in sport: optimising their management and outcome. World J Orthop. 2017;8(3):242–255. doi: 10.5312/wjo.v8.i3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennell KL, Malcolm SA, Thomas SA, Wark JD, Brukner PD. The incidence and distribution of stress fractures in competitive track and field athletes. A twelve-month prospective study. Am J Sports Med. 1996;24(2):211–217. doi: 10.1177/036354659602400217. [DOI] [PubMed] [Google Scholar]
- 7.Barrack MT, Gibbs JC, De Souza MJ, Williams NI, Nichols JF, Rauh MJ, et al. Higher incidence of bone stress injuries with increasing female athlete triad-related risk factors: a prospective multisite study of exercising girls and women. Am J Sports Med. 2014;42(4):949–958. doi: 10.1177/0363546513520295. [DOI] [PubMed] [Google Scholar]
- 8.Nattiv A, Kennedy G, Barrack MT, Abdelkerim A, Goolsby MA, Arends JC, et al. Correlation of MRI grading of bone stress injuries with clinical risk factors and return to play: a 5-year prospective study in collegiate track and field athletes. Am J Sports Med. 2013;41(8):1930–1941. doi: 10.1177/0363546513490645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tenforde AS, Sayres LC, McCurdy ML, Sainani KL, Fredericson M. Identifying sex-specific risk factors for stress fractures in adolescent runners. Med Sci Sports Exerc. 2013;45(10):1843–1851. doi: 10.1249/MSS.0b013e3182963d75. [DOI] [PubMed] [Google Scholar]
- 10.Kelsey JL, Bachrach LK, Procter-Gray E, Nieves J, Greendale GA, Sowers M, et al. Risk factors for stress fracture among young female cross-country runners. Med Sci Sports Exerc. 2007;39(9):1457–1463. doi: 10.1249/mss.0b013e318074e54b. [DOI] [PubMed] [Google Scholar]
- 11.Brukner P, Bradshaw C, Khan KM, White S, Crossley K. Stress fractures: a review of 180 cases. Clin J Sport Med. 1996;6(2):85–89. [PubMed] [Google Scholar]
- 12.Nieves JW, Melsop K, Curtis M, Kelsey JL, Bachrach LK, Greendale G, et al. Nutritional factors that influence change in bone density and stress fracture risk among young female cross-country runners. PM R. 2010;2(8):740–750. doi: 10.1016/j.pmrj.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 13.Lappe J, Cullen D, Haynatzki G, Recker R, Ahlf R, Thompson K. Calcium and vitamin d supplementation decreases incidence of stress fractures in female navy recruits. J Bone Miner Res. 2008;23(5):741–749. doi: 10.1359/jbmr.080102. [DOI] [PubMed] [Google Scholar]
- 14.Wentz L, Liu PY, Haymes E, Ilich JZ. Females have a greater incidence of stress fractures than males in both military and athletic populations: a systemic review. Mil Med. 2011;176(4):420–430. doi: 10.7205/milmed-d-10-00322. [DOI] [PubMed] [Google Scholar]
- 15.Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP, et al. American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867–1882. doi: 10.1249/mss.0b013e318149f111. [DOI] [PubMed] [Google Scholar]
- 16.Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk factors for recurrent stress fractures in athletes. Am J Sports Med. 2001;29(3):304–310. doi: 10.1177/03635465010290030901. [DOI] [PubMed] [Google Scholar]
- 17.Milner CE, Ferber R, Pollard CD, Hamill J, Davis IS. Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc. 2006;38(2):323–328. doi: 10.1249/01.mss.0000183477.75808.92. [DOI] [PubMed] [Google Scholar]
- 18.Pohl MB, Mullineaux DR, Milner CE, Hamill J, Davis IS. Biomechanical predictors of retrospective tibial stress fractures in runners. J Biomech. 2008;41(6):1160–1165. doi: 10.1016/j.jbiomech.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Milner CE, Hamill J, Davis IS. Distinct hip and rearfoot kinematics in female runners with a history of tibial stress fracture. J Orthop Sports Phys Ther. 2010;40(2):59–66. doi: 10.2519/jospt.2010.3024. [DOI] [PubMed] [Google Scholar]
- 20.Johnson AW, Weiss CB, Jr, Wheeler DL. Stress fractures of the femoral shaft in athletes--more common than expected. A new clinical test. Am J Sports Med. 1994;22(2):248–256. doi: 10.1177/036354659402200216. [DOI] [PubMed] [Google Scholar]
- 21.Lewiecki EM, Gordon CM, Baim S, Leonard MB, Bishop NJ, Bianchi ML, et al. International society for clinical densitometry 2007 adult and pediatric official positions. Bone. 2008;43(6):1115–1121. doi: 10.1016/j.bone.2008.08.106. [DOI] [PubMed] [Google Scholar]
- 22.Gaeta M, Minutoli F, Scribano E, Ascenti G, Vinci S, Bruschetta D, et al. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005;235(2):553–561. doi: 10.1148/radiol.2352040406. [DOI] [PubMed] [Google Scholar]
- 23.Dobrindt O, Hoffmeyer B, Ruf J, Steffen IG, Zarva A, Richter WS, et al. Blinded-read of bone scintigraphy: the impact on diagnosis and healing time for stress injuries with emphasis on the foot. Clin Nucl Med. 2011;36(3):186–191. doi: 10.1097/RLU.0b013e318208f0e6. [DOI] [PubMed] [Google Scholar]
- 24.Kiuru MJ, Pihlajamäki HK, Hietanen HJ, Ahovuo JA. MR imaging, bone scintigraphy, and radiography in bone stress injuries of the pelvis and the lower extremity. Acta Radiol. 2002;43(2):207–212. doi: 10.1080/028418502127347790. [DOI] [PubMed] [Google Scholar]
- 25.Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472–481. doi: 10.1177/036354659502300418. [DOI] [PubMed] [Google Scholar]
- 26.Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8(6):344–353. doi: 10.5435/00124635-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29(1):100–111. doi: 10.1177/03635465010290010201. [DOI] [PubMed] [Google Scholar]
- 28.Mandell JC, Khurana B, Smith SE. Stress fractures of the foot and ankle, part 1: biomechanics of bone and principles of imaging and treatment. Skeletal Radiol. 2017;46(8):1021–1029. doi: 10.1007/s00256-017-2640-7. [DOI] [PubMed] [Google Scholar]
- 29.Chen YT, Tenforde AS, Fredericson M. Update on stress fractures in female athletes: epidemiology, treatment, and prevention. Curr Rev Musculoskelet Med. 2013;6(2):173–181. doi: 10.1007/s12178-013-9167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raasch WG, Hergan DJ. Treatment of stress fractures: the fundamentals. Clin Sports Med. 2006;25(1):29–36. doi: 10.1016/j.csm.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 31.Ziltener JL, Leal S, Fournier PE. Non-steroidal anti-inflammatory drugs for athletes: an update. Ann Phys Rehabil Med. 2010;53(4):278–282. doi: 10.1016/j.rehab.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 32.Ekenman I, Milgrom C, Finestone A, Begin M, Olin C, Arndt T, et al. The role of biomechanical shoe orthoses in tibial stress fracture prevention. Am J Sports Med. 2002;30(6):866–870. doi: 10.1177/03635465020300061801. [DOI] [PubMed] [Google Scholar]
- 33.Milgrom C, Finestone A, Ekenman I, Simkin A, Nyska M. The effect of shoe sole composition on in vivo tibial strains during walking. Foot Ankle Int. 2001;22(7):598–602. doi: 10.1177/107110070102200713. [DOI] [PubMed] [Google Scholar]
- 34.Arndt A, Westblad P, Ekenman I, Lundberg A. A comparison of external plantar loading and in vivo local metatarsal deformation wearing two different military boots. Gait Posture. 2003;18(2):20–26. doi: 10.1016/s0966-6362(02)00191-1. [DOI] [PubMed] [Google Scholar]
- 35.Coyle EF, Martin WH, 3rd, Sinacore DR, Joyner MJ, Hagberg JM, Holloszy JO. Time course of loss of adaptations after stopping prolonged intense endurance training. J Appl Physiol. 1984;57(6):1857–1864. doi: 10.1152/jappl.1984.57.6.1857. [DOI] [PubMed] [Google Scholar]
- 36.Kaeding CC, Najarian RG. Stress fractures: classification and management. Phys Sportsmed. 2010;38(3):45–54. doi: 10.3810/psm.2010.10.1807. [DOI] [PubMed] [Google Scholar]
- 37.Grabowski AM. Metabolic and biomechanical effects of velocity and weight support using a lower-body positive pressure device during walking. Arch Phys Med Rehabil. 2010;91(6):951–957. doi: 10.1016/j.apmr.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 38.Hoffman MD, Donaghe HE. Physiological responses to body weight--supported treadmill exercise in healthy adults. Arch Phys Med Rehabil. 2011;92(6):960–966. doi: 10.1016/j.apmr.2010.12.035. [DOI] [PubMed] [Google Scholar]
- 39.Tenforde AS, Sainani KL, Carter Sayres L, Milgrom C, Fredericson M. Participation in ball sports may represent a prehabilitation strategy to prevent future stress fractures and promote bone health in young athletes. PM R. 2015;7(2):222–225. doi: 10.1016/j.pmrj.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 40.Patel DS, Roth M, Kapil N. Stress fractures: diagnosis, treatment, and prevention. Am Fam Physician. 2011;83(1):39–46. [PubMed] [Google Scholar]
- 41.Wentz L, Liu PY, Ilich JZ, Haymes EM. Dietary and training predictors of stress fractures in female runners. Int J Sport Nutr Exerc Metab. 2012;22(5):374–382. doi: 10.1123/ijsnem.22.5.374. [DOI] [PubMed] [Google Scholar]



