Abstract
Objectives
To assess the association between neonatal BCG vaccination and mortality between 28 days and 3 years of age among tuberculosis (TB)-exposed and TB-unexposed children.
Design
Prospective cohort study.
Setting
Bandim Health Project runs an urban Health and Demographic Surveillance site in Guinea-Bissau with registration of mortality, vaccination status and TB cases.
Participants
Children entered the analysis when their vaccination card was inspected after 28 days of age and remained under surveillance to 3 years of age. Children residing in the same house as a TB case were classified as TB-exposed from 3 months prior to case registration to the end of follow-up.
Methods
Using Cox-proportional hazards models with age as underlying time scale, we compared mortality of children with and without neonatal BCG between October 2003 and September 2017.
Main outcome measure
HR for neonatal BCG compared with no neonatal BCG by TB-exposure status.
Results
Among the 39 421 children who entered the analyses, 3022 (8%) had observation time as TB-exposed. In total, 84% of children received neonatal BCG. Children with neonatal BCG had lower mortality both in TB-exposed (adjusted HR: 0.57 (0.26 to 1.27)) and in TB-unexposed children (HR: 0.57 (95% CI 0.47 to 0.69)) than children without neonatal BCG. Children exposed to TB had higher mortality than TB-unexposed children if they had not received neonatal BCG.
Conclusion
Neonatal BCG vaccination was associated with lower mortality among both TB-exposed and TB-unexposed children, consistent with neonatal BCG vaccination having beneficial non-specific effects. Interventions to increase timely BCG vaccination are urgently warranted.
Keywords: epidemiology, public health, tuberculosis, paediatric infectious disease & immunisation, public health
Strengths and limitations of this study.
The study was conducted in Bandim Health Project’s urban Health and Demographic Surveillance Site with continuous registration of births, deaths and vaccination status and linked with the tuberculosis (TB) surveillance database, which allowed classification of households as TB-exposed and TB-unexposed.
More than 39 000 children entered the analysis; all children entering the analysis had their vaccination status assessed after the neonatal period.
The analyses were adjusted for potential confounders; however, residual confounding cannot be excluded.
Some TB cases may be undiagnosed, leading to some TB-exposed children being classified as TB-unexposed. We expect any misclassification to be independent of timing of BCG vaccination.
Introduction
BCG vaccine was developed to protect against tuberculosis (TB) and remains the only approved TB vaccine.1 The efficacy of the BCG vaccine to protect against TB has varied between different trials.2 However, trials of neonatal BCG vaccination consistently find that BCG is associated with reduced TB incidence.2
BCG is recommended at birth in countries with high burden of TB.1 According to WHO/UNICEF estimates, 88% of children are BCG vaccinated in countries where BCG is part of the routine vaccination programme.3 However, WHO/UNICEF coverage estimates are based on coverage at 12 months of age, and BCG is often delayed in low-income countries.4 5 If delayed BCG vaccination is associated with lower vaccine efficacy, delays may be critical.
Vaccines are designed to protect against specific target diseases. Increasing evidence supports that vaccines have additional effects affecting the susceptibility of untargeted infections, and these have been coined non-specific effects (NSEs), and increasing evidence suggests that BCG affects mortality by more than can be explained by the protection against TB,6 7 that is, BCG may have beneficial NSE. Three randomised trials in low-weight children in Guinea-Bissau found that BCG vaccination at birth was associated with 38% (17%–54%) lower neonatal mortality compared with children not BCG vaccinated at birth.8 Already 3 days after enrolment, BCG was associated with 45% (7%–68%) lower mortality compared with unvaccinated children,8 suggesting that even small delays in BCG vaccination may be important for survival.
A potential effect of early BCG on childhood mortality could be due to prevention of TB, NSEs of BCG or a combination. If the effect of BCG was merely specific, we should expect strong effects among children exposed to TB9 and no effect in children not exposed to TB.
The main objective of this study was to assess the association between neonatal BCG versus later BCG vaccination and mortality by registered exposure to TB. We furthermore assessed the association between neonatal BCG vaccination and positive tuberculin skin test (TST) reactions by registered exposure to TB.
Methods
Setting and study population
Bandim Health Project (BHP) runs a Health and Demographic Surveillance Site (HDSS) in six suburban districts in Bissau, the capital of Guinea-Bissau. Children are followed through trimonthly home visits until 3 years of age. At the home visits, a field assistant collects information on vital status, measures mid-upper-arm circumference and registers vaccination status by transcribing information from the child’s vaccination card. Each month, field assistants conduct home visits to follow pregnant women and register new births. Children above 3 years of age and adults are followed through censuses conducted every 2–5 years.
The BCG vaccines used in Guinea-Bissau have been provided by UNICEF and mainly the Russian strain has been used. However, during large periods within the study period, the BHP provided vaccines for the study area; these were the BCG-Denmark strain purchased at the Statens Serum Institut, Denmark.
Since 1996, all diagnosed TB cases above 15 years of age living in the study area have been registered and followed.10 In 2003, a register of information on all patients with TB from the study area was established, making it possible to identify houses with exposure to TB. We defined inhabitants as exposed to TB from 3 months prior to diagnosis of a TB case in the house (with several households) and until 2 weeks after diagnosis, to account for delay in diagnosis, which we, in line with previous studies,11 12 assumed was a median of 3 months. Children were classified as TB-exposed from three months prior to registration of the index case and remained classified as TB-exposed throughout the follow-up period. We expect some TB cases to be undiagnosed. Thus, some children classified as TB-unexposed may have been exposed.
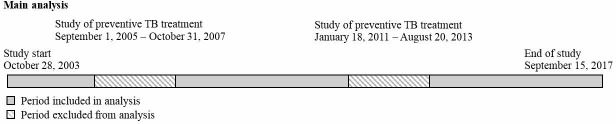
Preventive treatment to TB-exposed children is not routinely provided in Guinea-Bissau. Between 1 September 2005 and 31 October 2007, and between 18 January 2011 and 20 August 2013, studies of the effect of preventive treatment to TB-exposed children were conducted in the BHP study area.12 13 We excluded these periods for all children in the present study (figure 1). Thus, we included children who had their vaccination status assessed after 28 days of age between 28 October 2003 (start of the TB registry) and 15 September 2017 excluding periods with studies of preventive TB treatment. From July 2002 to April 2004, a randomised trial of BCG-revaccination at 19 months of age was conducted in the study area; we therefore censored follow-up at 19 months of age for children eligible for the BCG-revaccination trial.14
Figure 1.
Timeline of study period. TB, tuberculosis.
Between start of study and 1 July 2008, a sample of children living in the study area were TST tested using the Mantoux method with an intradermal application of 0.1 mL of purified protein derivatives (PPD) (2 tuberculin units RT23, Statens Serum Institut, Denmark) in the forearm at ages 6 and 12 months. The PPD reactions were measured after 48–72 hours using a ruler and ballpoint technique to measure two diameters.15 Among children with measured PPD reactions, we assessed the effect of neonatal BCG vaccination versus later BCG vaccination on PPD reactions using cut-offs of 10 mm and 15 mm.
Statistical analyses
We compared baseline characteristics of children with and without neonatal BCG in TB-exposed and TB-unexposed children using χ² and paired t-tests. We also compared baseline characteristics of children registered and not registered as TB-exposed.
In Cox-proportional hazards models with age as underlying time scale, we compared mortality rates (MRs) of children with neonatal BCG with MRs of children without neonatal BCG (delayed BCG or no BCG) separately for TB-exposed and TB-unexposed children, allowing for different baseline hazards according to sex and place of birth (maternity ward, health centre or home). Children entered the analysis the first time their vaccination status was assessed at a home visit after the neonatal period. Observation time was split at the first time-point, where the child was considered to be TB-exposed. Thus, TB-exposed children could contribute with observation time in the TB-unexposed group until 3 months prior to diagnosis of a coinhabitant. To control for potential confounding, we assessed whether baseline characteristics (table 1) changed the estimate by including the factors in the analysis one by one. We adjusted for baseline characteristics that changed the estimate by more than 5%.
Table 1.
Baseline characteristics of children by neonatal BCG and registered TB-exposure status
| TB-exposed children | TB-unexposed children | |||||||
| Total | Neonatal BCG (n %) | No neonatal BCG (n %) | P value | Total | Neonatal BCG (n %) | No neonatal BCG (n %) | P value | |
| Number | 3022 | 2605 (86.2%) | 417 (13.8%) | 36 399 | 30 532 (83.9%) | 5867 (16.1%) | ||
| Sex* | 0.849 | 0.35 | ||||||
| Male | 1574 | 1355 (52.0%) | 219 (52.5%) | 18 421 | 15 485 (50.7%) | 2936 (50.1%) | ||
| Female | 1448 | 1250 (48.0%) | 198 (47.5%) | 17 977 | 15 047 (49.3%) | 2930 (49.9%) | ||
| Twin† | <0.0001 | <0.0001 | ||||||
| Yes | 99 | 70 (2.7%) | 29 (7.0%) | 1233 | 826 (2.7%) | 407 (7.0%) | ||
| No | 2921 | 2534 (97.3%) | 387 (93.0%) | 35 114 | 29 669 (97.3%) | 5445 (93.0%) | ||
| Season of birth | 0.376 | 0.024 | ||||||
| Rainy season | 1474 | 1279 (49.1%) | 195 (46.8%) | 17 795 | 15 006 (49.1%) | 2789 (47.5%) | ||
| Dry season | 1548 | 1326 (50.9%) | 222 (53.2%) | 18 604 | 15 526 (50.9%) | 3078 (52.5%) | ||
| Birth location‡ | <0.0001 | <0.0001 | ||||||
| Home | 902 | 721 (27.7%) | 181 (43.6%) | 10 030 | 7463 (24.5%) | 2567 (44.1%) | ||
| Health centre | 1329 | 1259 (48.4%) | 70 (16.9%) | 16 171 | 15 285 (50.2%) | 886 (15.2%) | ||
| Hospital | 647 | 512 (19.7%) | 135 (32.5%) | 7923 | 6001 (19.7%) | 1922 (33.0%) | ||
| Other | 139 | 110 (4.2%) | 29 (7.0%) | 2179 | 1727 (5.7%) | 452 (7.8%) | ||
| Year of birth | 0.550 | <0.0001 | ||||||
| 2000–2006 | 1010 | 866 (33.2%) | 144 (34.5%) | 11 410 | 9430 (30.9%) | 1980 (33.7%) | ||
| 2007–2011 | 999 | 856 (32.9%) | 143 (34.3%) | 12 654 | 10 625 (34.8%) | 2029 (34.6%) | ||
| 2012–2017 | 1013 | 883 (33.9%) | 130 (31.2%) | 12 335 | 10 477 (34.3%) | 1858 (31.7%) | ||
| Number of pregnancies§ | 0.694 | <0.0001 | ||||||
| 1 | 838 | 723 (27.8%) | 115 (27.6%) | 10 972 | 9198 (30.1%) | 1774 (30.3%) | ||
| 2–3 | 1249 | 1083 (41.6%) | 166 (39.8%) | 15 316 | 12 987 (42.6%) | 2329 (39.7%) | ||
| 4 or more | 934 | 798 (30.6%) | 136 (32.6%) | 10 095 | 8336 (27.3%) | 1759 (30.0%) | ||
| Maternal age¶ | 2939 | 26.5 (6.25) | 25.6 (6.40) | 0.005 | 34 712 | 26.2 (6.22) | 25.3 (6.38) | <0.0001 |
| Education of caretaker** | <0.0001 | <0.0001 | ||||||
| 0 year | 772 | 639 (26.4%) | 133 (36.4%) | 9747 | 7637 (26.5%) | 2110 (39.8%) | ||
| 1–4 years | 384 | 330 (13.6%) | 54 (14.8%) | 4530 | 3686 (12.8%) | 844 (15.9%) | ||
| +4 years | 1629 | 1451 (60.0%) | 178 (48.8%) | 19 865 | 17 523 (60.7%) | 2342 (44.2%) | ||
| Suburb | 0.138 | <0.0001 | ||||||
| Bandim | 1426 | 1214 (46.6%) | 212 (50.8%) | 16 010 | 13 194 (43.2%) | 2816 (48.0%) | ||
| Belem/Mindara | 502 | 445 (17.1%) | 57 (13.7%) | 5556 | 4877 (16.0%) | 679 (11.6%) | ||
| Cuntum | 1094 | 946 (36.3%) | 148 (35.5%) | 14 833 | 12 461 (40.8%) | 2372 (40.4%) | ||
| Ethnicity†† | 0.001 | <0.0001 | ||||||
| Pepel | 819 | 685 (26.7%) | 134 (32.4%) | 10 007 | 8161 (27.0%) | 1846 (31.7%) | ||
| Balanta | 290 | 244 (9.5%) | 46 (11.1%) | 2947 | 2447 (8.1%) | 500 (8.6%) | ||
| Mandinga/Fula | 858 | 726 (28.3%) | 132 (31.9%) | 10 943 | 9038 (29.9%) | 1905 (32.7%) | ||
| Manjaco/Mancanha | 596 | 538 (21.0%) | 58 (14.0%) | 6464 | 5688 (18.8%) | 776 (13.3%) | ||
| Others | 417 | 373 (14.5%) | 44 (10.6%) | 5743 | 4941 (16.3%) | 802 (13.8%) | ||
| Socioeconomic factors | ||||||||
| Type of roof‡‡ | 0.330 | <0.0001 | ||||||
| Straw | 93 | 77 (3.0%) | 16 (3.9%) | 922 | 728 (2.4%) | 194 (3.3%) | ||
| Hard | 2919 | 2520 (97.0%) | 399 (96.1%) | 35 422 | 29 769 (97.6%) | 5653 (96.7%) | ||
| Toilet§§ | <0.0001 | <0.0001 | ||||||
| None | 11 | 6 (0.2%) | 5 (1.2%) | 95 | 75 (0.2%) | 20 (0.3%) | ||
| Latrine | 2618 | 2240 (86.3%) | 378 (91.1%) | 30 210 | 24 959 (81.9%) | 5251 (89.8%) | ||
| Inside | 381 | 349 (13.4%) | 32 (7.7%) | 6007 | 5428 (17.8%) | 579 (9.9%) | ||
| Electricity*** | <0.0001 | <0.0001 | ||||||
| Yes | 950 | 859 (33.0%) | 91 (21.9%) | 12 841 | 11 437 (37.5%) | 1404 (24.0%) | ||
| No | 2067 | 1742 (67.0%) | 325 (78.1%) | 23 505 | 19 060 (62.5%) | 4445 (76.0%) | ||
TB-exposed children are only represented in the TB-exposed group despite some children also contribute observation time as not TB-exposed to avoid comparing a child with itself.
*Missing information for 0 TB-exposed children and 1 TB-unexposed child.
†Missing information for 2 TB-exposed children and 52 TB-unexposed children.
‡Missing information for 5 TB-exposed children and 96 TB-unexposed children.
§Missing information for 1 TB-exposed children and 16 TB-unexposed children.
¶Missing information for 83 TB-exposed children and 1687 TB-unexposed children.
**Missing information for 237 TB-exposed children and 2257 TB-unexposed children.
††Missing information for 42 TB-exposed children and 295 TB-unexposed children.
‡‡Missing information for 10 TB-exposed children and 55 TB-unexposed children.
§§Missing information for 12 TB-exposed children and 87 TB-unexposed children.
¶¶Missing information for 5 TB-exposed children and 53 TB-unexposed children.
In a secondary analysis, we explored whether the effect of neonatal BCG differed by timing of BCG within the neonatal period; thus, we divided children with neonatal BCG in two groups: children with early neonatal BCG (vaccinated within 7 days after birth) and children with late neonatal BCG (vaccinated between day 8 and day 28).
In sensitivity analyses, we: (1) excluded all children, who potentially had been exposed to preventive TB treatment as part of the aforementioned studies (online supplementary figure 1); (2) restricted the analysis to children with a registered BCG vaccine (ie, allowing a child only to contribute time at risk from the first visit at which a BCG vaccine was registered, therefore, children with no registered BCG vaccine would not enter the analysis); (3) extended follow-up to 5 years of age; (4) excluded twins, as these are more likely to be low-birth-weight (LBW) children and thus receive delayed BCG; (5) stratified the analysis by LBW status for the subset of children for whom we had information on birth weight.
bmjopen-2019-035595supp001.pdf (53.7KB, pdf)
BCG vaccination may cause a transient weak response to PPD,16 but reactions above 15 mm would be less likely to be caused by BCG.17 Using log-binomial regression, we compared the prevalence of positive TST in children with neonatal BCG with children without neonatal BCG among TB-exposed and TB-unexposed children, respectively. We limited comparison to children BCG vaccinated prior to TST assessment and evaluated PPD reaction at age 6 and 12 months using cut-offs of 10 mm and 15 mm.
Ethical considerations
The data used for this study were mostly obtained from BHP’s urban HDSS, which has been following women and children since 1978, where data collection was initiated at the request of the Ministry of Health in Guinea-Bissau. Further already collected data on TST was obtained through previous studies approved by the Guinean Ethics Committee. Oral consent was obtained from mother/guardian of the children prior to TST. As no additional data were collected for this study, no further ethical approval was needed.
Patient and public involvement
The communities were involved in locating households, when the HDSS was set up and contributed information allowing tracing of internal migrants between suburbs throughout the study period. No participant was involved in setting the research question or the outcome measure, nor were they involved in developing plans for recruitment, design or implementation of the study. No participant was asked to advise on interpretation or writing up the results. The results are disseminated to the national public health institute. There are no plans to disseminate the results of the research to study participants or the community.
Results
A total of 39 421 children contributed time at risk, and among these 3022 had observation time while living in houses of registered TB cases. Among children with a vaccination card seen after 28 days, 33 137 (84%) had received neonatal BCG. The median age of vaccination in the neonatal BCG group was 2 days (IQR: 1–10). Among the 6284 children not BCG vaccinated in the neonatal period, 5450 (87%) had a BCG vaccine registered at some point of time during the follow-up period (median age of vaccination: 48 days (IQR: 36–69)).
Baseline characteristics
We compared baseline characteristics of children with and without neonatal BCG according to TB-exposure status. In this large dataset, most statistically significant differences were small absolute differences. In both groups, mothers of children with neonatal BCG were better educated, older and had better socioeconomic status (toilet, electricity, among not TB-exposed children also type of roof). Children with neonatal BCG were more likely to be born at a health facility and less likely to be twins. Ethnic groups also varied between children with and without neonatal BCG. Among TB-unexposed children, the distribution of season of birth, year of birth, number of pregnancies and suburb differed between neonatal BCG vaccinated and not neonatal BCG vaccinated children (table 1).
Several baseline characteristics were statistically significant different between TB-exposed and TB-unexposed children (birth location, number of pregnancies, maternal age, suburb, ethnicity and socioeconomic factors) (table 2).
Table 2.
Baseline characteristics of children registered as exposed to and not exposed to TB
| TB-exposed children vs TB-unexposed children | ||||
| Total | TB-exposed (n %) | TB-unexposed (n %) | P value | |
| Number | 39 421 | 3022 (7.7%) | 36 399 (92.3%) | |
| Sex* | 0.119 | |||
| Male | 19 995 | 1574 (52.1%) | 18 421 (50.6%) | |
| Female | 19 425 | 1448 (47.9%) | 17 977 (49.4%) | |
| Twin† | 0.739 | |||
| Yes | 1332 | 99 (3.3%) | 1233 (3.4%) | |
| No | 38 035 | 2921 (96.7%) | 35 114 (96.6%) | |
| Season of birth | 0.905 | |||
| Rainy season | 19 269 | 1474 (48.8%) | 17 795 (48.9%) | |
| Dry season | 20 152 | 1548 (51.2%) | 18 604 (51.1%) | |
| Birth location‡ | 0.002 | |||
| Home | 10 932 | 902 (29.9%) | 10 030 (27.6%) | |
| Health centre | 17 500 | 1329 (44.1%) | 16 171 (44.5%) | |
| Hospital | 8570 | 647 (21.4%) | 7923 (21.8%) | |
| Other | 2318 | 139 (4.6%) | 2179 (6.0%) | |
| Year of birth | 0.043 | |||
| 2000–2006 | 12 420 | 1010 (33.4%) | 11 410 (31.1%) | |
| 2007–2011 | 13 653 | 999 (33.1%) | 12 654 (34.5%) | |
| 2012–2017 | 13 348 | 1013 (33.5%) | 12 335 (33.6%) | |
| Number of pregnancies§ | <0.0001 | |||
| 1 | 11 810 | 838 (27.7%) | 10 972 (30.2%) | |
| 2–3 | 16 565 | 1249 (41.3%) | 15 316 (42.1%) | |
| 4 or more | 11 029 | 934 (30.9%) | 10 095 (27.7%) | |
| Maternal age¶ | 37 651 | 26.4 (6.28) | 26.1 (6.26) | 0.008 |
| Education of caretaker** | 0.553 | |||
| 0 year | 10 519 | 772 (27.7%) | 9747 (28.5%) | |
| 1–4 years | 4914 | 384 (13.8%) | 4530 (13.3%) | |
| +4 years | 21 494 | 1629 (58.5%) | 19 865 (58.2%) | |
| Suburb | <0.0001 | |||
| Bandim | 17 436 | 1426 (47.2%) | 16 010 (44.0%) | |
| Belem/Mindara | 6058 | 502 (16.6%) | 5556 (15.3%) | |
| Cuntum | 15 927 | 1094 (36.2%) | 14 833 (40.8%) | |
| Ethnicity†† | <0.0001 | |||
| Pepel | 10 826 | 819 (27.5%) | 10 007 (27.7%) | |
| Balanta | 3237 | 290 (9.7%) | 2947 (8.2%) | |
| Mandinga/Fula | 11 801 | 858 (28.8%) | 10 943 (30.3%) | |
| Manjaco/Mancanha | 7060 | 596 (20.0%) | 6464 (17.9%) | |
| Others | 6160 | 417 (14.0%) | 5743 (15.9%) | |
| Socioeconomic factors | ||||
| Type of roof‡‡ | 0.067 | |||
| Straw | 1015 | 93 (3.1%) | 922 (2.5%) | |
| Hard | 38 341 | 2919 (96.9%) | 35 422 (97.5%) | |
| Toilet§§ | <0.0001 | |||
| None | 106 | 11 (0.4%) | 95 (0.3%) | |
| Latrine | 32 828 | 2618 (87.0%) | 30 210 (83.2%) | |
| Inside | 6388 | 381 (12.7%) | 6007 (16.5%) | |
| Electricity*** | <0.0001 | |||
| Yes | 13 791 | 950 (31.5%) | 12 841 (35.3%) | |
| No | 25 572 | 2067 (68.5%) | 23 505 (64.7%) | |
TB-exposed children are only represented in the TB-exposed group despite some children also contribute observation time as not TB-exposed to avoid comparing a child with itself.
Missing information for 58 children.
*Missing information for one child.
†Missing information for 54 children.
‡Missing information for 101 children.
§Missing information for 17 children.
¶Missing information for 1770 children.
**Missing information for 2494 children.
††Missing information for 337 children.
‡‡Missing information for 65 children.
§§Missing information for 99 children.
TB, tuberculosis.
Effect of neonatal BCG on mortality among children registered as TB-exposed
We included 3022 TB-exposed children in the analyses, among these 2605 (86%) were neonatally BCG vaccinated, whereas 417 (14%) were not. TB-exposed children with neonatal BCG had a MR of 12.2 per 1000 person years (PYRS, 30 deaths during 2462 PYRS), and children without neonatal BCG (delayed or no BCG) had a MR of 35.2 per 1000 PYRS (13 deaths during 369 PYRS). The HR comparing TB-exposed children with and without neonatal BCG was 0.29 (95% CI 0.14 to 0.57). Adjusting for the baseline characteristics that changed the estimate by more than 5% resulted in an adjusted hazard ratio (aHR) of 0.57 (0.26 to 1.27) (table 3). Neonatal BCG was beneficial for TB-exposed boys (aHR: 0.23 (0.08 to 0.62)), but not for TB-exposed girls (aHR: 1.61 (0.36 to 7.08)) (p=0.03) (table 4).
Table 3.
Mortality of children with and without neonatal BCG by TB-exposure status
| Number of children | MR per 1000 PYRS | HR | Adjusted HR | |
| N | (deaths/PYRS) | (95% CI) | (95% CI) | |
| TB-exposed | ||||
| Neonatal BCG | 2605 | 12.2 (30/2462) | 0.29 (0.14 to 0.57) | 0.57 (0.26 to 1.27)* |
| No neonatal BCG | 417 | 35.2 (13/369) | Ref | Ref |
| TB-unexposed † | ||||
| Neonatal BCG | 32 040 | 13.5 (533/39 608) | 0.57 (0.47 to 0.69) | |
| No neonatal BCG | 6105 | 22.8 (157/6880) | Ref | |
| Combined TB-exposed and TB-unexposed † | ||||
| Neonatal BCG | 33 137 | 13.4 (563/42 069) | 0.54 (0.45 to 0.65) | |
| No neonatal BCG | 6284 | 23.4 (170/7250) | Ref | |
All HRs were obtained from Cox-proportional hazards models with age as underlying age, allowing different baseline hazards by sex and birth location.
*Adjusted HR calculated adjusting for twin status, maternal age and year of birth among TB-exposed children, excluding 85 children (four deaths) from the analysis. The crude analysis excluding children with missing information on twin status, maternal age or year of birth yielded HR: 0.43 (0.19 to 0.93).
†No factor changed the estimate by more than 5%, and adjusted HR are therefore not presented.
MR, mortality rate; PYRS, person years; TB, tuberculosis.
Table 4.
Mortality of children with and without neonatal BCG by TB-exposure status and sex
| Number of children | MR per 1000 PYRS | HR | Adjusted HR | |
| N | (deaths/PYRS) | (95% CI) | (95% CI) | |
| TB-exposed boys | ||||
| Neonatal BCG | 1355 | 8.5 (11/1,288) | 0.19 (0.07 to 0.51) | 0.23 (0.08 to 0.62)* |
| No neonatal BCG | 219 | 35.6 (7/197) | Ref | Ref |
| TB-unexposed boys † | ||||
| Neonatal BCG | 16 268 | 13.6 (275/20,166) | 0.58 (0.45 to 0.75) | |
| No neonatal BCG | 3072 | 23.0 (80/3,478) | Ref | |
| TB-exposed girls | ||||
| Neonatal BCG | 1250 | 16.2 (19/1,174) | 0.37 (0.14 to 0.96) | 1.61 (0.36 to 7.08)* |
| No neonatal BCG | 198 | 34.7 (6/173) | Ref | Ref |
| TB-unexposed girls † | ||||
| Neonatal BCG | 15 772 | 13.3 (258/19,442) | 0.56 (0.43 to 0.73) | |
| No neonatal BCG | 3032 | 22.6 (77/3,402) | Ref | |
All HRs were obtained from Cox-proportional hazards models with age as underlying age, allowing different baseline hazards by sex and birth location.
*Adjusted HR calculated adjusting for twin status, maternal age and year of birth among TB-exposed children, excluding 85 children (four deaths) from the analysis.
†No factor changed the estimate by more than 5%, and adjusted HR are therefore not presented.
MR, mortality rate; PYRS, person years; TB, tuberculosis.
The mortality was lowest among children with early neonatal BCG (aHR compared with children with no neonatal BCG: 0.39 (0.15 to 0.98) and an aHR of 0.90 (0.36 to 2.25) for children with late neonatal BCG compared with children with no neonatal BCG) (online supplementary table 1).
Extending follow-up to 5 years of age or excluding children with no registered BCG vaccination or excluding twins from the analysis did not alter the conclusions (online supplementary table 2). Excluding children who had potentially been eligible for studies of preventive TB treatment (online supplementary figure 1) resulted in an aHR of 0.95 (95% CI 0.31 to 2.97) (online supplementary table 2). Stratifying the analysis by LBW status (<2500 g) had limited power (online supplementary table 3).
Effect of neonatal BCG on mortality among children registered as TB-unexposed
We included 38 145 children classified as TB-unexposed in this analysis, 32 040 (84%) were neonatally BCG vaccinated, and 6105 (16%) were not. Children with neonatal BCG vaccination had a MR of 13.5 per 1000 PYRS (533 deaths during 39 608 PYRS) and not neonatal BCG vaccinated children had a MR of 22.8 per 1000 PYRS (157 deaths during 6880 PYRS). Children with neonatal BCG had 43% lower mortality (HR: 0.57 (95% CI 0.47 to 0.69) compared with not neonatal BCG vaccinated children (table 3). No background factor changed the estimate by more than 5% and thus adjusted estimates are not presented. The effect of neonatal BCG did not differ by sex (p=0.87) (table 4).
The effect of BCG within the neonatal period was similar: HR: 0.59 (0.48 to 0.74) for children with early neonatal BCG compared with no neonatal BCG and HR: 0.55 (0.44 to 0.68) for children with late neonatal BCG (online supplementary table 1).
Extending follow-up to 5 years of age, excluding children with no registered BCG vaccine, excluding twins from the analysis or excluding children potentially eligible for studies of preventive TB treatment (online supplementary figure 1) did not alter the conclusions (online supplementary table 2). Stratifying the analysis by LBW status indicated that neonatal BCG was associated with an HR of 0.70 (0.44 to 1.11) in LBW children, and an HR of 0.76 (0.50 to 1.16) in normal birth-weight children (online supplementary table 3).
Mortality in TB-exposed and TB-unexposed children according to vaccination status
We also examined the effect of being TB-exposed on mortality among children with neonatal BCG and children without neonatal BCG, respectively. Among children with neonatal BCG, TB-exposed children had slightly higher mortality than TB-unexposed children (HR: 1.11 (0.77 to 1.61)). Among not neonatally BCG-vaccinated children, TB-exposed children had higher mortality (HR: 1.93 (1.10 to 3.41)) (p=0.11 for interaction between neonatal BCG and TB-exposure, table 5).
Table 5.
Mortality of TB-exposed children compared with TB-unexposed children by timing of BCG and sex
| MR per 1000 PYRS | HR | |
| (deaths/PYRS) | (95% CI) | |
| All children | ||
| Neonatal BCG | ||
| TB-exposed | 12.2 (30/2462) | 1.11 (0.77 to 1.61) |
| TB-unexposed | 13.5 (533/39 608) | Ref |
| No neonatal BCG | ||
| TB-exposed | 35.2 (13/369) | 1.93 (1.10 to 3.41) |
| TB-unexposed | 22.8 (157/6880) | Ref |
| Boys | ||
| Neonatal BCG | ||
| TB-exposed | 8.5 (11/1288) | 0.77 (0.42 to 1.41) |
| TB-unexposed | 13.6 (275/20 166) | Ref |
| No neonatal BCG | ||
| TB-exposed | 35.6 (7/197) | 1.98 (0.91 to 4.28) |
| TB-unexposed | 23.0 (80/3478) | Ref |
| Girls | ||
| Neonatal BCG | ||
| TB-exposed | 16.2 (19/1174) | 1.50 (0.94 to 2.39) |
| TB-unexposed | 13.3 (258/19 442) | Ref |
| No neonatal BCG | ||
| TB-exposed | 34.7 (6/173) | 1.90 (0.83 to 4.35) |
| TB-unexposed | 22.6 (77/3402) | Ref |
All HRs were obtained from Cox-proportional hazards models with age as underlying age, allowing different baseline hazards by sex and birth location.
Adjusted HR are not presented as no baseline factor changed the estimates by more than 5%.
MR, mortality rate; PYRS, person years; TB, tuberculosis.
We explored whether the effect differed for boys and girls. TB-exposure was associated with higher mortality for girls both with and without neonatal BCG (HR: 1.50 (0.94 to 2.39) and 1.90 (0.83 to 4.35), respectively). In boys, TB-exposure was associated with higher mortality for children without neonatal BCG (HR: 1.98 (0.91 to 4.28)), whereas this was not the case for children with neonatal BCG (HR: 0.77 (0.42 to 1.41)) (table 5).
Tuberculin skin test reactions
Among 53 TB-exposed children with a TST assessed at 6 months, a total of 3 (5.7%) children (all with neonatal BCG) had a PPD reaction above 10 mm. Only seven TB-exposed children had a TST assessed at 12 months and no child had a PPD reaction above 15 mm (online supplementary table 4).
Among 1384 TB-unexposed children with assessed TST at 6 months, neonatal BCG did not affect PPD reactions; among the 335 children with TST assessed at 12 months, fewer children with neonatal BCG had large TSTs (online supplementary table 4).
Discussion
Main findings
Neonatal BCG was associated with lower mortality among both TB-exposed (aHR: 0.57 (95%CI 0.26 to 1.27)) and TB-unexposed children (HR: 0.57 (95% CI 0.47 to 0.69)), resulting in a combined HR of 0.54 (0.45 to 0.65), not adjusted as no factor changed the estimate by more than 5%. The results were robust to sensitivity analyses of longer follow-up, exclusion of children with no registered BCG vaccine, exclusion of children who were twins and exclusion of children potentially eligible for studies of preventive TB treatment. Children exposed to TB had higher mortality than TB-unexposed children if they had not received neonatal BCG.
Strengths and weaknesses
The study was conducted within the setup of BHP’s urban HDSS that since 1978 has followed the population in the study area with regular home visits to collect information on health status of children. Information on vaccination status and vital status is collected by experienced field assistants at home visits every third month, and hard endpoints like death are therefore unlikely to be misclassified. Only children with assessed vaccination status after 28 days of life were included in the analysis, and children only entered the analyses when the vaccination status was assessed at a home visit, thus avoiding differential misclassification of vaccination status and survival bias.
Self-selection to BCG vaccination could create healthy vaccinee bias, where early BCG is associated with lower mortality because the healthiest children receive BCG early, rather than early BCG causing healthy children. To remove potential confounding, we controlled for baseline characteristics that changed the estimate by more than 5% when included in the analyses one by one. Adjusting for available potential confounders affected the estimates for TB-exposed children, but did not alter the conclusions, neither did the sensitivity analyses conducted. Thus, self-selection for vaccination is unlikely to explain all of the effect. Since we find marked effects of neonatal BCG on all-cause mortality in both TB-exposed and TB-unexposed children, our results support that the effect of neonatal BCG is not merely due to protection against TB. However, there may be residual confounding not accounted for.
The registration of diagnosed TB cases from the study area allows for classifying children as TB-exposed. However, some TB cases will be undiagnosed, and some TB-exposed children may therefore have been misclassified as TB-unexposed. We expect any misclassification to be independent of timing of BCG vaccination. Unfortunately, we did not have HIV status for mothers or children, and we were therefore not able to assess whether HIV status influenced our results.
TB is difficult to diagnose, especially in children, and many TB cases are not diagnosed and treated.18 19 TST with PPD is commonly used to test for latent infection with Mycobacterium tuberculosis.20 A response to PPD can be due to either M. tuberculosis infection or BCG vaccination; however, BCG vaccination has been shown to result in lower PPD responses compared with latent TB infection.20 TST was only assessed for a subsample of our population, and we had scarce data in some groups. Our data did not allow for conclusions as to whether timing of BCG may have an impact on latent TB infection assessed by PPD reactions above 10 mm or 15 mm.
Comparison with other studies
The vaccine efficacy of BCG on preventing TB has been widely debated as different studies have yielded very different effects.21 However, a meta-analysis of BCG’s effect on TB found higher vaccine efficacy when BCG was given early in life.2 Our results support that BCG in early life has beneficial effects and furthermore suggest that timing of BCG is important. We did not study the vaccine efficacy on TB and the results are therefore not directly comparable, but our findings support that BCG should be administered early in life.
Increasing evidence supports that BCG aside from the specific effects also have NSEs.6 22 Most studies assessing the effect of BCG on all-cause mortality compared BCG-vaccinated children with unvaccinated children6 23 24 and randomised trials of BCG-Denmark have found beneficial effects in the neonatal period.8 It should be noted that two recent trials testing the effect of BCG-Russia in India found no effect;25 the different results may be related to different BCG strains.25 26 A previous study from the 1990s in Guinea-Bissau found that BCG was associated with stronger beneficial effects if provided in the first week of life.27 Our study supports that the timing of BCG is important, because children vaccinated later are deprived of beneficial effects early in life and that there are benefits beyond the initial early phase. Similar benefits have been observed for other live vaccines (oral polio vaccine28 and measles vaccine29).
In line with our study, data from the same setting between 1996 and 1998 indicate that TB exposure was associated with higher mortality in children aged 0-5 years.11 We also found that TB exposure was associated with higher mortality, but less so among children with neonatal BCG, due to no excess mortality among boys with neonatal BCG. It is generally accepted that TB-exposure can result in increased mortality,9 30 and it is recommended to provide preventive TB treatment for children younger than 5 years of age;31 however, a policy-practice gap remains, and the policy is rarely implemented.32 33 A recent modelling study estimated that more than 80 000 TB deaths could be averted globally in children younger than 5 years by altering coverage of household contact management from zero to full coverage.34 Our data suggest that part of this effect (in boys) may also be obtained by emphasising BCG at birth.
Interpretation and implications
Our conclusions were robust to sensitivity analyses and adjusting for available potential confounders. However, if BCG vaccination was delayed mainly for frail children, this could bias our results. To adjust for indicators of frailty, we conducted sensitivity analyses excluding twins, and stratifying by LBW status. Excluding twins or stratifying by LBW status did not alter the main conclusions. Assessing the effect of neonatal BCG by LBW limited the analysis to the 63% of the TB-exposed children and 65% of the TB-unexposed children with information on birth weight and should thus be interpreted with caution. As a whole, the sensitivity analyses did not suggest that frailty in children with no neonatal BCG explained our results.
Currently, timing of BCG is not captured as part of the WHO/UNICEF coverage estimates,5 and although BCG is planned to be given at birth in many countries, BCG is often delayed.4 5 Our results support that timing of BCG is important. WHO already recommends that BCG should be provided as soon as possible after birth,1 but we need more focus on barriers for neonatal BCG vaccination. Since policies are frequently implemented according to donor’s priorities, vaccine donors should be involved in creating incentives for neonatal BCG vaccination. Currently, vaccine donors evaluate performance of vaccine programmes by 12 months coverage estimates and vaccine wastage targets.35 Including neonatal BCG vaccination as a performance indicator in addition to 12 months coverage would provide countries with an incentive to strive for timely vaccination.
Conclusion
Neonatal BCG was associated with reduced mortality in TB-exposed and TB-unexposed children, supporting that timing of BCG is important for all-cause mortality. Neonatal BCG should be emphasised and barriers for neonatal BCG vaccination should be removed.
Supplementary Material
Acknowledgments
We wish to thank all children, mothers and patients with TB contributing with information to the present study. Furthermore, we would like to thank the dedicated staff working at BHP in Guinea-Bissau.
Footnotes
Twitter: @PerKallestrup
Contributors: SMT and AF conceived the idea for the study and planned the analyses. CSB, AR, PA and AF supervised the demographic surveillance data collection. AR and AF supervised and cleaned the PPD data. VFG, FR and CW supervised the data registration of patients with TB. SMT analysed the data and wrote the first manuscript draft with input from PK, PA and AF. All authors received and approved the final manuscript.
Funding: This work was supported by Augustinus Foundation. The Bandim Health Project received support from the Novo Nordisk Foundation, DANIDA; EU (ICA 4-CT-2002–10053), the Danish National Research Foundation via Research Centre for Vitamins and Vaccines (DNRF108) and Karen Elise Jensen Foundation.
Disclaimer: The sponsors had no role in designing the study, the data collection, data analysis, data interpretation or writing the paper.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request. Data are available on a collaborative basis; please see http://www.bandim.org for further information.
References
- 1. World Health Organisation BCG vaccines: who position paper – February 2018. Wkly Epidemiol Rec 2018;93:73–96. [PubMed] [Google Scholar]
- 2. Mangtani P, Abubakar I, Ariti C, et al. Protection by BCG vaccine against tuberculosis: a systematic review of randomized controlled trials. Clin Infect Dis 2014;58:470–80. 10.1093/cid/cit790 [DOI] [PubMed] [Google Scholar]
- 3. VanderEnde K, Gacic-Dobo M, Diallo MS, et al. Global Routine Vaccination Coverage - 2017. MMWR Morb Mortal Wkly Rep 2018;67:1261–4. 10.15585/mmwr.mm6745a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clark A, Sanderson C. Timing of children's vaccinations in 45 low-income and middle-income countries: an analysis of survey data. Lancet 2009;373:1543–9. 10.1016/S0140-6736(09)60317-2 [DOI] [PubMed] [Google Scholar]
- 5. Thysen SM, Fisker AB. Indepth Working group on vaccines and child survival. selecting the right indicators to ensure optimised implementation of BCG vaccination policy. Vaccine 2018;36:3406–7. [DOI] [PubMed] [Google Scholar]
- 6. Higgins JPT, Soares-Weiser K, López-López JA, et al. Association of BCG, DTP, and measles containing vaccines with childhood mortality: systematic review. BMJ 2016;355:i5170 10.1136/bmj.i5170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Uthayakumar D, Paris S, Chapat L, et al. Non-Specific effects of vaccines illustrated through the BCG example: from observations to demonstrations. Front Immunol 2018;9:2869 10.3389/fimmu.2018.02869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Biering-Sørensen S, Aaby P, Lund N, et al. Early BCG-Denmark and Neonatal Mortality Among Infants Weighing <2500 g: A Randomized Controlled Trial. Clin Infect Dis 2017;65:1183–90. 10.1093/cid/cix525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fox GJ, Barry SE, Britton WJ, et al. Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur Respir J 2013;41:140–56. 10.1183/09031936.00070812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lemvik G, Rudolf F, Vieira F, et al. Decline in overall, smear-negative and HIV-positive TB incidence while smear-positive incidence stays stable in Guinea-Bissau 2004-2011. Trop Med Int Health 2014;19:1367–76. 10.1111/tmi.12378 [DOI] [PubMed] [Google Scholar]
- 11. Gomes VF, Andersen A, Wejse C, et al. Impact of tuberculosis exposure at home on mortality in children under 5 years of age in Guinea-Bissau. Thorax 2011;66:163–7. 10.1136/thx.2010.141309 [DOI] [PubMed] [Google Scholar]
- 12. Gomes VF, Andersen A, Lemvik G, et al. Impact of isoniazid preventive therapy on mortality among children less than 5 years old following exposure to tuberculosis at home in Guinea-Bissau: a prospective cohort study. BMJ Open 2013;3. doi: 10.1136/bmjopen-2012-001545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lemvik G. Active TB among adults and latent TB among children in Guinea-Bissau - risk factors and adherence to preventive therapy. Aarhus University, 2013. [Google Scholar]
- 14. Roth AE, Benn CS, Ravn H, et al. Effect of revaccination with BCG in early childhood on mortality: randomised trial in Guinea-Bissau. BMJ 2010;340:c671 10.1136/bmj.c671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bouros D, Zeros G, Panaretos C, et al. Palpation vs Pen method for the measurement of skin tuberculin reaction (Mantoux test). Chest 1991;99:416–9. 10.1378/chest.99.2.416 [DOI] [PubMed] [Google Scholar]
- 16. Menzies D. What does tuberculin reactivity after Bacille Calmette-Guérin vaccination tell us? Clin Infect Dis 2000;31:S71–4. 10.1086/314075 [DOI] [PubMed] [Google Scholar]
- 17. Wang L, Turner MO, Elwood RK, et al. A meta-analysis of the effect of Bacille Calmette Guérin vaccination on tuberculin skin test measurements. Thorax 2002;57:804–9. 10.1136/thorax.57.9.804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organisation Global Tubeculosis report 2018. Licence: CC BY-NC-SA 3.0 IGO, 2018. [Google Scholar]
- 19. Jenkins HE. Global burden of childhood tuberculosis. Pneumonia 2016;8. doi: 10.1186/s41479-016-0018-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Enarson DA. Use of the tuberculin skin test in children. Paediatr Respir Rev 2004;5:S135–7. 10.1016/S1526-0542(04)90025-5 [DOI] [PubMed] [Google Scholar]
- 21. Abubakar I, Pimpin L, Ariti C, et al. Systematic review and meta-analysis of the current evidence on the duration of protection by Bacillus Calmette-Guérin vaccination against tuberculosis. Health Technol Assess 2013;17:1–372. 10.3310/hta17370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Arts RJW, Moorlag SJCFM, Novakovic B, et al. Bcg vaccination protects against experimental viral infection in humans through the induction of cytokines associated with trained immunity. Cell Host Microbe 2018;23:89–100. 10.1016/j.chom.2017.12.010 [DOI] [PubMed] [Google Scholar]
- 23. Kristensen I, Aaby P, Jensen H. Routine vaccinations and child survival: follow up study in Guinea-Bissau, West Africa. BMJ 2000;321:1435–8. 10.1136/bmj.321.7274.1435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aaby P, Jensen H, Gomes J, et al. The introduction of diphtheria-tetanus-pertussis vaccine and child mortality in rural Guinea-Bissau: an observational study. Int J Epidemiol 2004;33:374–80. 10.1093/ije/dyh005 [DOI] [PubMed] [Google Scholar]
- 25. Jayaraman K, Adhisivam B, Nallasivan S, et al. Two randomized trials of the effect of BCG-Russia alone or with oral polio vaccine on neonatal mortality in infants weighing. Pediatr Infect Dis J 2018. [DOI] [PubMed] [Google Scholar]
- 26. Curtis N. Bcg vaccination and all-cause neonatal mortality. Pediatr Infect Dis J 2019;38:195–7. 10.1097/INF.0000000000002230 [DOI] [PubMed] [Google Scholar]
- 27. Roth A, Jensen H, Garly M-L, et al. Low birth weight infants and Calmette-Guérin Bacillus vaccination at birth: community study from Guinea-Bissau. Pediatr Infect Dis J 2004;23:544–50. 10.1097/01.inf.0000129693.81082.a0 [DOI] [PubMed] [Google Scholar]
- 28. Lund N, Andersen A, Hansen ASK, et al. The effect of oral polio vaccine at birth on infant mortality: a randomized trial. Clin Infect Dis 2015;61:1504–11. 10.1093/cid/civ617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aaby P, Martins CL, Garly M-L, et al. Non-Specific effects of standard measles vaccine at 4.5 and 9 months of age on childhood mortality: randomised controlled trial. BMJ 2010;341:c6495 10.1136/bmj.c6495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Marais BJ. Preventing tuberculosis in household contacts crucial to protect children and contain epidemic spread. Lancet Glob Health 2018;6:e1260–1. 10.1016/S2214-109X(18)30449-2 [DOI] [PubMed] [Google Scholar]
- 31. World Health Organization Latent TB infection: updated and consolidated guidelines for programmatic management, 2018. Available: http://apps.who.int/iris/bitstream/handle/10665/260233/9789241550239-eng.pdf;jsessionid=822A28C5C42D1A1A1262F556FC0CEC7C?sequence=1 [PubMed]
- 32. Hill PC, Rutherford ME, Audas R, et al. Closing the policy-practice gap in the management of child contacts of tuberculosis cases in developing countries. PLoS Med 2011;8:e1001105 10.1371/journal.pmed.1001105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gomes VF, Wejse C, Oliveira I, et al. Adherence to isoniazid preventive therapy in children exposed to tuberculosis: a prospective study from Guinea-Bissau. Int J Tuberc Lung Dis 2011;15:1637–43. 10.5588/ijtld.10.0558 [DOI] [PubMed] [Google Scholar]
- 34. Dodd PJ, Yuen CM, Becerra MC, et al. Potential effect of household contact management on childhood tuberculosis: a mathematical modelling study. Lancet Glob Health 2018;6:e1329–38. 10.1016/S2214-109X(18)30401-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. GAVI Gavi 2016-2020 strategy indicators, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-035595supp001.pdf (53.7KB, pdf)