Abstract
Background:
True intramedullary epidermoid cysts (IECs) not associated with congenital anomalies or previous spinal procedures are extremely rare. In a review of the literature since 1992, only 29 such cases have been reported. Here, we add three new cases in this category.
Case Description:
Three adults presented with spastic paraparesis attributed to thoracic IECs. Gross total microsurgical removal was achieved in two cases, while one case was a partial resection due to capsular adherence to the cord. In all three cases, patients sustained complete recoveries of neurological function and remained symptom free for an average of 5 years follow-up.
Conclusion:
IECs are rare lesions; here, the three located in the thoracic spine, contributed to slow, progressive spastic paraparesis with/without incontinence, and resolved following total (2 patients) and partial (1 patient) resection.
Keywords: Epidermoid cyst, Intramedullary tumor, Paraparesis, Spinal cord, Thoracic spine

INTRODUCTION
Spinal epidermoid tumors are rare benign lesions, representing < 1% of all intraspinal tumors; most are intradural and extramedullary in location.[16,24,34,36] However, true intramedullary epidermoid cysts (IECs) occurring without spinal dysraphism or prior surgery are even more infrequent, comprising 0.8% of all spinal epidermoid tumors.[4,7,8,13,16,17,21,22,24,33-36]
CASE DESCRIPTION
Here, we present three cases of true IEC and review the literature concerning their overall clinical/radiographic presentation and surgical management.
Case 1
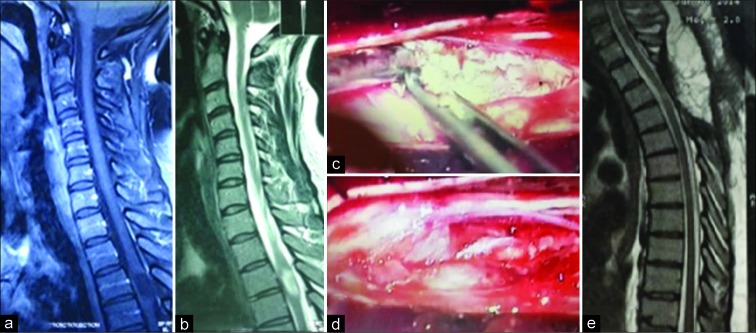
A 40-year-old female presented with a progressive spastic paraparesis and a sensory level bilaterally at T5 over 1 year (e.g. American Spinal Injury Association [ASIA] D classification). The magnetic resonance imaging (MRI) revealed a well-circumscribed intramedullary tumor at the T3-T4 level that was hypointense on T1 weighted and hyperintense on T2-weighted sequences [Figure 1a and b]. After T3 and T4 laminectomy and dural opening, the cord was enlarged and incised longitudinally in the midline allowing for the identification of a white cheese-like avascular tumor [Figure 1c]. Utilizing a microscope, piecemeal removal was achieved [Figure 1d], leaving a few small patches of capsule densely adherent to the cord, behind. The postoperative course was uneventful, and she regained full function within 3 months that was maintained at 2 postoperative years. Further, the postoperative MRI 1 week later shows no residual tumor [Figure 1e].
Figure 1:
(a) Cervicothoracic T1-weighted magnetic resonance imaging (MRI) a hypointense tumor at T3-T4 level, (b) in T2-weighted MRI the mass is hyperintense, (c) intraoperative photograph; a white avascular tumor inside the cord, (d) after total removal, (e) postoperative T2-weighted MRI which is clear from residue.
Case 2
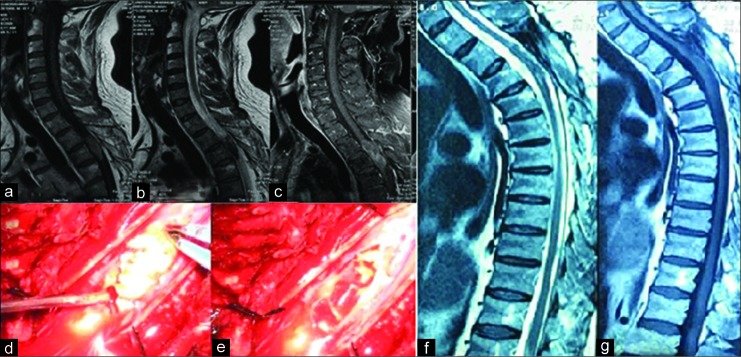
Progressively over a 3-year period, a 37-year-old female also presented with a spastic paraparesis and paresthesia/sensory level T5 bilaterally (ASIA C classification). The cervicothoracic sagittal MRI showed an intramedullary mass at the T3-T4 level; there was a mixture of hypo and hyperintensities on the T1- and T2-weighted images [Figure 2a and b]. On the fat-suppressed MRI, the entire mass was hyperintense [Figure 2c]. She too underwent T3 and T4 laminectomy with midline myelotomy; an avascular white tumor with sebaceous consistency was found and completely removed, including the entire capsule [Figure 2d and e]. The patient gradually improved over the next 6 months; she was able to ambulate without support (ASIA Class D). Five years later, she was intact (ASIA Class E).
Figure 2:
(a) Cervicothoracic T1-weighted sagittal magnetic resonance imaging (MRI) shows a mixed hypo-hyperintense mass at T3-T4 level, (b) in T2-weighted image, the mass is also hypo-hyperintense which is not usual in intramedullary epidermoid cysts, (c) but in fat-suppressed MRI the whole of the tumor is hyperintense, (d) intraoperative photograph; a milky white tumor is demonstrated after midline myelotomy, (e) after total removal of the mass.
Case 3
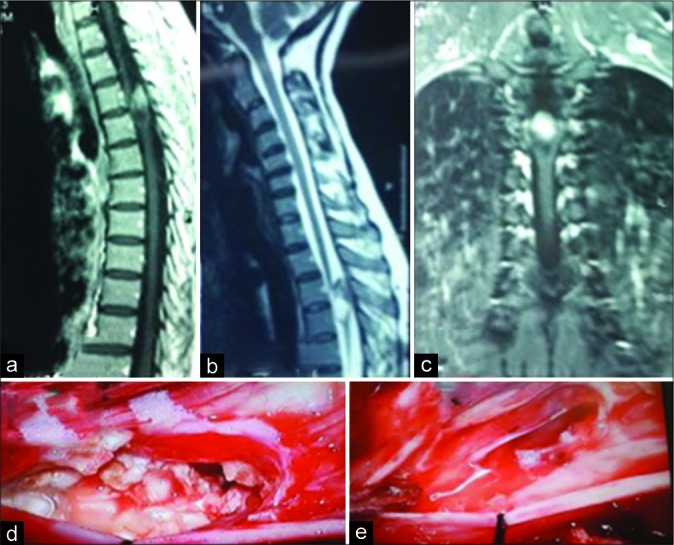
A 41-year-old male who also was paraparetic, had an intramedullary IEC at the T3-T4 level that was similarly grossly totally removed, resulting the in the patient’s eventual full and sustained recovery at 8 years follow-up (ASIA Class E) [Figure 3].
Figure 3:
(a) Cervicothoracic T1-weighted magnetic resonance imaging (MRI) the tumor is isointense, (b) in T2-weighted mage it is hypointense which is unusual for intramedullary epidermoid cysts, (c) but in fat-suppressed MRI the hyperintense mass is compatible with epidermoid, (d) intraoperative photograph shows the characteristic features of and epidermoid cyst, (e) after total removal, (f) T1-weighted MRI at 10-year follow-up shows neither residue nor recurrence, (g) T2-weighted image also is clear.
DISCUSSION
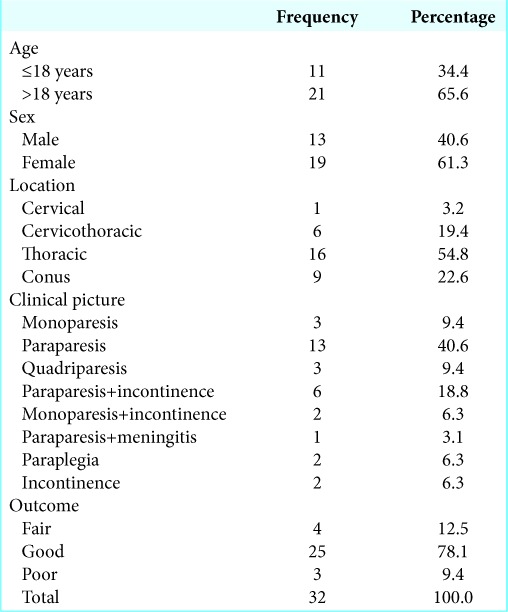
In 1992, Roux et al. reviewed all true IECs within medical literature and could find 47 cases including a case of their own.[34] We updated the literature and could add 31 more cases including our three new ones [Table 1].[16,24,36] Detailed information about the gender, age, and location of the tumor is shown in separately [Table 2].
Table 1:
Review of the literature: Published cases.
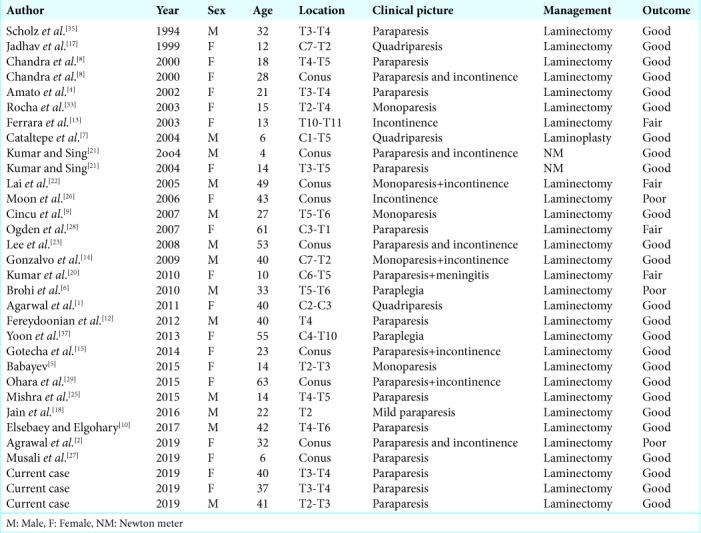
Table 2:
Descriptive statistics.
MRI characteristically demonstrates a nonhomogeneous, hypodense, or isointense mass on T1-weighted MRI scans attributed to the variable amounts of the lipids and proteins within the tumor. They are hyperintense on T2-weighted image due to the keratin content of the cyst.[1,2,4-10,12-15,17,18,20-23,25-29,33,35,37] The diffusion-weighted MR best demonstrates epidermoid cyst homogeneous hyperintensity.[11,19] With these characteristic features, IECs can be easily differentiated from intramedullary lipoma, teratoma, and arachnoid cyst.[30-32] ECs usually have relatively sharp boundaries without any edema and a minimal amount of rim enhancement with a gadolinium. Calcification is extremely.[2]
Surgical management
Surgical removal is the optimal management of IECs. At surgery, following midline myelotomy, the tumor is typically well demarcated; with a smooth, hypovascular, and capsule that is readily removed in over half of the patients. The other half may exhibit dense adhesions of the capsule to the cord, precluding total excision.[3] During operative dissection, spillage into the subarachnoid space is critical to prevent a postoperative chemical meningitis. Histologically, IECs have a thin capsule of stratified, keratinized, and squamous epithelium that contains an accumulation of desquamated epithelial cells, abundant keratin, small foci of calcifications, and cholesterol clefts.
CONCLUSION
IECs, most often found in the thoracic spine, typically contribute to progressive paraparesis. MR studies typically demonstrate well-circumscribed lesions that may be readily totally or partially excised, resulting in marked postoperative neurological recovery.
Footnotes
How to cite this article: Rahimizadeh A, Sharifi G. Spinal intramedullary epidermoid cysts: Three case presentations and literature review. Surg Neurol Int 2020;11:17.
Contributor Information
Abolfazl Rahimizadeh, Email: dr.rahimizadeh@hotmail.com.
Guive Sharifi, Email: gibnow@yahoo.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Agarwal A, Bhake A, Kakani A. Cervical intramedullary epidermoid cyst with liquid contents. Asian Spine J. 2011;5:59–63. doi: 10.4184/asj.2011.5.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agrawal M, Gour SS, Borkar SA. Unusual calcification in intramedullary epidermoid cyst. World Neurosurg. 2019;126:99–100. doi: 10.1016/j.wneu.2019.02.016. [DOI] [PubMed] [Google Scholar]
- 3.Alvord EC., Jr Growth rates of epidermoid tumors. Ann Neurol. 1977;2:367–70. doi: 10.1002/ana.410020504. [DOI] [PubMed] [Google Scholar]
- 4.Amato VG, Assietti R, Arienta C. Intramedullary epidermoid cyst: Preoperative diagnosis and surgical management after MRI introduction. Case report and updating of the literature. J Neurosurg Sci. 2002;46:122–6. [PubMed] [Google Scholar]
- 5.Babayev R, Abbasov B, Ekşi MŞ. Thoracic intramedullary epidermoid cyst-timely fashion diagnosis and treatment. Childs Nerv Syst. 2015;31:793–6. doi: 10.1007/s00381-015-2625-6. [DOI] [PubMed] [Google Scholar]
- 6.Brohi SR, Qureshi SM, Rajput SS, Bhatti NK. Thoracic intramedullary epidermoid with paraplegia for 12 years. J Coll Physicians Surg Pak. 2010;20:135–6. [PubMed] [Google Scholar]
- 7.Cataltepe O, Berker M, Akalan N. A giant intramedullary spinal epidermoid cyst of the cervicothoracic region. Pediatr Neurosurg. 2004;40:120–3. doi: 10.1159/000079853. [DOI] [PubMed] [Google Scholar]
- 8.Chandra P, Manjari T, Devi B, Chandramouli B, Srikanth S, Shankar S. Intramedullary spinal epidermoid cyst. Neurol India. 2000;48:75. [PubMed] [Google Scholar]
- 9.Cincu R, Lázaro JF, Liesa JL, Callizo JR. Dorsal intramedullary spinal epidermoid cysts: Report of two cases and review of literature. Indian J Orthop. 2007;41:395–7. doi: 10.4103/0019-5413.37005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elsebaey ME, Elgohary M. Thoracic spinal intradural intramedullary epidermoid cyst: Case report. Egypt Spine J. 2017;22:50–6. [Google Scholar]
- 11.Fazio MG, Kil AM, Rooks VJ, Biega TJ. Diffusion-weighted magnetic resonance imaging of an intramedullary epidermoid cyst with dorsal dermal sinus tract in a toddler. Case Rep Radiol. 2013;2013:878713. doi: 10.1155/2013/878713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fereydoonian NA, Bakhti S, Fereshtehnejad SM, Tabibkhooei AR. Intramedullary thoracic spine epidermoid cyst with myelopathic presentations: A report of a rare case. Clin Neurol Neurosurg. 2013;115:841–3. doi: 10.1016/j.clineuro.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Ferrara P, Costa S, Rigante D, Mule A, D’Aleo C, Pulitanò S, et al. Intramedullary epidermoid cyst presenting with abnormal urological manifestations. Spinal Cord. 2003;41:645–8. doi: 10.1038/sj.sc.3101482. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalvo A, Hall N, McMahon JH, Fabinyi GC. Intramedullary spinal epidermoid cyst of the upper thoracic region. J Clin Neurosci. 2009;16:142–4. doi: 10.1016/j.jocn.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 15.Gotecha S, Ranade D, Sharma S, Punia P, Kotecha M. Giant intradural intramedullary epidermoid cyst Report of two cases with varied presentations. Asian J Neurosurg. 2014;9:244. doi: 10.4103/1793-5482.146653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halcrow SJ, Crawford PJ, Craft AW. Epidermoid spinal cord tumour after lumbar puncture. Arch Dis Child. 1985;60:978–9. doi: 10.1136/adc.60.10.978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jadhav RN, Khan GM, Palande DA. Intramedullary epidermoid cyst in cervicodorsal spinal cord. J Neurosurg. 1999;90:161. doi: 10.3171/spi.1999.90.1.0161. [DOI] [PubMed] [Google Scholar]
- 18.Jain N, Narayan S, Patil H, Songara A. Epidermoid cyst of the thoracic spine: A rare case. J Spinal Surg. 2016;3:59–62. [Google Scholar]
- 19.Kukreja K, Manzano G, Ragheb J, Medina LS. Differentiation between pediatric spinal arachnoid and epidermoid-dermoid cysts: Is diffusion-weighted MRI useful? Pediatr Radiol. 2007;37:556–60. doi: 10.1007/s00247-007-0463-8. [DOI] [PubMed] [Google Scholar]
- 20.Kumar A, Singh P, Jain P, Badole CM. Intramedullary spinal epidermoid cyst of the cervicodorsal region: A rare entity. J Pediatr Neurosci. 2010;5:49–51. doi: 10.4103/1817-1745.66675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar R, Singh V. Intramedullary mass lesion of the spinal cord in children of a developing milieu. Pediatr Neurosurg. 2004;40:16–22. doi: 10.1159/000076572. [DOI] [PubMed] [Google Scholar]
- 22.Lai SW, Chan WP, Chen CY, Chien JC, Chu JS, Chiu WT. MRI of epidermoid cyst of the conus medullaris. Spinal Cord. 2005;43:320–3. doi: 10.1038/sj.sc.3101673. [DOI] [PubMed] [Google Scholar]
- 23.Lee JH, Shin JJ, Hwang YS, Kim TH, Shin HS, Park SK. Intramedullary epidermoid cyst in thoracolumbar junctiont: A case report. Korean J Spine. 2008;5:219. [Google Scholar]
- 24.Manno NJ, Uihlein A, Kernohan JW. Intraspinal epidermoids. J Neurosurg. 1962;19:754–65. doi: 10.3171/jns.1962.19.9.0754. [DOI] [PubMed] [Google Scholar]
- 25.Mishra AM, Prabhuraj AR, Pruthi N, Rao S. Adult intramedullary epidermoid cyst without spinal dysraphism: A case report. Surg Neurol Int. 2018;9:122. doi: 10.4103/sni.sni_117_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moon MS, Shim YS, Sun DH. Epidermoid cyst of the conus medullaris and cauda equina a case report. J Korean Soc Spine Surg. 2006;13:142–6. [Google Scholar]
- 27.Musali SR, Mohammed I, Gollapudi PR, Maley SK. Dorsal spinal intradural intramedullary epidermoid cyst: A rare case report and review of literature. J Neurosci Rural Pract. 2019;10:352–4. doi: 10.4103/jnrp.jnrp_304_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ogden AT, Khandji AG, McCormick PC, Kaiser MG. Intramedullary inclusion cysts of the cervicothoracic junction. Report of two cases in adults and review of the literature. J Neurosurg Spine. 2007;7:236–42. doi: 10.3171/SPI-07/08/236. [DOI] [PubMed] [Google Scholar]
- 29.Ohara T, Maki S, Furuya T, Inada T, Kamiya K, Ota M, et al. Elderly onset intramedullary epidermoid cyst in the conus medullaris: A case report. J Med Case Rep. 2015;9:7. doi: 10.1186/1752-1947-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rahimizadeh A, Sharifi G. Anterior cervical arachnoid cyst. Asian Spine J. 2013;7:119–25. doi: 10.4184/asj.2013.7.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rahimizadeh A, Soufiani H. Intramedullary arachnoid cyst in association with cervical spondylosis: Case report. Spine J. 2013;13:e21–5. doi: 10.1016/j.spinee.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 32.Rahimizadeh A, Soufiani H. Upper cervical intermedullary lipoma with extension into the cistern magna in an elderly: Report of a case and review of the literature. World Spinal Column J. 2011;2:114–8. [Google Scholar]
- 33.Rocha Júnior MA, de Carvalho GT, Faria MP, Faglioni W Jr, de Souza AA. Intramedullary epidermoid tumor: Case report. Arq Neuropsiquiatr. 2003;61:867–9. [PubMed] [Google Scholar]
- 34.Roux A, Mercier C, Larbrisseau A, Dube LJ, Dupuis C, Del Carpio R. Intramedullary epidermoid cysts of the spinal cord. Case report. J Neurosurg. 1992;76:528–33. doi: 10.3171/jns.1992.76.3.0528. [DOI] [PubMed] [Google Scholar]
- 35.Scholz M, Märzheuser-Brands S, Gottschalk J, Böck JC, Lanksch WR. Intramedullary epidermoid cyst. A case report. Neurosurg Rev. 1994;17:89–93. doi: 10.1007/BF00309994. [DOI] [PubMed] [Google Scholar]
- 36.Singh K, Pandey S, Gupta PK, Sharma V, Santhosh D, Ghosh A. Acquired dorsal intraspinal epidermoid cyst in an adult female. Surg Neurol Int. 2016;7:S67–9. doi: 10.4103/2152-7806.174890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yoon SH, Jahng TA, Kim KJ, Chung CK, Kim HJ. An extensive intramedullary epidermoid cyst with a longstanding history of paraplegia: A case report. J Neurol Surg A Cent Eur Neurosurg. 2013;74(Suppl 1):e1–3. doi: 10.1055/s-0032-1304221. [DOI] [PubMed] [Google Scholar]