Abstract
Background:
Invasive pain procedures can be valuable tools to manage chronic pain. Here, we compared the costs of three procedures used to address chronic pain; punctate midline myelotomy (PMM), placement of a spinal cord stimulator (SCS), or placement of an intrathecal pain pump (ITPP).
Case Description:
This retrospective chart review yielded 9 patients with chronic pain syndromes; 3 had PMM, 3 had SCS, and 3 had ITPP procedures. Variables studied included; pain type, the procedures performed, and the cost of each procedure. The Wilcoxon rank-sum and one-way analysis of variance were used to compare the three groups (P < 0.05). PMM was performed for patients with chronic nonmalignant visceral pain and SCS was utilized for failed back syndrome, while ITPP was placed in two patients with chronic visceral cancer pain and one patient with chronic somatic cancer pain. The mean length of stay was significant shorter for SCS and PMM versus ITPP (e.g., 1, 3.6 ± 0.6 and 15 ± 5.6 days). The mean procedure costs were significantly higher for SCS versus PMM and ITPP (105,234, $71,087, and $79,333); for the latter PMM and ITPP, procedural costs were not significantly different.
Conclusion:
For the three pain procedures discussed in this report, PMM is the most cost-effective as it obviates the need for efficacy trials, and there are: no implant device costs, no medication refills, no maintenance costs, and no complication management costs.
Keywords: Cost, Intrathecal, Myelotomy, Pain, Pump, Refractory, Stimulator

INTRODUCTION
Several reports have shown that three invasive pain procedures, punctate midline myelotomy (PMM), spinal cord stimulation (SCS), and intrathecal drug delivery, can be beneficial to treat chronic pain syndromes and reduce consumption of opioids;[4,5,8] PMM interrupts visceral pain signal transmission and SCS modulates pain signal transmission in the spinal cord, while intrathecal drug delivery systems achieve pain control utilizing smaller doses of opioids closer to the effective receptors. Here, we compared the respective costs of PMM, SCS, and intrathecal pain pump (ITPP) in managing chronic pain syndromes.
METHODS
We performed a retrospective chart review for 9 patients with chronic pain syndromes who underwent PMM (3 patients), SCS (3 patients), and ITPP (3 patients) procedures at our institution. Patients had to be >18 years of age with chronic pain resistant to conventional pain protocols [Table 1]. We used the Wilcoxon rank-sum test to compare the costs between groups along with a one-way analysis of variance (e.g., comparative length of stay (LOS) between groups) with significance level set to (P < 0.05).
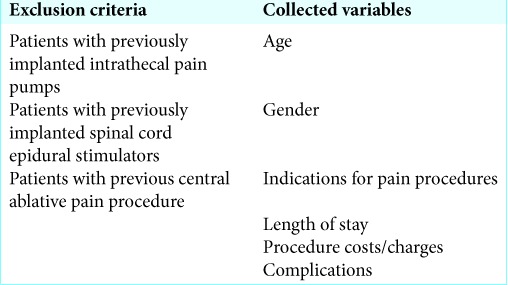
Table 1:
Exclusion criteria and collected variables.
RESULTS
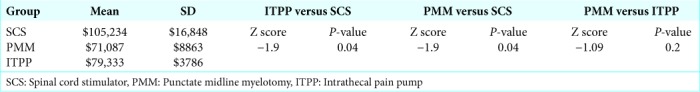
In the SCS, PMM, and ITPP group patients, respectively, averaged 53, 39.3, and 50.7 years of age. The indications for these chronic pain procedures included: SCS for failed back syndrome, PMM for non-malignant visceral pain, and ITPP; two for chronic visceral cancer pain and one for chronic somatic cancer pain. There were no complications in any of the three groups. For SCS, PMM, and ITPP, SCS had the shortest LOS and ITPP the longest: 1, 3.6 ± 0.6 and 15 ± 5.6 days, respectively. Notably, SCS was significantly more expensive ($105,234) than PMM ($71,087) and ITPP ($79,333): the latter two had comparable average costs [Figure 1 and Tables 2 and 3].
Figure 1:
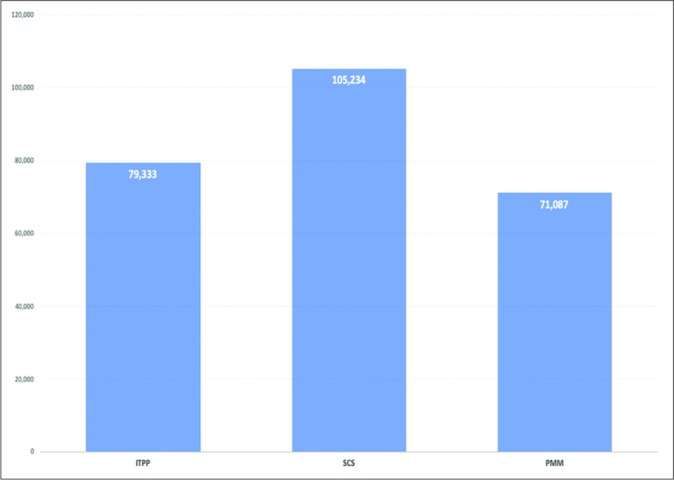
A bar chart shows the average cost of pain procedures (SCS: Spinal cord stimulator, PMM: Punctate midline myelotomy, ITPP: Intrathecal pain pump).
Table 2:
Patients’ characteristics, hospital LOS, and procedure-related cost and complications.
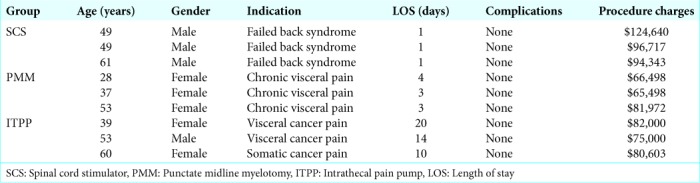
Table 3:
Results of data analysis.
DISCUSSION
All three pain procedures (SCS, PMM, and ITPP) achieve good pain control and reduced the consumption of opioids.[2,5,8] PMM, by lesioning the ascending postsynaptic dorsal column fibers above the segmental level of the pain, can result in immediate/ long-lasting relief of visceral pain with a low complication rate.[8] SCS treats neuropathic, visceral, and somatic pain through inhibition of the pain signal transmission.[5] ITPP delivers minute doses of opioids intrathecally close to the receptors resulting in pain relief without the untoward side effects of high dose intravenous or oral opioids.[2,7]
Relative cost analysis
For PMM, the mean cost was the lowest ($71,087) with the lowest LOS of 1 day, e.g. it does not require a preimplantation trial or annual maintenance cost. Although ITPP initially cost $79,333 with the longest mean LOS was 15 days, it had many other drawbacks both treatment and financial; a preimplantation trial, needed intermittent refills, had initial (median of 1.1 year), and late failures (median 5.9 years) required monthly costs of medication (about $486) and the cost of 1st year – $18,00–30,000 versus later complications ($1000–32,000).[3] The mean cost of SCS was the highest at $105,234 with an intermediate mean LOS of 3.3 days. However, SCS also required; a preimplantation trial, trial stimulation costs ($10,900 and $24,686), lead-related complications (27%), and a significant annual maintenance cost ($5071–7277).[1,6]
CONCLUSION
Three invasive pain procedures SCS, PMM, and ITPP help patients with chronic pain refractory to conventional regimens and may be performed safely and effectively. Here, we found: SCS had the shortest LOS (1 day) and ITPP the longest (15 ± 5.6 days), respectively, but SCS was significantly more expensive ($105,234) than PMM ($71,087) or ITPP ($79,333).
Footnotes
How to cite this article: Aljuboori Z, Meyer K, Sharma M, Ball T, Nauta H. Cost comparison among punctate midline myelotomy, intrathecal pain pump, and spinal cord epidural stimulator. Surg Neurol Int 2020;11:25.
Contributor Information
Zaid Aljuboori, Email: zaid.aljuboori@yahoo.com.
Kimberly Meyer, Email: kim.meyer@ulp.org.
Mayur Sharma, Email: mayur.sharma@ulp.org.
Tyler Ball, Email: tyler.ball@ulp.org.
Haring Nauta, Email: haring.nauta@ulp.org.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bell GK, Kidd D, North RB. Cost-effectiveness analysis of spinal cord stimulation in treatment of failed back surgery syndrome. J Pain Symptom Manage. 1997;13:286–95. doi: 10.1016/s0885-3924(96)00323-5. [DOI] [PubMed] [Google Scholar]
- 2.Bhatia G, Lau ME, Koury KM, Gulur P. Intrathecal drug delivery (ITDD) systems for cancer pain. F1000Res. 2013;2:96. doi: 10.12688/f1000research.2-96.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brogan SE, Winter NB, Abiodun A, Safarpour R. A cost utilization analysis of intrathecal therapy for refractory cancer pain: Identifying factors associated with cost benefit. Pain Med. 2013;14:478–86. doi: 10.1111/pme.12060. [DOI] [PubMed] [Google Scholar]
- 4.Burchiel KJ, Raslan AM. Contemporary concepts of pain surgery. J Neurosurg. 2019;130:1039–49. doi: 10.3171/2019.1.JNS181620. [DOI] [PubMed] [Google Scholar]
- 5.Jeon YH. Spinal cord stimulation in pain management: A review. Korean J Pain. 2012;25:143–50. doi: 10.3344/kjp.2012.25.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar K, Bishop S. Financial impact of spinal cord stimulation on the healthcare budget: A comparative analysis of costs in Canada and the United States. J Neurosurg Spine. 2009;10:564–73. doi: 10.3171/2009.2.SPINE0865. [DOI] [PubMed] [Google Scholar]
- 7.Meyer R, Patel AM, Rattana SK, Quock TP, Mody SH. Prescription opioid abuse: A literature review of the clinical and economic burden in the United States. Popul Health Manag. 2014;17:372–87. doi: 10.1089/pop.2013.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nauta HJ, Soukup VM, Fabian RH, Lin JT, Grady JJ, Williams CG, et al. Punctate midline myelotomy for the relief of visceral cancer pain. J Neurosurg. 2000;92(Suppl 2):125–30. doi: 10.3171/spi.2000.92.2.0125. [DOI] [PubMed] [Google Scholar]


