ABSTRACT
Aim
The aim of this paper is to present an interesting case of viral myocarditis complicated by sepsis, its sequelae, including multi-organ dysfunction syndrome, and the approach to manage it successfully.
Background
Viral myocarditis is an inflammatory disease of myocardium, often leading to residual heart disease. Commonly, dengue and Coxsackie B viruses are the causative agents. Patients usually present with dyspnea, fever, and signs of heart failure. A possibility of bacterial sepsis should not be overlooked, given similar presentations may occur.
Case description
A 21-year-old male presented with acute onset breathlessness, fever, chills, and severe neck pain. On a detailed workup, he was found to have features suggestive of viral myocarditis, bacterial sepsis, with bilateral pleural loculations, a posterior epidural spinal abscess. Elimination of infectious foci, along with a decision to stick to the ongoing antibiotics, instead of stepping up to the last available ones proved beneficial. Meticulous balance of diuretics and inotropes saved the patient's life from what turned out to be coxsackie myocarditis.
Conclusion
Here, we present the case of a young male who came in with congestive heart failure due to Coxsackie myocarditis and his condition complicated by severe sepsis.
Clinical significance
Up to 10% of the cases of coxsackie myocarditis progress to chronic dilated cardiomyopathy. The management is usually conservative, and antiviral agents have shown no role in speedy recovery. Elimination of infectious foci aggressively is of prime importance in the treatment of bacterial sepsis. A careful balance of inotropes, diuretics, and fluid management is needed to get the patient into remission in such cases.
How to cite this article
Morkar DN, Agarwal R, Patil RS. Coxsackie Myocarditis with Severe Methicillin-resistant Staphylococcus aureus Sepsis, Multi-organ Dysfunction Syndrome, and Posterior Epidural Spinal Abscess: A Case Report. Indian J Crit Care Med 2020;24(1):73–76.
Keywords: Coxsackie, Methicillin-resistant Staphylococcus aureus, Myocarditis, Sepsis
BACKGROUND
Myocarditis, an inflammatory disease of heart muscle, often results from an infection caused by a spectrum of viruses. Patients usually present with dyspnea, chest discomfort, or chest pain of acute onset. The insult can be directly caused by the virus, or the body's immune response can cause damage to cardiac myocytes.
There is a greater incidence of viral myocarditis in immunocompromised individuals, those with unhygienic habits, or poor living conditions. We present a case of a young individual who was found to have coxsackie myocarditis and had a complicated course in the hospital.
CASE DESCRIPTION
A 21-year-old male patient, from a village in rural Karnataka (India), presented to the ER with complaints of breathlessness since 1 day, acute onset, present at rest, progressive, associated with cough and scanty sputum. Patient had a history of fever for 4–5 days associated with chills and neck pain and was treated for the same in a teaching hospital near his hometown. He was informed that he has reduced cardiac function following the development of breathlessness and was referred to a higher center for further management. There was no history of rash or polyarthralgia. There was no history of alcohol consumption, exposure to a case of tuberculosis, and deaths in young age in the family. There was also no history of preexisting heart disease.
On examination, pulse rate was 160 bpm, blood pressure 80/52 mm Hg, and respiratory rate was 40/minute SpO2 78%. Patient was not febrile. Extremities were cold, and pulse was thready.
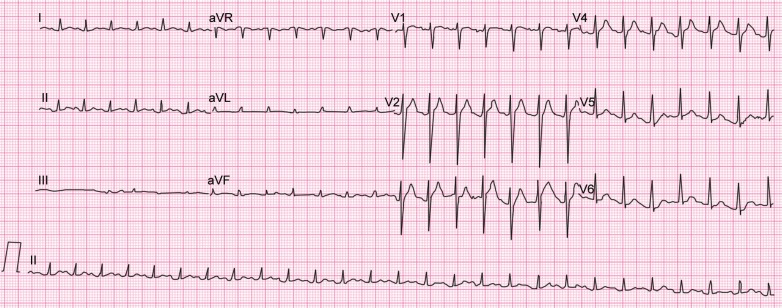
Coarse crackles were present in the bilateral infrascapular region, and basal air entry was reduced on both sides. Neck movements were very painful. No obvious sensory or motor deficits were seen. ECG revealed sinus tachycardia (Fig. 1).
Fig. 1.
ECG at admission
Patient was immediately administered 8 L/minute oxygen, inotropes, diuretics, low-dose aspirin, and atorvastatin. Empirical antibiotics were started after blood culture, and routine tests were performed. 2D-Echocardiogram showed a left ventricular ejection fraction of 20%. Chest X-ray revealed bilateral mild-to-moderate pleural effusion. Intravenous (IV) tramadol was administered in view of severe neck pain, and the presenting symptoms were all attributed to suspected viral infection, with a background of ongoing dengue epidemic in the region.
Lab results indicated bacterial sepsis, and dengue serology was negative (Table 1). Sequential organ failure assessment score was calculated to be 8. Total white blood cell (WBC) counts and serum (S.) creatinine levels were on an increasing trend, and the blood culture grew methicillin-resistant Staphylococcus aureus (MRSA) on day 3 of admission. Subsequently, IV vancomycin and linezolid were started according to a sensitivity report. Fever spikes persisted, accompanied by tachycardia and tachypnea.
Table 1.
Important laboratory investigations
| Lab reports | Day 1 | Day 2 | Day 3 | Day 10 | Day 15 | Day 20 |
|---|---|---|---|---|---|---|
| Hb (g/dL) | 12.5 | 9.6 | 7.7 | 9.0 | ||
| Platelets (/mm3) | 117,000 | 65,000 | 745,000 | 889,000 | 450,000 | |
| Total WBC (/mm3) | 5100 N-93, L-3 | 9600 | 16,900 | 37,400 | 19,100 | 11,100 |
| Peripheral smear | Neutrophilia with thrombocytopenia | Toxic granules seen | ||||
| S. creatinine (mg/dL) | 1.49 | 1.85 | 2.01 | 0.73 | 0.80 | |
| S. urea (mg/dL) | 66 | 32 | ||||
| Total bilirubin (mg/dL) | 1.43 | |||||
| D. bilirubin (mg/dL) | 1.05 | |||||
| Sodium (mEq/L) | 131 | 136 | ||||
| Potassium (mEq/L) | 4.41 | 3.43 | ||||
| Troponin T (ng/mL) | 0.12 | |||||
| CK-MB | 36 | |||||
| S. procalcitonin (ng/mL) | 82.49 | 2.48 | ||||
| S. lactate (mg/dL) | 23.5 | |||||
| Urine examination | Protein 1+, RBC-7, WBC-4 | |||||
| SGOT (IU/L) | 70 | |||||
| SGPT (IU/L) | 45 | |||||
| Total proteins (g/dL) | 5.2 | |||||
| Albumin (g/dL) | 2.7 g/dL | |||||
| A:G ratio | 1.1 | |||||
| INR | 1.94 | |||||
| PT | C-11.2s, T-21.4s | |||||
| Dengue serology | NS-1, IgG, IgM negative | |||||
| Widal test | Negative | |||||
| Malaria | Serology and smear negative | |||||
| Blood culture | MRSA |
Inotropes were tapered down by the sixth day of admission with blood pressure maintaining at 104/66 mm Hg. However, the total counts increased to 25,600/mm3. As the tachypnea was still persistent, the USG chest was done on day 6 that showed approximately 800 mL fluid on the left and 700 mL on the right side of the chest with septations. It was decided to drain the fluid by placing an intercostal tube on the left side. Pleural fluid was turbid, dark-colored, with pus cells but not remarkable for tuberculosis or malignancy.
Patient developed icterus, liver functions were found to be deranged. Serum creatinine was returning to normal and found to be 1.07 mg/dL on day 7. In view of continuous fever and tachypnea, netilmicin (according to culture sensitivity) was added. Intercostal tube was removed once the drain reduced to less than 50 mL by day 8.
Meanwhile, the neck pain had increased, but still no neurological deficits were present. MRI spine (Fig. 2) on day 8 showed a posterior epidural abscess, extending along the cervical, and visualized dorsal spine, maximum width 4.5 mm at the level of C4. Neurosurgeon's opinion was taken; however, it was decided not to drain the abscess and wait for a response to the ongoing antibiotics. Intravenous tramadol was administered for pain relief.
Fig. 2.

MRI (spine) showing posterior epidural abscess with maximum width at the level of C4 (4.5 mm)
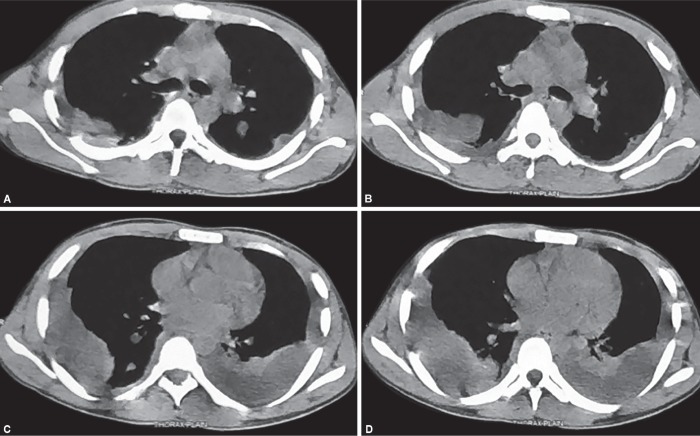
CT scan of thorax (Fig. 3) on day 10 revealed multiple loculated pleural collections, soft tissue densities in both lungs, and moderate effusion in bilateral pleura. Intercostal tube was put on the other side, to try and remove possible infectious foci. Visible improvement in tachypnea was seen by day 15.
Figs 3A to D.
CT (thorax) showing multiple loculated pleural collections, soft tissue densities in both lungs, and moderate effusion in bilateral pleura
Antibiotics were continued, and total counts started normalizing (11,100/mm3 on day 20), and fever spikes reduced. Repeat echo on day 20 showed improved left ventricle ejection fraction (60%).
Meanwhile, incentive spirometry with chest physiotherapy helped in improving lung function, and patient could maintain saturation without oxygen support.
Neck pain had reduced, and repeat MRI spine on day 22 showed reduced thickness of epidural abscess.
Initial IgM coxsackie investigation was reported as strong positive on day 22, and hence a certain diagnosis was established.
Patient was given IV antibiotics for a total of 6 weeks and was discharged in a state of good health.
DISCUSSION
Coxsackie B viruses are members of the human enterovirus B cluster in the family Picornaviridae. They are nonenveloped viruses with a single-stranded RNA genome of positive-strand orientation that acts as a messenger RNA upon infection. Coxsackie B viruses are best known as cytolytic viruses that kill the cells they infect.1 Coxsackie B3 and B4 viruses are the serotypes most commonly associated with myocarditis.
Myocarditis, an inflammatory disease of heart muscle, often results from an infection caused by a spectrum of viruses. The clinical spectrum of viral cardiomyopathy can be classified as fulminant, acute, or chronic. In the first phase, acutely infected cardiac myocytes die and initiate the activation of innate immune response with the involvement of interferon-gamma, natural killer cells, and nitric oxide. Although most patients recover from this infection, a small subset becomes victims to an adaptive immune response causing antibody-mediated damage to cardiac myocytes.
The immune responses then get downregulated in the third phase and fibrosis ensues in the myocardium. The inflammatory processes may persist and lead to ventricular dysfunction.2
Because patients generally present days to weeks after the initial viral infection, antiviral therapy has limited applicability in patients with acute viral myocarditis. The initial evaluation should include electrocardiography, echocardiography, and often contrast-enhanced cardiac MRI. If ischemia is suspected, patient should usually undergo coronary angiography.
Endomyocardial biopsies are usually not indicated unless tachyarrhythmias suggest possible sarcoidosis or giant cell myocarditis. Dallas criteria are used on biopsy to diagnose myocarditis.3
This case also highlights the need to eliminate infectious foci in order to aggressively clear the S. aureus infection as was tried by draining pleural collections. High-dose vancomycin has a good cerebrospinal fluid penetration and further bactericidal activity in epidural abscesses.4 The patient did not have established risk factors for epidural abscess recurrence and hence indicated a good prognosis.5
In this case, the patient was immediately put on inotropes and all supportive cardiac measures, and coxsackie viral IgM antibody was sent for, based on clinical suspicion. The disease was complicated by MRSA sepsis that needed further intervention to prevent accentuation of the preexisting illness. It is worthwhile to note that treating doctors stuck with the antibiotics going on, and a little patience proved beneficial to the patient.
Conservative management with supportive cardiac measures was helpful in getting the patient out of heart failure, and the patient was discharged after full antibiotic course in a healthy condition with ejection fraction 60%.
CONCLUSION
The patient recovered completely following 6 weeks of antibiotics. Coxsackie viral myocarditis should be suspected in such presentations, after ruling out more common causes of heart failure of likely infectious etiology. An aggressive approach for removal of infectious foci along with the use of antibiotics the causative organism is most sensitive to is advisable.
CLINICAL SIGNIFICANCE
Up to 10% of the cases of Coxsackie myocarditis progress to chronic dilated cardiomyopathy. The management is usually conservative, and antiviral agents have shown no role in speedy recovery. Elimination of infectious foci aggressively is of prime importance in the treatment of bacterial sepsis. A decision to not draining the posterior epidural abscess is where the aggressive approach was limited in this case, as it could have proven to be more harmful than beneficial. A careful balance of inotropes, diuretics, and fluid management with the appropriate antibiotics for an apt duration is needed to get the patient into remission in such cases.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Tam PE. Coxsackie virus myocarditis: Interplay between virus and host in the pathogenesis of heart disease. Viral Immunol. 2006;19(2):133–146. doi: 10.1089/vim.2006.19.133. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Schultz JC, Hilliard AA, Cooper LT, Rihal CS. Diagnosis and treatment of viral myocarditis. Mayo Clin Proc. 2009;84(11):1001–1009. doi: 10.1016/S0025-6196(11)60670-8. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lakdawala NK, Stevenson LW, Loscalzo J. Harrison's Principles of Internal Medicine, 20th ed., pp. 1783–1787. ch. 254.
- 4.Ricard JD, Wolff M, Lacherade JC, Mourvillier B, Hidri N, Barnaud G, et al. Levels of vancomycin in cerebrospinal fluid of adult patients receiving adjunctive corticosteroids to treat pneumococcal meningitis: a prospective multicenter observational study. Clin Infect Dis. 2007;44(2):250–255. doi: 10.1086/510390. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Shah AA, Yang H, Ogink PT, Schwab JH. Independent predictors of spinal epidural abscess recurrence. Spine J. 2018;18(10):1837–1844. doi: 10.1016/j.spinee.2018.03.023. DOI: [DOI] [PubMed] [Google Scholar]