Abstract
Objective
The current article is aimed at identifying the best practice for counseling around depression in community and outpatient pharmacies, resulting in a draft guideline, proposing key steps and an algorithm for integration of community pharmacists into care for patients with depression.
Methods
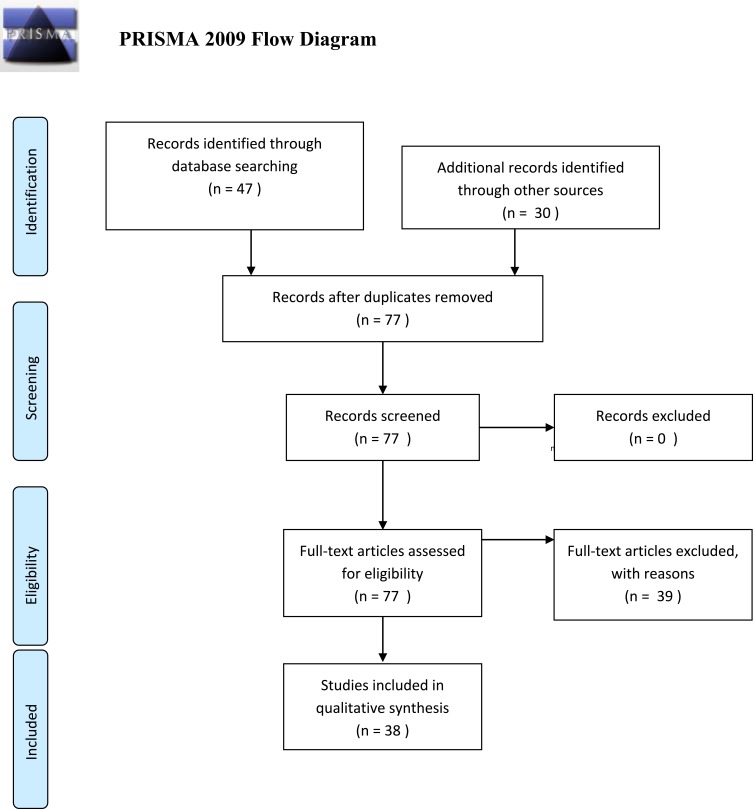
A literature review was performed followed by a detailed analysis, for the purpose of creation a short draft document used as a basis for creation of a guideline for pharmaceutical care for patients with depression. The technological scheme PRISMA flow diagram was applied. The paper is based on current knowledge, taking into consideration already published articles, guidelines, and recommendations about pharmaceutical care for patients with depression, giving a basis for further studies.
Results
This paper includes two main sections: 1) depression – a short description of the main symptoms, risk factors and pharmacotherapy guidelines available in Bulgaria important for the purposes of ensuring qualitative community-based pharmaceutical care; and 2) the pharmacists’ role in providing high-quality care – the main aspects of pharmaceutical care for patients with depression with specific examples.
Conclusion
The involvement of pharmacists in supporting depressive patients is crucial taking into account the specific characteristics of the pharmacological treatment: delayed onset of clinical results, risks in case of sudden pharmacotherapy abruption without physician consultation, multiple adverse drug reactions and drug–drug, drug–food and drug–alcohol interactions, etc. The current article could also be used as an initial document for creating a methodological guideline for providing pharmaceutical care services for patients with depression.
Keywords: depression, drug-related problems, pharmaceutical care, pharmacists, guideline
Background
Pharmaceutical care is a responsible provision of drug therapy for the purposes of achieving definite outcomes and improvement of patient’s quality-of-life.1 The main responsibilities of the pharmacists are defined as a result of long-term studies: 1) to ensure that all medications are appropriate, effective, and safe for a particular patient, and 2) to identify, solve, and prevent various drug-related problems (DRPs).2 In 2013 a working group formed by investigator members of the Pharmaceutical Care Network Europe (PCNE) preformulated the definition so as to respond to the current expectations and views: “Pharmaceutical Care is the pharmacist’s contribution to the care of individuals in order to optimize medicines use and improve health outcomes”.3
Depression is a common psychiatric illness, which is associated with several specific symptoms such as depressed mood, markedly diminished interest or pleasure in activities, psychomotor retardation, weight loss or weight gain, fatigue or loss of energy, feelings of worthlessness or guilt, recurrent thoughts of death, or recurrent suicidal ideation, etc.4 Being chronic in nature and affecting people of working age, depression leads to great economic and financial burden, which is also evaluated in a number of studies.5,6,7 Moreover, the World Health Organization (WHO) reports that depression will be the second leading cause of disability in the world by 2020.8 Non-adherence to antidepressants, which is defined as being over 75% after 6 months, could lead to a lack of effect, to higher costs and significant burden for the patient, family, and society.9
Pharmacists may play a significant role in the primary care for patients suffering from depression, giving advice, recommendations, counseling about medicines, following up the patients for drug-related problems, and assessing patients’ adherence on the basis of their skills and knowledge about the medicines.10 The community pharmacist is recognized as a crucial member of the multidisciplinary primary care team for all patients with chronic and acute diseases.11 Pharmacist-provided patient care services are proved to bring significant benefits on patient health outcomes.12 Gomes et al13 evaluated the effectiveness of pharmaceutical care services and their influence on the patients’ quality-of-life. As a result of ensuring various interventions for increasing the level of compliance and educational programs, the depressive symptoms were reduced and the quality-of-life was improved (P<0.05). Another study among patients with depressive disorder demonstrated quality-of-life improvement, improved adherence, and effectiveness of the therapy as a result of pharmaceutical care services.14 In comparison with the standard care, pharmaceutical care provides a reduction in the number of hospitalizations and emergency visits not only in patients with depression, but also in patients with bipolar disorder.15 Rubio-Valera et al9 found a probability of 0.71–0.75 for community pharmacy intervention vs usual care in depressed patients initiating treatment in terms of improved adherence level and Quality Adjusted Life Years (QALYs) to be cost-effective.
Searching in the literature we identified only review papers, a pharmacist guided protocol for improved of monitoring patients treated with antidepressants, and physician-focused clinical practice guidelines or some local implemented instructions regarding pharmaceutical services for this group of patients.16,17,18,19 In 2018, the Royal Pharmaceutical Society highlighted the need for implementing the pharmacists’ potential for supporting people with mental disorders without presenting any specific and concrete guidance.20 Moreover, the role of the pharmacists and their unique skills in medication management, provision of drug information, and counseling patients with mental diseases is clearly identified in a recent study by Rubio-Valera et al.21 Therefore, pharmacists all around the world need a detailed guideline providing algorithms and instructions on how and when pharmaceutical care should be provided to patients with depressive disorders.
The current article aimed at identifying the best practice for counseling around depression in community and outpatient pharmacies, resulting in a draft guideline, proposing key steps and algorithms. The article gives a short description of the main symptoms, risk factors, and pharmacotherapy guidelines important for the purposes of ensuring qualitative community-based pharmaceutical care for patients with depression. It also highlights the pharmacists’ role in providing a high-quality care presenting the main aspects of pharmaceutical care for patients with depression presenting the most common identifiable drug-related problems among the observed group of patients.
Methods
A literature review of the published literature regarding pharmaceutical care, depression treatment, and role of the pharmacist in the care for patients with depressive disorder was performed. A detailed analysis for the purpose of creating a short guideline for pharmaceutical care for patients with depression was made. The discussion about the guideline’s structure and further validation of the drafted guideline are planned to be the next steps. The paper is based on the current knowledge taking into consideration already published articles, guidelines, and recommendations about pharmaceutical care for patients with depression.
A search was conducted in the Internet based scientific data base PubMed as well as in other sources, such as paper-based journals and scientific books. The key words used were depression, pharmaceutical care, pharmacists, and pharmacy services. A particular consistency was followed:
Defining the study question: What are the best practices for counseling around depression in community and outpatient pharmacies?
Input the key words in the database PubMed Clinical Queries – “depression” AND “pharmaceutical care” OR “pharmacy services “AND “pharmacists” AND “community pharmacy” OR “outpatient pharmacy”.
Other relevant sources of information were also reviewed, and suitable studies were selected.
The search for the available studies in PubMed was initiated and the details shown by the system were subdivided into three categories: clinical studies, systematic reviews, and medical genetics.
The studies were analyzed following the PRISMA flow diagram. The duplicated studies were withdrawn from the analysis. Studies were selected only if they met the following inclusion criteria: 1) The studies were free full text systematic reviews, government documents, reports, comments, classical articles, or guidelines; 2) The objects in the studies were patients with depression (no limitation regarding the age); 3) Studies were in English; and 4) Studies including specific drug-related problems and ways for overcoming and preventing them. The exclusion criteria were: 1) duplicated studies; 2) language different from English; 3) studies focusing mainly on efficacy of specific therapies for depression; and 4) studies which covered patients who did not suffer from depression but from other mental disorders;
The technological scheme PRISMA Flow Diagram was applied.
Results and Discussion
There were 77 papers relevant to our research question: 47 in PubMed and 30 from other sources (books, paper-based reports, guidelines, and articles). The study selection process is presented in Figure 1. No potentially relevant studies after duplicates were removed. After reviewing the titles, abstracts, and the full publications, 39 of the articles meeting exclusion criteria were excluded and only 38 were summarized.
Figure 1.
PRISMA flow diagram. Adapted from: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6(6): e1000097. doi:10.1371/journal.pmed1000097.
The characteristics of the included studies are initially analyzed, summarized, and combined for the purposes of presenting initial ideas for creating a guideline. They are presented in the current part of the article as we are planning to present a discussed and validated version of the guideline in a further more detailed paper.
Depression – Symptoms, Epidemiology, and Treatment
Depression is a common psychiatric disorder affecting more than 300 million people worldwide. It causes significant distress, limitations in personal and social functioning, and worsens the quality-of-life of those affected.22,23 The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) outlines specific criteria for the diagnosis of depression. Some of the most specific symptoms are depressed mood, loss of interest or pleasure, significant weight loss or weight gain, a slowing down of thought and a reduction of physical movement, fatigue or loss of energy, feelings of worthlessness or excessive or inappropriate guilt, diminished ability to think or concentrate, recurrent thoughts of death or suicidal thoughts.24,25 Among all mental disorders, depression is related to the highest risk of suicide, followed by schizophrenia and alcohol abuse.26 The main causes for depression are genetic factors, personal predisposition, concomitant diseases, family history, huge life changes (negative or positive events), or social determinants (stress, isolation, loneliness, unemployment).27 Depression might be in mild, moderate, or severe form, which is defined after complex clinical evaluation based on the number, type, and severity of the symptoms. According to the monoamine hypothesis, depression is characterized by diminished activity of monoamine neurotransmitters (predominantly norepinephrine, dopamine, and serotonin) in the brain. The amygdala, the thalamus, the hippocampus, and the prefrontal cortex play significant roles in depression, where the low levels of monoamines cause the symptoms of dysthymia, anhedonia, lack of motivation, lack of activity, fatigue, insomnia, and cognitive effects. Depression is associated with chronic stress, which overactivates the hypothalamic–pituitary–adrenal axis, causing elevated levels of cortisol, induction of fight-or-flight response, and overactivation of the autonomous nervous system with somatic symptoms (tachycardia, palpitation, shortness of breath, and diaphoresis by overactivation of the sympathetic nervous system and gastrointestinal symptoms by overactivation of the parasympathetic nervous system). Chronic stress also changes the immune response and causes reduced neuroplasticity. Early losses and trauma experiences significantly increase the risk of depression later in life through their effect on the limbic system.28,29
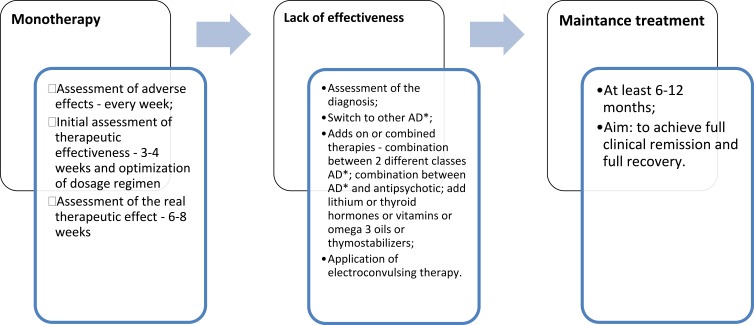
Pharmacotherapeutic guidelines for treatment of psychiatric disorders present the main principles of depression treatment on the basis of severity, age, and concomitant diseases (Figure 2). The goal of treatment is achieving remission and full recovery of the patient’s social functioning.22
Figure 2.
Pharmacotherapy principles for depression.
Abbreviation: АD, antidepressants.
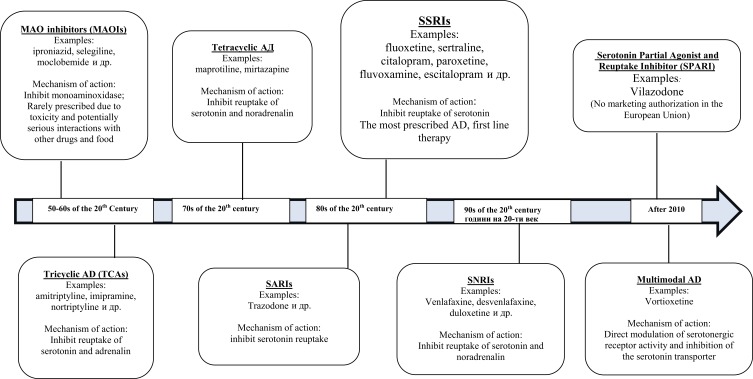
The first antidepressant (AD) was discovered in the 1950s, and several pharmacological groups are available now: monoaminoxidase inhibitors, selective inhibitors of serotonin reuptake (SSRIs) and/or noradrenaline (SNRIs), tricyclic and tetracyclic antidepressants, SPARI, and multimodal AD (Figure 3).30,31 The first line therapies are: SSRIs, SNRIs, and serotonin antagonist and reuptake inhibitors (SARIs), noradrenergic, and specific serotonergic antidepressant (NaSSA (mirtazapine)). Tricyclic AD, MAOIs, and others AD (tianeptine, agomelatine (melatonergic)) as well as some antipsychotics are indicated as second line therapy.32
Figure 3.
Main pharmacological groups antidepressants.
Pharmaceutical Care Aspects for Patients with Depression
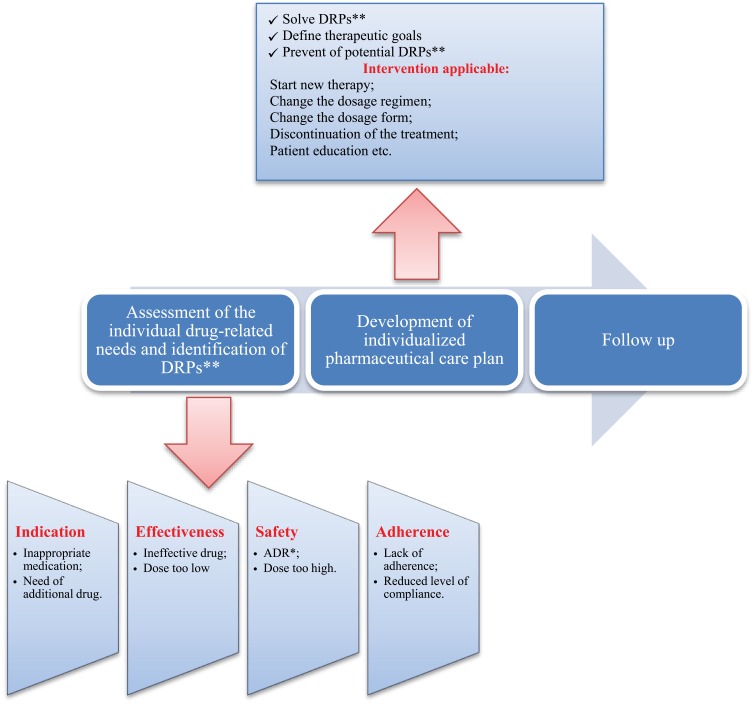
The pharmacist’s obligations in the process of providing pharmaceutical care are: (1) collection of specific information for the patient’s demographic data, history of disease, medication therapy (current therapy, dose, therapeutic regimen, allergies, immunizations, previous drug therapy), current complaints; (2) analyzing the collected information so as to identify drug-related problems, to assess whether all medications are effective and safe for the patient as well as patient’s adherence and compliance.33,34 Follow-up was aimed at defining the therapy effectiveness and long-term safety, assessing clinical results, defining the level of achieving the goals, level of adherence, and reassessing of new potential or actual DRPs (Figure 4).35
Figure 4.
Steps and key element of pharmaceutical care.
Abbreviations: ADR, adverse drug reaction; DRP, drug-related problem.
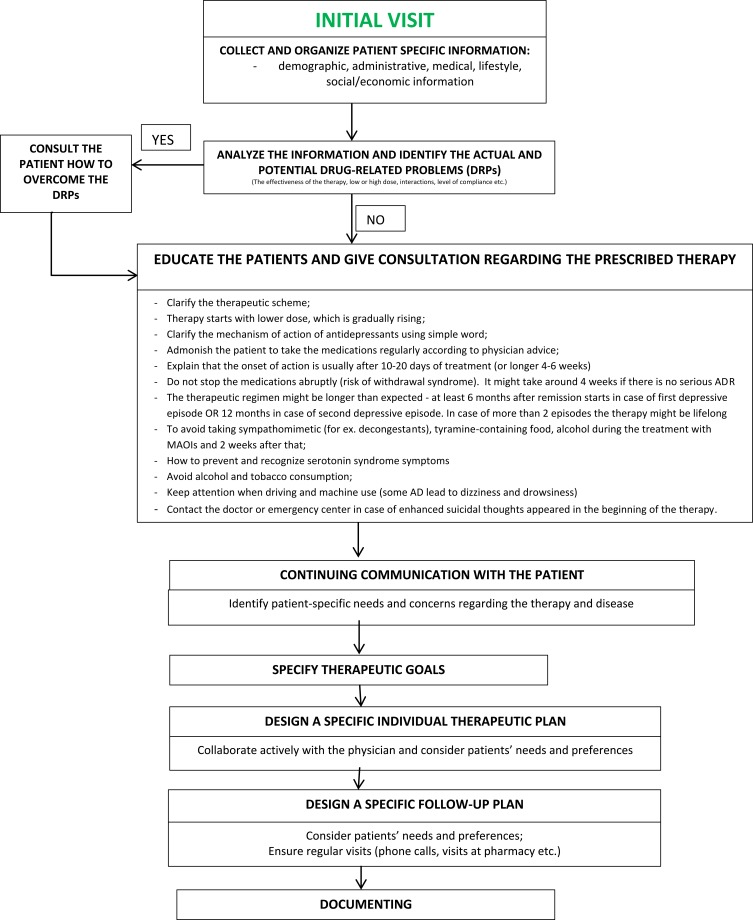
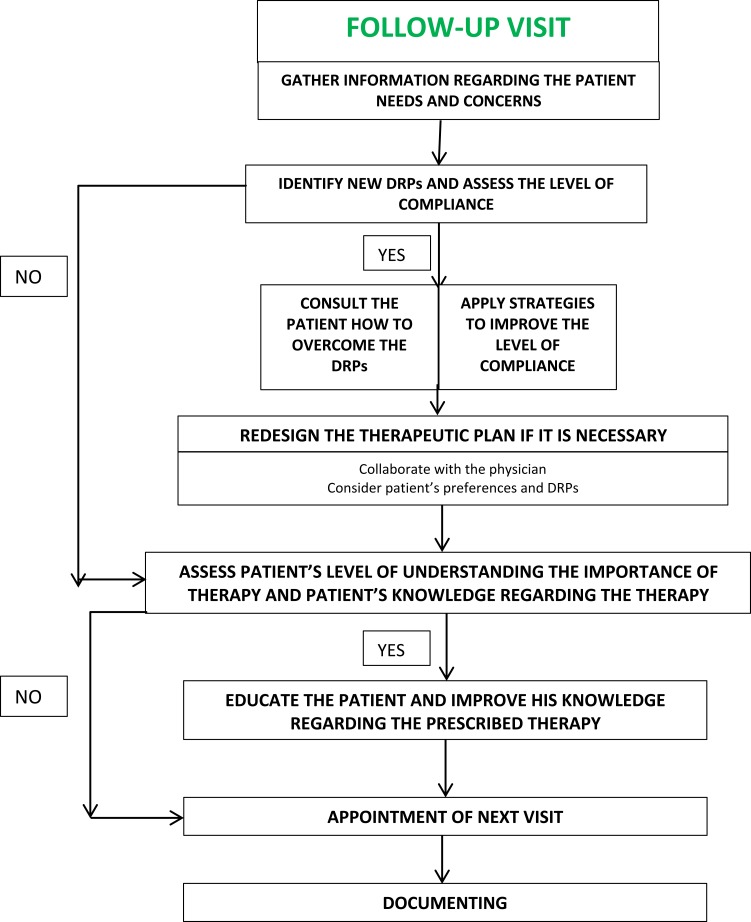
The concepts and goals of provided pharmaceutical care could be based on the type of patient’s visit: initial or follow-up (Figures 5 and 6).36
Figure 5.
Algorithm for applying pharmaceutical care for patients with depression – initial visit.
Figure 6.
Algorithm for applying pharmaceutical care for patients with depression – follow-up visit.
Communication with the Patients and Their Family Members/Caregivers
Establishment of contact with the patient with depression, asking appropriate questions
Communication with patients with mental problems presents a challenge for every pharmacist. Despite the various communication difficulties, the pharmacist should apply innovative strategies for overcoming them.37 The pharmacist should play the dominant role during the conversation, applying appropriate voice tone, using simple and short sentences and body language without discussing several issues simultaneously – a focus should be made on a specific problem through a variety of technical and non-technical skills.38 The consulting pharmacist should pay attention to and adapt the discussion towards patient’s difficulties related to verbal speech and memorization.
The pharmacist as a health professional is able to recognize the initial symptoms, to identify the risky groups, and to target vulnerable people to join supporting groups, initiate nonpharmacological treatment, or make an appointment with a psychiatrist for prescribing eventually of the most appropriate pharmacotherapy. Asking open-ended and closed questions, avoiding confusing questions and interrupting patients while he/she is speaking, listening actively, demonstrating empathy and using the most appropriate body language (eye contact, smile, understanding look, etc.) could help the pharmacist to significantly improve the communication process (Table 1). Moreover, the community pharmacists have frequent contact with patients with depression and other mental health problems which gives them the possibility to engage the patients more actively in the therapeutic process.39
Table 1.
Questions Asked by Pharmacists and Their Purposes
| Question | Purpose |
|---|---|
| What medications do you take in what dose and when do you take them? |
|
| How long do you take these medications according to the current dosage regimen? When was the last time your therapy was changed? |
|
| How do you feel after taking your medication(s)? |
|
| Do you consider stopping abruptly the medications for depression? Do you think interrupting the therapy suddenly is appropriate? |
|
| Do you consult with a pharmacist when buying OTC medicinal products? |
|
| Would you like to ask some questions regarding the medications you take? |
|
| Have you ever had suicidal thoughts? |
|
| |
| |
| Do you see your psychiatrist regularly? |
|
|
Education of the Patient and His/Her Relatives/Caregivers
Give Additional Information About the Disease and Symptoms
As one of the most accessible health professionals, the pharmacists could assist the risk groups (postpartum women, geriatric patients, teenagers, etc.) to visit a psychiatrist. Participating in community-based health campaigns, assuring appropriate advice and information flyers including suitable directions for rational drug use, clarifying the importance of therapy adherence, nonpharmacological treatment approaches and lifestyle modification, the pharmacists could not only improve community health but also contribute in decreasing the stigma of depressive disorders.40 Different studies confirmed the capability of the pharmacist to be involved in screening programs and risk assessment services for depression.41,42 Kondova et al43 identified that 70% of all patients screened in a community pharmacy setting have positive results of PHQ-2 test, and 55% of them had indications of mild-to-moderate depression. One of the possible methods for timely diagnosis is through giving various depression screening tools (Patient Health Questionnaire (PHQ-2 and PHQ-9), Self-Rating Depression Scale (Zung scale (SDS)) or Von Zerssen scale).44
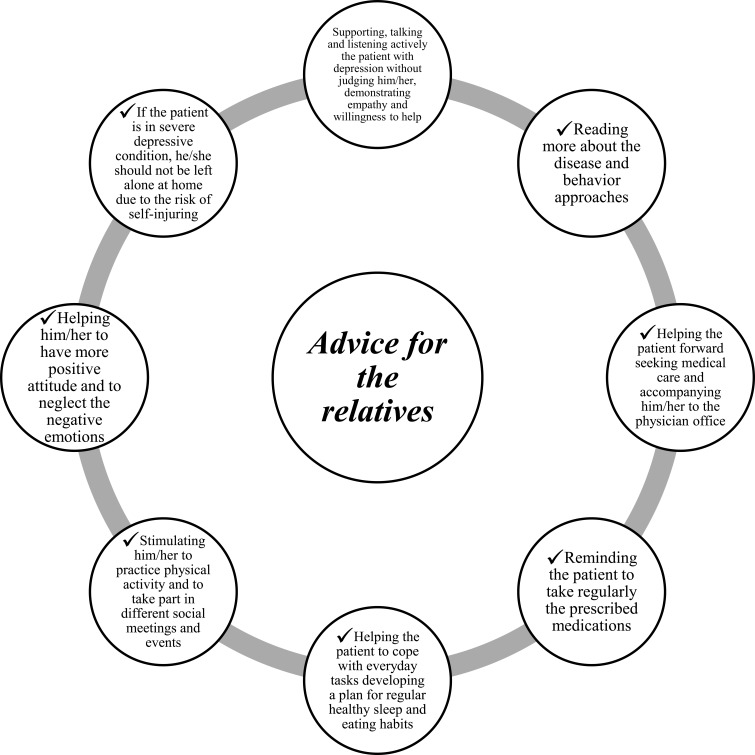
A systematic review published in 2018 concluded that educational materials, outreach visits, and feedback can improve counseling in community pharmacy settings.45 Therefore, additional information regarding the following topics should be given to patients with depression: what the first signs of depression are, how important the consultation with a psychiatrist is due to the risk of serious complications, how the medications should be taken, etc. The relatives and friends could also be involved in the team caring for patients with depression (Figure 7).
Figure 7.
Pharmacists’ advice for the relatives of those affected by depression.
Understanding the Principles of Non-Pharmacological Treatment
There are a lot of nonpharmacological approaches which could be implemented in the individualized care plan for depressive patients: cognitive behavioral therapy [CBT] (the psychotherapist identifies irrational and dysfunctional patient’s thoughts and looks for new more realistic ones; the purpose is to overcome the negative thinking and to modify the existing behavioral models); physical activity – 3–5 times per week, 20–30 minute nature walks, etc.; light therapy – in case of seasonal depressive disorders; music therapy; acupuncture; food supplements (omega 3 oils, Hypericum perforatum); stress management practicing yoga, meditation; healthy eating and sleeping habits; cognitive bibliotherapy.46,47,48
Assuring Effective, Safe, and Appropriate Pharmacological Treatment
Giving Instructions about Dosage Regimen and Therapeutic Scheme
Giving detailed guidance regarding pharmacotherapy by the provider of pharmaceutical care, the service pharmacist, is crucial. The educational process includes an explanation of the therapeutic scheme, the mechanism of action of antidepressant (AD), avoiding complex medical words, and clarification that the onset of action of the prescribed AD is usually after 10–20 days (or longer: 4–6 weeks) and the therapy is continuous (2–6 months) depending on the severity of the disease. The initial dose is lower and it increases gradually. The patient must adhere to the therapeutic scheme as long as it is prescribed knowing that there is no risk of addiction.49 The therapy must not be stopped suddenly – a period of 2–3 weeks is required. Even if the symptoms relieve the therapy must be continued and not stopped without the physician's recommendation due to the risk of withdrawal syndrome (irritability, headache, insomnia, palpitations, sweating, and others lasting several days). Regular monitoring should be provided to every patient with depression in order for suicidal thoughts to be identified in a timely manner. Depressive symptoms are assessed every week or every other week. So, the pharmacist should remind the patient to consult with his/her physician regularly.
Identification and Prevention of Drug-Related Problems
Understanding the Most Common Adverse Drug Reactions (ADRs) and Giving Advice for Overcoming Some ADRs
Informing About the Possible Drug–Drug and Drug–Food Interactions
An essential element of pharmaceutical care services is the so-called medication review aimed to optimize medicines use and improve health outcomes.50 Therefore, serious drug-related problems (DRPs) could be identified or prevented, and specific interventions for the prevention and overcoming of the revealed DRPs could be recommended. PCNE developed a detailed guideline of DRPs, classifying them into several groups according to the type of problems, the causes, planned interventions for overcoming, level of acceptance, status, etc. (Table 2). According to the causes, DRPs are related to prescribing, dispensing, and drug use (Table 3).51
Table 2.
Classification of DRPs According to PCNE51
| Code 8.01 | Groups of DRPs | |
|---|---|---|
| Problems | Р1 | Effectiveness (therapeutic failure, lack of effect, |
| Р2 | Untreated symptoms) | |
| Р3 | Safety (ADRs) | |
| Others (inappropriate drug, etc.) | ||
| Causes | C1 | Drug selection |
| C2 | Drug form | |
| C3 | Dose selection | |
| C4 | Treatment duration | |
| C5 | Dispensing | |
| C6 | Drug use | |
| C7 | Patient related | |
| C8 | Other | |
| Planned interventions | I0–4 | No intervention; at prescribing, patient, drug level; other |
| Intervention acceptance | А1 | Intervention accepted |
| А2 | Intervention not accepted | |
| А3 | Other | |
| Status of the DRP | О0 | Unknown |
| O1 | Solved | |
| О2 | Partially solved | |
| О3 | Not solved |
Table 3.
Classification of DRPs on the Basis of the Causes 51
| Group of DRPs | Examples | |
|---|---|---|
| Related to prescribing | Drug selection | Inappropriate drug; contraindications; duplication of drugs; too many drugs for one indication, etc. |
| Drug form | Inappropriate drug form | |
| Dose selection | Dose too low or too high; wrong instructions for dosing, etc. | |
| Treatment duration | Too short or too long | |
| Related to dispensing | Dispensing | No availability of the drug; no provision of the required information; wrong drug, wrong instructions, etc. |
| Related to drug use | Drug use process (administered by the health specialist or by the patient) | Inappropriate time dosing; patient abuses drug; takes too high or too low dose; wrong way of administration; inability to use the drug correctly, etc. |
Identification and prevention of actual and potential DRPs is one of the main tasks of the pharmacists in the process of providing medication management services. The patient who suffers from depression should be acquainted with the possible adverse drug reactions related to the therapy with antidepressants. The most frequent ADRs are dryness in mouth, tachycardia, tremor, vomiting, sedation, weight gain, arrhythmias, insomnia, skin reactions – photosensitization, reduced sexual functions, etc. Some of them are dose-dependent and decreasing over time. Tobacco consumption might influence the effect of antidepressants – there are several studies showing evidence regarding the reduction of plasma concentration of fluvoxamine, duloxetine, mirtazapine, and trazodone in smokers in comparison with non-smokers. The therapy choice should be based on the status of the patient – whether he is a smoker or non-smoker, due to the risk of pharmacokinetics interactions.52 Alcohol consumption is also contraindicated during the therapy with antidepressants. The pharmacist should clarify that antidepressants might lead to drowsiness and disturbances in concentration and therefore may influence the ability to drive and use machines. The appearance or enhancing of suicidal thoughts might be reported in the beginning of the therapy with AD, but it could not be a reason for interrupting the therapy – the patient and their caregivers should be advised to contact their psychiatrist or emergency center for more information.
Information regarding serotonin syndrome symptoms (SSS) and their prevention and recognition should be provided by the consulting pharmacist. SSS (hyper-reflection, tremor, dizziness, parasympathetic reactions, confusion, etc.) can be a result of simultaneously taking serotonin agonist and serotoninergic medicinal products.24
Other DRPs which could be identified by the pharmacist are: lack of effectiveness of the prescribed medicines, dose too high or too low, drug-drug, drug-food supplements or drug–food interactions (Table 4), and low level of adherence.53 The pharmacist is able to give practical advice for overcoming ADRs reported as a result of AD treatment (Table 5).54,55
Table 4.
Most Common Adverse Drug Reactions and Interactions Described for AD
| Medication (INN) | ADRs | Interactions |
|---|---|---|
| Amitriptyline | Arrhythmias, heart arrest, photo dermatitis, constipation, dryness in mouth, sexual dysfunctions | +Clonidine ≤ hypertonic crisis; +MAO inhibitors ≤ high blood pressure, hyperthermia, convulsion |
| Citalopram Escitalopram Fluoxetine Fluvoxamine Paroxetine Sertraline | Nausea, vomiting, insomnia, dryness in mouth, headache, hypotension, tremor, etc. | +MAO inhib.; +serotoninergic medications (triptans) ≤ SSS +H. perforatum ≤ increased risk of ADRs; +NSAIDs; p.o. anticoagulants ≤ risk of bleeding |
| Venlafaxine | Dryness in mouth, headache, sweating, nervousness, drowsiness, dizziness, etc. | +serotoninergic medications (triptans, SSRIs) ≤ SSS |
| Tianeptine | Tachycardia, insomnia, headache, dryness in mouth, myalgia, insomnia, etc. | +MAOinhibitors ≤ collapse, hyperthermia, convulsions |
Notes: Some ADRs like nausea, diarrhea, and anxiety appear only in the beginning of the therapy. A consultation with a physician is required in cases of lack of improvement. Tricyclic antidepressants (TCA) are not indicated in cases of recent myocardial infarction. Dose adjustment or switch to another medication in the case of lack of effectiveness at a minimum 6 weeks is required.
Table 5.
Some ADRs and Advice Given by Pharmacists for Overcoming Them
| Adverse Drug Reactions (ADRs) | Advice for Overcoming the ADRs |
|---|---|
| Dryness in mouth | Application of artificial saliva products, sugar free gum, vitamin c tablets (short-term use in order to prevent tooth erosion) |
| Antimuscarinic effects (blurred vision, sedation, confusion, etc.) caused by TCA | A strict monitoring in elderly patients as well as taking medications at bed time in order to prevent falls and fractures are recommended |
| Constipation | Advice for regular healthy eating habits: more fiber, liquids, warm water in the morning, abdominal massage, laxatives |
| Sedation | Taking the medications at bed time; otherwise – dose reduction |
| Nausea | Avoiding sweet, salty, or fatty food; taking the medicine after a meal, taking smaller portions of food during the day |
| Insomnia | Taking the medications in the morning |
| Sexual disturbances caused by SSRIs | Dose reduction or change therapy; inclusion of sildenafil at a pinch |
| Hypertension caused by venlafaxine | Blood pressure monitoring regularly; reduction of venlafaxine dosage; change the therapy |
| Tachycardia caused by TCA | Dose reduction or change the therapy |
| Weight gain | Dose reduction or change the therapy |
| Orthostatic hypotension | The patient should avoid standing up abruptly, reduce caffeine intake, drink more water, practice more physical exercise to strengthen the leg muscles |
| Headache | Dose reduction or change the therapy |
| Photosensitization caused by TCA, SSRIs, venlafaxine | Applying sun cream every 2 hours and avoiding sunbathing between 10 a.m. and 4 p.m. |
Creation of Individualized Therapeutic Plan and Defining of Specific Goals
The main therapeutic goal in patients with depression is overcoming the symptoms with reducing as much as possible the adverse drug reactions, prevention of suicidal thoughts, and improving the remission rates. The pharmacist may be actively involved in achieving the goals through realization of various educational programs for clarifying how important the therapy is. Development of an individualized therapeutic plan in collaboration with the psychiatrist and the affected patient and his family members/caregivers, taking into consideration the individual needs and preferences could significantly optimize the therapy and improve the level of adherence.
Assuring Adherence and Assessment of Adherence Level
Literature data shows that 56% of patients taking antidepressants do not adhere to the prescribed therapy for different reasons such as patients’ beliefs, side-effects, or cost.56 The patient should be convinced that the disease is curable, the therapy is based on the severity of the disease, and only strict adherence, psychotherapy provided by a specialist, and supportof family and friends may lead to improvement and full recovery. Assessment of the level of adherence might be made during the regular patient’s visits on the basis of the number of dispensed packages and the number of executed prescriptions, after a conversation with the patient regarding his attitude toward the therapy and the therapeutic plan. A study revealed that patients suggest several pharmacy services to improve the adherence to antidepressants such as: a reminder e-mail before each refill or a small group education session.10 Studies concluded that the pharmacists’ role is crucial for improving the level of adherence to antidepressants.57,58 A systematic review found that pharmacist interventions could be effective in improving the adherence level to antidepressants by15–27%.57 The individualized plan might be optimized on the basis of the reported adverse drug reactions and other DRPs so as to increase the level of adherence – for example to take the medication in the evening in order to avoid sedation during the day or to take the medication in the morning so as to prevent insomnia.
Follow-Up and Reassessment of DRPs
Patients should be aware of the possible ADRs accompanying AD therapy and be reminded to report all ADRs that occur. Tracking the status and reassessment of DRPs is essential and can be performed on the basis of a predefined plan at the pharmacy during the next visit or through telephone calls.59 A published study highlights the importance of clinical pharmacists as he/she is able to improve mild-to-moderate mental health conditions, promote interdisciplinary collaboration between various medical specialists, and to improve the process of documentation and follow-up.60
Conclusion
Application of pharmaceutical care services for patients with depression is effective and leads to condition improvement, reduction of the side-effects, timely identification of and the overcoming of potential or actual DRPs, and improvement of patients’ quality-of-life. Collaboration between psychiatrists, pharmacists, and the active inclusion of the affected and their relatives in the therapy could optimize and improve the complex care for patients with depression and achieving the targeted therapeutic outcomes.
The current article could be used as an initial proposal for creating a methodological guideline for providing pharmaceutical care services for patients with depression. A number of follow-up studies are needed to assess the feasibility of implementing community-based pharmaceutical care for patients with depression, the level of knowledge of pharmacists on depression, the effect of pharmaceutical care on this patient group, and the economic benefits from the point of view of society.
Acknowledgment
This work was supported by the Bulgarian Ministry of Education and Science under the National Program for Research ‘Young Scientists and Postdoctoral Students’.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Compliance with Ethical Standards
The tables and figures are original. No ethical issues exist.
Disclosure
All authors declare that they have no competing interests.
References
- 1.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–543. [PubMed] [Google Scholar]
- 2.Cipolle R, Strand L, Morley P. Chapter Three: Toward a Philosophy of Pharmaceutical Care Practice. Pharmaceutical Care Practice. The Patient Centered Approach to Medication Management. 3rd ed. McGrawHill Medical; 2012:73–100. [Google Scholar]
- 3.Position Paper on the definition of Pharmaceutical Care 2013. PCNE. Available from: https://www.pcne.org//upload/files/3_PCNE_Definition_Position_Paper_final.pdf. Accessed January, 2019.
- 4.Diagnostic and Statistical Manual of Mental Disorders (DSM–5). Available from: https://www.psychiatry.org/psychiatrists/practice/dsm. Accessed February5, 2020. [DOI] [PubMed]
- 5.Kessler RC. The costs of depression. Psychiatr Clin North Am. 2011;35(1):1–14. doi: 10.1016/j.psc.2011.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trautmann S, Rehm J, Wittchen HU. The economic costs of mental disorders: do our societies react appropriately to the burden of mental disorders? EMBO Rep. 2016;17(9):1245–1249. doi: 10.15252/embr.201642951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenberg PE, Birnbaum HG. The economic burden of depression in the US: societal and patient perspectives. Expert Opin Pharmacother. 2005;6(3):369–376. doi: 10.1517/14656566.6.3.369 [DOI] [PubMed] [Google Scholar]
- 8.Reddy MS. Depression: the disorder and the burden. Indian J Psychol Med. 2010;32(1):1–2. doi: 10.4103/0253-7176.70510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubio-Valera М, Bosmans J, Fernández A, et al. Cost-effectiveness of a community pharmacist intervention in patients with depression: a Randomized Controlled Trial (PRODEFAR study). PLOS. 2013. doi: 10.1371/journal.pone.0070588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guillaumie L, Ndayizigiye A, Beaucage C, et al. Patient perspectives on the role of community pharmacists for antidepressant treatment: a qualitative study. Can Pharm J (Ott). 2018;151(2):142–148. doi: 10.1177/1715163518755814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Munger MA. Primary care pharmacists: provision of clinical-decision services in healthcare. Am J Pharm Educ. 2014;78(2):43. doi: 10.5688/ajpe78243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blalock SJ, Roberts AW, Lauffenburger JC, Thompson T, O’Connor SK. The effect of community pharmacy-based interventions on patient health outcomes: a systematic review. Med Care Res Rev. 2013;70(3):235–266. doi: 10.1177/1077558712459215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gomes NC, Abrao PH, Fernandes MR, Beijo LA, Magalhaes VF, Marques LA. Effectiveness of pharmaceutical care about the quality of life in patients with depression. SM J Depress Res Treat. 2015;1(1):1005. [Google Scholar]
- 14.Binakaj Z. Pharmaceutical Care of the Patients Suffering from Depression. J Pharm Pharmacol. 2016;4:253–260. [Google Scholar]
- 15.Salazar-Ospina A, Amariles P, Hincapié-García JA, et al. Effectiveness of the Dader method for pharmaceutical care on patients with bipolar I disorder: results from the EMDADER-TAB study. J Managed Care Specialty Pharm. 2017;23(1):74–84. doi: 10.18553/jmcp.2017.23.1.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gallimore C, Kushner K. A pharmacist-guided protocol for improved monitoring of patients on antidepressants. WML. 2013;112:124–128.:. [PubMed] [Google Scholar]
- 17.Adult Depression Clinical Practice Guideline. 2012. Available from: http://www.providers.kaiserpermanente.org/info_assets/cpp_cod/cod_depression_guideline_0712.pdf. Accessed April, 2019.
- 18.Clinical Practice Guideline on the management of depression in adults. Clinical practice guideline in the Spanish NHS; 2014. Available from: http://www.guiasalud.es/contenidos/GPC/GPC_534_Depresion_Adulto_Avaliat_compl_en.pdf.
- 19.CCNC Adult Depression Toolkit for Primary Care.2015. Available from: https://www.communitycarenc.org/media/related-downloads/ccnc-depression-toolkit.pdf. Accessed April, 2019.
- 20.No health without mental health: How can pharmacy support people with mental health problems?1No health without mental health: How can pharmacy support people with mental health problems? Royal Pharmaceutical Society England. 2018. Available from: https://www.rpharms.com/Portals/0/Documents/RPS%20mental%20health%20roundtable%20report%20June%202018_FINAL.pdf?ver=2018-06-04-100634-577. Accessed April, 2019.
- 21.Rubio-Valera M, Chen TF, O’Reilly CL. New roles for pharmacists in community mental health care: a narrative review. Int J Environ Res Public Health. 2014;11(10):10967–10990. doi: 10.3390/ijerph111010967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pharmacotherapy guideline for psychiatric disorders. NCPRMP in Bulgaria. 2016. Available from: https://www.ncpr.bg/images/normativni_aktove/zakoni/2017/06022017_psyho/FTR_psihichni_zaboliavania.pdf. Accessed January, 2019.
- 23.Depression. World Health Organization, 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/depression. Accessed February, 5, 2020.
- 24.Diagnostic and Statistical Manual of Mental Disorders (DSM–5), APA. Available from: https://www.psychiatry.org/psychiatrists/practice/dsm. Accessed January, 2019. [DOI] [PubMed]
- 25.Tsonev T, Stoyanova V. Chapter 10. Psychiatric Syndromes and Disorders in Internal Diseases. Diagnostic and Therapy Manual of Internal Diseases. Sofia: АРСО; 2012:238–241. [Google Scholar]
- 26.Ferrari AJ, Norman RE, Freedman G, et al. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the global burden of disease study 2010. Baune BT, ed PLoS One. 2014;9(4):e91936. doi: 10.1371/journal.pone.0091936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Practice guidance: pharmaceutical care in depression, Pharmacy professional, 2009/2010. Available from: http://www.rpharms.com/support-pdfs/mental-health--depression-a4.pdf.
- 28.Stahl SM. Essential psychopharmacology online; 2008. Available from: https://stahlonline.cambridge.org/essential_4th_chapter.jsf?page=chapter7_introduction.htm&name=Chapter%207&title=General%20principles%20of%20antidepressant%20%20action#c02598-7-1. Accessed January19, 2020.
- 29.Leonard BE. The concept of depression as a dysfunction of the immune system. Curr Immunol Rev. 2010;6(3):205–212. doi: 10.2174/157339510791823835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwartz T, Siddiqui UA, Stahl SM, et al. Vilazodone: a brief pharmacological and clinical review of the novel serotonin partial agonist and reuptake inhibitor. Ther Adv Psychopharmacol. 2011;1(3):81–87. doi: 10.1177/2045125311409486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D’Agostino A, English CD, Rey JA, et al. Vortioxetine (Brintellix): a new serotonergic antidepressant. Pharm Ther. 2015;40(1):36–40. [PMC free article] [PubMed] [Google Scholar]
- 32.National Council on prices and reimbursement of medicines, Bulgaria. Pharmacotherapy guideline for patients with depression; 2016. Available from: https://www.ncpr.bg/images/normativni_aktove/zakoni/2017/06022017_psyho/FTR_psihichni_zaboliavania.pdf. Accessed February5, 2020.
- 33.van der Molen T, van Boven JF, Maguire T, Goyal P, Altman P. Optimizing identification and management of COPD patients - reviewing the role of the community pharmacist. Br J Clin Pharmacol. 2017;83(1):192–201. doi: 10.1111/bcp.13087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kelling SE, Rondon-Begazo A, DiPietro Mager NA, Murphy BL, Bright DR. Provision of clinical preventive services by community pharmacists. Prev Chronic Dis. 2016;13:E149. doi: 10.5888/pcd13.160232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cipolle R, Strand L, Morley P. Chapter Two: Pharmaceutical Care as the Professional Practice for Patient-Centered Medication Management Services. Pharmaceutical Care Practice. The Patient Centered Approach to Medication Management. 3rd ed. McGrawHill Medical; 2012:37–71. [Google Scholar]
- 36.ASHP Guidelines on a Standardized Method for Pharmaceutical Care. Medication Therapy and Patient Care: Organization and Delivery of Services–Guidelines. 349–351. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/standardized-method-pharmaceutical-care.ashx. Accessed February5, 2020.
- 37.Kamusheva M, Petkova V. [Chapter 3 Communication in Pharmacy Settings. Textbook on Pharmaceutical Care for Students in Pharmacy]. Sofia; 2018:72–119. Bulgarian. ISBN 978-619-183-062-6 [Google Scholar]
- 38.Yamada M, Sakaguchi T, Tokuda K, et al. Fostering mixed-skill pharmacists for careers in health support pharmacies-education to overcome the barrier of limited occupational expertise. Yakugaku Zasshi. 2019;139(4):539–543. doi: 10.1248/yakushi.18-00172-6 [DOI] [PubMed] [Google Scholar]
- 39.Gable KN. Starting the conversation about depression and suicide prevention. Pharm Today. 2019;25(2):44–53. doi: 10.1016/j.ptdy.2019.01.022 [DOI] [Google Scholar]
- 40.Taylor D, Donoghue J, Bleakley S How pharmacists can help patients during depression awareness week, the pharmaceutical journal; 2011. Available from: https://www.pharmaceutical-journal.com/opinion/comment/how-pharmacists-can-help-patients-during-depression-awareness-week/11072268.article?firstPass=false. Accessed February5, 2020.
- 41.Elkhodr S, Saba M, O’Reilly C, Saini B. The role of community pharmacists in the identification and ongoing management of women at risk for perinatal depression: a qualitative study. Int J Soc Psychiatry. 2017;64(1):37–48. doi: 10.1177/0020764017746198 [DOI] [PubMed] [Google Scholar]
- 42.Phimarn W, Kaewphila P, Suttajit S, et al. Depression screening and advisory service provided by community pharmacist for depressive students in university. SpringerPlus. 2015;4:470. doi: 10.1186/s40064-015-1259-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kondova A, Todorova A, Tsvetkova A, et al. Screening and risk assessment for depression in community pharmacy—pilot study. J IMAB. 2018;24:1928–1931. doi: 10.5272/jimab. [DOI] [Google Scholar]
- 44.Self-assessment depression scales. RHI-Razgrad, Bulgaria. Available from: http://www.rzi-razgrad.org/skali-depresiya.pdf. Accessed February5, 2020.
- 45.Al Aqeel S, Abanmy N, AlShaya H, Almeshari A. Interventions for improving pharmacist-led patient counselling in the community setting: a systematic review. Syst Rev. 2018;7(1):71. doi: 10.1186/s13643-018-0727-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Depression, MD. 2011. Available from: http://spisaniemd.bg/md/2013/02/depresiya. Accessed February5, 2020.
- 47.Lesperance F, Frasure-Smith N, St-Andre E, et al. The efficacy of omega-3 supplementation for major depression: a randomized controlled trial. J Clin Psychiatry. 2011;72:1054–1062. doi: 10.4088/JCP.10m05966blu [DOI] [PubMed] [Google Scholar]
- 48.Burns D. Feeling good; 2010. ISBN 978-954-321-678-9
- 49.Introduction to Pharmaceutical Care in Mental Health. NHS, Education for Scotland. Available from: https://www.nes.scot.nhs.uk/media/415392/nes_mental_pharmacy_-_final.pdf.
- 50.Pharmaceutical Care Network Europe. PCNE statement on medication review (pdf); 2013. Available from: https://www.pcne.org/upload/files/150_20160504_PCNE_MedRevtypes.pdf. Accessed January, 2019.
- 51.Classification of Drug-related problems. ‘The PCNE classification V 8.02’. 2012-2017. Available from: https://www.pcne.org/upload/files/230_PCNE_classification_V8-02.pdf. Accessed January, 2019.
- 52.Oliveira P, Ribeiro J, Donato H, Madeira N. Smoking and antidepressants pharmacokinetics: a systematic review. Ann Gen Psychiatry. 2017;16(17):. doi: 10.1186/s12991-017-0140-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pharmaceutical care of people with depression, Course information. Available from: http://www.nes.scot.nhs.uk/media/343889/depression_20information_20-_20updated_202010.pdf. Accessed February5, 2020.
- 54.Feio M, Sapeta P. Xerostomia em cuidados paliativos. Acta Med Port. 2005;18:459–466. [PubMed] [Google Scholar]
- 55.Marques LAM, Galduroz JCF, Noto AR. Pharmaceutical care to patients treated with antidepressants. Rev Calid Asist. 2012;27(1):55–64. doi: 10.1016/j.cali.2011.07.002 [DOI] [PubMed] [Google Scholar]
- 56.Moore CM, Powell BD, Kyle JK. The role of the community pharmacist in mental health. US Pharm. 2018;43:13–20. [Google Scholar]
- 57.Al-Jumah KA, Qureshi NA. Impact of pharmacist interventions on patients’ adherence to antidepressants and patient-reported outcomes: a systematic review. Patient Prefer Adherence. 2011;6:87–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aljumah K, Hassali M. Impact of pharmacist intervention on adherence and measurable patient outcomes among depressed patients: a randomised controlled study. BMC Psychiatry. 2015;15:219. doi: 10.1186/s12888-015-0605-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hattingh HL, Scahill S, Fowler J, Wheeler A. Exploring an increased role for Australian community pharmacy in mental health professional service delivery: evaluation of the literature. J Mental Health. 2015. doi: 10.3109/09638237.2015.1101418 [DOI] [PubMed] [Google Scholar]
- 60.Harms M, Haas M, Larew J, DeJongh B. Impact of a mental health clinical pharmacist on a primary care mental health integration team. Ment Health Clin. 2018;7(3):101–105. doi: 10.9740/mhc.2017.05.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Position Paper on the definition of Pharmaceutical Care 2013. PCNE. Available from: https://www.pcne.org//upload/files/3_PCNE_Definition_Position_Paper_final.pdf. Accessed January, 2019.