Abstract
The prevalence of mental disorders in Iran is rising for many reasons including the population growth and its problems, the collapse of the family foundation, the economic problems, etc. Epidemiological studies of psychiatric disorders play an important role in determining the general mental health of the population and policy-making and future planning of service delivery. To identify the relevant studies, two authors independently searched different scholarly databases including Embase, PubMed/MEDLINE, ISI/Web of Science (WOS), Scopus, Psych INFO, and Iranian databases such as MagIran, SID, IranPsych, and Irandoc from 1st January 2007 up to 1st July 2018. The gray literature (through Google Scholar) was also mined. Studies written in English or in the Persian language were searched. After searching the databases and removing duplicates cases, a total of 10 studies were selected and included in the study, which reported a total of 14 prevalence rates. There were a total of 72,262 participants, of whom 32,925 were male and 39,337 were female. The prevalence of psychiatric disorders in studies which used screening tool was 31.03% (95% confidence interval: 25.99–36.07). The prevalence was 25.42% in studies which used clinical interviews (95% CI: 15.96–34.88). There is an undeniable fact that the prevalence of mental disorders in Iran has been increasing, and this could be a warning to policy-makers and health system managers. Hence, it is necessary to pay attention to this issue to maintain social capital, vitality, and efficiency of individuals and society as a whole.
Keywords: Iran, mental health, meta-analysis, prevalence, psychiatry
Introduction
Today, we encounter a warning increase in the incidence of mental disorders around the world, which stems from political turmoil, continuous wave of violence, and frequent changes in the social texture of countries,[1,2] so that mental disorders and substance abuse are considered one of the most important health problems in the world.[3]
According to the conducted studies, psychiatric disorders are one of the most important and significant components of the overall burden of diseases.[4] The findings of the global burden of diseases study in 2015 have shown that psychiatric disorders are one of the main causes of the global burden of illnesses.[5] It is estimated that approximately 900 million people in the world suffer from mental illnesses, accounting for 19% of the world's total population.[6,7] Of these, 75% live in low- and middle-income countries.[8] In 2015, mental disorders caused 10.7 million disability-adjusted life year (DALYs) in the Eastern Mediterranean Region (EMR) of World Health Organization, which accounts for 4.7% of the total EMR's DALYs.[9] Mental disorders also created 10.7 million years lost due to disability (YLDs) in EMR, accounting for 15.9% of the total EMR's YLDS.[9]
Various studies have already been conducted on the prevalence of mental disorders in Iran.[10,11] According to mental health research in 2008, the prevalence of mental disorders in the population over the age of 15 years has been estimated to be 21% throughout the country. The prevalence of emotional disorders and schizophrenia in the country was 17% in 2001. The prevalence of mental disorders in Tehran was 34% in 2011.[12] According to another study, the prevalence of mental disorders in the country was 23%.[13] The results of the latest national study of mental disorders in Iran in 2015 showed that the prevalence of mental disorders in the country varies between 21% and 34.2%. However, one out of every four Iranian is suspected to mental disorders.[12]
Epidemiological studies of psychiatric disorders play an important role in determining the general mental health of the population and policy-making and future planning of service delivery. Given the diversity of studies conducted, review studies are appropriate options for extracting, combining, and integrating data from various studies.[14]
In this regard, various studies have been conducted in different countries on the prevalence of mental disorders.[15,16] To date, one systematic review has been conducted on the prevalence of psychiatric disorders in Iran in 2007. In this systematic review, 35 studies were reviewed by the end of 2006, and its results showed that the prevalence of psychiatric disorders in screening studies was 28.70% and in studies conducted through diagnostic interviews was 18.60%.[17] Extensive research have been done on the prevalence rate of mental disorders in Iran the during recent 10 years, which are diverse in terms of time, place, measurement tools, and so on. However, there is no systematic review of the integration and interpretation of these data. Therefore, the purpose of this study was to investigate the prevalence of psychiatric disorders in Iranian adult population through a systematic review from 2007 to 2018.
Materials and Methods
Search Strategy
This review has been performed according to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” guidelines.[18] Two authors independently searched different scholarly databases including Embase, PubMed/MEDLINE, ISI/Web of Science (WOS), Scopus, Psych INFO, and Iranian databases such as MagIran, SID, IranPsych, and Irandoc from 1st January 2007 up to 1st July 2018. The gray literature (through Google Scholar) was also mined. Studies written in English or in the Persian language were searched. Our search strategy was as follows: (Prevalence OR Epidemiology) AND (Mental Disorders OR Psychiatric Diagnosis OR Behavior Disorders OR Severe Mental Disorder) AND (Iran). Medical subject headings and wild-card options were used where appropriate. This search strategy was planned together with an information specialist. In addition, reference lists of each identified study were examined for potentially eligible studies.
Inclusion criteria
All main studies that examined the prevalence of mental disorders in the general population were included in the study. These include (1) the prevalence of mental disorders determined by screening tools such as questionnaires; and (2) The prevalence of mental disorders determined by clinical interviews. Prevalence can be determined as “point prevalence,” “lifetime prevalence,” or “periodic prevalence,” Point prevalence is a proportion of the population that has a mental disorder at a given point of time (for example, 1 day to 1 month). Periodic prevalence is a proportion of the population that has mental disorders in a specific time period (such as 12-month prevalence) and includes those who have had the disorder at the start of the study or have had mental disorders during the study. The lifetime prevalence is a proportion of the population experiencing mental disorders at a point in their life (up to the time of study).[18]
Exclusion criteria
Studies which were not original such as review studies, studies conducted in specific population groups such as immigrants, prisoners, students, or those who referred to treatment centers, and studies conducted exclusively in children and adolescents (under 15-year-old) were excluded from the study. In addition, studies have been conducted to follow-up the services and treatment provided to a specific group, studies that examine the relationship between genetic and mental disorders, or studies that were limited to assessing mental disorders associated with drug abuse and addiction, personality disorders, and backwardness of life were excluded. As we encountered with studies in which there was overlapping in the sample (such as cases where a large study was split into smaller studies), the most comprehensive report was examined.
Data extraction
Two authors independently extracted the following data from the selected studies: prevalence estimate of “any psychiatric disorder” among men, women, and total sample (along with confidence intervals and standard errors); study time frame; study location and the geographical extent of data collection; data collection tools and methods (questionnaire, face-to-face diagnostic interview or checklists, psychometric properties of the instruments); and sample characteristics. Prevalence rates are classified in two ways: life-time or point prevalence in one hand and prevalence rates obtained through diagnostic interview or screening (probable disorder) on the other hand. In the event that the two researchers' opinions differed on data extraction of any of the studies, they first tried to reach consensus through discussion; then they consulted the corresponding author, if they could not overcome the disagreement. All the information was entered in the forms which had been designed for this purpose.
Statistical analysis
The prevalence data were described and synthesized descriptively, and the sources of heterogeneity were discussed. A random-effects meta-analysis was used to give a pooled estimate of prevalence of mental health symptoms for each measure. Heterogeneity among studies was evaluated using the I2 statistic with greater than 75% representing high heterogeneity.[19] Statistical analyses were conducted using STATA version 13 (StataCorp, College Station, TX, USA).
Results
After searching the databases and removing duplicates cases, a total of 10 studies were selected and included in the study, which reported a total of 14 prevalence rates[13,20,21,22,23,24,25,26,27,28] [Figure 1]. All selected studies were journal articles. From 10 studies, two studies were conducted at the national level, seven studies at urban regions, and one study in rural areas. One study reported a periodic prevalence and nine studies measured the point prevalence. Six studies were conducted using the one-step method and four studies were performed in two stages so that first the suspected cases were identified using the screening tool, and then they measured the incidence of mental disorders using a clinical interview for suspected cases. Out of five studies that were conducted as one-step study using the screening tool, three studies used General Health Questionnaire (GHQ) questionnaire and two studies used SCL-90-R, and one study was conducted using a clinical interview. In four studies that were performed in two stages, three studies used GHQ questionnaire for screening and then they used DSM-IV checklist for clinical interview with suspicious persons. In another study, the Duke University Questionnaire (DUQ) questionnaire was used in the first stage for screening, and DSM-IV checklist was used for clinical interviews [Tables 1-3]. The quality assessment of studies using the STROBE checklist showed that seven studies had good quality, and three studies had moderate quality. The average response rate in the studies was 94.9%. The Persian version of the screening tool in all of the studies has had acceptable reliability and validity. There were a total of 72,262 participants, of whom 32,925 were male and 39,337 were female. The prevalence of psychiatric disorders in studies which used screening tool was 31.03% (95% confidence interval: 25.99–36.07) [Figure 2]. The prevalence was 25.42% in studies which used clinical interviews (95% CI: 15.96–34.88) [Figure 3]. One study only reported the periodic prevalence of mental disorders at 23.6%. The prevalence of mental disorders was 17.23% (95% CI: 15.78–18.68) according to the DUQ questionnaire, 29.66% (95% CI: 24.09–35.24) according to the GHQ questionnaire, and 42.70% (95% CI: 18.98–66.41) according to the SCL-90-R questionnaire [Figure 4].
Figure 1.

Flow diagram showing the different steps involved in searching for relevant publications (2007-2018)
Table 1.
Characteristics of studies conducted on point prevalence of mental disorders on the basis of screening among Iranian general population over 15 years old
| Authors | Publication year | Type of document | Target population | Year of the study | Total sample size | Male sample size | Female sample size | Response rate | Screening tool | Cut-off | Prevalence- persons | Prevalence male | Prevalence female |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Narimani | 2011 | Paper | 15-65 in the urban areas of Ardabil province | 2011 | 1430 | 700 | 730 | 98.6 | GHQ | 6 | 27.8 | 21.1 | 34.2 |
| Noorbala | 2017 | Paper | 10 and above in Iran nationwide | 2015 | 35813 | 17837 | 17976 | 99.4 | GHQ | 6 | 23.44 | 19.28 | 27.55 |
| Raeisoon | 2012 | Paper | Over 15 year olds in Birjand | 2010 | 582 | 305 | 277 | 97 | SCL-90-R | 2.5 | 54.8 | 47.54 | 63.17 |
| Noorbala | 2011 | Paper | Over 15 year olds in Tehran | 2009 | 19370 | 7705 | 11665 | 87.5 | GHQ | 6 | 34.2 | 28.6 | 37.9 |
| Kazemi | 2014 | Paper | 15 and higher in rural areas of Birjand | 2011 | 504 | 163 | 341 | ? | SCL-90-R | 2 | 30.6 | 20.9 | 35.2 |
| Ahmadvand | 2012 | Paper | 18 years and older Kahsan | 2008 | 1800 | 819 | 981 | ? | GHQ | 6 | 33.7 | ? | ? |
| Parvaresh | 2011 | Paper | Kerman residents city older than 15 years old | 2007 | 1527 | 495 | 1032 | 96 | GHQ | 6 | 33 | 27 | 34 |
| Fakhari | 2007 | Paper | 17 years and older in north-Weth Area. Tabriz city | 2007 | 2623 | 1210 | 1413 | 99.6 | DUQ | 30 or less | 17.23 | ? | ? |
| Veisani | 2017 | Paper | People aged 15 years and over from all 10 cities in Ilam province | 2016 | 763 | 340 | 423 | ? | GHQ | 6 | 25.8 | 20.9 | 29.8 |
GHQ=General Health Questionnaire, SCL-90=Symptom Checklist-90
Table 3.
Characteristics of the period prevalence studies of mental disorder
| Authors | Publication year | Type of document | Target population | Year of the study | Total sample size | Male sample size | Female sample size | Response rate | Tool | Cut-off | Prevalence- persons | Prevalence male | Prevalence female |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vandad sharifi | 2015 | Paper | 15-65 in the urban and rural areas of Iran | 2011 | 7,886 | 3,387 | 4,499 | 86.2 | CIDI | ? | 23.6 | 20.8 | 26.5 |
Figure 2.
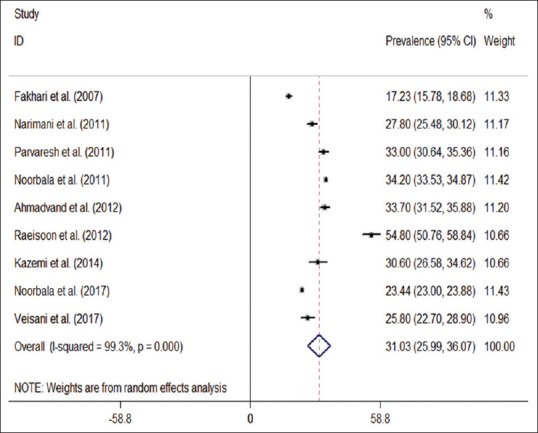
The overall prevalence of psychiatric disorders on the basis of screening tool
Figure 3.

The overall prevalence of psychiatric disorders on the basis of clinical interviews
Figure 4.
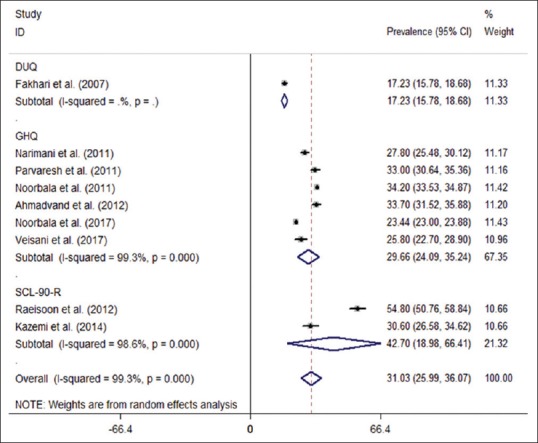
The results of subgroup analyses on the basis of the tools
Table 2.
Characteristics of the studies of point prevalence of mental disorders on the basis of screening and diagnostic interview among general population over 15 years old in Iran
| Authors | Publication year | Type of document | Target population | Year of the study | Total sample size | Male sample size | Female sample size | Response rate | Tool | Cut-off | Prevalence- persons | Prevalence male | Prevalence female | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening | Diagnostic interview | |||||||||||||
| Ahmadvand | 2012 | Paper | 18 years and older Kahsan | 2009 | 1800 | 819 | 981 | ? | GHQ | DSM-IV checklist | 6 | 29.2 | 21.2 | 35.5 |
| Parvaresh | 2011 | Paper | Kerman city residents older than 15 years old | 2007 | 1491 | 459 | 1032 | 96 | GHQ | DSM-IV checklist | 6 | 32.1 | 27.1 | 34.5 |
| Fakhari | 2007 | Paper | 17 years and older in north-Weth area. Tabriz | 2007 | 2623 | 1210 | 1413 | 99.6 | DUQ | DSM-IV checklist | 30 or less | 14.4 | 8.6 | 19.4 |
| Veisani | 2017 | Paper | People aged 15 years and over from all 10 cities in Ilam province | 2016 | 763 | 340 | 423 | ? | GHQ | DSM-IV checklist | 6 | 26.1 | ? | ? |
DUQ=Duke University Questionnaire, DSM-IV=Diagnostic and Statistical Manual of Mental Disorders
To evaluate possible heterogeneity sources among studies, meta-regression analyses were carried out according to the year of publication, sample size, tools, and gender in screening studies. Table 4 shows the results. The relation between prevalence and gender was at the borderline in terms of significance (P = 0.085). In addition, meta-regression analyses were carried out according to the year of publication, sample size, and gender in studies depending clinical interview. Table 5 shows the result.
Table 4.
The results of meta-regression in study on the basis of screening among Iranian general population over 15 years old
| Variables | Co-efficient | CI | P |
|---|---|---|---|
| Sample size | −1.97 * 10−4 | −9.26 * 10−4-5.31 * 10−4 | 0.542 |
| Tools | 5.09 | −4.46 to 14.66 | 0.248 |
| Gender | 10.83 | -1.73 to 23.40 | 0.085 |
| Year of publication | −1.70 | −4.28 to 0.87 | 0.175 |
Table 5.
The results of meta-regression in study on the basis of clinical interview among Iranian general population over 15 years old
| Variables | Co-efficient | CI | P |
|---|---|---|---|
| Sample size | −6.65 * 10−3 | −3.009* 10−2-1.67* 10−2 | 0.346 |
| Gender | 10.78 | −10.35-31.87 | 0.229 |
| Year of publication | 1.03 | −3.80-5.87 | 0.458 |
Discussion and Conclusion
The present study was designed to determine the prevalence of psychiatric disorders in the general population. In this study, the prevalence of psychiatric disorders was 31.03% (95% CI 25.99–36.07) depending on screening in the general population and 25.42% (95% CI 15.96–34.88) depending on clinical interview, which was higher than countries such as Iraq (18.8%), India (12.2%), Turkey (20%), Finland (17.4%), Germany (27.7%), Greece (29%) and less than Norway (32.8%), Pakistan (34%), and Afghanistan (50%).[14,16,29,30,31,32,33] The global mean prevalence of mental disorders is also 17.6%.[34] The prevalence of mental disorders in Iran's general population was reported 29% in Farhudian et al. study, which was conducted through systematic review in 2007.[17] In addition, the prevalence of mental disorders was 22% on the basis of clinical interviews in that study. The comparison of the two studies showed that the prevalence of mental disorders increased by approximately 2% depending on screening and more than 3% on the basis of clinical interviews over a decade. There are many social and economic factors, such as the economic crisis, unemployment, and poverty in the community, which are risk factors for health problems and predispose to mental disorders, suicide, and addiction. The high ratio of unemployed people and the high proportion of people living in poverty in the country can be the reasons for this issue.[35] These indicators are among the determinants of mental health in societies.[36,37] It is necessary to mentions that mental health is influenced by many variables and is not dependent solely on one agent, and these factors can vary in any society.[38] Therefore, attention to a conceptual framework of mental health indicators that make it possible to create a common language for measuring mental health status seems necessary,[39] as various countries have developed these indicators.[40] The differences between existing studies can be owing to methodological reasons, and it is suggested that an integrated instruction be provided to serve as a basis for measuring the prevalence of mental disorders and provided the minimum standards for these studies.
Screening instruments have been GHQ and SCL-90-R in most of our studies like many other studies in the world. The advantage of the GHQ is not only considerations of time but also widespread use in other disciplines, which provide the possibility for comparison.[41] Another advantage of this tool is the simplicity of completing and easy scoring.[42,43] In addition, the benefit of the SCL-90-R is the fact that this tool covers a lot of dimensions, and it is more effective in multidimensional psychiatric research.[44] However, the only negative point in these studies was a different cut-off point. The results of the study indicate that the most prevalence was in studies that used SCL-90-R as a measuring tool. The reason for this issue is that this tool is used to diagnose suspected cases in most studies; therefore, the measured prevalence through this tool is high.
Given the difference in the prevalence rate that was measured on the basis of screening and clinical interviews, there is an undeniable fact that the prevalence of mental disorders in Iran has been increasing, and this could be a warning to policy-makers and health system managers. Hence, it is necessary to pay attention to this issue to maintain social capital, vitality, and efficiency of individuals and society as a whole.
Financial support and sponsorship
This study was part of a PhD thesis supported by the School of Health Services Management and Medical Information Science, Iran University of Medical Sciences, Iran (IUMS/SHMIS_1397-01-136-33038).
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. The World Health Report 2001: Mental Health: New Understanding. New Hope: World Health Organization; 2001. [Google Scholar]
- 2.Health WHODoM, Abuse S, Health WHODoM, Health SAM, Organization WH, Evidence WHOMH, et al. Mental Health Atlas 2005. World Health Organization; 2005. [Google Scholar]
- 3.Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: An analysis from the global burden of disease study 2010. PloS One. 2015;10:e0116820. doi: 10.1371/journal.pone.0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olfson M, Marcus SC, Druss B, Elinson L, Tanielian T, Pincus HA. National trends in the outpatient treatment of depression. JAMA. 2002;287:203–9. doi: 10.1001/jama.287.2.203. [DOI] [PubMed] [Google Scholar]
- 5.Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388:1545–602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Organization WH. The world health report 2003: Shaping the future: World Health Organization. 2003 [Google Scholar]
- 7.Kassebaum NJ, Arora M, Barber RM, Bhutta ZA, Brown J, Carter A, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1603–58. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. mhGAP: Mental Health Gap Action Programme: Scaling Up Care For Mental, Neurological And Substance Use Disorders. World Health Organization; 2008. [PubMed] [Google Scholar]
- 9.Faten E, Nader M, Raies H, Sana M, Amel M, Fadhel MM. Body image disorder in 100 Tunisian female breast cancer patients. Bull Cancer. 2018;105:350–6. doi: 10.1016/j.bulcan.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Mohammadi MR, Davidian H, Noorbala AA, Malekafzali H, Naghavi HR, Pouretemad HR, et al. An epidemiological survey of psychiatric disorders in Iran. Clin Pract Epidemiol Ment Health. 2005;1:16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noorbala AA, Bagheri Yazdi SA, Yasamy MT, Mohammad K. Mental health survey of the adult population in Iran. Br J Psychiatry. 2004;184:70–3. doi: 10.1192/bjp.184.1.70. [DOI] [PubMed] [Google Scholar]
- 12.Noorbala AA, Faghihzadeh S, Kamali K, Bagheri Yazdi SA, Hajebi A, Mousavi MT, et al. Mental health survey of the Iranian adult population in 2015. Arch Iran Med. 2017;20:128–34. [PubMed] [Google Scholar]
- 13.Vandad Sharifi M, Hajebi A, Radgoodarzi R. Twelve-month prevalence and correlates of psychiatric disorders in Iran: The Iranian mental health survey, 2011. Arch Iran Med. 2015;18:76–84. [PubMed] [Google Scholar]
- 14.Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: Systematic review. BMJ. 2004;328:794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moreno-Küstner B, Martín C, Pastor L. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One. 2018;13:e0195687. doi: 10.1371/journal.pone.0195687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ranjan JK, Asthana HS. Prevalence of mental disorders in India and other south Asian countries. Asian J Epidemiol. 2017;10:45–53. [Google Scholar]
- 17.Yousefi-Nooraie R, Mohammadi MR, Salesian N, Amin-Esmaeeli M, Mansouri N, Mesgarpour B, et al. Prevalence of psychiatric disorders in Iran: A systematic review. Iran J Psychiatry. 2007;2:137–50. [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. PLoS Med. 2007;4:e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Narimani M, Sadeghieh Ahari S, Abdi R. Epidemiological survey of mental disorders in urban regions of Ardabil province (Iran) J Psychiatr Ment Health Nurs. 2011;18:368–73. doi: 10.1111/j.1365-2850.2011.01700.x. [DOI] [PubMed] [Google Scholar]
- 22.Ahmadvand A, Sepehrmanesh Z, Ghoreishi FS, Afshinmajd S. Prevalence of psychiatric disorders in the general population of Kashan, Iran. Arch Iran Med. 2012;15:205–9. [PubMed] [Google Scholar]
- 23.Parvaresh N, Ziyaodini H, Nakhaei N, Nahid A, Safavi H, Sajadi B. The frequency of mental disorders among Kerman residents above 15 years of age. J Kerman Univ Med Sci. 2011;18:291–300. [Google Scholar]
- 24.Fakhari A, Ranjbar F, Dadashzadeh H, Moghaddas F. An epidemiological survey of mental disorders among adults in the north, west area of Tabriz, Iran. Pak J Med Sci. 2007;23:54–8. [Google Scholar]
- 25.Noorbala AA, Bagheri Yazdi SA, Faghihzadeh S, Kamali K, Faghihzadeh E, Hajebi A, et al. A Survey on mental health status of adult population aged 15 and above in the province of Kordestan, Iran. Arch Iran Med. 2017;20(11 Suppl 1):S71–4. [PubMed] [Google Scholar]
- 26.Veisani Y, Mohamadian F, Delpisheh A. Prevalence and comorbidity of common mental disorders and associations with suicidal ideation in the adult population. Epidemiol Health. 2017;39:e2017031. doi: 10.4178/epih.e2017031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rieson M, Miri M, Dastjerdi R, Sharifzadeh G. Prevalence of mental disorders in Birjand – 2010. J Birjand Univ Med Sci. 2012;19:81–7. [Google Scholar]
- 28.Noorbala AA, Bagheri Yazdi SA, Asadi Lari M, Vaez Mahdavi MR. Mental health status of individuals fifteen years and older in Tehran-Iran (2009) Iran J Psychiatry Clin Psychol. 2011;16:479–83. [Google Scholar]
- 29.Alhasnawi S, Sadik S, Rasheed M, Baban A, Al-Alak MM, Othman AY, et al. The prevalence and correlates of DSM-IV disorders in the Iraq Mental Health Survey (IMHS) World Psychiatry. 2009;8:97–109. [PMC free article] [PubMed] [Google Scholar]
- 30.Dereboy C, Güzel HS, Dereboy F, Okyay P, Eskin M. Personality disorders in a community sample in Turkey: Prevalence, associated risk factors, temperament and character dimensions. Int J Soc Psychiatry. 2014;60:139–47. doi: 10.1177/0020764012471596. [DOI] [PubMed] [Google Scholar]
- 31.Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatry. 2001;158:1091–8. doi: 10.1176/appi.ajp.158.7.1091. [DOI] [PubMed] [Google Scholar]
- 32.Lehtinen V, Joukamaa M, Lahtela K, Raitasalo R, Jyrkinen E, Maatela J, et al. Prevalence of mental disorders among adults in Finland: Basic results from the Mini Finland Health Survey. Acta Psychiatr Scand. 1990;81:418–25. doi: 10.1111/j.1600-0447.1990.tb05474.x. [DOI] [PubMed] [Google Scholar]
- 33.Ghulam Dastagir S. Mental health in Afghanistan: Mental health in Afghanistan: burden, challenges and the way forward (English) Health, Nutrition and Population (HNP) discussion paper. Washington, DC: World Bank; 2011. [Google Scholar]
- 34.Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int J Epidemiol. 2014;43:476–93. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mohamadi K, Ahmadi K, Ashtiani AF, Fallah PA, Ebadi A, Yahaghi E. Indicators of mental health in various Iranian populations. Iran Red Crescent Med J. 2014;16:e14292. doi: 10.5812/ircmj.14292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stone SA, Frost LE, Van Norman JR, Casey KA. Creating a mentally healthy community through the use of behavioral health indicators. Appl Res Qual Life. 2010;5:273–85. [Google Scholar]
- 37.Shield T, Campbell S, Rogers A, Worrall A, Chew-Graham C, Gask L. Quality indicators for primary care mental health services. BMJ Qual Saf. 2003;12:100–6. doi: 10.1136/qhc.12.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nolen-Hoeksema S. SexSex Differences in Depression. Stanford University Press; 1990. [Google Scholar]
- 39.Mohamadi K, Ahmadi K, Fathi Ashtiani A, Azad Fallah P, Ebadi A, Yahaghi E. Indicators of mental health in various Iranian populations. Iranian Red Crescent Med J. 2014;16:e14292. doi: 10.5812/ircmj.14292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han H, Ahn DH, Song J, Hwang TY, Roh S. Development of mental health indicators in Korea. Psychiatry Investig. 2012;9:311–8. doi: 10.4306/pi.2012.9.4.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jackson C. The general health questionnaire. Occup Med. 2007;57:79. [Google Scholar]
- 42.Feyer A-M, Herbison P, Williamson AM, de Silva I, Mandryk J, Hendrie L, et al. The role of physical and psychological factors in occupational low back pain: A prospective cohort study. Occup Environ Med. 2000;57:116–20. doi: 10.1136/oem.57.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones M, Rona RJ, Hooper R, Wesseley S. The burden of psychological symptoms in UK Armed Forces. Occup Med. 2006;56:322–8. doi: 10.1093/occmed/kql023. [DOI] [PubMed] [Google Scholar]
- 44.Koeter MW. Validity of the GHQ and SCL anxiety and depression scales: A comparative study. J Affect Disord. 1992;24:271–9. doi: 10.1016/0165-0327(92)90112-j. [DOI] [PubMed] [Google Scholar]


