Abstract
Racial health inequities are not fully explained by socioeconomic status (SES) measures like education, income and wealth. The largest inequities are observed among African American and white college graduates suggesting that African Americans do not receive the same health benefits of education. African Americans do not receive the same income and wealth returns of college education as their white counterparts indicating a racial non-equivalence of SES that may affect health inequities. The aim of this study is to determine whether racial non-equivalence of SES mediates race inequities in self-rated health by education and sex. Using data from the 2007–2016 National Health and Nutrition Examination Survey in the United States, the mediation of the associations between race and self-rated health through household income ≥400% federal poverty line, homeownership, and investment income were assessed among college graduates and non-college graduates by sex. Indirect associations were observed among college graduate women (odds = 0.08, standard error (s.e.) = 0.03), and non-college graduate men (odds = 0.14, s.e. = 0.02) and women (odds = 0.06, s.e. = 0.02). Direct associations between race and self-rated health remained after accounting for household income and wealth indicators suggesting that race differences in income and wealth partially mediate racial inequities in self-rated health. This study demonstrates that the racial non-equivalence of SES has implications for health inequities, but the magnitude of indirect associations varied by sex. Other factors like discrimination, health pessimism and segregation should be considered in light of the racial non-equivalence of SES and racial inequities in self-rated health.
Highlights
-
•
Racial inequities in self-rated health increase in magnitude as educational attainment increases.
-
•
College graduate African Americans have lower incomes and less wealth than whites.
-
•
Racial inequities in self-rated health among college graduate women and men are mediated by income and wealth.
1. Introduction
Racial health inequities are of important interest to public health professionals, policymakers and healthcare practitioners (Beck, Finch, Lin, Hummer, & Masters, 2014; Belgrave & Abrams, 2016; Landrine & Corral, 2014; Centers for Disease Control and Prevention, 2013; Yearby, 2018). Large differences in physical health outcomes are observed between African Americans and whites, including higher all-cause mortality rates and higher prevalence of chronic conditions among African Americans (Centers for Disease Control and Prevention, 2013). African Americans experience inequities with regard to self-rated health, a subjective health measure. Self-rated health is a predictor of mortality and is associated with other health conditions such as hypertension, stroke, heart disease, and disability (Benyamini, Blumstein, Lusky, & Modan, 2003a; Chandola & Jenkinson, 2000; Idler & Benyamini, 1997; Idler, Hudson & Leventhal, 1999; Schnittker & Bacak, 2014). African Americans are more likely to report fair or poor health compared to whites (Cummings & Jackson, 2008; Spencer et al., 2009; Yao & Robert, 2008), and there are racial differences in the associations between self-rated health and mortality (Ferraro & Kelley-Moore, 2001; Woo & Zajacova, 2017). However, self-rated health is associated with identity, comparison and adaptation for African Americans (McMullen & Luborsky, 2006) suggesting potential race differences in the attribution of self-rated health. Because self-rated health is a strong predictor of mortality and morbidity (Benyamini, Leventhal, & Leventhal, 2003b; Idler & Benyamini, 1997), fully explicating racial differences in self-rated health is important to understanding racial inequities in mortality and other health outcomes. Racial inequities in self-rated health can persist after accounting for race differences in important predictors like health behaviors, number of chronic conditions, psychosocial factors, social environment and socioeconomic status (SES) (Cummings & Jackson, 2008; Farmer & Ferraro, 2005; Spencer et al., 2009; Yao & Robert, 2008).
1.1. Race, socioeconomic status (SES) and health
SES has long been implicated in racial health inequities in the U.S. (Braveman, Cubbin, Egerter, Williams, & Pamuk, 2010; LaVeist, 2005; Nuru-Jeter et al., 2018; Williams, Mohammed, Leavell, & Collins, 2010; Williams, Priest, & Anderson, 2016). SES is a construct that captures social status, power and material resources (Krieger, Williams, & Moss, 1997; Nuru-Jeter et al., 2018), and is considered a fundamental cause of disparities in health (Link & Phelan, 1995; Phelan, Link, & Tehranifar, 2010; Williams & Jackson, 2005). Income and education are the most widely used indicators of SES in public health research in the U.S. (Adler & Newman, 2002; Nuru-Jeter et al., 2018). Because of the persistent disadvantages in income, education and other SES indicators experienced by African Americans due to structural and institutional racism (Gee & Ford, 2011; Yearby, 2018), scholars have sought to examine SES as an important factor in differences in health between African Americans and whites (Farmer & Ferraro, 2005; Nuru-Jeter et al., 2018; Williams et al., 2010; Williams et al., 2016). However, SES does not fully explain racial differences in health (Nuru-Jeter et al., 2018; Williams et al., 2010; Williams et al., 2016), and SES does not account for disparities in self-rated health among African Americans and whites (Beck et al., 2014).
The literature has demonstrated a nuanced association between race, SES and self-rated health such that the SES-health gradient is weaker or non-existent among African Americans. The SES-health gradient generally finds better self-rated health with increasing SES (Braveman et al., 2010; Farmer & Ferraro, 2005; Phelan et al., 2010). Studies find a strong positive association between education and self-rated health among whites, but a weak association among African Americans or no association at all (Braveman et al., 2010; Holmes & Zajacova, 2014). There are variations in associations between self-rated health and different SES measures (Braveman et al., 2005; Pollack, Chideya, Cubbin, Dekker, & Braveman, 2007). Several studies have demonstrated that the associations between self-rated health and various SES measures like education (Boen, 2016; Braveman et al., 2010; Farmer & Ferraro, 2005; Holmes & Zajacova, 2014; Kimbro, Bzostek, Goldman, & Rodríguez, 2008; Liu & Hummer, 2008), income (Boen, 2016; Braveman et al., 2010), homeownership (Finnigan, 2014; Ortiz & Zimmerman, 2013) and wealth (Boen, 2016; Pollack et al., 2013) differ by race. The weaker SES-health gradient among African Americans can result in larger inequities in self-rated health between higher SES African Americans and whites (Farmer & Ferraro, 2005).
1.2. The Diminishing Returns Hypothesis and racial non-equivalence of SES
Studies suggest that race inequities in self-rated health increase in magnitude as SES increases (Assari, 2018; Farmer & Ferraro, 2005; Wilson, Thorpe, & LaVeist, 2017). For example, a study by Wilson et al. (2017) found racial inequities in self-rated health were observed among adults with household incomes ≥$175,000 (Wilson et al., 2017). Farmer and Ferraro (2005) highlighted the larger gap in self-rated health among African Americans and whites with higher education (Farmer & Ferraro, 2005). Wider gaps in health between high SES African Americans and whites has led to theories such as “The Diminishing Returns Hypothesis” which suggests that African Americans do not receive the same health returns of high SES as whites (Farmer & Ferraro, 2005). Posited explanations can include the role of childhood adversity and a lifecourse perspective on SES (Boen, 2016; Brown, Richardson, Hargrove, & Thomas, 2016; Hargrove & Brown, 2015; Turner, Thomas, & Brown, 2016), greater reported discrimination that may negate the health benefits of higher SES (Colen, Ramey, Cooksey, & Williams, 2018; Hudson et al., 2012, 2013), and unmet expectations and status incongruence (Holmes & Zajacova, 2014) among high SES African Americans. The latter centers on the non-equivalence of SES among African Americans compared to whites (Adler & Stewart, 2010; Braveman et al., 2005; Do, Frank, & Finch, 2012; Kaufman, 2008; Kaufman, Cooper, & McGee, 1997; Krieger et al., 1997; Landrine & Corral, 2014; Nuru-Jeter et al., 2018; Pearson, 2008; Shavers, 2007; Turner, Brown, & Hale, 2017; Williams et al., 2010; Williams et al., 2016). Pearson (2008) suggests that one of the factors behind the weaker or non-existent associations between SES and health among African Americans is that, because of restricted access to income, education and wealth for African Americans throughout U.S. history, the traditional markers of high SES do not have the same social status meaning for African Americans as they do for whites (Pearson, 2008).
Another view of the non-equivalence of SES considers the fact that when African Americans have one high SES marker, like college education or high income, they do not experience the other markers of high SES that whites do (Williams et al., 2016). For example, Williams et al. (2016) point to lower household income levels among African Americans who are college graduates compared to whites who are college graduates, and argue that this non-equivalence of SES between African Americans and whites contributes to racial inequities in health (D. R. Williams et al., 2010; Williams et al., 2016). Additionally, higher income African Americans live in poorer neighborhoods (Reardon, Fox, & Townsend, 2015) and have less wealth than their white counterparts (Meschede, Taylor, Mann, & Shapiro, 2017; Shapiro, Meschede, & Osoro, 2014; Sullivan, Meschede, Dietrich, & Shapiro, 2015). There are also racial differences in wealth accumulation (Brown, 2016) such that college graduate African Americans have less wealth than college graduate whites (Hanks, Solomon, & Weller, 2018; Meschede et al., 2017). African Americans are also less likely to have intergenerational wealth (Killewald & Bryan, 2018). Policies have historically restricted wealth generation and transmission of wealth among African Americans and promoted these opportunities among whites (Hanks et al., 2018; Rothstein, 2017). Structural racism may be defined as “the macrolevel systems, social forces, institutions, ideologies, and processes that interact with one another to generate and reinforce inequities among racial and ethnic groups” (Gee & Ford, 2011). This indicates that racial non-equivalence of SES is associated with structural racism.
Scholars suggest that the racial non-equivalence of SES is likely a key contributor to racial health inequities (Phelan & Link, 2015; Williams & Jackson, 2005; Williams et al., 2010; Williams et al., 2016). The pathways between education and health differ from those between income and health or wealth and health (Braveman et al., 2005; Nuru-Jeter et al., 2018). These SES indicators are correlated to a degree (Braveman et al., 2005), but the differences in pathways with health and the racial non-equivalence of SES (that is, the inequities in income and wealth between college graduate African Americans and whites) could be important to understanding The Diminishing Returns Hypothesis and racial inequities in self-rated health. For example, education is theorized to be associated with health-related knowledge and prestige (Braveman et al., 2005), while income is associated with purchasing of resources like healthcare, housing, and nutrition (Adler & Newman, 2002). Wealth is thought to be associated with health because it is associated with environmental factors, financial security and stress (Hajat, Kaufman, Rose, Siddiqi, & Thomas, 2011; Pollack et al., 2013). Additionally, education is posited as a key determinant of income and occupation (Adler & Newman, 2002), and potentially wealth. Because income and wealth are both associated with better self-rated health among African Americans (Boen, 2016; Finnigan, 2014; Pollack et al., 2013) but income and wealth levels are lower in college graduate African Americans (Hanks et al., 2018; Williams et al., 2010), it is possible that these racial inequities in income and wealth indicators among college graduates may account for at least some of the race differences in self-rated health among college graduate African Americans and whites (Williams et al., 2010; Williams et al., 2016). One study has suggested that income partially mediates the race disparity in self-rated health as education increases (Assari, 2018). However, the study did not measure the potential mediating effects of measures of wealth, leaving a gap in the literature.
1.3. Aim & hypothesis
The aim of this study is to determine the role of the racial non-equivalence of SES in inequities in self-rated health among college graduate African Americans and whites. The study will examine whether race differences in income and wealth (measured as homeownership and income from investments) mediate race differences in self-rated health among African Americans and whites who completed a 4-year college degree. The mediation of race differences in self-rated health will also be assessed among non-college graduates to compare the results by educational attainment. Mediation analyses will be stratified by education for several reasons. First, previous studies on the Diminishing Returns Hypotheses have focused on the diminished returns of education and find that racial disparities in self-rated health are larger in college graduates compared to those who had not completed high school (Bell, Thorpe, Bowie, & LaVeist, 2018a; Farmer & Ferraro, 2005). Second, education is generally thought to influence income through occupational opportunities (Adler & Newman, 2002). Third, racial differences in wealth are also associated with education as demonstrated by studies that find that college graduate African Americans have less wealth than whites who had not completed high school (Hamilton, Darity, WilliamPrice, Sridharan, & Tippett, 2015). It is hypothesized that race differences in self-rated health among college graduates will be fully accounted for by income and wealth. Analyses will also be stratified by sex. Previous work has demonstrated that race, SES and sex interact on self-rated health (Brown et al., 2016; Cummings & Jackson, 2008), so it is possible that the racial non-equivalence of SES accounts for racial inequities in self-rated health differently among women and men. The results of this study will further understanding about the reduced benefits of college education on self-rated health among African Americans compared to whites, and will assist efforts to eliminate racial health inequities.
2. Methods
2.1. Data and variables
The National Health and Nutrition Examination Survey (NHANES) is an ongoing nationally representative survey of the health, functional and nutritional status of the U.S. population that is completed over two consecutive year. The civilian, non-institutionalized population is sampled in each sequential series of this cross-sectional survey. The following groups were oversampled: low-income individuals, youth aged 12 to 19 years, adults over age 60 years, and those who identified as black/African American and Mexican American. NHANES used a stratified, multistage probability sampling design where data were collected in two phases. First, data about respondents’ health history, health behaviors and risk factors were obtained during a home interview. Participants were then invited to take part in a medical examination that included a detailed physical examination and laboratory testing. Previous studies on the Diminished Returns Hypothesis have used data from NHANES III (Farmer & Ferraro, 2005). Additionally, NHANES has data on adults across the age spectrum. Other studies on self-rated health or racial inequities in higher SES adults have focused on older or younger adults specifically (Brown et al., 2016; Colen et al., 2018; Kimbro et al., 2008). Data on investment income was first collected in NHANES 2007–2008. Therefore, data from 2007 to 2016 were combined to obtain a sufficient sample college graduate African Americans in order for the use of complex survey weights required of analysis of NHANES data. Respondents were asked whether they were Hispanic or Latino and asked to which racial group they belong. Those who responded that they were non-Hispanic black or white and who were not missing data on any analytic variables were included in this study (n = 14,823).
The dependent variable was self-rated health. Previous studies that have examined the Diminishing Returns Hypothesis and the interrelationship between race, SES and health have studied this particular health outcomes (Boen, 2016; Colen et al., 2018; Farmer & Ferraro, 2005). Respondents were asked “Would you say your health in general is: excellent, very good, good, fair or poor?” A categorical variable was created such that those who responded “excellent” were given a value of 0, “very good” a value of 1, “good” a value of 2, “fair” a value of 3, and those who responded “poor” were given a value of 4.
The independent variable was race such that those who identify as non-Hispanic white were given a value of “0” and those who identify as African American were given a value of “1”. The potential mediating SES variables included household income, homeownership and investment income. Respondents were asked their household income and household size was reported. Income as a percentage of the federal poverty line (FPL) was calculated and a dichotomous variable was created such that those with incomes ≥400% FPL were given a value of “1” and those with income <400% FPL were given a value of “0”. Respondents were asked whether their home was owned or being bought, rented or some other arrangement. A dichotomous variable was calculated to represent those who owned or were buying their home. Respondents were asked if they or any family member living in the home received interest from savings or other bank accounts, income from dividends received from stocks or mutual funds or net income from property, royalties, estates or trusts. Those who responded “yes” received a value of “1” and those who responded “no” received a value of “0”.
Education was included as a stratifying variable. Respondents were asked their level of educational attainment and a variable with the following categories was created: non-high school graduate, high school graduate/GED equivalent recipient, some college or Associate's degree and 4-year college graduate. Sex was dichotomized as female or male and analyses were stratified by sex.
Age, marital status, insurance status, chronic conditions, body mass index (BMI), depressive symptoms, smoking status, alcohol intake, and physical inactivity were included as covariates in statistical analyses. Age and BMI was measured continuously while other variables were measured dichotomously or categorically. Marital status was categorized as currently married or living with partner, formerly married (separated, divorced or widowed) and never married. Insurance status was determined by whether the respondent reported having health insurance or not. The respondents were asked whether or not they had been diagnosed with angina, asthma, arthritis, cancer, chronic bronchitis, congestive heart failure, coronary heart disease, diabetes, emphysema, heart attack, hypertension, a liver condition, or stroke. A dichotomous variable was created to indicate having one or more of these chronic conditions. Measured height and weight were collected in the medical examination and body mass index (BMI) was calculated as weight in kilograms per height in squared meters. Depressive symptoms were assessed by the Patient Health Questionnaire-9 and categorized as minimal, mild, moderate, moderately severe or severe. Those who reported currently smoking cigarettes some days or everyday were categorized as current smokers. Variables that measured the frequency of alcohol consumption were used to categorize a variable on alcohol intake. These categories included: never, less than one drink per day, one to two drinks per day, and more than two drinks per day.
2.2. Analytic strategy
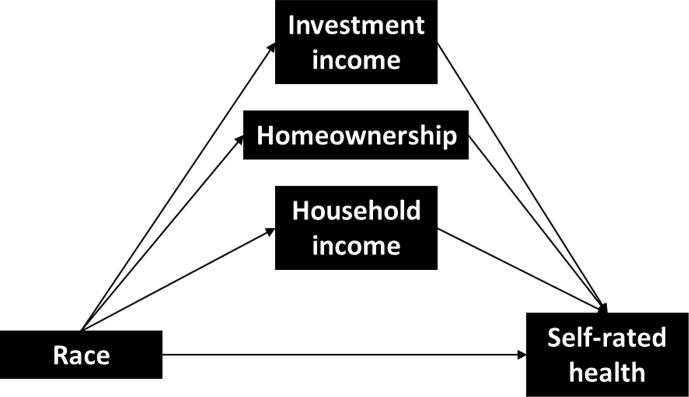
The mean and proportional differences between race groups for analytical variables were evaluated using Student's t (for continuous variables) and chi-square tests (for dichotomous or categorical variables). The associations between race, educational attainment and self-rated health (Model 1) were assessed among women and men using ordinal regressions. A multiplicative interaction term between race and education was included in regressions to determine whether the association between race and self-rated health differed by level of education (Model 2). Fig. 1 illustrates the mediation of the association between race and self-rated health through income, homeownership and investment income. Using the Karlson, Holm & Breen (KHB) method (Breen, Karlson, & Holm, 2013; Karlson, Holm, & Breen, 2012; Kohler, Karlson, & Holm, 2011), the total, direct and indirect associations between race and self-rated health through household income, homeownership and investment income are assessed. The KHB method allows for the assessment of mediation for a categorical dependent variable (Buis, 2010; Erikson, Goldthorpe, Jackson, Yaish, & Cox, 2005; Karlson et al., 2012). This method also displays decomposition of the indirect association through multiple mediators (Kohler et al., 2011). This method has previously been used to assess multiple mediators of race differences in health outcomes including self-rated health (Daw, 2017; Santos-Lozada & Daw, 2018). The KHB method displays results for the reduced model which does not include mediators and should be understood as the total association, and the full model which does include mediators and is the direct association between race and self-rated health. The KHB method also calculates the difference between these models which is understood as the indirect association of race with self-rated health through the mediators. Additionally, the KHB method calculates the percentage of the total association that is due to the mediators. Following the procedure recommended by the National Center for Health Statistics, all analyses used Taylor-linearization procedures for the complex multistage sampling design and a weight variable was created to account for the combining of multiple years of NHANES. STATA statistical software, version 14 (StataCorp LP, College Station, TX) was used for all statistical analyses. .
Fig. 1.
Mediation of the association between race and self-rated health through household income, homeownership and investment income.
3. Results
Racial differences in demographics, socioeconomic status (SES) and self-rated health are displayed in Table 1. A higher percentage of African Americans were women. African Americans were younger, less likely to be currently married and less likely to be insured. Fewer African Americans had ≥1 chronic condition, but African Americans had higher average BMI than whites and were more likely to have severe depressive symptoms. African Americans were more likely to be current smokers, never drinkers and to be physically inactive. A lower percentage of African Americans were college graduates (p < 0.001). Fewer than two in ten (19.3%) African Americans had household incomes that were ≥400% of the federal poverty line (FPL), while about twice as many whites (43.2%) were in that income category (p < 0.001). About half (47.1%) of African Americans were homeowners, while about three-quarters (74.8%) of whites were homeowners (p < 0.001). A smaller percentage of African Americans (12.9%) had investment income compared to whites (44.5%, p < 0.001). A smaller percentage of African Americans (8.2%) reported excellent health than whites (11.8%), and a larger percentage of African Americans reported poor health (3.7%) compared to whites (2.3%, p < 0.001).
Table 1.
Selected demographic, socioeconomic status and health-related measures by race, NHANES 2007–2016.
| African American |
White |
p-value | |
|---|---|---|---|
| N = 4,744 | N = 10,079 | ||
| Women, % | 55.5 | 51.7 | <0.001 |
| Age (years), mean ± s.e. | 44.8 ± 0.4 | 49.4 ± 0.3 | <0.001 |
| Marital status, % | |||
| Currently | 42.6 | 65.6 | <0.001 |
| Formerly | 23.6 | 18.9 | |
| Never | 33.9 | 15.5 | |
| Insured, % | 76.7 | 87.9 | <0.001 |
| ≥1 chronic condition, % | 58.9 | 60.9 | 0.047 |
| BMI (kg/m2), mean ± s.e. | 30.7 ± 0.1 | 28.7 ± 0.1 | <0.001 |
| Depressive symptoms, % | |||
| Minimal | 76.7 | 79.2 | 0.005 |
| Mil | 14.6 | 13.9 | |
| Moderate | 5.4 | 4.4 | |
| Moderately severe | 2.5 | 1.8 | |
| Severe | 0.9 | 0.7 | |
| Current smoker, % | 25.6 | 20.4 | <0.001 |
| Alcohol intake, % | |||
| Never | 32.1 | 19.0 | <0.001 |
| Less than 1 drink per day | 55.3 | 65.7 | |
| 1–2 drinks per day | 3.3 | 5.1 | |
| >2 drinks per day | 9.3 | 10.2 | |
| Physically inactive, % | 53.3 | 44.1 | <0.001 |
| Education, % | |||
| Non-high school graduate | 21.5 | 11.3 | <0.001 |
| High school graduate/GED equivalent | 26.2 | 22.4 | |
| Some college/Associate's degree | 34.7 | 32.7 | |
| 4-year college graduate | 17.6 | 33.6 | |
| Income >400% federal poverty line (FPL), % | 19.3 | 43.2 | <0.001 |
| Homeowner, % | 47.1 | 74.8 | <0.001 |
| Investment income, % | 12.9 | 44.5 | <0.001 |
| Self-rated health, % | |||
| Excellent | 8.2 | 11.8 | <0.001 |
| Very good | 23.6 | 36.7 | |
| Good | 42.8 | 37.9 | |
| Fair | 21.7 | 11.4 | |
| Poor | 3.7 | 2.3 | |
In Table 2, the interactions between race, and education on worse self-rated health are displayed by sex. Adjusting for covariates, Model 1 demonstrates that African American women have 0.61 higher log-odds of worse self-rated health (odds = 0.61, s.e. = 0.05) and the odds of worse self-rated health decreases with educational attainment. Among men, African Americans had higher odds of worse self-rated health (odds = 0.25, s.e. = 0.06) and being a college graduate was associated with lower odds of poorer self-rated health compared to men without a high school diploma (odds = −0.85, s.e. = 0.10) in Model 1. The interaction between race and educational attainment on self-rated health is assessed in Models 2. Among women, there was no significant interaction. However, among men, race interacted with being a college graduate (odds = 0.41, s.e. = 0.17) suggesting diminished returns of education on self-rated health among African American men.
Table 2.
Associations between race, education, and self-rated health by sex, NHANES 2007–2016.
| Women |
Men |
|||
|---|---|---|---|---|
| Model 1 |
Model 2 |
Model 1 |
Model 2 |
|
| Odds (s.e.) | Odds (s.e.) | Odds (s.e.) | Odds (s.e.) | |
| African American | 0.61 (0.05)* | 0.61 (0.11)* | 0.25 (0.06)* | 0.04 (0.12) |
| Education | ||||
| Non-high school graduate | --- | --- | --- | --- |
| High school graduate/GED equivalent | −0.30 (0.11)* | −0.29 (0.13)* | −0.38 (0.09)* | −0.44 (0.11)* |
| Some college/Associate's degree | −0.53 (0.10)* | −0.53 (0.11)* | −0.59 (0.10)* | −0.63 (0.10)* |
| 4-year college graduate | −0.92 (0.11)* | −0.92 (0.12)* | −0.85 (0.10)* | −0.91 (0.11)* |
| African American × Education | ||||
| Non-high school graduate | --- | --- | ||
| High school graduate/GED equivalent | −0.07 (0.15) | 0.28 (0.16) | ||
| Some college/Associate's degree | 0.03 (0.14) | 0.17 (0.13) | ||
| 4-year college graduate | 0.01 (0.16) | 0.41 (0.17)* | ||
Notes: *p ≤ 0.05. Models adjusted for age, marital status, insurance, chronic conditions, BMI, depressive symptoms, smoking status, alcohol intake and physically inactivity.
Table 3 displays the potential mediation of the association between race and self-rated health through household income, homeownership and investment income among college graduates. Model 1, in which no covariates were included, demonstrates a significant indirect association among women (odds = 0.18, s.e. = 0.04), but also a direct association between race and self-rated health after accounting for income, homeownership and investment income (odds = 0.87, s.e. = 0.11). However, among men, there was no significant indirect association between race and self-rated health through income, homeownership and investment income. In Model 2, after adjusting for age, marital and insurance status, there was a significant indirect (odds = 0.07, s.e. = 0.03) and direct association (odds = 0.51, s.e. = 0.13) of race with self-rated health among men. There were no indirect associations between race and self-rated health through income and wealth indicators among men in Models 3 and 4. After accounting for all covariates in Model 4, a direct association between race and self-rated health among men was observed such that African American men had 0.38 higher log odds of worse self-rated health (odds = 0.38, s.e. = 0.14) indicating that household income and wealth indicators do not account for the race difference in self-rated health among college graduate men. Among women in Model 4, a significant indirect (odds = 0.08, s.e. = 0.03) and direct association (odds = 0.50, s.e. = 0.13) between race and self-rated health was observed suggesting that household income, homeownership and investment income partially mediate the race difference in self-rated health among college graduate women. The decomposition of the mediation suggests that about 64% of this indirect association was due to race differences in investment income (odds = 0.05, s.e. = 0.03).
Table 3.
Association between race, income, wealth indicators and self-rated health by sex among college graduates, NHANES 2007–2016.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|
|---|---|---|---|---|
| Odds (s.e.) | Odds (s.e.) | Odds (s.e.) | Odds (s.e.) | |
| Women | ||||
| Total | 1.05 (0.11)* | 1.01 (0.11)* | 0.67 (0.12)* | 0.57 (0.13)* |
| Direct | 0.87 (0.11)* | 0.86 (0.11)* | 0.56 (0.13)* | 0.50 (0.13)* |
| Indirect | 0.18 (0.04)* | 0.15 (0.04)* | 0.11 (0.03)* | 0.08 (0.03)* |
| Components of difference | ||||
| Income ≥400% FPL | 0.10 (0.03) | 0.06 (0.02) | 0.04 (0.02) | 0.02 (0.01) |
| Homeowner | −0.02 (0.03) | 0.00 (0.01) | 0.00 (0.01) | 0.01 (0.01) |
| Investment income | 0.10 (0.04) | 0.09 (0.03) | 0.07 (0.03) | 0.05 (0.03) |
| Men | ||||
| Total | 0.54 (0.13)* | 0.59 (0.13)* | 0.43 (0.13)* | 0.39 (0.14)* |
| Direct | 0.50 (0.13)* | 0.51 (0.13)* | 0.38 (0.14)* | 0.38 (0.14)* |
| Indirect | 0.04 (0.04) | 0.07 (0.03)* | 0.04 (0.03) | 0.01 (0.03) |
| Components of difference | ||||
| Income ≥400% FPL | 0.04 (0.03) | 0.04 (0.02) | 0.02 (0.02) | 0.01 (0.02) |
| Homeowner | −0.02 (0.02) | 0.00 (0.01) | 0.01 (0.01) | 0.01 (0.01) |
| Investment income | 0.02 (0.03) | 0.03 (0.03) | 0.01 (0.03) | 0.00 (0.03) |
Notes: *p ≤ 0.05. Model 1 includes no covariates. Model 2 adjusts for age, marital status and insurance. Model 3 additionally adjusts for chronic conditions, BMI and depressive symptoms. Model 4 additionally adjusts for smoking status, alcohol intake and physically inactivity.
In Table 4, the total, direct and indirect associations of race with self-rated health through household income and wealth indicators among non-college graduates are displayed by sex. Among women, African Americans had higher odds of reporting worse self-rated health as indicated by a significant direct association (odds = 0.49, s.e. = 0.17) after accounting for household income, homeownership and investment income in Model 1 (which includes no covariates). This association was partially mediated as indicated by a significant indirect association (odds = 0.41, s.e. = 0.17). Among men, there was no direct association between race and self-rated health after accounting for household income and wealth indicators in Model 1. Models 2, 3 and 4 demonstrate similar results among women such that there was a significant indirect and direct association between race and self-rated health in Model 4. This suggests that household income, homeownership and investment income partially mediate the race difference in self-rated health among non-college graduate women. The decomposition of the mediation suggests that this is disproportionately due to race differences in homeownership (odds = 0.05, s.e. = 0.02) and investment income (odds = 0.05, s.e. = 0.02). For men, after adjusting for all covariates, income, homeownership and investment income in Model 4, African Americans had higher odds of reporting worse self-rated health (odds = 0.19, s.e. = 0.09), though this race difference was partially mediated as indicated by a significant indirect association (odds = 0.06, s.e. = 0.02). Decomposition of the mediation suggests that this is mostly due to race differences in household income (odds = 0.04, s.e. = 0.01) and investment income (odds = 0.05, s.e. = 0.02).
Table 4.
Association between race, income, wealth indicators and self-rated health by sex among non-college graduates, NHANES 2007–2016.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|
|---|---|---|---|---|
| Odds (s.e.) | Odds (s.e.) | Odds (s.e.) | Odds (s.e.) | |
| Women | ||||
| Total | 0.77 (0.06)* | 0.77 (0.06)* | 0.68 (0.06)* | 0.64 (0.07)* |
| Direct | 0.49 (0.06)* | 0.52 (0.06)* | 0.50 (0.07)* | 0.51 (0.07)* |
| Indirect | 0.28 (0.03)* | 0.25 (0.02)* | 0.18 (0.02)* | 0.14 (0.02)* |
| Components of difference | ||||
| Income ≥400% FPL | 0.09 (0.01) | 0.06 (0.01) | 0.05 (0.01) | 0.03 (0.01) |
| Homeowner | 0.07 (0.02) | 0.08 (0.02) | 0.06 (0.02) | 0.05 (0.02) |
| Investment income | 0.11 (0.02) | 0.12 (0.02) | 0.08 (0.02) | 0.05 (0.02) |
| Men | ||||
| Total | 0.24 (0.06)* | 0.24 (0.06)* | 0.26 (0.06)* | 0.25 (0.07)* |
| Direct | 0.11 (0.06) | 0.10 (0.07) | 0.17 (0.07)* | 0.19 (0.07)* |
| Indirect | 0.13 (0.02)* | 0.14 (0.02)* | 0.10 (0.02)* | 0.06 (0.02)* |
| Components of difference | ||||
| Income ≥400% FPL | 0.09 (0.01) | 0.06 (0.01) | 0.05 (0.01) | 0.04 (0.01) |
| Homeowner | −0.03 (0.02) | 0.00 (0.02) | −0.02 (0.02) | −0.03 (0.02) |
| Investment income | 0.08 (0.02) | 0.09 (0.02) | 0.07 (0.02) | 0.05 (0.02) |
Notes: *p ≤ 0.05. Model 1 includes no covariates. Model 2 adjusts for age, marital status and insurance. Model 3 additionally adjusts for chronic conditions, BMI and depressive symptoms. Model 4 additionally adjusts for smoking status, alcohol intake and physically inactivity.
Table 5 includes a summary of the indirect associations between race and self-rated health through household income, homeownership, and investment income by education and sex. Among college graduate women, the ratio of total-to-direct associations between race and self-rated health was 1.16 and the mediators accounted for about 13.5% of the total association. There was a small difference between the total and the direct association between race and self-rated health among college graduate men, and race differences in household income, homeownership, and investment income accounted for only 3.6% of the total association. However, among both non-college graduate women and men, there was a larger ratio of total-to-direct associations and mediators accounted for comparably more of the total association between race and self-rated health. Among non-college graduate women, the total-to-direct association ratio was 1.27, and household income, homeownership and investment income accounted for 21.2% of the total association between race and self-rated health. The ratio of total-to-direct associations between race and self-rated health was 1.30 among non-college graduates, and the mediators accounted for 22.9% of the total association between race and self-rated health.
Table 5.
Proportion of total association between race and self-rated health accounted for by income and wealth by education and sex, NHANES 2007–2016.
| Ratio of total to direct association | % of total association accounted for by mediators | |
|---|---|---|
| College graduate | ||
| Women | 1.16 | 13.5 |
| Men | 1.04 | 3.6 |
| Non-college graduate | ||
| Women | 1.27 | 21.2 |
| Men | 1.30 | 22.9 |
Models adjusted for age, marital status, insurance, chronic conditions, BMI, depressive symptoms, smoking status, alcohol intake and physically inactivity.
4. Discussion
The aim of this study was to assess the implications of racial non-equivalence of SES on self-rated health inequities by determining whether income and indicators of wealth (i.e. homeownership and income from investments) mediated race differences in health among African American and white men and women who were college graduates and among those who had not completed a 4-year college degree. The results of the study demonstrate that race differences in income, homeownership and investment income partially mediate race inequities in self-rated health among college graduate women, but not among college graduate men. The indirect associations between race and self-rated health among college graduate women where mostly through racial differences in investment income. Among non-college graduates, there was an indirect association between race and self-rated health, but the majority of this association was through homeownership and investment income in women, but through household income and investment income in men. These results suggest that the racial non-equivalence of SES is an important factor in race differences in self-rated health because racial differences in household income and wealth indicators partially mediated race differences in self-rated health in most education-sex groups. However, racial inequities in self-rated health remained after accounting for household income, homeownership and investment income. This suggests that, in addition to the racial non-equivalence of SES, other factors should be considered with regard to racial inequities in self-rated health.
To our knowledge, no previous studies have empirically sought to examine the role of SES non-equivalence on racial health inequities among college graduates. Several studies have demonstrated racial inequities in self-rated health among college graduates (Farmer & Ferraro, 2005; Holmes & Zajacova, 2014; Liu & Hummer, 2008), and a few studies have examined multiple measures of SES with race and health (Assari, 2018; Boen, 2016). Boen (2016) examined several measures of SES and found that race modifies the effects of 4-year college education, high income and wealth on health (Boen, 2016). A study by Assari (2018) sought to determine whether the interaction between race and education on health was explained by income (Assari, 2018). The study did not find a significant interaction between race and education, but the p-value for the interaction term did decrease after including income in the model (Assari, 2018).
The race difference in self-rated health among women was partially mediated when household income, homeownership and investment income were included in the regression model, however the indirect associations of income and wealth indicators on race differences in health were not observed in college graduate men. Investment income was the largest contributor to the indirect association between race and self-rated health among college graduate women. Income from properties, royalties, estates, trusts or dividends from stocks and mutual funds may give an additional sense of financial security that may be particularly important for African American women who are college graduates given a potentially more precarious financial situation compared to whites (Meschede et al., 2017). For example, African American college graduates are more likely report student loan debt (Jackson & Reynolds, 2013) and higher SES African Americans report having to give gifts to family members (Cross, Nguyen, Chatters, & Taylor, 2018). White college graduates are more likely to receive gifts and other generational wealth which gives more financial stability. The financial security (and potentially social status) that college graduate African American women who have investment income experience may be associated with better self-rated health, and account for a portion of the racial gap. Though the more frequent experiences of discrimination (or interpersonal racism) has been implicated in racial inequities in higher SES African Americans (Colen et al., 2018; Williams, Lawrence, & Davis, 2019; Williams et al., 2016), racial inequities in investment income are also important factors indicating the importance of structural racism in racial inequities in self-rated health. Investment income also contributed substantially to the partial mediation of race differences in self-rated health among non-college graduate men and women. Because racial differences in wealth are observed across educational attainment (Hamilton et al., 2015), racial differences in investment income have implications for inequities in self-rated health among African American college graduates and non-college graduates. Racial inequities in wealth are also indicators of structural racism (Hanks et al., 2018; Yearby, 2018). Although the data on racial inequities in wealth is well established, less is known about whether African American families are able to pass wealth on to their children in terms of monetary gifts, down payments, or other lump sums to offset income shocks through the lifecourse (Killewald & Bryan, 2018). However, Killewald & Bryan (2018) estimated the impact of intergenerational wealth transfers on the racial wealth gap and found that whites accumulate wealth more rapidly through early and middle adulthood. As a result, African Americans fall further behind in amassing wealth with each passing year. Although this study was unable to estimate the impact of actual wealth transfers, future studies should explore the relationship between intergenerational transfers and health outcomes. In the U.S., homeownership is the main driver of wealth accumulation (Shapiro, Meschede, & Osoro, 2013, 2014). Among non-college graduate women, homeownership accounted for a substantial portion of the partial mediation of race differences in self-rated health. However, racial inequity in investment income also indicate structural racism as it can contribute to the racial wealth gap (Shapiro et al., 2013).
Though mass incarceration is often the focus when discussing structural racism and African American men (Bailey et al., 2017; Roberts, 2004), the gender differences in income and wealth within African Americans are dwarfed by the racial inequities in income and wealth that are the result of racist policies and social forces. Among men, the racial inequity in self-rated health was larger among college graduates compared to non-college graduates. However, accounting for the racial differences in household income and wealth that indicate structural racism had no impact on the racial inequities in self-rated health among college graduates. These differences in household income and wealth only partially mediated the race inequities in self-rated health among non-college graduates. The role of stress, discrimination, masculinity and role strain have been implicated in African American men's health (Gilbert et al., 2016; Griffith, Gunter, & Allen, 2011; Hudson et al., 2012). Specifically, studies show that discrimination is associated with worse self-rated health among African Americans, and this relationship is mediated by stress and depression (Cuevas et al., 2013). Previous studies have also suggested that health pessimism is an important factor to self-rated health among African Americans (Boardman, 2004; Spencer et al., 2009), and this may be particularly salient to African American men with a similar SES profile as white counterparts. The concept of health pessimism among African American men aligns with qualitative work by McMullen and Luborsky which finds that resilience is a concept that is important to self-appraisal of health in elderly African Americans, but also highlights the role of comparison with others and the inability to have “perfect” health. This approach of rating one's health could contribute to lower self-rated health among college graduate African American men in particular. Overall, these other factors may contribute to racial inequities in self-rated health in college graduate men.
Because several psychosocial factors and experiences of discrimination may contribute to racial inequities in self-rated health, the concept of cultural racism may be important here. Definitions of cultural racism note that the United States is characterized by “cultural processes, girded by racial inequities in power, that result in a racialized social environment in which Black (and other non-White ethno-racial) group members are routinely stigmatized” (Hicken, Lee, & Hing, 2018). This goes beyond overt racial discrimination to describe an environment that can have an amalgam of racialized factors that contribute to the larger racial inequities in health among college graduate African American men. Structural racism is culturally reinforced (Bailey et al., 2017), so cultural racism links to racial inequities in SES facilitated by structural racism.
Other studies have identified additional domains of SES that may also affect health outcomes. Racial segregation and social environment could play an important role in racial non-equivalence of SES and racial inequities in self-rated health (Do, Frank, & Iceland, 2017). Scholars have examined racial segregation and racial inequities in neighborhood environment as an indicator of structural racism (Bailey et al., 2017; Gee & Ford, 2011; Riley, 2018; Williams et al., 2019). Previous studies have demonstrated that racial inequities in self-rated health are eliminated among African Americans and whites living in a low-income, urban social environment (Bell, Thorpe, & LaVeist, 2018b). Meltzer and Schuetz note that minority neighborhoods have limited access to retail stores and household services, which may result in higher priced goods and services (Meltzer & Schuetz, 2012). They also find, for example, that in New York City, Black neighborhoods have fewer options for buying food, services, and other retail goods (Meltzer & Schuetz, 2012). Although limited access to retail goods is typically considered only in relation to food options, this research suggests African Americans may have to pay more for everyday goods and services, thereby reducing their buying power overall. This aspect of SES is frequently overlooked and should be considered in future studies.
The results of this study have important implications. First, the study demonstrates that the racial non-equivalence of SES experienced by African American college graduate and non-college graduate women, as well as non-college graduate men, is important to racial inequities in self-rated health. College education is often thought of as an equalizer and a mode of social mobility in the U.S., but does not have the same SES and health benefits for African Americans (Holmes & Zajacova, 2014; Meschede et al., 2017). Though African American college graduates may have higher incomes and wealth than less educated African Americans, college graduate African Americans still have lower incomes and less wealth than their white counterparts (Meschede et al., 2017; Shapiro et al., 2014; Sullivan et al., 2015; Williams et al., 2016). This study demonstrates that this is associated with worse self-rated health among college graduate African American men compared to college graduate white men, but that differences in household income, homeownership and investment income partially account for race inequities in self-rated health among college graduate women and non-college graduate women and men. Lower incomes and less wealth among African Americans are due to historical and contemporary structural racism through less intergenerational wealth, discriminatory hiring practices, and student debt (Brown, 2016; Hanks et al., 2018; Jackson & Reynolds, 2013; Killewald & Bryan, 2018; Meschede et al., 2017; Shapiro et al., 2014). These factors have health implications including the cost burden of racial inequities in health (Thorpe, Richard, Bowie, LaVeist, & Gaskin, 2013). The results suggest that policy and other efforts to increase investment income could contribute to addressing the health effects of racial non-equivalence of SES at all education levels.
Another implication is that the diminished returns of college education on self-rated health were only observed among men. There was no difference in the magnitude of racial disparities in self-rated health across educational attainment among women. It is possible that the factors that contribute to worse self-rated health among African American women (e.g. discrimination, segregation, other psychosocial factors) may not differ by college graduate status. Previous studies had not interrogated the role of sex in the Diminishing Returns Hypothesis (Assari, 2018; Colen et al., 2018; Farmer & Ferraro, 2005).
This study is strengthened by the use of nationally representative data that combine multiple years of NHANES data to obtain a sufficient number of college graduate African Americans. However, there are some limitations. The analyses could not establish causality. Racial/ethnic groups other than African Americans and whites were not included, so the potential mediation of household income, homeownership and investment income on the effects of race/ethnicity on health are not fully understood. Lastly, homeownership and investment income may be considered proxy measures of wealth. An actual measure of wealth (i.e. assets minus debts) was not included in this dataset.
This study sought to evaluate the mediation of racial health inequities among African Americans and whites by education and sex through the racial non-equivalence of SES. The results demonstrate that household income, homeownership and investment income partially mediate the race difference in self-rated health among college graduate women, and women and men who are non-college graduates. The results of this study contribute to the literature by finding that the diminished returns of education on self-rated health among African Americans is observed among men and not women. The study also contributes to the literature by finding that the racial non-equivalence of SES partially mediates racial inequities in self-rated health. The study results point to other factors that could explain racial inequities in self-rated health. Future studies should additionally interrogate discrimination, psychosocial factors and racial segregation along with racial non-equivalence of SES on race inequities in self-rated health. Policies and social justice efforts to reduce racial inequities in investment income, in particular, can address racial inequities in self-rated health.
Financial disclosures
Roland Thorpe is supported by the National Institute on Minority Health and Health Disparities (U54MD000214) and the National Institute on Aging (K02AG059140 and R01AG054363).
Ethics approval
Ethics approval for the study titled “Racial Non-equivalence of Socioeconomic Status and Health among African Americans and Whites” is not required as it does not contain data from human subjects.
CRediT authorship contribution statement
Caryn N. Bell: Conceptualization, Data curation, Formal analysis, Writing - original draft, Writing - review & editing. Tina K. Sacks: Writing - original draft, Writing - review & editing. Courtney S. Thomas Tobin: Writing - original draft, Writing - review & editing. Roland J. Thorpe: Funding acquisition, Writing - original draft, Writing - review & editing.
Declaration of competing interest
Caryn Bell, Tina Sacks, Courtney Thomas Tobin, and Roland Thorpe, Jr. have no conflicts of interest.
Acknowledgement
The authors would like to thank Dr. Michael Wagner for his expertise and help in conducting statistical analyses.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100561.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Adler N.E., Newman K. Socioeconomic disparities in health: Pathways and policies. Health Affairs. 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- Adler N.E., Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Biology of Disadvantage: Socioeconomic Status and Health. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- Assari S. Blacks' diminished return of education attainment on subjective health; mediating effect of income. Brain Sciences. 2018;8 doi: 10.3390/brainsci8090176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Z.D., Krieger N., Agenor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: Evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Beck A.N., Finch B.K., Lin S.F., Hummer R.A., Masters R.K. Racial disparities in self-rated health: Trends, explanatory factors, and the changing role of socio-demographics. Social Science & Medicine. 2014;104:163–177. doi: 10.1016/j.socscimed.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belgrave F.Z., Abrams J.A. Reducing disparities and achieving equity in african American women's health. American Psychologist. 2016;71:723–733. doi: 10.1037/amp0000081. [DOI] [PubMed] [Google Scholar]
- Bell C.N., Thorpe R.J., Bowie J.V., LaVeist T.A. Race disparities in cardiovascular disease risk factors within socioeconomic status strata. Annals of Epidemiology. 2018;28:147–152. doi: 10.1016/j.annepidem.2017.12.007. [DOI] [PubMed] [Google Scholar]
- Bell C.N., Thorpe R.J., LaVeist T.A. The role of social context in racial disparities in self-rated health. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2018;95:13–20. doi: 10.1007/s11524-017-0211-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benyamini Y., Blumstein T., Lusky A., Modan B. Gender differences in the self-rated health-mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? The Gerontologist. 2003;43:396–405. doi: 10.1093/geront/43.3.396. [DOI] [PubMed] [Google Scholar]
- Benyamini Y., Leventhal E.A., Leventhal H. Elderly people's ratings of the importance of health-related factors to their self-assessments of health. Social Science & Medicine. 2003;56:1661–1667. doi: 10.1016/s0277-9536(02)00175-2. [DOI] [PubMed] [Google Scholar]
- Boardman J.D. Health pessimism among black and white adults: The role of interpersonal and institutional maltreatment. Social Science & Medicine. 2004;59:2523–2533. doi: 10.1016/j.socscimed.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Boen C. The role of socioeconomic factors in Black-White health inequities across the life course: Point-in-time measures, long-term exposures, and differential health returns. Social Science & Medicine. 2016;170:63–76. doi: 10.1016/j.socscimed.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P.A., Cubbin C., Egerter S., Chideya S., Marchi K.S., Metzler M. Socioeconomic status in health research: One size does not fit all. Journal of the American Medical Association. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Braveman P.A., Cubbin C., Egerter S., Williams D.R., Pamuk E. Socioeconomic disparities in health in the United States: What the patterns tell us. American Journal of Public Health. 2010;100:S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen R., Karlson K.B., Holm A. Total, direct, and indirect effects in logit and probit models. Sociological Methods & Research. 2013;42:164–191. [Google Scholar]
- Brown T.H. Diverging fortunes: Racial/ethnic inequality in wealth trajectories in middle and late life. Race and Social Problems. 2016;8:29–41. [Google Scholar]
- Brown T.H., Richardson L.J., Hargrove T.W., Thomas C.S. Using multiple-hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. Journal of Health and Social Behavior. 2016;57:200–222. doi: 10.1177/0022146516645165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buis M.L. Direct and indirect effects in a logit model. STATA Journal. 2010;10:11–29. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Vol. 62. Morbidity & Mortality Weekly Report; 2013. (CDC health disparities and inequalities report--United States, 2013). [Google Scholar]
- Chandola T., Jenkinson C. Validating self-rated health in different ethnic groups. Ethnicity and Health. 2000;5:151–159. doi: 10.1080/713667451. [DOI] [PubMed] [Google Scholar]
- Colen C.G., Ramey D.M., Cooksey E.C., Williams D.R. Racial disparities in health among nonpoor African Americans and Hispanics: The role of acute and chronic discrimination. Social Science & Medicine. 2018;199:167–180. doi: 10.1016/j.socscimed.2017.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross C.J., Nguyen A.W., Chatters L.M., Taylor R.J. Instrumental social support exchanges in african American extended families. Journal of Family Issues. 2018;39:3535–3563. doi: 10.1177/0192513X18783805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuevas A.G., Reitzel L.R., Cao Y.M., Nguyen N., Wetter D.W., Adams C.E. Mediators of discrimination and self-rated health among african Americans. American Journal of Health Behavior. 2013;37:745–754. doi: 10.5993/AJHB.37.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J.L., Jackson P.B. Race, gender, and SES disparities in self-assessed health, 1974-2004. Research on Aging. 2008;30:137–167. [Google Scholar]
- Daw J. Contribution of four comorbid conditions to racial/ethnic disparities in mortality risk. American Journal of Preventive Medicine. 2017;52:S95–S102. doi: 10.1016/j.amepre.2016.07.036. [DOI] [PubMed] [Google Scholar]
- Do D.P., Frank R., Finch B.K. Does SES explain more of the black/white health gap than we thought? Revisiting our approach toward understanding racial disparities in health. Social Science & Medicine. 2012;74:1385–1393. doi: 10.1016/j.socscimed.2011.12.048. [DOI] [PubMed] [Google Scholar]
- Do D.P., Frank R., Iceland J. Black-white metropolitan segregation and self-rated health: Investigating the role of neighborhood poverty. Social Science & Medicine. 2017;187:85–92. doi: 10.1016/j.socscimed.2017.06.010. [DOI] [PubMed] [Google Scholar]
- Erikson R., Goldthorpe J.H., Jackson M., Yaish M., Cox D.R. On class differentials in educational attainment. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:9730–9733. doi: 10.1073/pnas.0502433102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer M.M., Ferraro K.F. Are racial disparities in health conditional on socioeconomic status? Social Science & Medicine. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Ferraro K.F., Kelley-Moore J.A. Self-rated health and mortality among black and white adults: Examining the dynamic evaluation thesis. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2001;56:S195–S205. doi: 10.1093/geronb/56.4.s195. [DOI] [PubMed] [Google Scholar]
- Finnigan R. Racial and ethnic stratification in the relationship between homeownership and self-rated health. Social Science & Medicine. 2014;115:72–81. doi: 10.1016/j.socscimed.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Ford C.L. Structural racism and health inequities: Old issues, new directions. Du Bois Review-Social Science Research on Race. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert K.L., Ray R., Siddiqi A., Shetty S., Baker E.A., Elder K. Visible and invisible trends in black men's health: Pitfalls and promises for addressing racial, ethnic, and gender inequities in health. Annual Review of Public Health. 2016;37(37):295–311. doi: 10.1146/annurev-publhealth-032315-021556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D.M., Gunter K., Allen J.O. Male gender role strain as a barrier to african American men's physical activity. Health Education & Behavior. 2011;38:482–491. doi: 10.1177/1090198110383660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A., Kaufman J.S., Rose K.M., Siddiqi A., Thomas J.C. Long-term effects of wealth on mortality and self-rated health status. American Journal of Epidemiology. 2011;173:192–200. doi: 10.1093/aje/kwq348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton D., Darity J., William, Price A.E., Sridharan V., Tippett R. Insight Center for Community Economic Development; Oakland, CA: 2015. Umbrellas don't make it rain: Why studying and working hard isn't enough for black Americans. [Google Scholar]
- Hanks A., Solomon D., Weller C.E. Center for American Progress; Washington, DC: 2018. Systematic inequality: How America's structural racism helped create the black-white wealth gap. [Google Scholar]
- Hargrove T.W., Brown T.H. A life course approach to inequality: Examining racial/ethnic differences in the relationship between early life socioeconomic conditions and adult health among men. Ethnicity & Disease. 2015;25:313–320. doi: 10.18865/ed.25.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken M.T., Lee H., Hing A.K. The weight of racism: Vigilance and racial inequalities in weight-related measures. Social Science & Medicine. 2018;199:157–166. doi: 10.1016/j.socscimed.2017.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes C.J., Zajacova A. Education as "the Great Equalizer": Health benefits for black and white adults. Social Science Quarterly. 2014;95:1064–1085. [Google Scholar]
- Hudson D.L., Bullard K.M., Neighbors H.W., Geronimus A.T., Yang J., Jackson J.S. Are benefits conferred with greater socioeconomic position undermined by racial discrimination among African American men? Journal of Men's Health. 2012;9:127–136. doi: 10.1016/j.jomh.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson D.L., Puterrnan E., Bibbins-Domingo K., Matthews K.A., Adler N.E. Race, life course socioeconomic position, racial discrimination, depressive symptoms and self-rated health. Social Science & Medicine. 2013;97:7–14. doi: 10.1016/j.socscimed.2013.07.031. [DOI] [PubMed] [Google Scholar]
- Idler E.L., Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler E.L., Hudson S.V., Leventhal H. The meanings of self-ratings of health: A qualitative and quantitative approach. Research on Aging. 1999;21:458–476. [Google Scholar]
- Jackson B.A., Reynolds J.R. The price of opportunity: Race, student loan debt, and college achievement. Sociological Inquiry. 2013;83:335–368. [Google Scholar]
- Karlson K.B., Holm A., Breen R. Comparing regression coefficients between same-sample nested models using logit and probit: A new method. Sociological Methodology. 2012;42(42):286–313. 2012. [Google Scholar]
- Kaufman J.S. Epidemiologic analysis of racial/ethnic disparities: Some fundamental issues and a cautionary example. Social Science & Medicine. 2008;66:1659–1669. doi: 10.1016/j.socscimed.2007.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J.S., Cooper R.S., McGee D.L. Socioeconomic status and health in blacks and whites: The problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. [PubMed] [Google Scholar]
- Killewald A., Bryan B. Falling behind: The role of inter- and intragenerational processes in widening racial and ethnic wealth gaps through early and middle adulthood. Social Forces. 2018;97:705–740. [Google Scholar]
- Kimbro R.T., Bzostek S., Goldman N., Rodríguez G. Race, ethnicity, and the education gradient in health. Health Affairs. 2008;27:361–372. doi: 10.1377/hlthaff.27.2.361. [DOI] [PubMed] [Google Scholar]
- Kohler U., Karlson K.B., Holm A. Comparing coefficients of nested nonlinear probability models. STATA Journal. 2011;11:420–438. [Google Scholar]
- Krieger N., Williams D.R., Moss N.E. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annual Review of Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Landrine H., Corral I. Advancing research on racial–ethnic health disparities: I mproving measurement equivalence in studies with diverse samples. Frontiers in Public Health. 2014;2:1–22. doi: 10.3389/fpubh.2014.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist T.A. Disentangling race and socioeconomic status: A key to understanding health inequalities. Journal of Urban Health. 2005;82:iii26–iii34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Liu H., Hummer R.A. Are educational differences in US self-rated health increasing?: An examination by gender and race. Social Science & Medicine. 2008;67:1898–1906. doi: 10.1016/j.socscimed.2008.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMullen C.K., Luborsky M.R. Self-rated health appraisal as cultural and identity process: African American elders' health and evaluative rationales. The Gerontologist. 2006;46:431–438. doi: 10.1093/geront/46.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer R., Schuetz J. Bodegas or bagel shops? Neighborhood differences in retail and household services. Economic Development Quarterly. 2012;26:73–94. [Google Scholar]
- Meschede T., Taylor J., Mann A., Shapiro T. "Family achievements?": How a college degree accumulates wealth for whites and not for blacks. Federal Reserve Bank of St. Louis Review. 2017;99:121–137. [Google Scholar]
- Nuru-Jeter A.M., Michaels E.K., Thomas M.D., Reeves A.N., Thorpe R.J. Relative roles of race versus socioeconomic position in studies of health inequalities: A matter of interpretation. Annual Review of Public Health. 2018;39 doi: 10.1146/annurev-publhealth-040617-014230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz S.E., Zimmerman F.J. Race/ethnicity and the relationship between homeownership and health. American Journal of Public Health. 2013;103:e122–e129. doi: 10.2105/AJPH.2012.300944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson J. Can't buy me whiteness: New lessons from the Titanic on race, ethnicity, and health. Du Bois Review. 2008;5:27–47. [Google Scholar]
- Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annual Review of Sociology. 2015;41(41):311–330. [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010;51:S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Pollack C.E., Chideya S., Cubbin C., Dekker M., Braveman P. Should health studies measure wealth? American Journal of Preventive Medicine. 2007;33:250–264. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]
- Pollack C.E., Cubbin C., Sania A., Hayward M., Vallone D., Flaherty B. Do wealth disparities contribute to health disparities within racial/ethnic groups? Journal of Epidemiology & Community Health. 2013;67(5):439–445. doi: 10.1136/jech-2012-200999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon S.F., Fox L., Townsend J. Neighborhood income composition by household race and income, 1990-2009. The Annals of the American Academy of Political and Social Science. 2015;660:78–97. [Google Scholar]
- Riley A.R. Neighborhood disadvantage, residential segregation, and beyond-lessons for studying structural racismand health. Journal of Racial and Ethnic Health Disparities. 2018;5:357–365. doi: 10.1007/s40615-017-0378-5. [DOI] [PubMed] [Google Scholar]
- Roberts D.E. The social and moral cost of mass incarceration in African American communities. Stanford Law Review. 2004;56:1271–1305. [Google Scholar]
- Rothstein R. W.W. Norton & Company, Inc; New York, NY: 2017. The color of law: A forgotten history of how our government segregated America. [Google Scholar]
- Santos-Lozada A.R., Daw J. The contribution of three dimensions of allostatic load to racial/ethnic disparities in poor/fair self-rated health. Ssm-Population Health. 2018;4:55–65. doi: 10.1016/j.ssmph.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker J., Bacak V. The increasing predictive validity of self-rated health. PloS One. 2014;9 doi: 10.1371/journal.pone.0084933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro T., Meschede T., Osoro S. Institute on Assets and Social Policy; 2013. The roots of the widening racial wealth gap: Explaining the black-white economic divide. [Google Scholar]
- Shapiro T., Meschede T., Osoro S. Assets perspective: The rise of asset building and its impact on social policy. 2014. The widening racial wealth gap: WHY wealth IS not color blind; pp. 99–122. [Google Scholar]
- Shavers V.L. Measurement of socioeconomic status in health disparities research. Journal of the National Medical Association. 2007;99:1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Spencer S.M., Schulz R., Rooks R.N., Albert S.M., Thorpe R.J. Racial differences in self-rated health at similar levels of physical functioning: An examination of health pessimism in the Health, Aging and Body Composition Study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64:87–94. doi: 10.1093/geronb/gbn007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan L., Meschede T., Dietrich L., Shapiro T. Demos; New York, NY: 2015. The racial wealth gap: Why policy matters. [Google Scholar]
- Thorpe R.J., Richard P., Bowie J.V., LaVeist T.A., Gaskin D.J. Economic burden of men's health disparities in the United States. International Journal of Men's Health. 2013;12:195–212. [Google Scholar]
- Turner R.J., Brown T.N., Hale W.B. Race, socioeconomic position, and physical health: A descriptive analysis. Journal of Health and Social Behavior. 2017;58:23–36. doi: 10.1177/0022146516687008. [DOI] [PubMed] [Google Scholar]
- Turner R.J., Thomas C.S., Brown T.H. Childhood adversity and adult health: Evaluating intervening mechanisms. Social Science & Medicine. 2016;156:114–124. doi: 10.1016/j.socscimed.2016.02.026. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Jackson P.B. Social sources of racial disparities in health. Health Affairs. 2005;24:325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40(40):105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A., Leavell J., Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Sciences. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Priest N., Anderson N.B. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychology. 2016;35:407–411. doi: 10.1037/hea0000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson K.B., Thorpe R.J., Jr., LaVeist T.A. Dollar for Dollar: Racial and ethnic inequalities in health and health-related outcomes among persons with very high income. Preventive Medicine. 2017;96:149–153. doi: 10.1016/j.ypmed.2016.08.038. [DOI] [PubMed] [Google Scholar]
- Woo H., Zajacova A. Predictive strength of self-rated health for mortality risk among older adults in the United States: Does it differ by race and ethnicity? Research on Aging. 2017;39:879–905. doi: 10.1177/0164027516637410. [DOI] [PubMed] [Google Scholar]
- Yao L., Robert S.A. The contributions of race, individual socioeconomic status, and neighborhood socioeconomic context on the self-rated health trajectories and mortality of older adults. Research on Aging. 2008;30:251–273. [Google Scholar]
- Yearby R. Racial disparities in health status and access to healthcare: The continuation of inequality in the United States due to structural racism. The American Journal of Economics and Sociology. 2018;77:1113–1152. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.