Abstract
Objective:
The aim of this study was to describe individuals seeking care for injury at a major emergency department (ED) in southern Puerto Rico in the months after Hurricane Maria on September 20, 2017.
Methods:
After informed consent, we used a modified version of the Natural Disaster Morbidity Surveillance Form to determine why patients were visiting the ED during October 16, 2017–March 28, 2018. We analyzed visits where injury was reported as the primary reason for visit and whether it was hurricane-related.
Results:
Among 5 116 patients, 573 (11%) reported injury as the primary reason for a visit. Of these, 10% were hurricane-related visits. The most common types of injuries were abrasions, lacerations, and cuts (43% of all injury visits and 50% of hurricane-related visits). The most common mechanisms of injury were falls, slips, trips (268, 47%), and being hit by/or against an object (88, 15%). Most injury visits occurred during the first 3 months after the hurricane.
Conclusions:
Surveillance after Hurricane Maria identified injury as the reason for a visit for about 1 in 10 patients visiting the ED, providing evidence on the patterns of injuries in the months following a hurricane. Public health and emergency providers can use this information to anticipate health care needs after a disaster.
Keywords: hurricane, injury, syndromic surveillance
Unintentional injuries were the third leading cause of death in the United States in 2016.1 In addition, injuries are a leading cause of disability and a major contributor to health care expenditures; the economic burden of injury is estimated at over US $500 billion annually in medical care costs and loss of productivity across the life span of injury victims. Injury surveillance to advance public health policy has become an increasingly important issue in recent decades.2 Improving the integration and application of data collected from different injury surveillance tools is an important goal.2,3
Natural disasters, such as hurricanes, have a hazardous impact on human populations. The effects of weather and climate events are becoming more severe in developing countries because of the changes in weather patterns and the growing numbers of people and structures located in vulnerable areas.4 In these settings, natural disasters are likely to lead to greater numbers of injuries and deaths.4 A systematic literature review of worldwide natural disasters revealed that approximately 200 000 people died in storm events in the last 20 years, with storms having negatively affected around 660 000 people.4 In the United States and its territories, hurricane landfalls have been increasingly destructive and frequent in the past 2 decades, with some examples being Ivan (2004); Wilma, Rita, and Katrina (2005); Ike (2008); Sandy (2012); and Irma, Maria, and Harvey (2017).4 Hurricane Katrina was the deadliest hurricane to strike the US Gulf Coast since 1928. In a review of Hurricane Katrina–related deaths, injuries were the most common causes of death, including drowning (40% of deaths) and trauma (25% of deaths).5 Recent data show that injuries regularly increase in the period immediately after a natural disaster.4
On September 20, 2017, Hurricane Maria made landfall on the island of Puerto Rico as a Category 4 storm, affecting the entire island in its course. The hurricane caused an estimated US $90 billion in damages, making it the third costliest tropical storm in the United States since 1900 and the costliest hurricane on record to strike Puerto Rico and the US Virgin Islands.6,7
Disaster surveillance is important to help identify populations at risk and assess the effectiveness of public health response efforts, especially for a large-scale disaster when many illnesses and injuries occur. Knowledge of the types and mechanisms of injuries following a natural disaster is essential to the design of injury prevention measures and to effective mitigation. This is a key aspect of future disaster planning and preparedness, with the ultimate goal being to improve patient outcomes.8 A syndromic surveillance system was implemented in the emergency department (ED) of a major hospital system in southern Puerto Rico 3 weeks after Hurricane Maria. This paper aims to describe the types and mechanisms of injuries and the characteristics of the patients who reported them.
METHODS
Study Population
This was a cross-sectional study that used de-identified data from patients enrolled during October 16, 2017–March 28, 2018 at Saint Luke’s Episcopal Hospital (SLEH), a tertiary care teaching hospital, and the Centro de Emergencia y Medicina Integrada (CEMI), an associated urgent care clinic, both located in southern Puerto Rico. Because the study was implemented after Hurricane Maria’s landfall, it took approximately 3 weeks to obtain approvals, develop protocols, and train staff before beginning data collection. The catchment area included approximately 500 000 residents from the 15 municipalities in the Ponce health district. Patients seeking care at the ED at SLEH and the urgent clinic at CEMI during the study staff s working hours (8:00 AM to 11:00 PM) were eligible for enrollment.
Study Enrollment and Procedures
This study implemented a syndromic surveillance system using a modified version of the Natural Disaster Morbidity Surveillance Individual Form, a standardized single-page form developed by the Centers for Disease Control and Prevention’s (CDC’s) Disaster Epidemiology Community of Practice (formerly known as the Disaster Surveillance Workgroup).9 The goals of the surveillance system were to describe the distribution of injuries and illnesses, detect outbreaks, and guide timely interventions during the disaster.
The study staff in charge of enrollment received 8 hours of training focused on data collection and specific data elements of the form. Study research assistants and nurses enrolled patients in the surveillance system from the triage area of the ED. Patients who visited the ED during staff working hours were approached for participation; study personnel obtained informed consent and administered the morbidity surveillance form. Using portable tablets, the staff collected data electronically in Epi Info and uploaded form data to a centralized database on a daily basis. CDC staff provided technical assistance in the form of database development, data management, data analysis, weekly report development and dissemination, and troubleshooting of technical or questionnaire-related issues.
Measures in the Morbidity Surveillance Form
The validated surveillance form used in the study is divided into 4 sections: (1) visit information; (2) patient information; (3) reason for the visit; and (4) disposition. The form captured the primary reason for the visit using a list of the following areas: injury (type and mechanism), acute illness/symptoms, exacerbation of chronic disease, mental health, routine/follow-up, and other. For this analysis of injury-related visits, we categorized visits for any reason other than injury as “other.” For hurricane or non-hurricane-related classification, participants were asked whether the reason for their visit occurred because of work (paid or volunteer) involving disaster response or rebuilding efforts. The disposition information was updated on the day following the visit using the electronic medical record (EMR) corresponding to that visit. The age variable categories included children (< 19 years old), adults (19–59 years old), and elderly individuals (> 60 years old). The type of injury was defined as the type of trauma that resulted from the injury, which included abrasion, laceration, or cut; sprain or strain; concussion or head injury; and other. The mechanism of injury was defined as the process by which the injury took place and included fall, slip, or trip; hit by or against an object; bite or sting; motor vehicle crash; foreign body; and use of machinery, tools, or equipment. We collected data on disposition using the following categories: admitted to hospital, discharged to self-care, referred to other care, and left before being seen.
Baseline Data on Injuries From the Electronic Medical Records
We extracted patient data from EMRs from August 28, 2016, to March 25, 2018, to determine the baseline level of injury visits before and after Hurricane Maria. In the EMR, the patient’s reason for a visit was captured as a free-text field at registration. Diagnosis codes based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) were assigned at the end of the visit by the attending physician and verified or reassigned by the medical record department 5 to 10 days later.
The EMR data used for comparison were de-identified and included the patient’s age, sex, and visit date; the facility; the reason for the visit; and the ICD-10 diagnosis code (1–10). To categorize the ICD-10 codes, we used the variables on the morbidity surveillance form and identified 1 or more matching ICD-10 codes for each variable and assessed the number and types of visits over time and by site. Each record was given a primary reason for the visit based on the first diagnosis code; visits that remained uncategorized were instead classified based on the second diagnosis code. If the first 2 diagnosis codes did not fall into any of the morbidity-surveillance form categories, the visit was categorized as “other.” All of the ICD-10 codes were reviewed by the category of assignment to ensure that they had been assigned correctly.
Statistical Analysis
We calculated frequencies and percentages to describe injury-related visits by type of injury, mechanism of injury, and hurricane-related injuries, and assessed differences by age and sex. We tested comparisons for statistical significance using a chi-square (X2) test and Fisher’s exact test, and the results were considered to be statistically significant when P ≤ 0.05. The number of injury visits in the EMR data was presented as absolute counts. We conducted all analyses in SAS 9.4 and SPSS® Statistics for Windows, Version 25 (IBM Corp, Armonk, NY).
Ethics Statement
The study investigators do not report any potential financial or ethical conflicts of interest. Prior to the enrollment of the potential participants, a written informed consent was administered to them. The Institutional Review Board of the Ponce Research Institute/Ponce School of Medicine Foundation approved the study protocol. The CDC reviewed the protocol and approved it as non-research activity.
RESULTS
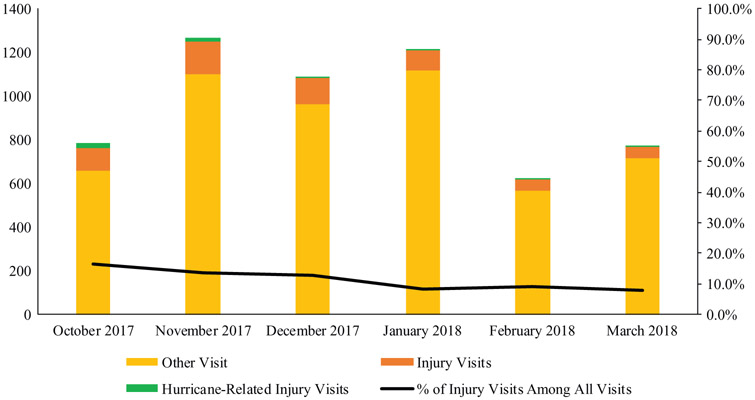
During the 6-month study period, the 2 surveillance sites registered 29 383 patient visits, of which, 5116 (17%) patients were enrolled in the syndromic surveillance study. Injury was reported as the primary reason for the visit for 573 (11%) participants, with those individuals having a mean age of 38 (range 0–96) years. Among participants with injury as the primary visit reason, 42% were ages 19–59 years. The participants resided in 24 of the 78 municipalities in Puerto Rico; however, the majority were residents of the Ponce municipality (60%). Half (51%) of the participants were male. Most of the injury visits (93%) resulted in a discharge to self-care (Table 1) and occurred during the first 3 months of the study period (Figure 1).
TABLE 1.
Characteristics of Participants With Injury in the Post-Hurricane Maria Surveillance System, Ponce, October 2017–March 2018
| All Injury Visits n = 573 |
Hurricane-Related n = 56 |
Non-Hurricane-Related n = 517 |
P value* | ||||
|---|---|---|---|---|---|---|---|
| Characteristics | N | % | n | % | N | % | |
| Sex, Male | 290 | 50.6 | 37 | 66.1 | 253 | 48.9 | 0.017 |
| Age Group | |||||||
| Children (< 19 years old) | 186 | 32.5 | 3 | 5.4 | 183 | 35.4 | <0.001 |
| Adults (19–59 years old) | 238 | 41.5 | 31 | 55.4 | 207 | 40.0 | 0.032 |
| Elderly (≥ 60 years old) | 149 | 26.0 | 22 | 39.3 | 127 | 24.4 | 0.024 |
| Municipality | |||||||
| Ponce | 341 | 59.5 | 34 | 60.7 | 307 | 59.4 | 0.887 |
| Peñuelas | 79 | 13.8 | 10 | 17.9 | 69 | 13.3 | 0.412 |
| Juana Diaz | 51 | 8.9 | 6 | 10.7 | 45 | 8.7 | 0.620 |
| Adjuntas | 18 | 3.1 | 0 | 0.0 | 18 | 3.5 | 0.241 |
| Other | 84 | 14.7 | 6 | 10.7 | 78 | 15.1 | 0.550 |
| Disposition | |||||||
| Discharged | 531 | 92.6 | 48 | 85.7 | 483 | 93.4 | 0.053 |
| Admitted | 16 | 2.8 | 4 | 7.1 | 12 | 2.3 | 0.061 |
| Referred to other care | 15 | 2.6 | 3 | 5.4 | 12 | 2.3 | 0.173 |
| Left before being seen | 11 | 1.9 | 1 | 1.8 | 10 | 1.9 | 1.000 |
| Type of Injury† | |||||||
| Abrasion, laceration, cut | 247 | 43.1 | 28 | 50.0 | 219 | 42.4 | 0.320 |
| Sprain/strain | 85 | 14.8 | 9 | 16.1 | 76 | 14.7 | 0.843 |
| Concussion, head injury | 45 | 7.9 | 7 | 12.5 | 38 | 7.4 | 0.188 |
| Other injury type‡ | 62 | 10.8 | 7 | 12.5 | 55 | 10.6 | 0.651 |
| No response | 141 | 24.6 | 7 | 12.5 | 134 | 25.9 | 0.032 |
| Mechanism of Injury† | |||||||
| Fall, slip, trip | 268 | 46.8 | 11 | 19.6 | 257 | 49.7 | <0.001 |
| Hit by or against an object | 88 | 15.4 | 17 | 30.4 | 71 | 13.7 | 0.003 |
| Bite/sting | 48 | 8.4 | 2 | 3.6 | 46 | 8.9 | 0.211 |
| Motor vehicle crash | 45 | 7.9 | 1 | 1.8 | 44 | 8.5 | 0.111 |
| Foreign body | 36 | 6.3 | 7 | 12.5 | 29 | 5.6 | 0.073 |
| Use of machinery, tools, or equipment | 31 | 5.4 | 11 | 19.6 | 20 | 3.9 | <0.001 |
| Other injury mechanism§ | 27 | 4.7 | 2 | 3.6 | 25 | 4.8 | 1.000 |
| No response | 33 | 5.7 | 5 | 8.9 | 28 | 5.4 | 0.357 |
Fisher’s exact test was used to calculate P values.
More than 1 injury type or mechanism could be selected.
Other injury type included fracture, avulsion, amputation, inflammation, irritation, puncture, and bruise.
Other injury mechanism included poisoning, burn, violence/assault, non-fatal drowning/submersion, cold/heat exposure, and electric shock.
Figure 1.
Percentage of Injury Visits Among All Enrolled Participants, Post-Hurricane Maria Surveillance System, Ponce, October 2017–March 2018.
Of the 573 participants who reported injury as the primary visit reason, 10% indicated that the visit was hurricane-related, occurring as a result of work involving disaster response or rebuilding efforts. Of the hurricane-related injury visits, 7% resulted in admission to the hospital; in comparison, 2% of the non-hurricane-related injury visits were admitted. Adults (19–59 years old) represented 55% of the hurricane-related visits and 40% of the non-hurricane-related visits.
Among hurricane-related injury visits, the types of injury most frequently reported were abrasions, lacerations, and cuts (50%), and sprains or strains (16%). The most frequently reported mechanisms of injury for the hurricane-related visits were being hit by or against an object (30%), falls, slips, and trips (20%), the use of machinery, tools, or equipment (20%), and foreign bodies (13%) (see Table 1). For non-hurricane-related visits, the types of injury most frequently reported were also abrasions, lacerations, and cuts (42%), and sprains or strains (15%). The mechanisms of injury most frequently reported for non-hurricane-related visits were falls, slips, and trips (50%) and being hit by or against an object (14%). A higher proportion of participants with hurricane-related injury visits were male compared with non-hurricane-related injury visits (66% vs 49%, respectively; P = 0.017) (see Table 1).
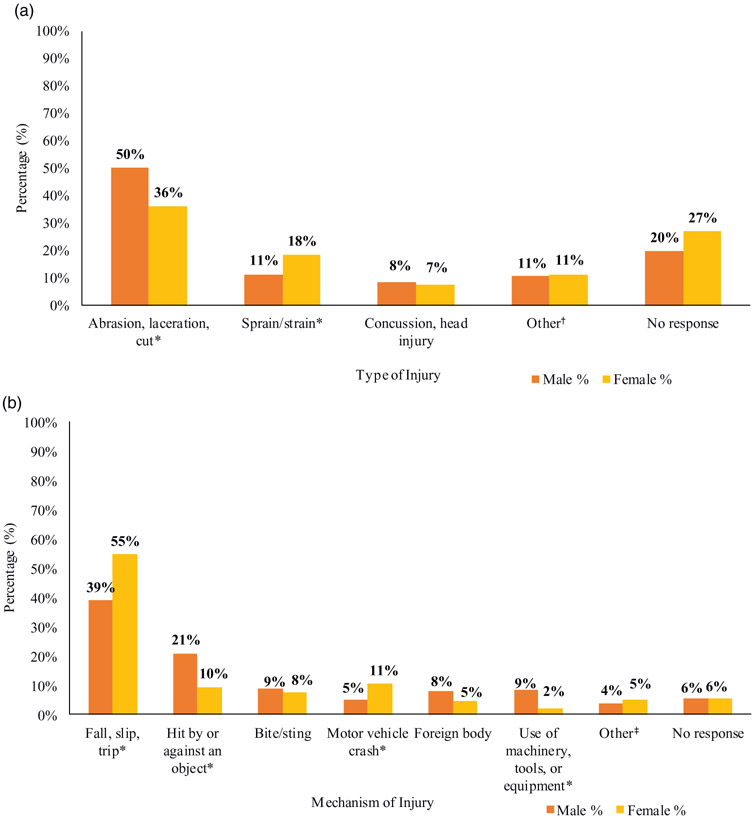
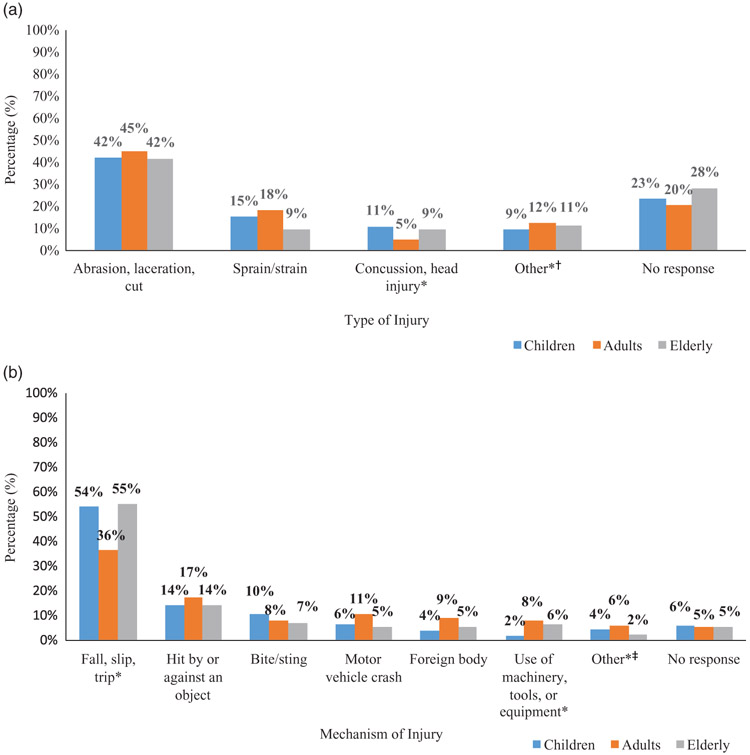
Abrasion, lacerations, and cuts accounted for a higher proportion of injuries reported by males (50% of injuries) than were reported by females (36% of injuries; P < 0.05). Falls, slips, and trips accounted for a higher proportion of injuries reported by females (55% of injuries) than were reported by males (39% of injuries; P < 0.05) (Figure 2). No statistically significant gender differences were observed in the types and mechanisms of injury that involved head injuries, fractures, bites/stings, burns, heat/cold exposure, drowning, or poisoning. Concussions and head injuries were more commonly reported by children (11%) and the elderly (9%) than were reported by adults (5%) (P = 0.048), while abrasions, lacerations, and cuts were reported by the members of all of the age groups in similar proportions (Figure 3). Adult males reported all of the avulsions or amputations (n = 4). In reference to mechanism of injury, injured children and injured elderly patients reported similar percentages of falls, slips, and trips with 54% and 55%, respectively, with only 36% reported by adults (P < 0.001). Adults reported the highest proportion of injuries sustained while using machinery, tools, or equipment (8%; P = 0.015).
Figure 2. Type (2a) and Mechanism (2b) of Injury by Sex Among All Enrolled Participants, Post-Hurricane Maria Surveillance System, Ponce, October 2017–March 2018.
*Significant difference between men and women, P < 0.05.
†Type of injury “other” includes: avulsion, amputation, fracture, or no response.
‡Mechanism of injury “other” includes: poisoning, burn, violence/assault, non-fatal drowning/submersion, cold/heat exposure, electric shock
Figure 3. Type (3a) and Mechanism (3b) of Injury by Age Among All Enrolled Participants, Post-Hurricane Maria Surveillance System, Ponce, October 2017–March 2018.
*Significant differences by age, P < 0.05.
†Type of injury “other” includes: avulsion, amputation, fracture.
‡Mechanism of injury “other” includes: poisoning, burn, violence/assault, non-fatal drowning/submersion, cold/heat exposure, electric shock.
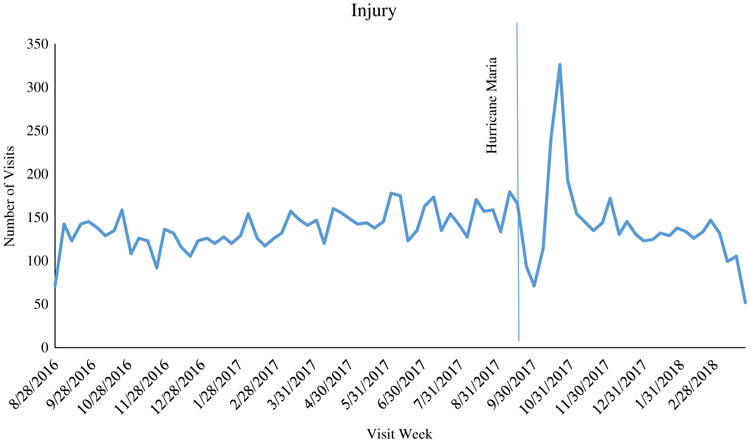
From August 2016 to September 2017, the number of injury visits remained fairly steady, with a sharp drop in the number of visits during and immediately after the hurricane. The number of visits began to increase above previous levels beginning in early October, with a peak in injury visits in the week of October 22, 2017. Six weeks after the hurricane, the number of injury visits was similar to what was being reported before the hurricane (Figure 4).
Figure 4.
Injury Visits From Electronic Medical Records Before and After Hurricane Maria Seen at San Lucas Episcopal Hospital and CEMI, Ponce, Southern Puerto Rico, August 2016–March 2018.
DISCUSSION
Our study describes the frequency, types, and mechanisms of injuries and the characteristics of the patients who reported them, as well as observed injury patterns in the months following Hurricane Maria. We found that the most common types of injuries included abrasions, lacerations, or cuts; sprains or strains; and concussions or head injuries. These types of injuries may reflect the activities frequently undertaken and hazards typically encountered in the early response after a major disaster and are similar to the types of injury reported in the medical literature as usually taking place after a natural disaster.10-12 With injuries reported by approximately 1 in 10 of the patients enrolled in our study, this clinical presentation was an important reason for the need for emergency care after Hurricane Maria. The proportion of all visits that were linked to injuries was highest after the disaster and continued in a descending trend toward the end of the 6-month surveillance period. As injury visits decreased, more patients sought emergency care for other health concerns, including acute illnesses and complications of chronic disease.
The EMR data collected at the hospital and outpatient clinic from before and after the hurricane also indicated that there was an increase in the number of injury visits after Hurricane Maria. The EMR data demonstrated a steep drop and subsequent increase in injury cases after the hurricane, with injury-related visit numbers going back to pre-hurricane levels several weeks after the hurricane. The increase in visit numbers after the hurricane was likely due to increases in injuries after the storm, but also to the closure of other, smaller health care facilities after the hurricane, with the result (in both cases) that more patients sought care at our facilities.
This study’s findings are similar to those of other studies on the mechanisms of injury and their distribution by sex and age. However, differences in location,13,14 design,2 timing of data collection after the disaster, and data collection tools10,14,15 make comparisons challenging. The most frequent mechanisms of injury (falls, slips, and trips) seen in the months following Hurricane Maria were also the most frequently reported after hurricanes Gustav, Ike, and Sandy.10,13 In our analyses, a higher proportion of injured women than men reported falling and motor vehicle crashes as the mechanisms of their injuries. A higher proportion of injured men (than women) reported foreign bodies, operating machinery, and being hit by an object as their mechanism of injury. In contrast with previously reported data, a higher proportion of injured women than injured men reported sprains or strains as their type of injury.10 Some of the differences by sex may be linked to the different responses of and clean-up activities performed by men and women after the hurricane. A study after Hurricane Andrew reported that the activities performed by women were more likely to take place in the household and be related to caring for family, while men were in charge of external rebuilding tasks.16 Other studies have reported that response and recovery workers experience particular types of injury and health problems (falls, cuts, struck-by injuries, overexertion/heat stress, and sunburn).12,15
In the overall study population, more than half of the injured children and injured elderly participants reported a fall as a mechanism of injury. In addition, injured children reported a higher proportion of head injuries than injured adults did. The World Health Organization has identified older adults as having an increased risk of falls.17 Falls are also a major public health problem, leading to increased morbidity and mortality.17 Our post-hurricane data also suggest that the elderly are at increased risk of falls compared with adults, and indeed may be particularly vulnerable after a hurricane, in which loss of power, debris in the area, poor road and/or sidewalk conditions, and slippery floors create additional hazards.
Our study had some limitations. The syndromic surveillance system was implemented almost a month after Hurricane Maria made landfall, meaning that early injury-related visits were not recorded. This likely resulted in an underestimation of the injuries that occurred during and in the rebuilding phase immediately after the hurricane. However, the EMR data indicate that there was a steep drop in injury-related visits immediately after the hurricane, so the number of cases missed may have been small. By design, our staff enrolled participants during peak ED visit hours (8:00 AM to 11:00 PM), which is when trauma is more likely to occur; however, this is still an underestimation because staff was not available around the clock to enroll patients. Finally, the determination of whether a visit was hurricane-related and occurred because of work involving disaster response and rebuilding efforts was self-reported data. This may have resulted in an underestimation of hurricane-related visits.
The study had several strengths. This injury surveillance study is the first such study performed following a hurricane in Puerto Rico. The study was implemented in a hospital system using a previously established and validated research platform for acute febrile illness surveillance, a supported collaboration with the CDC. The study staff included experienced interviewers trained for study data collection. Reports from the surveillance system were distributed weekly to stakeholders, including clinicians and hospital management staff at SLEH, CEMI, and the CDC. Reports of notifiable diseases, such as leptospirosis and vector-borne diseases, were shared within 48 hours with the Puerto Rico Department of Health. The study recruited a large number of participants and, unlike other studies, was able to collect the participants’ dispositions.
CONCLUSION
This surveillance system was developed in the aftermath of a major natural disaster, Hurricane Maria, and documented, for the first time in Puerto Rico, injury trends after such a disaster. Our findings have implications for public health prevention, as well as for emergency preparedness.
Hospitals and other health care facilities should prepare for the increased strain on wound care resources due to the increased numbers of skin repairs and increases in the need for general wound care after a hurricane, which may extend into the weeks and months beyond the immediate aftermath. After a natural disaster, a reasonable supply of injury-related immunizations such as the tetanus vaccine,14 injury-related medications such as antibacterial and anti-inflammatory agents, and pain medications is needed in the ED to ensure that proper treatment and supplies will be available to injured patients. These interventions should be administered under the appropriate indications and, in the case of immunizations, based on an individual’s tetanus vaccine history to avoid overuse. In terms of public health and injury prevention, educational campaigns should include instructions and reminders about injury risks during the cleanup and rebuilding phase.
Both electronic and manual formats for syndromic surveillance data collection should be available, because prolonged power outages and lack of availability of EMR could make electronic data collection difficult or impossible immediately after a natural disaster. Furthermore, a validated and standardized paper form can be used in places where electronic data gathering is not routinely possible in non-disaster conditions.
The information collected in this study can be used by public health officials and emergency medicine providers when preparing for future hurricanes or providing emergency care during and after a disaster response. Local capacity building and strengthening collaborations leave the hospital and public health system better prepared for future public health emergencies or disasters in which injury surveillance may play a critical role in planning and response activities.
Acknowledgments
We would like to thank the personnel from Saint Luke’s Episcopal Hospital (especially the Emergency Medicine Residency Program) and the Centro de Emergencia y Medicina Integrada for allowing us to implement the syndromic surveillance system in the ED. We would also like to recognize those of the Ponce Health Sciences University/Ponce Research Institute (including Bob Ritchie of the Publications Office) and the Centers for Disease Control and Prevention for their collaboration, the Sentinel Enhanced Dengue Surveillance System staff, and the ZiPer study staff for their collaboration during data collection, data entry, and data cleaning. (Note: None of the previous organizations received compensation for their efforts.)
Footnotes
Conflict of Interest
The authors have no conflicts of interest to declare. The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the CDC.
Contributor Information
Verónica M. Frasqueri-Quintana, Ponce Health Sciences University, Saint Luke’s Episcopal Hospital, Ponce, Puerto Rico.
Carene A. Oliveras García, Ponce Health Sciences University, Saint Luke’s Episcopal Hospital, Ponce, Puerto Rico.
Laura E. Adams, Centers for Disease Control and Prevention, Division of Vector-Borne Diseases, Dengue Branch, San Juan, Puerto Rico.
Xiomara Torres-Figueroa, Ponce Health Sciences University, Saint Luke’s Episcopal Hospital, Ponce, Puerto Rico.
Rafael Iván Iriarte, Ponce Health Sciences University, Saint Luke’s Episcopal Hospital, Ponce, Puerto Rico.
Kyle Ryff, Centers for Disease Control and Prevention, Division of Vector-Borne Diseases, Dengue Branch, San Juan, Puerto Rico.
Liliana Sánchez-González, Centers for Disease Control and Prevention, Division of Vector-Borne Diseases, Dengue Branch, San Juan, Puerto Rico.
Vivian Pérez Gómez, Ponce Health Sciences University, Saint Luke’s Episcopal Hospital, Ponce, Puerto Rico.
Nicole M. Pérez-Rodríguez, Ponce Health Sciences University, Saint Luke’s Episcopal Hospital, Ponce, Puerto Rico.
Luisa I. Alvarado, Ponce Health Sciences University, Saint Luke’s Episcopal Hospital, Ponce, Puerto Rico.
Gabriela Paz-Bailey, Centers for Disease Control and Prevention, Division of Vector-Borne Diseases, Dengue Branch, San Juan, Puerto Rico.
REFERENCES
- 1.Heron M Deaths: Leading Causes for 2016. Hyattsville, MD: National Vital Statistics Report; 2018. [PubMed] [Google Scholar]
- 2.Horan JM, Mallonee S. Injury surveillance. Epidemiol Rev. 2003;25:24–42. [DOI] [PubMed] [Google Scholar]
- 3.Rivara FP, Grossman DC, Cummings P. Injury prevention. First of two parts. N Engl J Med. 1997;337(8):543–548. [DOI] [PubMed] [Google Scholar]
- 4.Saulnier DD, Brolin Ribacke K, von Schreeb J. No calm after the storm: a systematic review of human health following flood and storm disasters. Prehosp Disaster Med. 2017;32(5):568–579. [DOI] [PubMed] [Google Scholar]
- 5.Brunkard J, Namulanda G, Ratard R. Hurricane Katrina deaths, Louisiana, 2005. Disaster Med Public Health Prep. 2008;2(4):215–223. [DOI] [PubMed] [Google Scholar]
- 6.Pasch RJ, Penny AB, Berg R. National Hurricane Center Tropical Cyclone Report Hurricane Maria; 2017. [Google Scholar]
- 7.Zorrilla CD. The view from Puerto Rico – Hurricane Maria and its aftermath. N Engl J Med. 2017;377(19):1801–1803. [DOI] [PubMed] [Google Scholar]
- 8.Ciottone GR. Disaster Medicine. 2nd ed. Philadelphia, PA: Elsevier; 2016: 13–26 (vol 3-4). [Google Scholar]
- 9.Schnall AH, Wolkin AF, Noe R, et al. Evaluation of a standardized morbidity surveillance form for use during disasters caused by natural hazards. Prehosp Disaster Med. 2011;26(2):90–98. [DOI] [PubMed] [Google Scholar]
- 10.Brackbill RM, Caramanica K, Maliniak M, et al. Nonfatal injuries 1 week after Hurricane Sandy – New York city metropolitan area, October 2012. Morb Mortal Wkly Rep. 2014;63(42):950–954. [PMC free article] [PubMed] [Google Scholar]
- 11.Platz E, Cooper HP, Silvestri S, et al. The impact of a series of hurricanes on the visits to two central Florida emergency departments. J Emerg Med. 2007;33(1):39–46. [DOI] [PubMed] [Google Scholar]
- 12.Marshall EG, Lu SE, Shi Z, et al. Work-related unintentional injuries associated with Hurricane Sandy in New Jersey. Disaster Med Public Health Prep. 2016;10(3):394–404. [DOI] [PubMed] [Google Scholar]
- 13.Noe RS, Schnall AH, Wolkin AF, et al. Disaster-related injuries and illnesses treated by American Red Cross disaster health services during Hurricanes Gustav and Ike. South Med J. 2013; 106(1): 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Morbidity surveillance after Hurricane Katrina – Arkansas, Louisiana, Mississippi, and Texas, September 2005. Morb Mortal Wkly Rep. 2006;55(26):727–731. [PubMed] [Google Scholar]
- 15.Rusiecki JA, Thomas DL, Chen L, et al. Disaster-related exposures and health effects among US Coast Guard responders to Hurricanes Katrina and Rita: a cross-sectional study. J Occup Environ Med. 2014;56(8): 820–833. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Gender and health in natural disasters. 2005. http://wvw.who.int/gender. Accessed September 6, 2018.
- 17.World Health Organization. Falls. 2018. http://www.who.int/news-room/fact-sheets/detail/falls. Accessed September 6, 2018.