Abstract
Cochrane is an international non-profit organization established in 1993 to produce and disseminate high quality and unbiased systematic reviews of evidence on health care interventions. At the forefront of systematic review methodology, Cochrane is generally accepted to be among the most carefully prepared and rigorous sources of systematic review evidence. There are numerous Cochrane reviews on nonpharmacologic interventions for pain and multiple Cochrane reviews evaluating acupuncture therapy in pain conditions. But how complete and up to date are those reviews relative to other rigorous systematic reviews with meta-analyses of acupuncture therapy for pain published in the literature? In this ‘snapshot’ overview, we found 22 relevant Cochrane reviews, some concluding that acupuncture therapy is probably useful for treating specific pain conditions. However, many of the conditions for which acupuncture is most commonly used are either not represented in Cochrane reviews or the existing Cochrane reviews are seriously outdated and do not reflect current evidence. This creates confusion with the risks of adverse effects and addiction liability associated with pain medications, the prevalence of chronic pain, the ongoing opioid epidemic and the need for evidence-based options for pain as part of comprehensive pain care. Clinicians and patients want clarification on safe and effective options to treat pain. Issues involving reviewed trials’ inadequate use of sham comparators, of acupuncture as a complex intervention with interactive components and a shift in research focus from efficacy trials to real-world pragmatic trials are discussed in relation to updating Cochrane reviews of acupuncture therapy for pain.
Background
The prevalence of chronic pain problems in the general adult U.S. population is high; estimates have ranged from 11% to 47% in recent large surveys depending on the specific sample, with a documented association between pain and impairment in physical and psychological functioning and lost work productivity.1 Recent estimates for the US cost of pain care range from US$560 to US$635 billion annually2 This exceeds the annual expenditures for the nation’s priority health conditions (heart disease, cancer and diabetes) combined.3 Low back and neck pain, osteoarthritis (OA) and headache are the most common pain conditions in the United States and are leading global causes of disability in 2015 in most countries.4
This prevalence of pain is set in the context of the ongoing prescription opioid epidemic that continues to claim 130 lives a day in the U.S, where nearly 80% of heroin users reported misusing prescription opioids prior to heroin.5 The probability of long-term opioid use increases after as little as five days of prescribed opioids as the initial treatment of pain.6 While not addictive, nonsteroidal anti-inflammatory medications (NSAIDs) commonly used for pain carry risks of adverse events including gastrointestinal (GI) symptoms like nausea, abdominal pain, stroke, heart attack, renal failure and GI complications including acute and chronic bleeding as well as delaying healing of injury.7,8 There are 16,500 deaths annually from NSAID-associated GI complications among rheumatoid arthritis (RA) and OA patients alone;9,10 and as of the year 2000, 25% of all reported adverse drug reactions were attributed to prescription NSAID use.11
In response to the risks of pharmacological treatments for both acute and chronic pain, and more specifically to the ongoing opioid crisis, nonpharmacologic pain approaches are recommended as a first line of care by the Centers for Disease Control and Prevention (CDC)12 and the U.S. Food and Drug Administration (FDA),13 with acupuncture listed as a first line option by the Army Surgeon General Pain Task Force,14 and the American College of Physicians (ACP),15 and as part of comprehensive pain care1 by the U.S Agency for Health Care Research and Quality (AHRQ),16 National Institutes of Health (NIH),17 the National Academy of Medicine (NAM, formerly the Institute of Medicine IOM)8 and the Joint Commission (TJC).18,19 Nonpharmacologic therapies generally and acupuncture specifically have very low risk profiles. The NIH Consensus Statement on Acupuncture published in 1998 found that ‘the incidence of adverse effects is substantially lower than that of many drugs or other accepted procedures for the same conditions’.20 Systematic reviews and surveys of adverse events have clarified that acupuncture is safe when performed by appropriately trained practitioners 21–27 with infrequent minor side effects such as feeling relaxed, elated, tired, or having point sensation or itching24 and rare serious complications such as infection or pulmonary embolism directly related to insufficient training.25,26 Abbreviated training raises the risk of harms. 25,28–30 Clinicians and patients want safe and effective options to treat pain and rely on organizational guidelines but also, on information provided in published trials and systematic reviews including those provided by Cochrane.
The international Cochrane collaboration was established in 1993 as a non-profit organization focused on producing and disseminating high quality and unbiased systematic reviews of evidence on health care interventions. Cochrane has been in the forefront of systematic review methodology since its founding, and it is generally accepted that Cochrane reviews of randomized trials are among the most carefully prepared and rigorous sources of systematic review evidence. Cochrane reviews are designed to be regularly updated when new evidence becomes available, and they are therefore ideally not only high quality but also up to date. Finally, Cochrane does not accept commercial or conflicted funding, in order that their work may be unbiased and trustworthy. The majority of the organizational funding is obtained from governmental or other nonprofit sources and from subscriptions to the online Cochrane Library, which contains all published Cochrane reviews.
Cochrane reviews cover diverse medical interventions and a wide range of medical conditions. There are numerous Cochrane reviews on nonpharmacologic interventions for acute or chronic pain, and Cochrane has published multiple reviews of trials evaluating acupuncture therapy in pain conditions. The abstracts and plain language summaries from Cochrane reviews are freely available to the public without any need for subscriptions. Clinicians and patients who consider Cochrane to be a reliable source of up-to-date and unbiased information on the effectiveness of interventions may refer to Cochrane reviews for guidance on acupuncture and related therapies for pain. The objective of this project is to provide an overview or ‘snapshot’ of the current Cochrane review evidence on acupuncture therapy for acute or chronic pain, to see what information on effectiveness is available through Cochrane and how up to date, complete and appropriate this information is.
Methods
One author (LSW) searched the Cochrane Database of Systematic Reviews for all completed reviews with both ‘acupuncture’ and ‘pain’ in title, abstract, or keywords, then screened the retrieved records to identify current systematic reviews of acupuncture for pain. To focus the snapshot on pain, only reviews in which pain was a primary symptom of the condition, for example, osteoarthritis) and/or pain was a primary outcome chosen by the authors as in, for example, chronic kidney disease) were included. All types of acupuncture, including needle acupuncture, laser acupuncture, and electroacupuncture, administered anywhere on the body according to any principles, were included. However, reviews focused solely on TENS were excluded, even if the reviews contained some trials of TENS administered to acupuncture points. Overviews, which summarize multiple Cochrane reviews, were excluded in favor of the individual reviews focused on acupuncture specifically, and withdrawn or superseded reviews were also excluded.
For each included review, one author (LSW) extracted the topic condition and a summary of the author conclusions regarding the effectiveness of acupuncture for pain in that condition. Cochrane review authors have increasingly been encouraged to incorporate explicit evaluations of quality or certainty for each outcome when expressing their conclusions.31,32 Evaluations of certainty for outcomes from systematic reviews in Cochrane reviews are based upon the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework (gradeworkinggroup.org) and include levels of high, moderate, low or very low certainty. Five factors are involved in assessing the certainty of evidence from randomized trials: 1) the risk of bias in included studies; 2) the heterogeneity between included effect estimates; 3) the indirectness of available evidence; 4) the sparseness or imprecision of the evidence; and 5) any strong suspicions of publication bias. Although explicit statements of certainty in estimates of effectiveness are not consistently present in recent Cochrane reviews and are largely missing from earlier reviews, we distinguished to the best of our ability between conclusions based explicitly or implicitly on evidence of overall high or moderate certainty and statements based on evidence of overall low or very low certainty. We then presented the conclusions using suggested terms for presenting different levels of certainty in plain language.33 For example, when an estimate of effectiveness is considered to be moderately certain, this is expressed by stating that the intervention ‘probably’ improves the outcome, while low certainty corresponds to a statement that the intervention ‘may’ improve the outcome, and very low certainty leads to a statement that the evidence is ‘uncertain’. The citation, topic condition, and summary findings on acupuncture for pain were then entered into a table in reverse date order of review publication.
Results
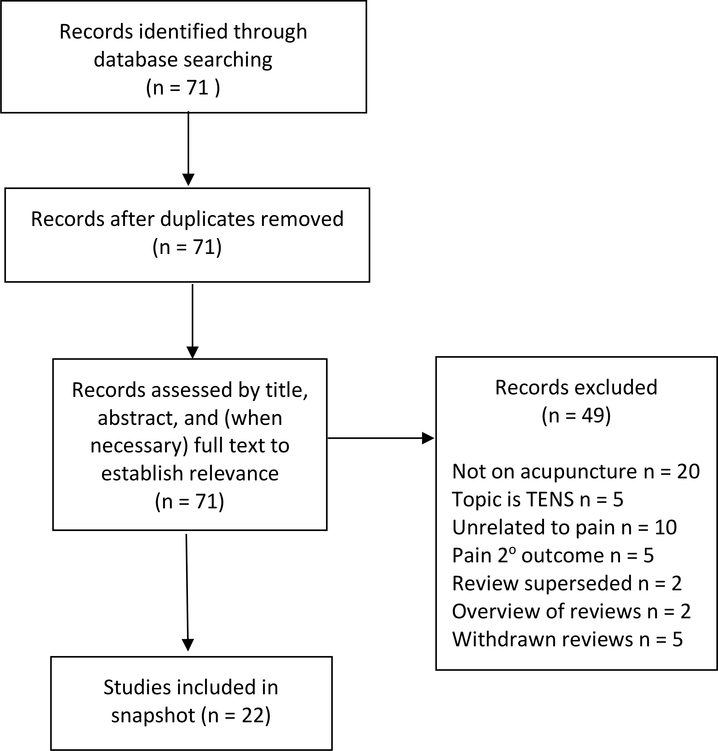
The search of CDSR retrieved 71 reviews, of which 49 were excluded. Most of the excluded reviews were either unrelated to acupuncture or to pain as a primary outcome. Two reviews had been partially superseded by more relevant reviews. For example, the 2003 review of non-surgical interventions for carpal tunnel syndrome included acupuncture but this was superseded by a 2018 review focused on acupuncture for carpal tunnel syndrome), two reviews were overviews of multiple Cochrane reviews, and five reviews were withdrawn by the authors. A total of 22 reviews were included in this snapshot. See Figure 1 for details of the search and selection process.
Figure 1.
Search and Selection Process.
The included reviews focus on musculoskeletal conditions including back pain,34,35 elbow pain,36 shoulder pain,37 and OA,38,39 fibromyalgia40 and RA41 as well as other pain conditions ranging from cancer pain42 to pain during oocyte retrieval.43 Eight reviews contained one or more author conclusions that reflected the presence of high or moderate-certainty evidence, and these statements included both positive and negative assessments of acupuncture. Almost all reviews stated that there was uncertainty about the effectiveness of acupuncture with regard to one or more comparisons, and the primary reason given for this uncertainty was the limited number and size of available trials. Four reviews were published in 2018 and overall 13 reviews were published in the last five years, however five reviews are 12 or more years old, including reviews on RA, low back pain, shoulder pain and tennis elbow. Table 1 lists each review in date order, with most recent reviews first, and presents the review authors’ conclusions on the effectiveness of acupuncture for pain. Statements that appeared to reflect author assessments that the evidence was of high or moderate certainty are given in bold type.
Table 1.
Cochrane reviews assessing effectiveness of acupuncture therapy for pain
| Citation | Condition(s) | Author conclusions* |
|---|---|---|
| Choi 2018 68 | Carpal tunnel syndrome | It is uncertain whether acupuncture is helpful for pain or overall symptom improvement in this condition. |
| Kwan 2018 43 | Pain during oocyte retrieval | It is uncertain whether adding different types of acupuncture to other forms of analgesia is associated with greater or lesser pain. |
| Franco 2018 69 | Chronic prostatitis / chronic pelvic pain | There is probably a clinically relevant reduction in prostatitis symptoms for acupuncture compared with sham acupuncture. Compared to standard medical therapy, acupuncture may lead to greater relief in prostatitis symptoms. |
| Manheimer 201839 | Hip osteoarthritis | There is probably little or no difference in pain between acupuncture and sham acupuncture. Acupuncture may improve pain when added to routine care. It is uncertain whether acupuncture improves pain when added to patient education or is better for pain than NSAIDs or advice plus exercise. |
| Ju 201770 | Neuropathic pain | It is uncertain whether acupuncture is better for pain than sham acupuncture or active treatments (comparator inositol). It is also uncertain whether acupuncture improves pain when added to active treatments. |
| Kim 2016 71 | Chronic kidney disease | None of the included studies reported on pain. |
| Linde 2016a 72 | Tension headache (prevention) | Acupuncture probably reduces headache frequency compared to usual care and reduces headache days slightly when compared to sham. It is uncertain whether acupuncture is more effective than other interventions. |
| Linde 2016b 62 | Migraine (prevention) | Acupuncture probably reduces headache frequency compared to usual care or to sham. Acupuncture is probably as effective as treatment with prophylactic drugs in the short term. |
| Mangesi 2016 73 | Breast engorgement during lactation | It is uncertain whether acupuncture or acupressure are better for pain than usual care (oxytocin spray or hot and cold compresses). |
| Smith 2016 74 | Dysmenorrhea | Findings for acupuncture compared to sham or placebo were inconsistent. Acupuncture may be better than no treatment or an active treatment such as an NSAID. Acupressure may be better than sham, but it is uncertain whether it is better than no treatment or NSAIDs. |
| Liddle 2015 34 | Low back and pelvic pain during pregnancy | There may be little or no difference in pelvic pain with acupuncture plus usual prenatal care compared to sham or placebo acupuncture plus usual prenatal care. Acupuncture plus usual care is probably more effective than stabilizing exercises plus usual care or usual prenatal care alone, and acupuncture may be better than physiotherapy. For mixed populations of low back and pelvic pain, acupuncture plus usual prenatal care may be more effective than sham or placebo acupuncture plus usual prenatal care, and acupuncture plus usual care may be better than individual physiotherapy plus usual prenatal care. |
| Paley 201542 | Cancer-related pain | Acupuncture may be more effective for pain relief in cancer than either sham treatment or medications. |
| Boldt 2014 75 | Chronic pain from spinal cord injury | It is uncertain whether acupuncture is better than either sham acupuncture or Trager treatment. |
| Deare 2013 40 | Fibromyalgia | There is probably no difference between acupuncture and sham acupuncture at up to one month after treatment, however acupuncture may be better than no acupuncture or amitriptyline. Acupuncture plus standard therapy (tricyclic antidepressants and exercise) is probably better than standard therapy alone. |
| Smith 2011 76 | Pain during labor | There may be no difference in pain between treatment with acupuncture and sham acupuncture, however true acupuncture may have resulted in greater patient satisfaction with pain relief. There may be no difference in either pain or patient satisfaction with pain relief between acupuncture and standard care. Acupuncture may be more effective for pain than no treatment. |
| Zhu 2011 77 | Endometriosis | Because of limited good-quality evidence, it is uncertain whether acupuncture is better than Chinese herbal medicine for pain. |
| Manheimer 2010 78 | Peripheral joint osteoarthritis (knee, hip or hand) | Acupuncture may be slightly better than sham acupuncture for pain. Acupuncture is probably more effective than no acupuncture (waiting list) or an education intervention. There may be no difference in pain between acupuncture and exercise interventions, or between acupuncture added to exercise compared to exercise alone.** |
| Verhagen 2007 79 | Whiplash injuries | Based on one small study there may be no difference between acupuncture and sham or placebo treatment. |
| Casimiro 2005 41 | Rheumatoid arthritis | It is uncertain whether acupuncture is better than sham or placebo acupuncture. |
| Furlan 2005 35 | Low back pain | For acute low back pain, there is probably no difference between acupuncture and sham acupuncture or acupuncture and Naproxen. There is no evidence on acupuncture versus no treatment. For chronic low back pain, acupuncture may be better than sham acupuncture at short term, but it is uncertain whether acupuncture is better than sham acupuncture at intermediate term, and acupuncture is probably no better than sham acupuncture at long term. Acupuncture may not be more effective than other active treatments, but it may be slightly more effective for pain when added to other treatments than those other treatments alone. |
| Green 2005 37 | Shoulder pain | It is uncertain whether acupuncture is better than sham acupuncture, corticosteroid injection, ultrasound, or Trager treatment for pain. Acupuncture may be less effective than stellate ganglion block and suprascapular nerve block. Acupuncture plus mobilization may not be better than mobilization alone but acupuncture plus exercise may be better than exercise alone in improving a composite measure of pain, range of motion and functioning. |
| Green 2002 36 | Lateral elbow pain (tennis elbow) | Acupuncture may be better than sham or placebo acupuncture at short term but there may be no difference at 3 months or longer. There may be no difference between acupuncture plus Vitamin B12 injection and Vitamin B12 injection alone. |
Author conclusions expressing high or moderate certainty are in bolded text.
These findings are for peripheral joint osteoarthritis overall. Note that findings for hip osteoarthritis have been updated in Manheimer 2018.
Discussion
There are multiple Cochrane reviews on acupuncture therapy for pain currently available in the Cochrane Library. Recent Cochrane reviews on this topic have concluded that acupuncture is probably beneficial for chronic prostatitis and useful in the treatment or prevention of recurrent migraines and tension headaches. Some earlier Cochrane reviews conclude that acupuncture may be useful as an adjunctive treatment in conditions such as fibromyalgia or in low back and pelvic pain during pregnancy. However, many of the conditions for which acupuncture is most commonly used, including knee OA, RA, back pain and neck pain, are either not represented in Cochrane reviews or present only in reviews that are a decade or more old. For real-world comparisons such as acupuncture compared to standard treatments or acupuncture as an adjunct to other active treatments, there are many reviews in which authors support that acupuncture may be a valuable approach to treating pain. The primary limitation of the evidence base in Cochrane reviews is described as a need for additional high-quality trials.
Aside from the needed review updates and conduct of further high-quality trials in specific conditions we suggest there are several factors that may contribute to the lack of firm conclusion in many of the dated Cochrane systematic reviews on acupuncture therapy for pain. Early RCTs designs were based in pharmacologic study design of a simple intervention compared to a simple placebo or sham for a more narrowly defined cohort of subjects. Sham or placebo arms involved either insertion of acupuncture needles or forms of surface stimulation meant to mimic needle insertion. However, research recognized these control comparators to be biologically active,44 i.e., not inert controls, biasing the outcomes from true acupuncture towards the null.45 The controls were, in effect, a kind of acupuncture and those trials were essentially comparisons of kinds or even dosages of treatment, not treatment and inert comparator as with a placebo pill.46
Researchers challenged these trial designs as limited when assessing a complex intervention such as acupuncture therapy wherein clinical virtuosity is based in an ability to be responsive to different presentations of similar conditions and as conditions evolve or respond over time.47 To address this, researchers have adapted the Medical Research Councils guidance on developing and evaluating complex interventions that have interacting components.48 Manualization describes one such adaptation and is engaged as a means of promoting standardization as well as flexibility in acupuncture research49 for trials on depression,50 stroke51 and chronic pain.52–54 The move toward more complex and responsive acupuncture research protocols represents study closer to real-world practice.54 The development of those acupuncture research protocols and manuals typically engages the ‘Delphi technique’, developed by the Rand Corporation in the 1950s, a widely used and accepted method for achieving convergence of opinion concerning real-world knowledge solicited from experts within certain topic areas.55
Future Cochrane reviews will need to approach acupuncture as a complex intervention, and not as a simple intervention that can easily be standardized and compared to an equally simple placebo or sham procedure. Acknowledging acupuncture therapy as a complex intervention will also require revisiting the importance of blinding. Lack of blinding is a primary reason for downgrading the Cochrane evidence on acupuncture versus sham or non-sham comparators. However, blinding practitioners and patients is a challenge in any complex interventions with interacting components.56 The importance of blinding patients and practitioners when comparing acupuncture to controls should be reconsidered.
In fact the emphasis on blinded placebo efficacy RCTs for interventions is shifting. Classical efficacy trials test interventions against a placebo using rigid study protocols and minimal variation in a highly defined and carefully selected population. In 17 years, according the NIH Collaboratory, only 14% of research findings from all efficacy RCTs have led to widespread change in clinical care.57,58 Pragmatic clinical trials are performed in real-world clinical settings with highly generalizable populations to generate actionable clinical evidence at a fraction of the typical cost/time needed to conduct a traditional clinical trial.58,59 Pragmatic clinical trials are part of the NIH’s vision for bridging the gap between research and care,59,60 and are also supported through initiatives at the Center for Medicare & Medicaid, the Agency for Healthcare Research and Quality, the Patient Centered Outcomes Research Institute (PCORI), Practice-Based Research Networks (PBRNs) and community-based participatory research initiatives across the Federal government.61
Finally, a primary component to downgrading of evidence in some of the Cochrane reviews is imprecision based on not enough trials, even if the trials reviewed are sound. This trend is shifting as more trials are published and reviews are updated. The Cochrane reviews with conclusions supporting the efficacy and effectiveness of acupuncture-related interventions for pain, such as the Linde et al 2016 reviews on acupuncture for migraine62 and tension headache,63 include multiple trials with thousands of participants. These reviews are consistent with the Vickers et al. updated large individual patient data meta-analysis of 39 trials and over 20,000 patients evaluating acupuncture for nonspecific musculoskeletal pain, including of the neck and back, OA, chronic headache or shoulder pain.64 Main outcome measures for Vickers et al. were pain and function: acupuncture was found superior to sham as well as to no acupuncture for each pain condition. There was also clear evidence that the effects of acupuncture persist over time with only a small decrease, approximately 15%, in treatment effect at 1 year, in part due to increased self-efficacy that is an associated outcome of acupuncture care.65 This meta-analysis also confirmed smaller effects sizes for sham-controlled trials that used a penetrating needle for sham, and for trials that had high intensity of intervention in the control arm. Additionally, trial data clarified that effective dosage of acupuncture therapy, i.e. number of needle sites (6–20) and number of sessions (8–15 weekly), were associated with better outcomes.64,66
Based on the precision of this large meta-analysis, the authors conclude acupuncture is effective for the treatment of chronic musculoskeletal, headache, and osteoarthritis pain. Treatment effects of acupuncture persist over time and cannot be explained solely in terms of placebo effects. When updates of the Cochrane reviews on back pain, knee OA, and neck pain are published within the next 1–2 years we will observe whether their conclusions are consistent with Vickers et al., but we do not need to wait for these review updates to agree, per the recommendations of multiple governmental organizations and guidelines producers, the CDC, FDA, the Army Surgeon General Pain Task Force, ACP, AHRQ, NIH, NAM and TJC, that referral for a course of acupuncture treatment is a reasonable option for a patient with chronic pain.64
A very recent analysis of the same data-set to identify possible moderators on the effect of acupuncture found only baseline severity of pain moderated treatment effect, wherein patients reporting more severe pain at baseline experience more benefit from acupuncture compared to either sham-control or non-acupuncture control.67 Therefore acupuncture is not only an important referral option for chronic pain but even for severe chronic pain.
One limitation of the current ‘snapshot’ is that the summary of author conclusions was extracted by a single author. Many Cochrane reviews are still lacking a transparent assessment and standard presentation of certainty for each outcome, and judgement is frequently required to interpret the author conclusions. The recent other large data set meta-analyses papers help to contextualize the current state of Cochrane reviews for conditions often treated with acupuncture like musculoskeletal pain, that are either missing or are seriously outdated and in need of updating, or where author conclusions are currently uncertain or unclear. And, for example, updated Cochrane reviews of acupuncture for chronic low back pain, acupuncture for knee osteoarthritis and acupuncture for chronic neck pain are in progress.
Conclusion
Current Cochrane review evidence on acupuncture therapy for pain is promising for some conditions, but inadequate or outdated for other conditions. In this term of the ongoing opioid epidemic, with the risks of adverse effects and addiction liability associated with pain medications, and the need for evidence-based options for pain as part of comprehensive pain care, acupuncture therapy has been shown by other research to be safe and effective for chronic pain and a viable referral option. Future Cochrane reviews should assist clinicians and patients in weighing the evidence on acupuncture therapy compared to other interventions as applied to specific pain conditions. Ongoing research and updated reviews, including Cochrane reviews, will assist clinicians and patients in not only weighing the relevant evidence as it is updated but in the features of research that will continue to clarify the dosage and frequency of interventions like acupuncture therapy as a stand-alone treatment for pain and as part of comprehensive pain care, combined with medicine and other therapies, for specific pain conditions.
Acknowledgments
L. Susan Wieland was funded by grant no. R24 AT001293 from the National Center for Complementary and Integrative Health (NCCIH) of the US National Institutes of Health (NIH). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NCCIH or the NIH.
References
- 1.Tick H, Nielsen A, Pelletier KR, et al. Evidence-based Nonpharmacologic Strategies for Comprehensive Pain Care: The Consortium Pain Task Force White Paper. Explore (NY). 2018;14(3):177–211. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine, Committee on Advancing Pain Research, Care and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. [PubMed] [Google Scholar]
- 3.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724. [DOI] [PubMed] [Google Scholar]
- 4.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.hhs.gov Help, resources and information: national opioids crisis; the opioid epidemic in numbers. 2018; https://www.hhs.gov/opioids/ Accessed January 6, 2019.
- 6.Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use - United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manchikanti L, Kaye AM, Knezevic NN, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician. 2017;20(2s):S3–s92. [PubMed] [Google Scholar]
- 8.National Academies of Sciences Engineering and Medicine. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use (2017). Washington, DC: The National Academies Press. doi: 10.17226/24781; 2017. [DOI] [PubMed] [Google Scholar]
- 9.Singh G, Triadafilopoulos G. Epidemiology of NSAID induced gastrointestinal complications. J Rheumatol Suppl. 1999;56:18–24. [PubMed] [Google Scholar]
- 10.Singh G, Ramey DR, Morfeld D, Shi H, Hatoum HT, Fries JF. Gastrointestinal tract complications of nonsteroidal anti-inflammatory drug treatment in rheumatoid arthritis. A prospective observational cohort study. Arch Intern Med. 1996;156(14):1530–1536. [PubMed] [Google Scholar]
- 11.Singh G Gastrointestinal complications of prescription and over-the-counter nonsteroidal anti-inflammatory drugs: a view from the ARAMIS database. Arthritis, Rheumatism, and Aging Medical Information System. Am J Ther. 2000;7(2):115–121. [DOI] [PubMed] [Google Scholar]
- 12.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315(15):1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Food and Drug Administration. Introduction FDA’s Opioid Analgesic REMS Education Blueprint for Health Care Providers Involved in the Treatment and Monitoring of Patients with Pain (January 2018). 2018; https://www.fda.gov/media/99496/download. Accessed June 10, 2019, 2019.
- 14.Office of the Army Surgeon General. Pain Management Task Force Final Report May 2010. 2010; http://www.dvcipm.org/site/assets/files/1070/pain-task-force-final-report-may-2010.pdf Accessed May 24, 2017.
- 15.Qaseem A, Wilt TJ, McLean RM, Forciea M, Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. [DOI] [PubMed] [Google Scholar]
- 16.Skelly AC, Chou R, Dettori JR, et al. AHRQ Comparative Effectiveness Reviews. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018. [PubMed] [Google Scholar]
- 17.Nahin RL, Boineau R, Khalsa PS, Stussman BJ, Weber WJ. Evidence-based evaluation of complementary health approaches for pain management in the United States. Mayo Clin Proc. 2016;91(9):1292–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Joint Commission. Clarification of the pain management standard. 2015; https://www.jointcommission.org/assets/1/18/Clarification_of_the_Pain_Management__Standard.pdf. Accessed May 22, 2019.
- 19.Joint Commission enhances pain assessment and management requirements for accredited hospitals. 2017; https://www.jointcommission.org/assets/1/18/Joint_Commission_Enhances_Pain_Assessment_and_Management_Requirements_for_Accredited_Hospitals1.PDF Accessed May 22, 2019.
- 20.NIH Consensus Conference. Acupuncture. JAMA. 1998;280(17):1518–1524. [PubMed] [Google Scholar]
- 21.Bergqvist D Vascular injuries caused by acupuncture. A systematic review. Int Angiol. 2013;32(1):1–8. [PubMed] [Google Scholar]
- 22.Ernst E, White AR. Prospective studies of the safety of acupuncture: a systematic review. Am J Med. 2001;110(6):481–485. [DOI] [PubMed] [Google Scholar]
- 23.MacPherson H, Thomas K, Walters S, Fitter M. A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional acupuncturists. Acupunct Med. 2001;19(2):93–102. [DOI] [PubMed] [Google Scholar]
- 24.MacPherson H, Thomas K. Short term reactions to acupuncture--a cross-sectional survey of patient reports. Acupunct Med. 2005;23(3):112–120. [DOI] [PubMed] [Google Scholar]
- 25.White A A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22(3):122–133. [DOI] [PubMed] [Google Scholar]
- 26.Yamashita H, Tsukayama H, White AR, Tanno Y, Sugishita C, Ernst E. Systematic review of adverse events following acupuncture: the Japanese literature. Complement Ther Med. 2001;9(2):98–104. [DOI] [PubMed] [Google Scholar]
- 27.Zhao L, Zhang F-w, Li Y, et al. Adverse events associated with acupuncture: three multicenter randomized controlled trials of 1968 cases in China. Trials. 2011;12:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Macpherson H, Scullion A, Thomas JJ, Walters S. Patient reports of adverse events associated with acupuncture treatment: a prospective national survey. Qual Saf Health Care. 2004;13(5):349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peuker PGG, Peuker E, Gronemeyer D. Rare but serious complications of acupuncture: traumatic lesions. Acupunct Med. 2001;19(2):103–108. [DOI] [PubMed] [Google Scholar]
- 30.Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9(1):72–83. [PubMed] [Google Scholar]
- 31.Schünemann H, Oxman A, Higgins J, et al. Chapter 11: Presenting results and ‘summary of findings’ tables In: Higgins JPTGS, ed. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Available from http://cochrane-handbook.org : The Cochrane Collaboration; 2011. [Google Scholar]
- 32.Schünemann H, Oxman A, Vist G, et al. Chaper 12: Interpreting results and drawing conclusions. In: Higgins JPTGS, ed. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Available from http://cochrane-handbook.org : The Cochrane Collaboration; 2011. [Google Scholar]
- 33.Glenton C, Santesso N, Rosenbaum S, et al. Presenting the results of Cochrane Systematic Reviews to a consumer audience: a qualitative study. Medical decision making : an international journal of the Society for Medical Decision Making. 2010;30(5):566–577. [DOI] [PubMed] [Google Scholar]
- 34.Liddle S, Pennick V. Interventions for preventing and treating low‐back and pelvic pain during pregnancy. Cochrane Database of Systematic Reviews. 2015(9). 10.1002/14651858.CD001139.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Furlan A, van TM, Cherkin D, et al. Acupuncture and dry‐needling for low back pain. Cochrane Database of Systematic Reviews. 2005(1). 10.1002/14651858.CD001351.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Green S, Buchbinder R, Barnsley L, et al. Acupuncture for lateral elbow pain. Cochrane Database of Systematic Reviews. 2002(1). 10.1002/14651858.CD003527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Green S, Buchbinder R, Hetrick S. Acupuncture for shoulder pain. Cochrane Database of Systematic Reviews. 2005(2). 10.1002/14651858.CD005319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev. 2010(1):CD001977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Manheimer E, Cheng K, Wieland L, et al. Acupuncture for hip osteoarthritis. Cochrane Database of Systematic Reviews. 2018(5). 10.1002/14651858.CD013010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Deare J, Zheng Z, Xue C, et al. Acupuncture for treating fibromyalgia. Cochrane Database of Systematic Reviews. 2013(5). 10.1002/14651858.CD007070.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Casimiro L, Barnsley L, Brosseau L, et al. Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis. Cochrane Database of Systematic Reviews. 2005(4). 10.1002/14651858.CD003788.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paley C, Johnson M, Tashani O, Bagnall A. Acupuncture for cancer pain in adults. Cochrane Database of Systematic Reviews. 2015(10). 10.1002/14651858.CD007753.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kwan I, Wang R, Pearce E, Bhattacharya S. Pain relief for women undergoing oocyte retrieval for assisted reproduction. Cochrane Database of Systematic Reviews. 2018(5). 10.1002/14651858.CD004829.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med. 2006;24(1):13–15. [DOI] [PubMed] [Google Scholar]
- 45.Lundeberg T, Lund I, Naslund J, Thomas M. The Emperors sham - wrong assumption that sham needling is sham. Acupunct Med. 2008;26(4):239–242. [DOI] [PubMed] [Google Scholar]
- 46.Chae Y, Lee YS, Enck P. How Placebo Needles Differ From Placebo Pills? Front Psychiatry. 2018;9:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Farquhar J Knowing practice : the clinical encounter of chinese medicine. Boulder: Westview; 1996. [Google Scholar]
- 48.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schnyer RN, Allen JJ. Bridging the gap in complementary and alternative medicine research: manualization as a means of promoting standardization and flexibility of treatment in clinical trials of acupuncture. J Altern Complement Med. 2002;8(5):623–634. [DOI] [PubMed] [Google Scholar]
- 50.MacPherson H, Schroer S. Acupuncture as a complex intervention for depression: a consensus method to develop a standardised treatment protocol for a randomised controlled trial. Complement Ther Med. 2007;15(2):92–100. [DOI] [PubMed] [Google Scholar]
- 51.Citkovitz C Acupuncture during stroke rehabilitation: development of a manual for researching a complex intervention (Doctoral Dissertation, University of Westminster). 2015. [Google Scholar]
- 52.Kligler B, Nielsen A, Kohrrer C, et al. Acupuncture therapy in a group setting for chronic pain. Pain Med. 2018;19:393–403. [DOI] [PubMed] [Google Scholar]
- 53.Schnyer RN, Iuliano D, Kay J, Shields M, Wayne P. Development of protocols for randomized sham-controlled trials of complex treatment interventions: Japanese acupuncture for endometriosis-related pelvic pain. J Altern Complement Med. 2008;14(5):515–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nielsen A, Anderson B, Citkovitz C, et al. Developing and employing a ‘responsive manualization’ in the ‘Acupuncture Approaches to Decrease Disparities in Outcomes of Pain Treatment’ comparative effectiveness study. Acupunct Med. 2019:964528419834015. [DOI] [PubMed] [Google Scholar]
- 55.Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Practical Assessment, Research & Evaluation (PARE). 2007;12(10):1–8. [Google Scholar]
- 56.Deng S, Zhao X, Du R, et al. Is acupuncture no more than a placebo? Extensive discussion required about possible bias. Exp Ther Med. 2015;10(4):1247–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Balas EA, Boren SA. Medical clinical knowledge for health care improvement In: Bemmel J, AT M, eds. Yearbook of medical informatics. Stuttgart; Germany: Schattauer; Verlagsgesellschaft mbH;; 2000:65–70. [PubMed] [Google Scholar]
- 58.NIH Introduction to pragmatic clinical trials. Health Care Systems Research Collaboratory, Rethinking Clinical Trials 2014; https://dcricollab.dcri.duke.edu/sites/NIHKR/KR/Introduction%20to%20pragmatic%20clinical%20trials.pdf. Accessed May 22, 2019.
- 59.Weinfurt KP, Hernandez AF, Coronado GD, et al. Pragmatic clinical trials embedded in healthcare systems: generalizable lessons from the NIH Collaboratory. BMC Med Res Methodol. 2017;17(1):144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rethinking Clinical Trials: Living Textbook of Pragmatic Clinical Trials. NIH Collaboratory Living Textbook of Pragmatic Clinical Trials http://rethinkingclinicaltrials.org/. Accessed September 27, 2018.
- 61.Concannon TW, Guise JM, Dolor RJ, et al. A national strategy to develop pragmatic clinical trials infrastructure. Clin Transl Sci. 2014;7(2):164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. 2016;2016(6):Art. No.:CD001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev. 2016;2016(4):Art. No.: CD007587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. 2018;19(5):455–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.MacPherson H, Tilbrook H, Richmond S, et al. Alexander technique lessons or acupuncture sessions for persons with chronic neck pain: a randomized trial. Ann Intern Med. 2015;163(9):653–662. [DOI] [PubMed] [Google Scholar]
- 66.MacPherson H, Maschino AC, Lewith G, et al. Characteristics of acupuncture treatment associated with outcome: an individual patient meta-analysis of 17,922 patients with chronic pain in randomised controlled trials. PLoS One. 2013;8(10):e77438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Witt CM, Vertosick EA, Foster NE, et al. The Effect of Patient Characteristics on Acupuncture Treatment Outcomes: An Individual Patient Data Meta-Analysis of 20,827 Chronic Pain Patients in Randomized Controlled Trials. Clin J Pain. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Choi G, Wieland L, Lee H, Sim H, Lee M, Shin B. Acupuncture and related interventions for the treatment of symptoms associated with carpal tunnel syndrome. Cochrane Database of Systematic Reviews. 2018(12). 10.1002/14651858.CD011215.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Franco J, Turk T, Jung J, et al. Non‐pharmacological interventions for treating chronic prostatitis/chronic pelvic pain syndrome. Cochrane Database of Systematic Reviews. 2018(5). 10.1002/14651858.CD012551.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ju Z, Wang K, Cui H, et al. Acupuncture for neuropathic pain in adults. Cochrane Database of Systematic Reviews. 2017(12). 10.1002/14651858.CD012057.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kim K, Lee M, Kim T, Kang J, Choi T, Lee J. Acupuncture and related interventions for symptoms of chronic kidney disease. Cochrane Database of Systematic Reviews. 2016(6). 10.1002/14651858.CD009440.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of tension‐type headache. Cochrane Database of Systematic Reviews. 2016(4). 10.1002/14651858.CD007587.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mangesi L, Zakarija‐Grkovic I. Treatments for breast engorgement during lactation. Cochrane Database of Systematic Reviews. 2016(6). 10.1002/14651858.CD006946.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Smith C, Armour M, Zhu X, Li X, Lu Z, Song J. Acupuncture for dysmenorrhoea. Cochrane Database of Systematic Reviews. 2016(4). 10.1002/14651858.CD007854.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boldt I, Eriks‐Hoogland I, Brinkhof M, de BR, Joggi D, von EE. Non‐pharmacological interventions for chronic pain in people with spinal cord injury. Cochrane Database of Systematic Reviews. 2014(11). 10.1002/14651858.CD009177.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Smith C, Collins C, Crowther C, Levett K. Acupuncture or acupressure for pain management in labour. Cochrane Database of Systematic Reviews. 2011(7). 10.1002/14651858.CD009232. [DOI] [PubMed] [Google Scholar]
- 77.Zhu X, Hamilton K, McNicol E. Acupuncture for pain in endometriosis. Cochrane Database of Systematic Reviews. 2011(9). 10.1002/14651858.CD007864.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database of Systematic Reviews. 2010(1). 10.1002/14651858.CD001977.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Verhagen A, Scholten‐Peeters G, van WS, de BR, Bierma‐Zeinstra S. Conservative treatments for whiplash. Cochrane Database of Systematic Reviews. 2007(2). 10.1002/14651858.CD003338.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]