In this study, we assessed temporal trends in the prevalence of suicidal ideation, plans, and attempts among sexual minority and heterosexual youth over a 23-year period.
Abstract
OBJECTIVES:
In this study, we determined trends in prevalence of suicidal thoughts and behaviors among lesbian, gay, bisexual, and heterosexual youth from 1995 to 2017 using population-based surveillance data.
METHODS:
Data were drawn from the Massachusetts Youth Risk Behavior Survey from 1995 to 2017 (unweighted N = 41 636). The annual percent change (APC) in prevalence of suicidal ideation, plans, and attempts was stratified by sexual orientation as indexed by sexual identity and sexual behavior.
RESULTS:
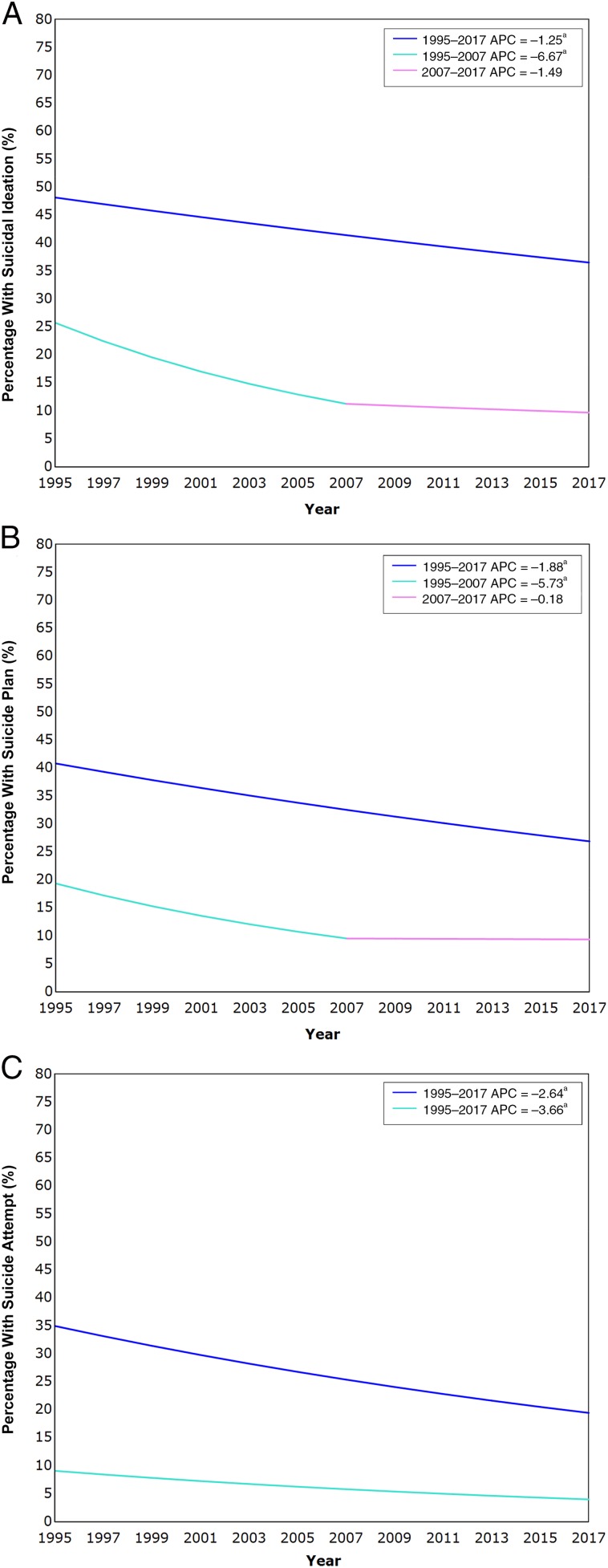
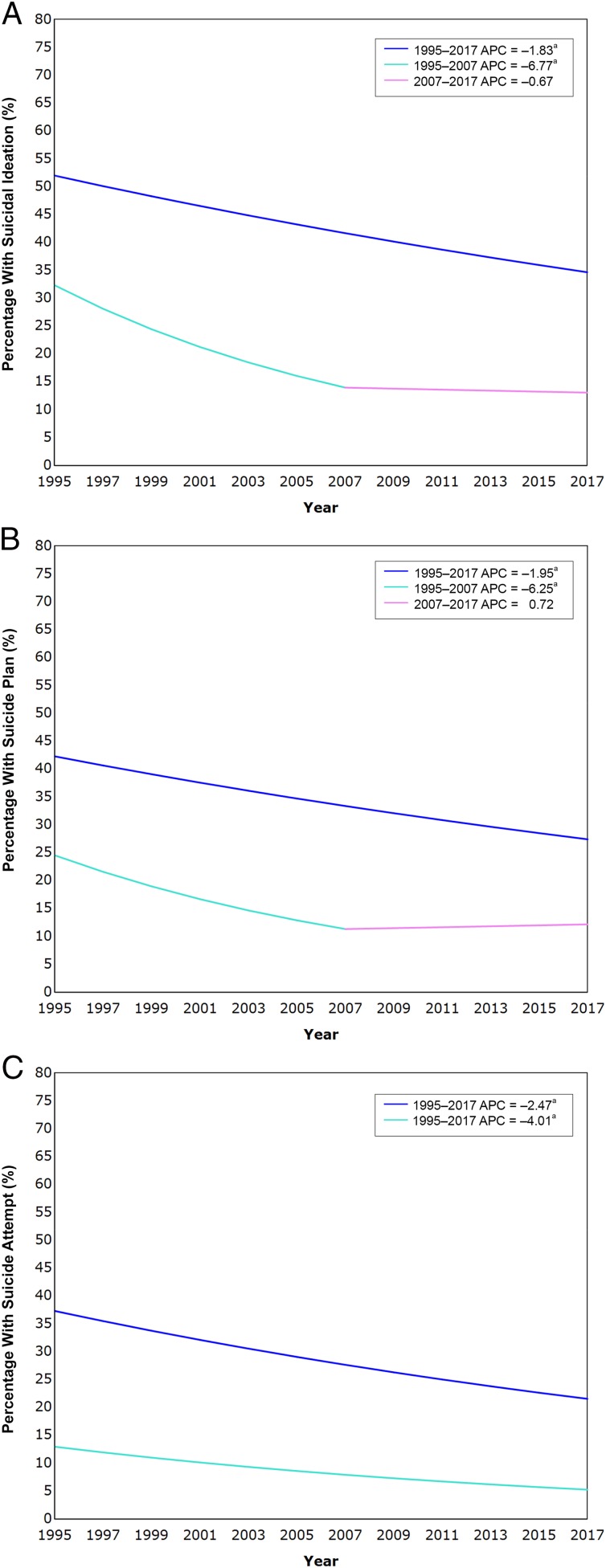
Among sexual minority youth, prevalence rates declined over the entire study period for suicidal ideation (APCsexual identity = −1.25; APCsexual behavior = −1.83), plans (APCsexual identity = −1.88; APCsexual behavior = −1.95), and attempts (APCsexual identity = −2.64; APCsexual behavior = −2.47). Among heterosexual youth, prevalence rates declined from 1995 to 2007 for suicidal ideation (APCsexual identity = −6.67; APCsexual behavior = −6.77) and plans (APCsexual identity = −5.73; APCsexual behavior = −6.25). These declines in ideation and plans were steeper than those for sexual minority youth. Prevalence of suicide attempts declined across the entire study period among heterosexual youth (APCsexual identity = −3.66; APCsexual behavior = −4.01). Prevalence of all 3 outcomes remained markedly high among sexual minority youth across the 23-year study period.
CONCLUSIONS:
Although suicidal thoughts and behavior have generally declined among sexual minority and heterosexual youth, disparities in these outcomes persist, and their prevalence among sexual minority youth has remained consistently elevated. Prioritized screening for risk for suicidal thoughts and behaviors in this vulnerable population is imperative to reduce disparities and prevalence of these outcomes.
What’s Known on This Subject:
Sexual minority youth are at higher risk for suicide-related outcomes compared with heterosexual youth.
What This Study Adds:
Although suicidal thoughts and behaviors have declined among sexual minority youth in a population-representative sample, disparities relative to heterosexual youth in these outcomes persist.
Disparities in health and the attendant health care needs of sexual minority individuals have received increasing attention in recent years.1,2 Indeed, in October 2016, the National Institute of Minority Health and Health Disparities and the Agency for Healthcare Research and Quality together officially designated sexual (and gender) minority populations as health disparity populations to facilitate research with the ultimate aim of eliminating these disparities.3 Concerns regarding health disparities are especially relevant to suicidal thoughts and behaviors,4,5 and adolescence is a period of development associated with a marked increase in the onset of these clinical outcomes.6 Limiting progress in addressing these issues, however, is the relative dearth of population-representative studies that allow for accurate estimates of the prevalence of suicidal thoughts and behaviors among sexual minority populations7; most studies of adolescents in this area are based on convenience samples.8 Such studies featuring nonrandom samples often introduce significant bias in estimates of prevalence of these outcomes.9 Moreover, in a report commissioned by the National Institutes of Health on sexual and gender minority health, the National Academy of Medicine concluded that the “existing body of evidence is sparse and that substantial research is needed.”2 Therefore, characterizing suicide risk in these populations remains a high priority,4 with the National Institutes of Health recently issuing a call for further study on the prevalence of suicide among sexual minority populations.10 In addition to characterizing the prevalence of suicidal thoughts and behaviors in sexual minority populations, a question of particular public health importance is whether the prevalence of these outcomes has changed over time. Monitoring temporal trends in prevalence of suicidal thoughts and behaviors is especially critical for evaluating our progress relative to the goal put forth by the National Academy of Medicine of eliminating disparities in health for sexual minority populations.2
How sexual minority status is defined within individual studies has important implications for estimating prevalence in clinical outcomes.11 In many studies, researchers have relied on a single index of sexual orientation, for example, same-sex behavior. Yet, relying solely on this strategy is potentially problematic insofar as a substantial proportion of individuals who identify as a sexual minority, particularly in the case of adolescents, have not engaged in same-sex behavior, and conversely, not everyone who has engaged in same-sex behavior necessarily identifies as a sexual minority.12 For these reasons, adopting multiple indices of sexual orientation is necessary to accurately characterize the prevalence of health-related outcomes in sexual minority populations.13
Within this context, in the current study, we examined temporal trends in suicidal thoughts and behaviors in population-representative data for sexual minority and heterosexual adolescents. That is, we assessed the 12-month prevalence of suicidal ideation, suicide plans, and suicide attempts among these 2 groups over a 23-year period. In so doing, we also sought to provide a comprehensive assessment of these issues by employing multiple indices of sexual orientation, specifically self-reported sexual orientation and same-sex behavior.
Methods
The Youth Risk Behavior Surveillance System (YRBSS) was established by the Centers for Disease Control and Prevention to monitor health risk behaviors among adolescents over time. Data were drawn from the Massachusetts YRBSS for 1995–2017 (unweighted N = 41 636) because Massachusetts was the first state, beginning in 1995, to include items used to assess sexual orientation on the basis of identity and behavior, thus allowing for a population-based analysis of trends over a substantial period of time. Using a multistage cluster sample design, the state YRBSS obtains biannual data representative of students in grades 9 to 12 for the state.14 All data were collected anonymously. The participant response was typically high (eg, 83.7% in 2017).15 This study used publicly available secondary data and was exempt from institutional review board review.
Sexual orientation was assessed 2 ways: by self-reported sexual orientation identity and by same-sex behavior. For sexual orientation identity, respondents were asked to self-identify with 1 of the following: heterosexual, gay or lesbian, bisexual, and not sure. Respondents who selected any of the latter 3 options were classified as sexual minority individuals on the basis of identity. Those unsure of their sexual orientation were included because such individuals appear to be at elevated risk for suicidal thoughts and behaviors and to follow the precedence of previous studies.16–19 Same-sex behavior was assessed by asking respondents about sexual partners in their lifetime, with the options being: girls only, boys only, girls and boys, and no sexual partners. Respondents who endorsed having same-sex partners were classified as sexual minority individuals on the basis of behavior, and respondents with no sexual partners were excluded from analyses relating to sexual behavior.
For past-year suicidal thoughts and behaviors, respondents were asked 3 questions about whether they (1) had seriously considered suicide, (2) had a suicide plan, and (3) had attempted suicide. These items have been found to be valid for assessing suicidal thoughts and behaviors.20
Rates of these 4 outcomes were stratified by sexual orientation status and weighted to obtain population-representative estimates. Joinpoint regression21,22 was conducted to estimate annual percent change (APC) with 95% confidence intervals. Trends are presented as linear segments connected at the years (ie, joinpoints) when the slope of each trend changed significantly. If no significant change in trend is observed, a straight line is fitted over the full period on the basis of a simple loglinear model. z scores were then calculated to determine if the difference between APCs for sexual minority and heterosexual youth was statistically significant.23
These analyses were conducted separately for sexual identity and sexual behavior. Following the precedence of previous population-based studies, lesbian, gay, bisexual, and unsure youth were combined to ensure adequately powered analyses.17,18 Sensitivity analyses were conducted for sexual identity, and respondents unsure of their sexual identity were excluded.
Results
Prevalence of Suicide-Related Outcomes
In Supplemental Table 1 we present unweighted n values and weighted percentages and SEs for the sample stratified by year, sexual identity, sexual behavior, and gender. The 12-month prevalence rates of suicidal ideation, suicide plans, and suicide attempts from 1995 to 2017 stratified by sexual identity and sexual behavior are provided in Supplemental Table 2, and 12-month prevalence rates of all suicide-related outcomes for sexual minority youth, excluding youth unsure of their sexual identity, are presented in Supplemental Table 3. When sexual minority status was based on sexual identity, 12-month prevalence rates among sexual minority youth across the 23-year study period ranged from 32.5% to 40.4% for suicidal ideation, from 24.3% to 40.4% for suicide plans, and from 15.0% to 32.7% for suicide attempts. When those unsure of their sexual identity were excluded, these prevalence rates ranged from 35.6% to 62.8% for suicidal ideation, from 26.0% to 50.9% for suicide plans, and from 12.8% to 46.0% for suicide attempts. Among heterosexual youth, 12-month prevalence rates ranged from 9.4% to 25.1% for suicidal ideation, from 8.8% to 18.2% for suicide plans, and from 3.5% to 9.0% for suicide attempts.
A similar set of results was obtained when sexual minority status was defined by sexual behavior. That is, among sexual minority youth, 12-month prevalence ranged from 34.5% to 55.1% for suicidal ideation, from 26.1% to 43.7% for suicide plans, and from 12.2% to 37.9% for suicide attempts. Among heterosexual youth, 12-month prevalence rates varied from 12.0% to 31.0% for suicidal ideation, from 10.2% to 22.8% for suicide plans, and from 5.5% to 13.0% for suicide attempts.
Trend Analyses
Across this 23-year period, the prevalence rates of all suicide-related outcomes declined for both sexual minority and heterosexual youth. These results held true regardless of whether sexual orientation was based on self-identification or sexual behavior (see Supplemental Table 4 for a summary of all regression analyses). In the case of suicidal ideation, a significant decline in prevalence was observed across the entire study period for sexual minority youth (see Figs 1A and 2A). Among heterosexual youth, a significant decrease was found from 1995 to 2007, after which a plateau appeared to emerge from 2007 to 2017. Additionally, the decline from 1995 to 2007 was significantly sharper for heterosexual youth than for sexual minority peers (z scoresexual identity = 5.49, P < .001; z scoresexual behavior = 4.45, P < .001). For suicide plans, a similar set of findings was revealed (see Figs 1B and 2B). Specifically, sexual minority youth experienced a decrease in prevalence of suicide plans across the 23-year period, whereas heterosexual counterparts saw a significantly steeper decrease from 1995 to 2007 (z scoresexual identity = 4.28, P < .001; z scoresexual behavior = 4.25, P < .001) before reaching a plateau from 2007 to 2017. In the case of suicide attempts, however, both sexual minority and heterosexual youth saw a significant decrease in prevalence from 1995 to 2017 (see Figs 1C and 2C), and the APCs for these 2 groups did not differ (z scoresexual identity = 1.29, P = .10; z scoresexual behavior = 1.43, P = .08).
FIGURE 1.
A, APC in 12-month prevalence of suicidal ideation among sexual minority and heterosexual youth based on sexual identity, 1995–2017. B, APC in 12-month prevalence of suicide plans among sexual minority and heterosexual youth based on sexual identity, 1995–2017. C, APC in 12-month prevalence of suicide attempts among sexual minority and heterosexual youth based on sexual identity, 1995–2017. a The APC is significantly different from zero at the α = .05 level.
FIGURE 2.
A, APC in 12-month prevalence of suicidal ideation among sexual minority and heterosexual youth based on sexual behavior, 1995–2017. B, APC in 12-month prevalence of suicide plans among sexual minority and heterosexual youth based on sexual behavior, 1995–2017. C, APC in 12-month prevalence of suicide attempts among sexual minority and heterosexual youth based on sexual behavior, 1995–2017. a The APC is significantly different from zero at the α = .05 level.
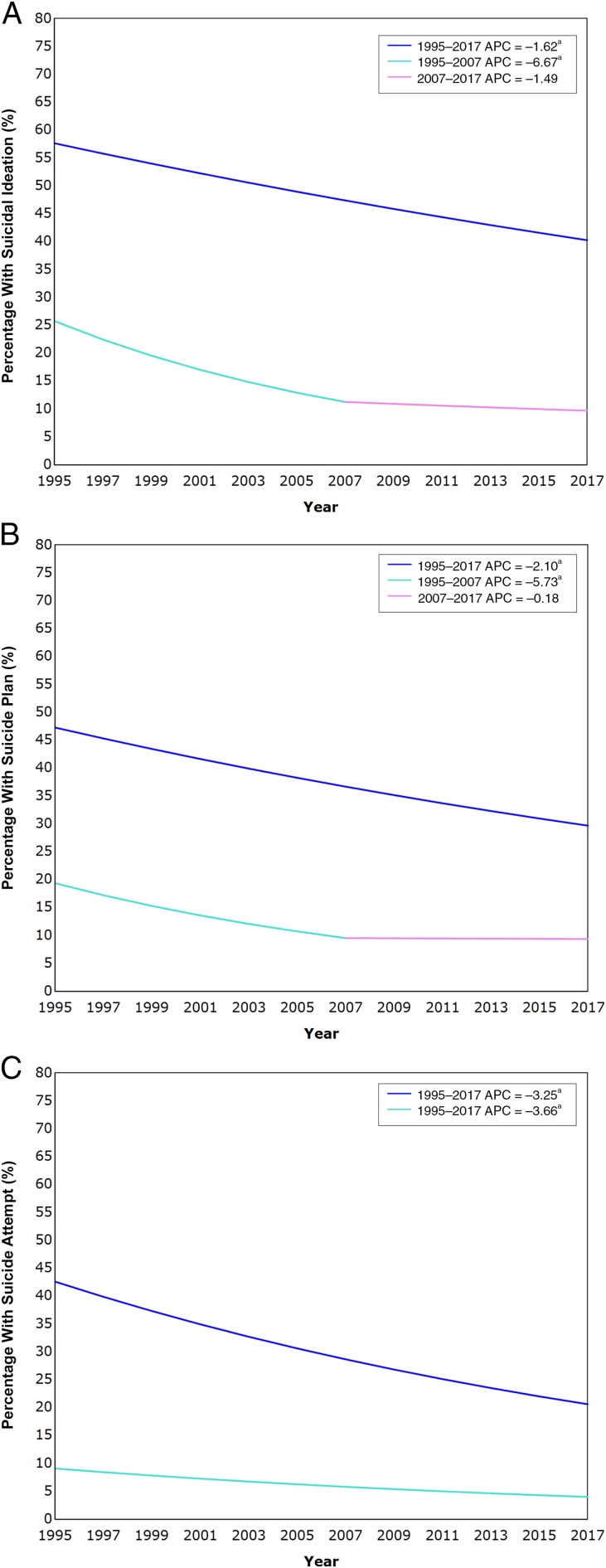
In sensitivity analyses, after we excluded respondents who had reported being unsure of their sexual identity, the results remained essentially unchanged. That is, significant declines in prevalence rates were observed across the entire 23-year period for suicidal ideation, plans, and attempts among sexual minority youth (see Fig 3). Among heterosexual youth, declining rates were found for suicidal ideation and plans from 1995 to 2007 and for suicide attempts across the entire study period. The APCs from 1995 to 2007 remained significantly steeper for heterosexual youth than for sexual minority counterparts in the case of suicidal ideation (z score = 4.82, P < .001) and suicide plans (z score = 3.83, P < .001). The APCs also did not differ between these 2 groups for suicide attempts (z score = 0.34, P = .37).
FIGURE 3.
A, APC in 12-month prevalence of suicidal ideation among sexual minority and heterosexual youth based on sexual identity, excluding those unsure of their sexual identity, 1995–2017. B, APC in 12-month prevalence of suicide plans among sexual minority and heterosexual youth based on sexual identity, excluding those unsure of their sexual identity, 1995–2017. C, APC in 12-month prevalence of suicide attempts among sexual minority and heterosexual youth based on sexual identity, excluding those unsure of their sexual identity, 1995–2017. a The APC is significantly different from zero at the α = .05 level.
Discussion
With the current study, we provide the first examination of long-term temporal trends in the prevalence of suicidal ideation, plans, and attempts in a large population-representative sample of youth stratified by sexual orientation. Several notable trends were found across the 23-year study period. An important positive development is that all 3 suicide-related outcomes have experienced a significant decline since 1995, and this is true for both sexual minority and heterosexual youth, although a leveling off occurred for the prevalence of suicidal ideation and plans in the case of heterosexual youth starting in 2007. These findings held regardless of how sexual orientation was operationalized, be it sexual identity or sexual behavior.
Closer examination of the data, however, revealed a general pattern of concern regarding the prevalence of suicide-related outcomes and persistence of disparities among sexual minority youth over the past several decades. Specifically, throughout the entire study period, the prevalence rates of all 3 suicide-related outcomes were persistently and substantially higher among sexual minority youth relative to their heterosexual peers. Furthermore, although significant declines were observed for the prevalence of all 3 outcomes among sexual minority youth across the entire study period, the rate of this decline was significantly slower than that for heterosexual youth, despite the higher prevalence of these outcomes among sexual minority youth allowing for greater potential room for improvement. Only for suicide attempts was this not the case, although even for this outcome, differences between sexual minority and heterosexual youth in APCs were marginally significant. Finally, even with the significant decline in these clinical outcomes among sexual minority youth across the 23-year period, their prevalence rates remained markedly high during the most recent assessment in 2017, highlighting the substantial progress that remains to be made in addressing major mental health concerns in this at-risk population. Indeed, although the most recent year for which data were available saw the lowest rates of all suicide-related outcomes among sexual minority youth, these rates were still as high as 35.6% for suicidal ideation among sexual minority youth based on self-identification as lesbian, gay, or bisexual and as high as 15.0% for suicide attempts among sexual minority youth as indexed by sexual identity, including those unsure of their sexual identity. Of note, these values are not dissimilar to those observed for sexual minority youth in recent national YRBSS data.18,24
These findings speak to the need to prioritize screening of sexual minority youth for suicide risk in school settings. Given findings that 85.9% of suicidal youth have made a primary care visit in the past year but did not receive treatment of mental health care,25 with many making such visits in the past month alone,26 screening for suicidal thoughts and behaviors in primary care settings may be critical for addressing this clinical concern. Screening in such settings may be particularly effective for identifying suicidal sexual minority youth insofar as it may be a relatively comprehensive means of having clinical contact with this population without requiring self-disclosure of sexual orientation because concerns of stigma regarding such self-disclosure may exist.27 Furthermore, in cases in which adolescents do openly identify as a sexual minority individual, screening for suicidal risk in primary care settings appears particularly warranted given the high prevalence of suicidal ideation and behaviors in this population.
Although in the current study, we do not directly evaluate potential factors driving the persistent disparity in suicidal thoughts and behaviors, a potential explanation may be found in the minority stress model,27 according to which specific stress processes unique to sexual minority individuals (eg, experiencing prejudice, discrimination, victimization, rejection, nondisclosure of sexual minority status) confer added risk for negative mental health outcomes, such as suicide. The relevance of the minority stress model to suicide risk in sexual minority individuals has received empirical support.28,29 Additionally, it may be that currently available psychotherapeutic interventions and treatments are more effective at targeting general risk factors, but are less effective with risk involving sexual minority stress, and this may be, in part, driving the slower decline observed among sexual minority youth. Congruent with this possibility, certain sexual minority groups have reported being less positive about the treatment they received,30 which speaks to the need for interventions tailored to sexual minority populations.
Among the strengths of this study is our use of multiple indices of sexual orientation (ie, sexual identity, with and without those unsure of their sexual identity, and sexual behavior). The fact that essentially the same pattern of results was obtained with these difference indices suggests that the current findings are robust. Also important to mention is that responses were collected anonymously, which has been found to increase openness in disclosing of personally sensitive information, particularly relating to sexuality and violence in adolescents.31,32
The current study, however, is also not without its limitations. In particular, YRBSS data were collected from school-attending youth. Given that sexual minority status and mental health concerns are both associated with school nonattendance,33 sexual minority youth are likely underrepresented in this study, especially those with suicidal ideation and behavior. The current data may therefore provide an underestimate of the prevalence of suicide-related outcomes in sexual minority youth.
Additionally, the present data do not allow for direct inferences regarding causality. What factors, for example, may account for the decline in prevalence of suicide-related outcomes among sexual minority youth since 1995 and for the persistence in disparity relative to heterosexual peers in these outcomes? One possible explanation for the decrease in prevalence of these outcomes among sexual minority youth over time is the increasing societal acceptance of sexual minority individuals since the 1990s.34,35 Yet, this possibility admittedly provides an imperfect account of the current findings given that heterosexual youth have also experienced an overall decline in the prevalence of suicide-related outcomes since 1995, although with a plateau in the case of suicidal ideation and plans starting in 2007, and given that the rate of decline was significantly steeper among heterosexual youth for these 2 outcomes. Indeed, this pattern of findings is consistent with the view that the factors driving disparity in suicide-related outcomes persist. Identifying the factors associated with the persistence of disparity in suicidal ideation and behavior over time is therefore necessary for reducing the mental health burden of sexual minority youth. Risk factors for suicidal ideation and behavior specific to sexual minority individuals (eg, minority stress or victimization27,36) may be of particular relevance here and may be promising candidates for future study.
Furthermore, all sexual minority youth were combined to ensure adequately powered analyses. This reflects the challenge of conducting research on suicide-related outcomes with specific sexual minority groups and follows the common practice of previous studies,17,18 and there remains a need for research in this area to observe the distinction between these different populations given evidence that certain groups (eg, bisexual individuals) may be at greater risk for self-harm–related outcomes.30,37
Although, to our knowledge, data do not currently exist to assess temporal trends in suicide-related outcomes among sexual minority youth on a national level, it is worth noting that the trends in the current study are nonetheless similar to overall trends in the national YRBSS data, in which general decreases in suicidal ideation, plans, and attempts have been found in youth since 1991, albeit with increases rather than a leveling off in suicidal ideation and plans occurring since 2007 and 2009, respectively.38 The findings of the current study also stand in notable contrast, however, to national trends since 1999 of an increasing prevalence of suicide deaths in this age group.39 Therefore, a degree of caution should be taken regarding generalizing findings from the current study. Insofar as they are generalizable, however, these findings may be suggestive of the concerning possibility that although there has been a general decrease in suicidal ideation and behavior among youth, when adolescents in recent years do attempt suicide, they have taken to engaging in increasingly severe attempts (ie, increased case fatality ratio). If and why this may be the case is an important question warranting future investigation.
Conclusions
In our study, the prevalence of suicidal ideation, plans, and behaviors has generally declined among both sexual minority and heterosexual youth from 1995 to 2017. Nonetheless, disparities persist, and the prevalence of these outcomes remains markedly high among sexual minority youth. Prioritized monitoring of trends in risk for suicide-related outcomes and screening of suicidal thoughts and behaviors in primary care settings for this vulnerable population is warranted and may be an important step to reduce disparities in these outcomes.
Glossary
- APC
annual percent change
- YRBSS
Youth Risk Behavior Surveillance System
Footnotes
Dr Liu conceptualized and designed the study, conducted the analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Ms Walsh, Ms Sheehan, Ms Cheek, and Ms Carter contributed to interpretation of the data and drafting of the initial manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by the National Institute of Mental Health of the National Institutes of Health under awards R01MH101138, R01MH115905, and R21MH112055 as well as by an American Psychological Foundation Wayne F. Placek grant (to the first author). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPERS: Companions to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2019-1658 and www.pediatrics.org/cgi/doi/10.1542/peds.2019-4002.
References
- 1.Obedin-Maliver J, Goldsmith ES, Stewart L, et al. . Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306(9):971–977 [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press; 2011 [PubMed] [Google Scholar]
- 3.National Institutes of Health Sexual and gender minority populations in NIH-supported research. 2019. Available at: https://grants.nih.gov/grants/guide/notice-files/NOT-OD-19-139.html. Accessed July 3, 2019
- 4.National Action Alliance for Suicide Prevention Research Prioritization Task Force A Prioritized Research Agenda for Suicide Prevention: An Action Plan to Save Lives. Rockville, MD: National Institute of Mental Health and the Research Prioritization Task Force; 2014 [Google Scholar]
- 5.Haas AP, Eliason M, Mays VM, et al. . Suicide and suicide risk in lesbian, gay, bisexual, and transgender populations: review and recommendations. J Homosex. 2011;58(1):10–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Brien KHM, Liu RT, Putney JM, Burke TA, Aguinaldo LD. Suicide and Self-Injury in Gender and Sexual Minority Populations In: Smalley KB, Warren JC, Barefoot KN, eds. LGBT Health: Meeting the Needs of Gender and Sexual Minorities. New York, NY: Springer; 2018:181–198 [Google Scholar]
- 8.Miranda-Mendizábal A, Castellví P, Parés-Badell O, et al. . Sexual orientation and suicidal behaviour in adolescents and young adults: systematic review and meta-analysis. Br J Psychiatry. 2017;211(2):77–87 [DOI] [PubMed] [Google Scholar]
- 9.Hottes TS, Bogaert L, Rhodes AE, Brennan DJ, Gesink D. Lifetime prevalence of suicide attempts among sexual minority adults by study sampling strategies: a systematic review and meta-analysis. Am J Public Health. 2016;106(5):e1–e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institutes of Health The health of sexual and gender minority (SGM) populations (R01 clinical trial optional). 2017. Available at: https://grants.nih.gov/grants/guide/pa-files/PA-18-037.html. Accessed July 3, 2019
- 11.Savin-Williams RC. Who’s gay? Does it matter? Curr Dir Psychol Sci. 2006;15(1):40–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mustanski B, Liu RT. A longitudinal study of predictors of suicide attempts among lesbian, gay, bisexual, and transgender youth. Arch Sex Behav. 2013;42(3):437–448 [DOI] [PubMed] [Google Scholar]
- 13.Newcomb ME, Birkett M, Corliss HL, Mustanski B. Sexual orientation, gender, and racial differences in illicit drug use in a sample of US high school students. Am J Public Health. 2014;104(2):304–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brener ND, Kann L, Shanklin S, et al. ; Centers for Disease Control and Prevention (CDC) . Methodology of the Youth Risk Behavior Surveillance System–2013. MMWR Recomm Rep. 2013;62(RR):1–20 [PubMed] [Google Scholar]
- 15.Office of Data Management and Outcomes Assessment Massachusetts Youth Health Survey (MYHS). 2017. Available at: https://www.mass.gov/lists/massachusetts-youth-health-survey-myhs#methodology-. Accessed July 3, 2019
- 16.Stone DM, Luo F, Ouyang L, Lippy C, Hertz MF, Crosby AE. Sexual orientation and suicide ideation, plans, attempts, and medically serious attempts: evidence from local Youth Risk Behavior Surveys, 2001-2009. Am J Public Health. 2014;104(2):262–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raifman J, Moscoe E, Austin SB, Hatzenbuehler ML, Galea S. Association of state laws permitting denial of services to same-sex couples with mental distress in sexual minority adults: a difference-in-difference-in-differences analysis. JAMA Psychiatry. 2018;75(7):671–677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caputi TL, Smith D, Ayers JW. Suicide risk behaviors among sexual minority adolescents in the United States, 2015. JAMA. 2017;318(23):2349–2351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao Y, Montoro R, Igartua K, Thombs BD. Suicidal ideation and attempt among adolescents reporting “unsure” sexual identity or heterosexual identity plus same-sex attraction or behavior: forgotten groups? J Am Acad Child Adolesc Psychiatry. 2010;49(2):104–113 [DOI] [PubMed] [Google Scholar]
- 20.May A, Klonsky ED. Validity of suicidality items from the Youth Risk Behavior Survey in a high school sample. Assessment. 2011;18(3):379–381 [DOI] [PubMed] [Google Scholar]
- 21.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates [published correction appears in Stat Med. 2001;20(4):655]. Stat Med. 2000;19(3):335–351 [DOI] [PubMed] [Google Scholar]
- 22.Statistical Research and Applications Branch, National Cancer Institute Joinpoint Regression Program [computer program]. Version 4.7.0.0. Bethesda, MD: National Cancer Institute; 2019
- 23.van Belle G. Statistical Rules of Thumb, 2nd ed Hoboken, NJ: John Wiley & Sons, Inc; 2008 [Google Scholar]
- 24.Zaza S, Kann L, Barrios LC. Lesbian, gay, and bisexual adolescents: population estimate and prevalence of health behaviors. JAMA. 2016;316(22):2355–2356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCarty CA, Russo J, Grossman DC, et al. . Adolescents with suicidal ideation: health care use and functioning. Acad Pediatr. 2011;11(5):422–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Asarnow JR, Jaycox LH, Anderson M. Depression among youth in primary care models for delivering mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11(3):477–497, viii [DOI] [PubMed] [Google Scholar]
- 27.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mereish EH, Peters JR, Yen S. Minority stress and relational mechanisms of suicide among sexual minorities: subgroup differences in the associations between heterosexist victimization, shame, rejection sensitivity, and suicide risk. Suicide Life Threat Behav. 2019;49(2):547–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mongelli F, Perrone D, Balducci J, et al. . Minority stress and mental health among LGBT populations: an update on the evidence. Minerva Psichiatr. 2019;60(1):27–50 [Google Scholar]
- 30.Beard C, Kirakosian N, Silverman AL, Winer JP, Wadsworth LP, Björgvinsson T. Comparing treatment response between LGBQ and heterosexual individuals attending a CBT- and DBT-skills-based partial hospital. J Consult Clin Psychol. 2017;85(12):1171–1181 [DOI] [PubMed] [Google Scholar]
- 31.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873 [DOI] [PubMed] [Google Scholar]
- 32.Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull. 2007;133(5):859–883 [DOI] [PubMed] [Google Scholar]
- 33.Burton CM, Marshal MP, Chisolm DJ. School absenteeism and mental health among sexual minority youth and heterosexual youth. J Sch Psychol. 2014;52(1):37–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Newcomb ME, Mustanski B. Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: a meta-analysis. Arch Sex Behav. 2011;40(1):189–199 [DOI] [PubMed] [Google Scholar]
- 35.Savin-Williams RC. Then and now: recruitment, definition, diversity, and positive attributes of same-sex populations. Dev Psychol. 2008;44(1):135–138 [DOI] [PubMed] [Google Scholar]
- 36.Liu RT, Mustanski B. Suicidal ideation and self-harm in lesbian, gay, bisexual, and transgender youth. Am J Prev Med. 2012;42(3):221–228 [DOI] [PubMed] [Google Scholar]
- 37.Liu RT, Sheehan AE, Walsh RFL, Sanzari CM, Cheek SM, Hernandez EM. Prevalence and correlates of non-suicidal self-injury among lesbian, gay, bisexual, and transgender individuals: A systematic review and meta-analysis. Clinical Psychology Review. 2019;74:101783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention Trends in the prevalence of suicide–related behaviors. National YRBS: 1991–2017. 2018. Available at: https://www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/2017_suicide_trend_yrbs.pdf. Accessed July 3, 2019
- 39.Hedegaard H, Curtin SC, Warner M. Suicide mortality in the United States, 1999–2017. NCHS Data Brief. 2018;(330):1–8 [PubMed] [Google Scholar]