Abstract
Background:
Atlantoaxial pseudoarticulation rarely involves the cervical spine, and its etiology is unclear. In theory, pseudoarticulation is comparable to Bertolotti’s syndrome in the lumbar spine or may be attributed to an aberrant focal fusion between C0-C1-C2 that occurs during the gastrulation of embryologic development.
Case Description:
A 39-year-old female presented with neck pain and upper extremity weakness. Magnetic resonance/computed tomography studies documented a left-sided unilateral pseudoarticulation between the lamina of C1 and C2 causing compression of the dorsal spinal cord. Following resection of the accessory C1/C2 joint utilizing a C1 hemilaminectomy and partial C2 laminectomy, the patient’s neck pain and weakness resolved. Histologically, the tissue showed benign osteocartilaginous tissue with no synovial capsule.
Conclusion:
Here, the authors present a case of occiput-C1-C2 pseudojoint formation, leading to clinical and radiographic findings of cord compression due to boney outgrowth.
Keywords: Accessory joint, Atlantoaxial joint, Bertolotti’s syndrome, Cervical spine, Pseudoarticulation

INTRODUCTION
Pseudoarticulations of the C1-C2 complex are rare.[1,3,5,6] They can be due to a developmental abnormality or may be acquired. Here, we present a 39-year-old female who exhibited a unilateral accessory joint involving the C1-C2 junction and reviewed some of the pertinent literature.
CASE REPORT
A 39-year-old female presented with a 10-month history of the right-sided neck pain and bilateral hand numbness/weakness, accompanied by leg heaviness. Her neck pain was exacerbated by movement but was also present at rest. She described an accident while on an all-terrain vehicle 2 years ago but did not recall sustaining any specific cervical injury. She exhibited 4/5 strength involving both hands and the right triceps, decreased sensation throughout the hands, with diminished light touch, pain, and temperature in the hands. Reflexes remained intact. The outside computed tomography obtained 2 months previously demonstrated osseous hypertrophy of the C1 lamina, while the cervical magnetic resonance (MR) showed a pseudoarticulation between the lamina of C1 and C2 [Figure 1].
Figure 1:

Computed tomography (CT) images in sagittal (a) and coronal (b) plans show an osseous pseudojoint between the left lamina of C1 and C2. T2-weighted magnetic resonance images in the sagittal (c) and axial (d) planes demonstrate the degree of cord compression caused by the complex. Finally, the topography of the pseudojoint can be appreciated on three-dimensional CT reconstruction (e).
The patient underwent left-sided C1 hemilaminectomy and partial C2 laminectomy at which time the thickened pseudoarticulation at C1 was removed and was sent for pathology. Histologically, it proved to be “benign osteocartilaginous tissue with fibrosis.” The patient did well and regained full strength bilaterally on postoperative day 1. Two weeks later, initial neck pain and prior numbness resolved. Postoperative flexion and extension films showed no delayed instability. Six months later, with mild residual occipital pain, the MR image demonstrated complete resection of the lesion and no residual left-sided stenosis.
DISCUSSION
We found three similar reported cases in the literature focusing on C1-C2 pseudoarticulation [Table 1].[1,5,6]
Table 1:
Summary of relevant literature to date on C1-C2 pseudoarticulation.
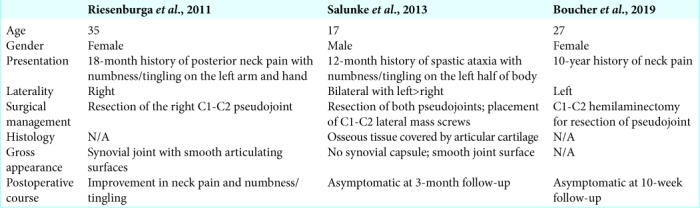
All three cases underwent successful resection of the pseudoarticulation with neurologic improvement.[1,5,6] These studies reported different potential etiologies of these lesions. Riesenburger et al. suggested an embryonic explanation, for example, an aberrant focal fusion of the C0, C1, and C2 sclerotomes which occurred during gastrulation and was then influenced by genetic and fetal factors resulting in improper synovial joint synthesis between the C1 and C2 lamina.[5] Salunke et al. agreed that joint formation was likely precipitated by abnormal segmentation initiated at the embryologic stage noting the presence of hyaline cartilage which could only represent a true joint.[6] However, there was no grossly apparent synovial capsule surrounding the joint and thus the author’s acknowledged the possibility the pseudojoint. Boucher et al. likened the condition to Bertolotti’s syndrome, as understanding the pathogenesis underlying Bertolotti’s syndrome may help elucidate the mechanism of the C1-C2 pseudoarticulation.[1] We believe an analogous biomechanical mechanism to Bertolotti’s syndrome that occurs in the upper cervical spine in the patient presented and the three prior cases leading to the C1-C2 pseudoarticulation.[2,4]
Further work is required to quantify the relationship between subaxial kyphosis and formation of upper cervical accessory joints. Further work should focus on delineating the clinical conditions that may increase risk for the formation of upper cervical accessory joints, particularly the degree subaxial kyphosis.
CONCLUSION
This case describes a 39-year-old female who presented with neck pain and was found to have left-sided unilateral pseudoarticulation between the lamina of C1 and C2 causing compression of the dorsal spinal cord who improved with C1 hemilaminectomy and partial C2 laminectomy. Atlantoaxial pseudoarticulation of the C1-C2 complex is exceedingly rare and, in theory, is comparable to Bertolotti’s syndrome in the lumbar spine, although further work is needed to describe the biologic and mechanical factors that are involved in this disorder.
Footnotes
How to cite this article: Eaton RG, Viljoen SV. Unilateral atlantoaxial pseudoarticulation: A case report, literature review, and proposed mechanism. Surg Neurol Int 2020;11:20.
Contributor Information
Ryan G. Eaton, Email: ryan.eaton@osumc.edu.
Stephanus V. Viljoen, Email: stephanus.viljoen@osumc.edu.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Boucher AB, Kashlan ON, Gary MF, Refai D. Atlantoaxial pseudoarticulation as a cause of neck pain: case illustration. J Neurosurg Spine. 2018;30:182–3. doi: 10.3171/2018.8.SPINE18918. [DOI] [PubMed] [Google Scholar]
- 2.Jancuska JM, Spivak JM, Bendo JA. A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg. 2015;9:42. doi: 10.14444/2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klimo P, Jr, Rao G, Brockmeyer D. Congenital anomalies of the cervical spine. Neurosurg Clin N Am. 2007;18:463–78. doi: 10.1016/j.nec.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Mahato NK. Morphological traits in sacra associated with complete and partial lumbarization of first sacral segment. Spine J. 2010;10:910–5. doi: 10.1016/j.spinee.2010.07.392. [DOI] [PubMed] [Google Scholar]
- 5.Riesenburger RI, Klimo P, Jr, Yao KC. A fourth atlantoaxial joint: An initial description. Spine J. 2011;11:e6–9. doi: 10.1016/j.spinee.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Salunke P, Futane S, Vaiphei K. Posterior bilateral supernumerary atlantoaxial facets: True or false joint? Spine (Phila Pa 1976) 2013;38:E1633–5. doi: 10.1097/BRS.0b013e3182a8a603. [DOI] [PubMed] [Google Scholar]


