Abstract
Background
Pregnancy is presumed to be a major contributory factor in the increased incidence of varicose veins in women, which can in turn lead to venous insufficiency and leg oedema. The most common symptom of varicose veins and oedema is the substantial pain experienced, as well as night cramps, numbness, tingling, the legs may feel heavy, achy, and possibly be unsightly. Treatments for varicose veins are usually divided into three main groups: surgery, pharmacological and non‐pharmacological treatments. Treatments of leg oedema comprise mostly symptom reduction rather than cure and use of pharmacological and non‐pharmacological approaches.
Objectives
To assess any form of intervention used to relieve the symptoms associated with varicose veins and leg oedema in pregnancy.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (31 May 2015) and reference lists of retrieved studies.
Selection criteria
Randomised trials of treatments for varicose veins or leg oedema, or both, in pregnancy.
Data collection and analysis
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy.
Main results
We included seven trials (involving 326 women). The trials were largely unclear for selection bias and high risk for performance and detection bias.
Two studies were placebo‐controlled trials. The first one compared a phlebotonic (rutoside) with placebo for the reduction in symptoms of varicose veins; the second study evaluated the efficacy of troxerutin in comparison to placebo among 30 pregnant women in their second trimester with symptomatic vulvar varicosities and venous insufficiency in their lower extremities. Data from this study were not in useable format, so were not included in the analysis. Two trials compared either compression stockings with resting in left lateral position or reflexology with rest for 15 minutes for the reduction of leg oedema. One trial compared standing water immersion for 20 minutes with sitting upright in a chair with legs elevated for 20 minutes. Women standing in water were allowed to stand or walk in place. One trial compared 20 minutes of daily foot massage for five consecutive days and usual prenatal care versus usual prenatal care. The final trial compared three treatment groups for treating leg oedema in pregnancy. The first group was assigned to lateral supine bed rest at room temperature, women in the second group were asked to sit in a bathtub of waist‐deep water at 32 ± 0.5 C with their legs horizontal and the third group included the women who were randomised to sitting immersed in shoulder‐deep water at 32 ± 0.5 C with legs extended downward. We did not include this study in the analysis as outcomes reported in the paper were not pre‐specified outcomes of this review.
We planned to use GRADE methods to assess outcomes for two different comparisons and assign a quality rating. However, only two out of three outcomes for one comparison were reported and could be assessed. Evidence from one trial (rutoside versus placebo) for the outcomes of reduction in symptoms and incidence of complications associated with varicose veins and oedema was assessed as of moderate quality.
Rutoside versus placebo
One trial involving 69 women, reported that rutoside significantly reduced the symptoms associated with varicose veins (risk ratio (RR) 1.89, 95% confidence interval (CI) 1.11 to 3.22; moderate quality evidence). The incidence of complications (deep vein thrombosis) did not differ significantly between the two groups (risk ratio (RR) 0.17, 95% CI 0.01 to 3.49; moderate quality evidence). There were no significant differences in side‐effects (RR 1.30, 95% CI 0.23 to 7.28). Women's perception of pain was not reported in this trial.
External pneumatic intermittent compression versus rest
One trial, involving 35 women, reported no significant difference in lower leg volume when compression stockings were compared against rest (mean difference (MD) ‐258.80, 95% CI ‐566.91 to 49.31).
Reflexology versus resting
Another trial, involving 55 women, compared reflexology with rest. Reflexology significantly reduced the symptoms associated with oedema (reduction in symptoms: RR 9.09, 95% CI 1.41 to 58.54). The same study showed a trend towards satisfaction and acceptability with the intervention (RR 6.00, 95% CI 0.92 to 39.11).
Water immersion versus leg elevation
There was evidence from one trial, involving 32 women, to suggest that water immersion for 20 minutes in a swimming pool reduces leg volume (RR 0.43, 95% CI 0.22 to 0.83).
Foot massage versus routine care
One trial, involving 80 women reported no significant difference in lower leg circumference when foot massage was compared against routine care (MD ‐0.11, 95% CI ‐1.02 to 0.80).
No other primary or secondary outcomes were reported in the trials.
Authors' conclusions
There is moderate quality evidence to suggest that rutosides appear to help relieve the symptoms of varicose veins in late pregnancy. However, this finding is based on one study (69 women) and there are not enough data presented in the study to assess its safety in pregnancy. Reflexology or water immersion appears to help improve symptoms for women with leg oedema, but again this is based on two small studies (43 and 32 women, respectively).
Plain language summary
Interventions for varicose veins and leg oedema in pregnancy
There is not enough evidence on treatments for varicose veins and leg oedema in pregnancy.
Varicose veins, sometimes called varicosity, occur when a valve in the blood vessel walls weakens and the blood stagnates. This in turn leads to problems with the circulation in the veins and to oedema or swelling. The vein then becomes distended, its walls stretch and sag, allowing the vein to swell into a tiny balloon near the surface of the skin. The veins in the legs are most commonly affected as they are working against gravity, but the vulva (vaginal opening) or rectum, resulting in haemorrhoids (piles), can be affected too. Pregnancy seems to increase the risk of varicose veins and they cause considerable pain, night cramps, numbness, tingling, the legs may feel heavy, achy, and they are rather ugly. Treatments for varicose veins are usually divided into three main groups: pharmacological treatments, non‐pharmacological and surgery. The review identified seven trials involving 326 women. Although there was a moderate quality evidence to suggest that the drug rutoside seemed to be effective in reducing symptoms, the study was too small to be able to say this with real confidence. Similarly, with reflexology and water immersion, there were insufficient data to be able to assess benefits and harms, but they looked promising. Compression stockings do not appear to have any advantages. More research is needed.
Summary of findings
Background
Description of the condition
The body's veins are responsible for ensuring blood flows back to the heart. To assist this process veins are designed with a series of valves, which close between heartbeats to prevent the blood flowing backwards. A varicose vein, sometimes called varicosity, occurs when a valve weakens, putting more pressure on other valves and causing blood to stagnate. The vein then becomes distended, its walls stretch and, like tired elastic, sag, allowing the vein to swell in that region into a miniature balloon near the surface of the skin. The veins in the legs are most commonly affected as they are working against gravity, but the vulva (vaginal opening) or rectum, resulting in haemorrhoids (piles), can be affected.
Varicose veins are most commonly seen in North America and Western Europe. Vein problems are less common in the Mediterranean Basin, South America, and India and even more uncommon in the Far East and Africa (Carr 2006). They are more common in women compared with men (Criquiui 2003). Pregnancy is presumed to be a major contributory factor in the increased incidence of varicose veins in women (Stansby 2000); varicose veins affecting about 40% of pregnant women (Rabhi 2000). Evidence suggests that parous women (having had a previous pregnancy) have a higher incidence of varicose veins compared with nulliparous women (no previous pregnancy), and that multiparous women (more than one previous pregnancy) have the highest risk (Beebe‐Dimmer 2005). In 70% to 80% of women who develop problems with varicose veins during pregnancy, the symptoms appear during the first trimester (first three months of pregnancy), often within two to three weeks of a woman becoming pregnant (Carr 2006).
During pregnancy increased blood volume puts veins under increased pressure. In addition, an increase in the hormone progesterone relaxes the muscular walls of the blood vessels. This makes it even more difficult for veins to move blood from the lower body back to the heart. The increasing weight of the growing uterus (womb) puts pressure on the pelvic veins and on the inferior vena cava (a large vein on the right side of the body that receives blood from the lower limbs and the greater part of the pelvic and abdominal organs and carries it back to the heart). This increases blood pressure in the leg veins, and thus influences the development of varicose veins. As the baby grows and the uterus enlarges, the veins become even more prominent. Moreover, there are oestrogen and progesterone receptors in saphenous veins (veins in the leg) and, although their function is not known, it has been claimed that they may provoke venous dilation and valve failure in pregnancy (Mashiah 1999).
This same process can in turn lead to venous insufficiency and leg oedema (excess fluid collecting in tissues causing swelling). The slowing down of the circulation causes blood to pool in the legs, forcing fluid from the veins into the tissues of the feet and ankles. Leg oedema can affect up to 80% of pregnant women, and should not be considered to be a sign of pregnancy‐induced hypertension or pre‐eclampsia (Enkin 2000).
The most common symptom of varicose veins and oedema is the substantial pain experienced, as well as night cramps, numbness, tingling, the legs may feel heavy, achy, and possibly be unsightly. The skin around the varicose vein may also itch, throb, or feel like it is burning. Symptoms tend to worsen after long periods of standing and with each successive pregnancy. For some women, however, varicose veins or oedema can cause little or no discomfort.
Although unlikely, there are potential complications associated with varicose veins and the resulting oedema. Possibilities include venous thrombus (small blood clot in vein), thrombophlebitis (inflammation of the vein), bleeding of the varicose vein, deep vein thrombosis (blood clots in the deep veins, usually legs), and pulmonary embolism (blocking of a blood vessel by a blood clot that has travelled to the lungs by the blood stream) (Rabhi 2000). Varicose veins often improve three or four months after giving birth, and the oedema tend to diminish soon after the birth. With chronic venous insufficiency, problems including varicose eczema (brown or purple discolouration of the skin) and venous ulcers (a minor wound that fails to heal, causing an ulcer) can occur (Feied 2004).
Description of the intervention
Treatments for varicose veins are usually divided into three main groups: surgery, pharmacological and non‐pharmacological treatments. Treatments for leg oedema comprise mostly of symptom reduction rather than cure and use pharmacological and non‐pharmacological approaches.
Pharmacological treatments
Sclerotherapy is a procedure used to treat the affected veins. The veins are injected with liquid sclerosing drugs (detergent type with tensio‐active properties), which make them shrink immediately and then dissolve over a period of weeks as the body naturally absorbs the treated vein. Because the solution is injected directly into the vein, there is thought to be little or no damage to the surrounding skin. A compression bandage has to be worn for between three and six weeks after treatment. Often several injections are needed.
Phlebotonics are a class of medications used to treat venous insufficiency, known as venoactive drugs. Their action is not well established; however, they are associated with increasing venous tone and preventing oedema. They include rutosides, hidrosmine, diosmine, calcium dobesilate, chromocarbe, centella asiatica, disodium flavodate, french maritime pine bark extract, grape seed extract and aminaftone.
O‐Beta‐hydroxyethyl rutoside is a semi‐synthetic compound; the mode of action is probably based on a direct effect on the capillary wall as well as capillary functions (Lund 1970; Tschopp 1970). Though rutosides may help women with varicose veins with symptoms (nocturnal cramps, feelings of tiredness, paraesthesia), it is not yet clear that the drug is safe enough to use in pregnancy.
Non‐pharmacological treatments
Compression stockings
These may relieve the swelling and aching of the legs and may prevent more varicose veins from developing. They are worn during the day and taken off at night. Graduated compression stockings are tightest at the ankle and gradually get looser further up the leg, as this helps to encourage the blood flow back to the heart.
Rest
Women are advised not to stand for long periods of time and take short breaks from standing either with exercise or elevating their feet and legs. When resting for longer periods, women are advised to rest on their left side (as the inferior vena cava is on the right, left‐sided rest relieves it of the weight of the uterus, thus decreasing pressure on the veins in the legs and feet). Gentle flexion of the foot to stretch the calf muscles is also advised.
Reflexology
This is a concept that all body organs and glands have corresponding reflex points in the feet, hands and ears. It has the potential to provide pain relief and symptom relief and induce relaxation without harmful side‐effects. Reflexology may be used for specific conditions in the lower limbs and generalised oedema as it moves fluids from extravascular compartments without affecting intravascular fluids (Mollart 2003).
Water immersion
Historically, water has always been believed to promote healing and has therefore been widely used in the management of medical disorders. In terms of reducing leg oedema, water immersion can help the blood of an individual immersed in water to be displaced upward through the venous and lymphatic systems, firstly into the thighs, then into the abdominal cavity vessels, and finally into the great vessels of the chest cavity and into the heart. This is because that the individual is subjected to external water pressure in a gradient, which within a relatively small depth exceeds venous pressure (Risch 1978).
Foot massage
Foot massage is another example of a non‐pharmacological intervention that is proving popular among healthcare providers. The technique in leg and foot oedema works by moving extravascular fluid without disturbing intravascular fluid (Hayes 1999), and thus reducing the oedema.
Surgery
This involves removing the affected vein(s). There are many variations of the operation, depending on which veins need treatment. The most common method is called ligation and stripping. Under a general or regional anaesthetic, the vein to be treated is ligated (tied off) at the top of the leg. A flexible wire is passed through the affected vein and attached to one end. By pulling the wire back, the vein is 'stripped' out. Although removed veins cannot reoccur, other leg veins can become varicosed. Vein stripping is often delayed until after the pregnancy (Pernoll 1991).
Treatment during pregnancy, however, mainly concentrates on the reprieve of symptoms. For the majority of women, varicose veins subside on their own within three or four months of the baby's birth. Any corrective treatment is often deferred to after this period.
How the intervention might work
Treatments for varicose veins are usually divided into three main groups: surgery, pharmacological and non‐pharmacological treatments. Treatments of leg oedema comprise mostly of symptom reduction rather than cure and use pharmacological and non‐pharmacological approaches. Historically, surgery, for treatment of varicose veins, has been the most widely recommended treatment option. Surgery may reduce the risk of complications of varicose veins (Campbell 2006). Some pharmacological treatments work through increasing venous tone and preventing oedema (phlebotonics). Non‐pharmacological interventions including include avoidance of prolonged standing and straining, external compression devices (e.g. bandages, support stockings, intermittent pneumatic compression devices) and leg elevation can provide relief from discomfort and may improve symptoms in some women. However, evidence to support these therapies is lacking (Bartholomew 2005).
Why it is important to do this review
To date, there is no clear recommendations on the best management approach for patients with varicose veins and leg oedema during pregnancy. There is little evidence to preferentially support any single treatment modality. Choice of therapy is affected by many factors, such as symptoms, preference, cost, potential for iatrogenic complications, available medical resources. A formal evaluation of published studies is therefore very important to guide national and international recommendations for appropriate low‐cost, safe and effective methods of intervention.
Objectives
To assess the effect of any form of intervention for the treatment of varicose veins and leg oedema in pregnancy.
Methods
Criteria for considering studies for this review
Types of studies
Randomised trials examining the effects of treatments for varicose veins or leg oedema, or both. Quasi‐randomised trials and cross‐over trials were excluded.
Types of participants
Pregnant women with varicose veins or leg oedema, or both, at any gestation period.
Types of interventions
Any described method used to treat varicose veins or leg oedema compared with placebo or no treatment, or any other method. These may include:
pharmacological interventions (sclerotherapy or phlebotonics);
non‐pharmacological interventions (compression stockings, leg elevation, any form of rest, any form of exercise, immersion in water, reflexology, physiotherapy, massage);
surgical interventions.
Types of outcome measures
Primary outcomes
Maternal
Woman's perception of pain (as defined by trialists)
Complications associated with varicose veins and leg oedema (venous leg ulcer, venous thrombus, thrombophlebitis, bleeding of the varicose vein, deep vein thrombosis, pulmonary embolism, varicose eczema, or venous leg ulcers)
Secondary outcomes
Maternal
Women's satisfaction and acceptability with intervention
Symptoms associated with varicose veins and oedema (burning, discomfort, aching, itching, limb heaviness, oedema, nocturnal cramps, etc)
Need for pain relief
Side‐effects, or adverse events of intervention
Preterm birth (as defined by authors) (not prespecified)
Economic
Duration of hospital stay (during pregnancy or postnatally)
Cost of hospital stay
Cost associated with intervention
Neonatal
Death (perinatal/neonatal death) (not prespecified)
Congenital malformations (not prespecified)
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (31 May 2015).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE, Embase and CINAHL, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
We searched the reference lists of retrieved studies.
We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, seeBamigboye 2007.
For this update, the following methods were used for assessing the four reports that were identified as a result of the updated search.
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we planned to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding was unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Assessment of the quality of the evidence using GRADE
For this update we assessed the quality of the evidence using the GRADE approach as outlined in the GRADE handbook. We assessed the quality of the body of evidence relating to the following outcomes for the comparisons of 1. Rutoside versus placebo and 2. External pneumatic intermittent compression versus rest.
Woman's perception of pain (as defined by trialists)
Complications associated with varicose veins and leg oedema (venous leg ulcer)
Reduction in symptoms associated with varicose veins
We used GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create 'Summary of findings' tables. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
We used the mean difference if outcomes were measured in the same way between trials. In future updates, if appropriate, we will use the standardised mean difference to combine trials that measured the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
We have not included cluster‐randomised trials in this review.
If in future updates we identify eligible cluster‐randomised trials, we will include these in the analyses along with individually‐randomised trials. We will adjust their sample sizes using the methods described in the Handbook [Section 16.3.4 or 16.3.6] using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity or subgroup analysis to investigate the effects of the randomisation unit.
Cross‐over trials
Cross‐over trials are not eligible for inclusion in this review.
Other unit of analysis issues
Multiple pregnancies
None of the included studies reported the inclusion of women with multiple pregnancies. If such data are included in future updates of this review, we will consider for each outcome whether the appropriate denominator is the number of babies or the number of women. For all infant outcomes, the number of babies will be the appropriate denominator, and for maternal outcomes, the number of women will be used.
Multiple groups from one study
In studies that included more than two interevention groups, we combined groups to create a single pair‐wise comparison e.g. In Mollart 2003 women were randomly allocated to one of three groups: (i) relaxing foot reflexology, (ii) lymphatic foot reflexology and (iii) a control group resting on a couch. In this trial Mollart 2003 we combined the reflexology groups to create a single pair‐wise comparison of reflexology versus resting.
Dealing with missing data
For included studies, we noted levels of attrition. In future updates, if more eligible studies are included, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either a Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. If we identified substantial heterogeneity (above 30%), we planned to explore it by pre‐specified subgroup analysis.
Assessment of reporting biases
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we planned to use random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary would have been treated as the average range of possible treatment effects and we planned to discuss the clinical implications of treatment effects differing between trials. If the average treatment effect had not been clinically meaningful, we would not have combined trials. Had we used random‐effects analyses, we would have presented the results as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
Due to the limited number of trials included in this review, we did not conduct subgroup analysis to explore heterogeneity. If in future updates we identify substantial heterogeneity, we will investigate it using subgroup analyses and sensitivity analyses. We will consider whether an overall summary is meaningful, and if it so, we will use random‐effects analysis to produce it.
We will carry out the following subgroup analyses for the primary outcomes.
1. Parity (primigravid women compared with parous women).
The following outcomes will be used in subgroup analyses.
Woman's perception of pain (as defined by trialists).
Complications associated with varicose veins and leg oedema (venous leg ulcer, venous thrombus, thrombophlebitis, bleeding of the varicose vein, deep vein thrombosis, pulmonary embolism, varicose eczema, or venous leg ulcers).
We will assess subgroup differences by interaction tests available within RevMan (RevMan 2014). We will report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
We did not conduct sensitivity analysis in this review due to lack of data. If in future updates we have sufficient numbers of trials, we plan to carry out sensitivity analyses to explore the effect of trial quality assessed by concealment of allocation, high attrition rates, or both, with poor quality studies being excluded from the analyses in order to assess whether this makes any difference to the overall result.
Results
Description of studies
See table of Characteristics of included studies.
Results of the search
Five new reports (relating to four studies) were identified in the search for the update of this review (31 May 2015). Two studies were included (Coban 2010; Irion 2011), one was excluded (Adamczyk 2013), and one is ongoing (Heller 2013). Two trials (Katz 1990; Marhic 1991) previously excluded are now included in the update.
Included studies
Seven trials, involving 326 women from six studies (in Katz 1990 the total number of recruited participants was not mentioned in the paper), were included in the review. Data were available for only some of the prespecified outcomes. Two trials compared either compression stockings (Jacobs 1986) with resting in left lateral position or reflexology (Mollart 2003) with rest for 15 minutes for the reduction of leg oedema. Two studies were placebo‐controlled trials. The first one (Bergstein 1975), compared a phlebotonic (rutoside) with placebo for the reduction in symptoms of varicose veins. Marhic 1991 evaluated the efficacy of troxerutin in comparison to placebo among 30 pregnant women in their second trimester with symptomatic vulvar varicosities and venous insufficiency in their lower extremities. Data from this study were not in useable format, so could not be included in the analysis.The trial by Coban 2010 included 80 healthy pregnant women, > 30 weeks' gestation with visible oedema in the ankles and feet, the randomised participants received either 20 minutes of daily foot massage for five consecutive days and usual prenatal care or usual prenatal care. Irion 2011 compared standing water immersion for 20 minutes with sitting upright in a chair with legs elevated for 20 minutes. Women standing in water were allowed to stand or walk in place. The study randomised 32 women, and data for all women were reported. Katz 1990 compared three treatment groups for treating leg oedema in pregnancy. The first group was assigned to lateral supine bed rest at room temperature; women in the second group were asked to sit in a bathtub of waist‐deep water at 32 ± 0.5 C with legs horizontal; the third group included women who were randomised to sitting immersed in shoulder‐deep water at 32 ± 0.5 C with legs extended downward. We did not include this study in the analysis as outcomes reported in paper were not of interest for this review.
Excluded studies
We excluded nine studies.The study by Coughlin 2001 was excluded as it included pregnant women with superficial venous reflux and normal deep veins diagnosed by duplex scan. We excluded Adamczyk 2013 and Thaler 2001 as both studies aimed to determine whether prophylactic use of compression stockings would prevent varicose veins. The studies by Steiner 1990 and Steiner 1991 were placebo‐controlled randomised double‐blind cross‐over trials and therefore were excluded. Three studies were excluded as they were not randomised (Heynen 1972; Mauss 1969; Sohn 1995). We excluded Tsouderos 1989 as it evaluated a single administration of Daflon 500 mg on venous haemodynamics in a clinical pharmacological trial. Details of the number of participants are unknown, the result showed a decrease in mean venous capacitance in the pregnancy group.
Risk of bias in included studies
See Figure 1 and Figure 2 for a summary of ’Risk of bias’ assessments.
1.
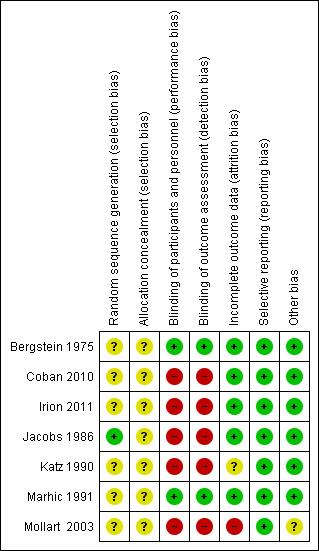
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
2.
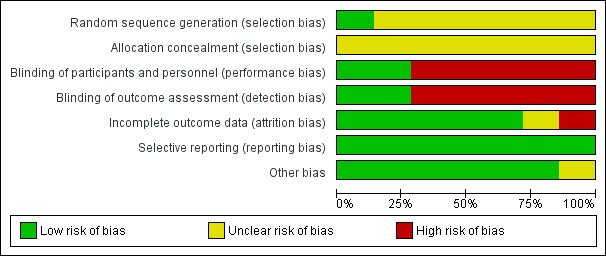
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
All included trials stated the women were randomly allocated to the intervention or control group. Information regarding generation of the randomisation sequence was described as using a schedule generated from a table of random numbers in one study (Jacobs 1986); no information was given for the other trials (Bergstein 1975; Coban 2010; Irion 2011; Katz 1990; Marhic 1991; Mollart 2003). Allocation concealment was classified as unclear for all included trials.
Blinding
Blinding of the participants and clinicians was not possible for the non‐pharmacological trials (Coban 2010; Irion 2011; Jacobs 1986; Katz 1990; Mollart 2003). The two included placebo‐controlled trials (Bergstein 1975; Marhic 1991), were described as 'double‐blind' and therefore assessed as being low risk of bias. As blinding of outcome assessment was not reported in any of the other studies, it is unlikely to have been done.
Incomplete outcome data
Three women in Bergstein 1975 were lost to follow‐up. In the reflexology study (Mollart 2003), three women withdrew from the study in the rest group, six had incomplete data and one delivered prematurely. Hence 10 women were analysed for the rest group versus 33 in the intervention group. Total number of recruited participants in Katz 1990 trial was not mentioned in the paper. The authors stated that 11 women completed the study. All participants entered in the other studies were accounted for in the prespecified outcome measures.
Selective reporting
There are no obvious sources of selective reporting.
Other potential sources of bias
In one trial (Mollart 2003), up to four reflexology sessions were planned, but by the third session only 20/69 women remained. Analysis was performed on the results of the first session only.
Effects of interventions
Summary of findings for the main comparison. Rutoside compared with placebo for varicose veins and leg oedema in pregnancy.
| Rutoside compared with placebo for varicose veins and leg oedema in pregnancy | ||||||
| Patient or population: Pregnant women with varicose veins and leg oedema in pregnancy Settings: Netherlands Intervention: Rutoside Comparison: Placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo | Rutoside | |||||
| Woman's perception of pain (as defined by trialists) | This outcome was not reported by this included study. | |||||
| Complications associated with varicose veins and leg oedema (deep vein thrombosis) | Study population | RR 0.17 (0.01 to 3.49) |
69 (1 RCT) |
⊕⊕⊕⊝ MODERATE 1 | ||
| 63 per 1000 | 11 per 1000 (1 to 218) |
|||||
| Symptoms associated with varicose veins and oedema (improvement in symptoms) | Study population | RR 1.89 (1.11 to 3.22) | 69 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 344 per 1000 | 650 per 1000 (382 to 1000) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1One study of small sample size
Summary of findings 2. External pneumatic intermittent compression compared with rest for varicose veins and leg oedema in pregnancy.
| External pneumatic intermittent compression compared with rest for varicose veins and leg oedema in pregnancy | ||||
| Patient or population: Pregnant women with varicose veins and leg oedema in pregnancy Settings: USA Intervention: External pneumatic intermittent compression Comparison: Rest | ||||
| Outcomes | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments |
| Woman's perception of pain (as defined by trialists) | None of these outcomes were reported. | |||
| Complications associated with varicose veins and leg oedema (venous leg ulcer) | ||||
| Symptoms associated with varicose veins and oedema | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1: Rutoside versus placebo
There was just one study (Bergstein 1975), involving 69 women that compared a phlebotonic agent (rutoside) with placebo for the reduction in symptoms of varicose veins. Outcomes reported by the rutoside study were concerned with the women's subjective responses to the intervention, which included improvements in nocturnal cramps, feelings of tiredness and reduction in paraesthesia. Data were also presented on side‐effects and the incidence of deep vein thrombosis.
Primary outcomes
The incidence of deep vein thrombosis did not differ significantly between the two groups (risk ratio (RR) 0.17, 95% confidence interval (CI) 0.01 to 3.49; participants = 69; studies = one), (Analysis 1.1).
1.1. Analysis.
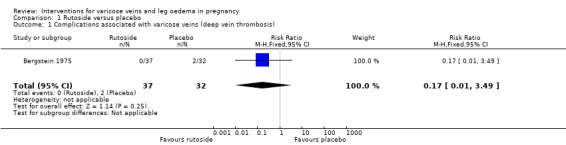
Comparison 1 Rutoside versus placebo, Outcome 1 Complications associated with varicose veins (deep vein thrombosis).
Secondary outcomes
Rutoside significantly reduced the symptoms associated with varicose veins (nocturnal cramps, feelings of tiredness, paraesthesia) (RR 1.89, 95% CI 1.11 to 3.22; participants = 69; studies = one), Analysis 1.2. There was no statistical difference in the side‐effect rate between the treatment groups (RR 1.30, 95% CI 0.23 to 7.28; participants = 69; studies = one), (Analysis 1.3). There were no cases of neonatal mortality or congenital malformation reported (Analysis 1.4; Analysis 1.5).
1.2. Analysis.
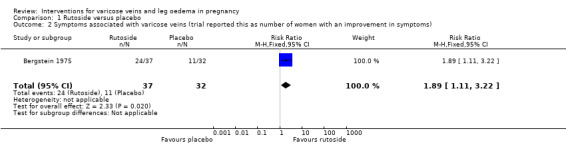
Comparison 1 Rutoside versus placebo, Outcome 2 Symptoms associated with varicose veins (trial reported this as number of women with an improvement in symptoms).
1.3. Analysis.
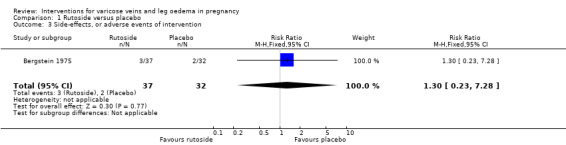
Comparison 1 Rutoside versus placebo, Outcome 3 Side‐effects, or adverse events of intervention.
1.4. Analysis.
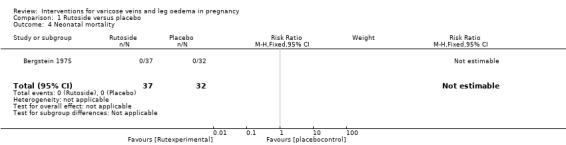
Comparison 1 Rutoside versus placebo, Outcome 4 Neonatal mortality.
1.5. Analysis.
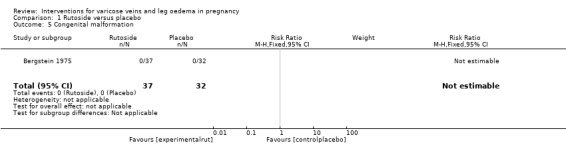
Comparison 1 Rutoside versus placebo, Outcome 5 Congenital malformation.
No other primary or secondary outcomes were reported in the study.
2: External pneumatic intermittent compression versus rest
This comparison included one trial (Jacobs 1986) involving 35 women. In this study, leg volume was calculated from a formula using four circumference measurements prior to treatment (time 1). Measurements were then taken again immediately after 30 minutes of treatment (time 2) and again after 10 minutes of walking (time 3). Data from time 3 measurements, that is, after walking, are provided in this review. The study does not concern itself with what women felt about the treatment or whether they felt any benefit from the reduction in leg volume.
Primary outcomes
The trial reported none of the review's primary outcomes.
The trial reported no significant difference in lower leg volume (oedema) when the use of compression stockings was compared against rest (mean difference (MD) ‐258.80, 95% CI ‐566.91 to 49.31; participants = 35; studies = one), (Analysis 2.1). No other secondary outcomes were reported.
2.1. Analysis.
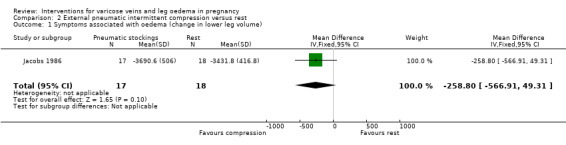
Comparison 2 External pneumatic intermittent compression versus rest, Outcome 1 Symptoms associated with oedema (change in lower leg volume).
3: Reflexology versus resting
This comparison included one trial (Mollart 2003), involving 55 women, which compared two different reflexology techniques (relaxing and lymphatic) with a period of rest for symptoms of oedema. We report the results for the reflexology groups combined to create a single pair‐wise comparison of reflexology versus resting. Additional analyses are presented below comparing the two different types of reflexology (Analysis 4.1; Analysis 4.2). The study did not report either of the primary outcomes for this review. Questionnaire responses to women's satisfaction and acceptability of intervention and reduction in symptoms associated with oedema between lymphatic and relaxing reflexologies were analysed.
4.1. Analysis.
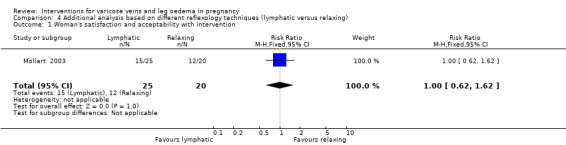
Comparison 4 Additional analysis based on different reflexology techniques (lymphatic versus relaxing), Outcome 1 Woman's satisfaction and acceptability with intervention.
4.2. Analysis.
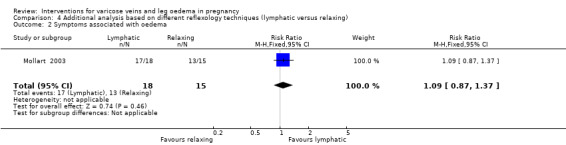
Comparison 4 Additional analysis based on different reflexology techniques (lymphatic versus relaxing), Outcome 2 Symptoms associated with oedema.
Primary outcomes
The trial reported none of the review's primary outcomes.
Secondary outcomes
Women satisfaction and acceptability with the intervention did not differ significantly when compared with rest alone (RR 6.00, 95% CI 0.92 to 39.11; participants = 55; studies = one) (Analysis 3.1). More women in the reflexology group experienced reduction in symptoms of leg oedema compared to the resting group (RR 9.09, 95% CI 1.41 to 58.54; participants = 43; studies = one), (Analysis 3.2).
3.1. Analysis.
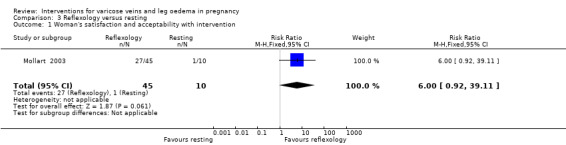
Comparison 3 Reflexology versus resting, Outcome 1 Woman's satisfaction and acceptability with intervention.
3.2. Analysis.
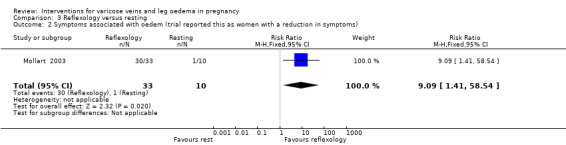
Comparison 3 Reflexology versus resting, Outcome 2 Symptoms associated with oedem (trial reported this as women with a reduction in symptoms).
Data are presented that show significant improvement in all groups for symptoms of varicose veins, including stress, tension, anxiety, discomfort, irritability, pain and tiredness. However, data are not presented separately according to treatment group.
No other secondary outcomes are reported.
4: Additional analysis
Comparing lymphatic reflexology with relaxing reflexology, one trial (Mollart 2003) found no significant differences in woman's satisfaction and acceptability with the intervention (RR 1.00, 95% CI 0.62 to 1.62; participants = 45; studies = one), (Analysis 4.1), or reduction in symptoms associated with oedema (RR 1.09, 95% CI 0.87 to 1.37; participants = 33; studies = one), (Analysis 4.2).
5: Water immersion versus leg elevation
The study by Irion 2011 compared standing water immersion for 20 minutes with sitting upright in a chair with legs elevated for 20 minutes.
Primary outcomes
The trial reported none of the review's primary outcomes.
Secondary outcomes
More women in the water immersion group experienced reduction of leg volume (oedema) compared to women in the leg elevation group (RR 0.43, 95% CI 0.22 to 0.83; participants = 32; studies = one), (Analysis 5.1). No other secondary outcomes were reported.
5.1. Analysis.
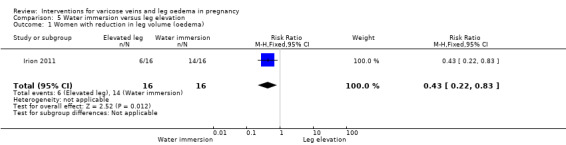
Comparison 5 Water immersion versus leg elevation, Outcome 1 Women with reduction in leg volume (oedema).
6: Foot massage versus routine care
Only one study (Coban 2010) was included under this comparison.
Primary outcomes
None of the review's primary outcomes were reported by the study.
Secondary outcomes
The trial reported no significant difference in lower leg circumference (oedema) when foot massage was compared against routine care (MD ‐0.11, 95% CI ‐1.02 to 0.80; participants = 80; studies = one), (Analysis 6.1). No other secondary outcomes were reported.
6.1. Analysis.
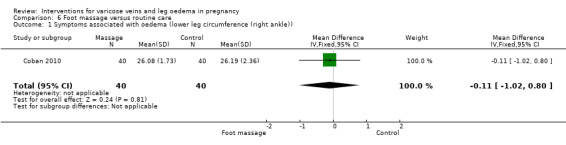
Comparison 6 Foot massage versus routine care, Outcome 1 Symptoms associated with oedema (lower leg circumference (right ankle)).
Subgroup analysis
Due to the limited number of trials included in this review, we did not conduct subgroup analysis to explore heterogeneity.
Discussion
Summary of main results
In this updated review, we examined the effectiveness and safety of any form of intervention used to relieve the symptoms associated with varicose veins and leg oedema in pregnancy. A total of 326 women were recruited into seven trials.
This review unfortunately can provide very little guidance to pregnant women or their carers as the evidence available is insufficient to draw reliable conclusions for clinical practice. The commonest treatments for venous insufficiency in pregnancy are compression stockings and elevation of the feet, however, neither of these methods has been adequately assessed within the context of a randomised controlled trial. No significant differences were found in lower leg volume (oedema) with compression stockings when they were compared against rest or foot massage with routine care.
Rutosides appear to help women with varicose veins experiencing symptoms (nocturnal cramps, feelings of tiredness, paraesthesia). However, it is not yet clear that the drug is safe enough to use in pregnancy and the findings relate to one study only. O‐Beta‐hydroxyethyl rutoside is a semi‐synthetic compound; the mode of action is probably based on a direct effect on the capillary wall as well as capillary functions (Lund 1970; Tschopp 1970). The trial was done 40 years ago; rutoside is no longer popular and the drug safety in pregnancy is not established.
There was a significant reduction in symptoms associated with oedema (less swelling/tightness, less pain/soreness, more mobility, and comfortable/relaxed) when two different techniques of reflexology (relaxing and lymphatic) were compared with rest alone (Mollart 2003). The same study (Mollart 2003), suggested that women who had reflexology were more satisfied with the intervention.
There was evidence, from one trial (Irion 2011), suggesting that water immersion for 20 minutes in a swimming pool compared with sitting upright in a chair with legs elevated for 20 minutes reduced leg volume significantly.
There were no differences found in any other outcomes examined in this review. Of note, all of the outcomes that are reported in this review were only examined in single studies, and it would therefore be difficult to draw any meaningful conclusions. Only one trial Bergstein 1975 that included 69 women, reported data on neonatal mortality and congenital malformations, and did not show a difference between groups.
There was a disappointing lack of information from most trials about maternal satisfaction and acceptability with the intervention, especially given that five of the seven trials were published from 1990 onwards. Due to unclear presentation of data in some published reports, we were unable to extract information for certain outcomes.
Overall completeness and applicability of evidence
Given the paucity of trials, and the absence of relevant and important information from available trials, no reliable conclusions can be made from this review to guide clinical practice regarding the management of women with varicose veins or leg oedema in pregnancy. The possibility of adverse effects remains; the safety of both pharmacological and non‐pharmacological interventions of all the interventions in this review cannot be verified from the available data.
Quality of the evidence
Three outcomes were chosen to be assessed and assigned a quality rating using the GRADE methods for two comparisons: 1. Rutoside versus placebo and 2. External pneumatic intermittent compression versus rest. Evidence was only available for two outcomes 'Symptoms associated with varicose veins and oedema' (change in lower leg volume) and 'Complications associated with varicose veins (deep vein thrombosis)', which came from one study for the comparison of rutoside versus placebo. The evidence for this outcome was graded as 'moderate quality' and the reason for downgrading of evidence was based on including only one study with a small sample size.
Potential biases in the review process
Evidence in this review was derived from studies identified in a detailed search process. Trials comparing interventions of Doppler ultrasound versus no Doppler that have not been published may not have been identified. We attempted to minimise bias in the review process by having two review authors independently extract data.
Agreements and disagreements with other studies or reviews
Four Cochrane systematic reviews have been performed in the non‐pregnant population comparing different interventions (sclerotherapy versus surgery (Rigby 2004). injection sclerotherapy (Tisi 2006), compression stockings (Shingler 2013), surgery (use of tourniquet) (Rigby 2013)) for the treatment of varicose veins.
The evidence supports the current place of sclerotherapy in modern clinical practice, which is usually limited to treatment of recurrent varicose veins following surgery and thread veins (Tisi 2006). There have been no reported differences between the use or non‐use of a tourniquet in terms of complications and morbidity (Rigby 2013).There is insufficient evidence on the use of sclerotherapy or surgery (Rigby 2004). There is insufficient, high quality evidence to determine whether or not compression stockings are effective as the sole and initial treatment of varicose veins in people without healed or active venous ulceration, or whether any type of stocking is superior to any other type (Shingler 2013).
Authors' conclusions
Implications for practice.
Rutosides appear to help relieve the symptoms of varicose veins in late pregnancy. However, this finding is based on one study (69 women) and there are not enough data presented in the study to assess its safety in pregnancy.
Reflexology and water immersion appears to help improve symptoms for women with leg oedema, but again, the findings are based on single studies.
Implications for research.
We are unable to provide clear guidance regarding any form of intervention used to relieve the symptoms associated with varicose veins and leg oedema in pregnancy. We have identified that there is a need for large, well‐designed multicentre randomised controlled trials with clear allocation concealment, which will allow for robust conclusions to be drawn. It is of note that the largest trial included in this review involved only 69 women.
As a result of the findings of this Cochrane review, we make the following suggestions for the design and conduct of future trials investigating the use of any form of intervention used to relieve the symptoms associated with varicose veins and leg oedema in pregnancy.
Large multicentre trials are needed, which look at clinically relevant outcomes; neonatal outcomes, adverse effects and maternal satisfaction.
Data on economic outcomes should be obtained, to allow for allocation of resources and service planning.
It is difficult to blind women and caregivers to their randomised allocation because of the invasive nature of the interventions. It is possible to blind the outcome assessor to treatment allocation, which is strongly recommended. Any blinding should be clearly stated in the trial report.
Trial protocols should be made publicly available in order to allow comparison of the reported outcomes with prespecified outcomes. This will allow outcome reporting bias to be kept to a minimum.
It is essential to involve consumers in any future trials at all stages, and most significantly during the planning stages, in order to identify those outcomes which are deemed of most relevance and importance.
There was no information in any of the included trials regarding long‐term outcomes for women and babies. We propose that future trialists should consider instituting some form of long‐term follow‐up which is feasible and appropriate for the study population in question.
If interventions such as those identified in this review are shown to do more good than harm, the next step would be to establish the optimum dosage, timing of intervention, and which are acceptable to women.
Feedback
Herxheimer, April 2002
Summary
There are six studies listed as 'awaiting assessment'. It would be helpful to know why there has been a delay in assessing them. Also, these titles do not state what rutoside preparations were used. When the review is updated, I suggest that a clear description of each preparation is included, because they may have differed in various ways.
[Summary of comment received from Andrew Herxheimer, April 2002]
Reply
The intervention used in Bergstein 1975 was o‐beta‐hydroxyl ethyl rutoside.
All studies waiting assessment have now been assessed and excluded; reasons for exclusion are summarised in the 'Characteristics of excluded studies' table.
[Reply from Anthony Bamigboye, October 2006]
Contributors
Andrew Herxheimer
What's new
| Date | Event | Description |
|---|---|---|
| 31 May 2015 | New citation required but conclusions have not changed | Four new studies have been included in this update. Methods updated and 'Summary of findings' tables have been included. There are new data for immersion in water and foot massage, although the conclusions remain largely the same. |
| 31 May 2015 | New search has been performed | Updated search identified four new studies (Adamczyk 2013; Coban 2010; Heller 2013; Irion 2011), of which two were included (Coban 2010; Irion 2011), one excluded (Adamczyk 2013), and one placed in ongoing studies (Heller 2013). Two trials (Katz 1990; Marhic 1991) previously excluded are now included in the update. A new review author helped to prepare this update (NA). |
History
Protocol first published: Issue 2, 1998 Review first published: Issue 2, 1998
| Date | Event | Description |
|---|---|---|
| 24 September 2009 | New search has been performed | Search updated. No new trials identified. |
| 11 September 2008 | Amended | Converted to new review format. |
| 8 November 2006 | New citation required but conclusions have not changed | Dr A Bamigboye has taken over responsibility for the updating of this review. Title changed to 'Interventions for varicose veins and leg oedema in pregnancy'. We updated and expanded all sections of the review. New outcomes added to this update include woman's perception of pain, need for pain relief, woman's satisfaction and acceptability with intervention, side‐effects, or adverse events of intervention, stopping of intervention early, complications associated with varicose veins and leg oedema (venous leg ulcer, venous thrombus, thrombophlebitis, bleeding of the varicose vein, deep vein thrombosis, pulmonary embolism, varicose eczema, or venous leg ulcers), admission to neonatal intensive care unit or special care nursery, low Apgar score less than seven at five minutes, duration of hospital stay, cost of hospital stay, and cost associated with intervention. We performed subgroup analysis. The conclusions of this update are unchanged. |
| 8 November 2006 | New search has been performed | New search conducted in October 2006, as a result of which this update includes nine new studies (Coughlin 2001; Marhic 1991a; Mauss 1969; Mollart 2003; Sohn 1995; Steiner 1990; Steiner 1991; Thaler 2001; Tsouderos 1989). All apart from one (Mollart 2003) were excluded. Katz 1990a, which was included in the previous version, has now been excluded. |
| 18 July 2006 | Feedback has been incorporated | Response to feedback added. |
Acknowledgements
Gavin Young and David Jewell conducted the first Cochrane review on this subject (Young 1998). Justus Hofmeyr provided technical advice when needed.
Nasreen Aflaifel's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors alone are responsible for the views expressed in this publication
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Data and analyses
Comparison 1. Rutoside versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Complications associated with varicose veins (deep vein thrombosis) | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.01, 3.49] |
| 2 Symptoms associated with varicose veins (trial reported this as number of women with an improvement in symptoms) | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.89 [1.11, 3.22] |
| 3 Side‐effects, or adverse events of intervention | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.23, 7.28] |
| 4 Neonatal mortality | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Congenital malformation | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. External pneumatic intermittent compression versus rest.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptoms associated with oedema (change in lower leg volume) | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐258.80 [‐566.91, 49.31] |
Comparison 3. Reflexology versus resting.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Woman's satisfaction and acceptability with intervention | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.0 [0.92, 39.11] |
| 2 Symptoms associated with oedem (trial reported this as women with a reduction in symptoms) | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.09 [1.41, 58.54] |
Comparison 4. Additional analysis based on different reflexology techniques (lymphatic versus relaxing).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Woman's satisfaction and acceptability with intervention | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.62, 1.62] |
| 2 Symptoms associated with oedema | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.87, 1.37] |
Comparison 5. Water immersion versus leg elevation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Women with reduction in leg volume (oedema) | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.22, 0.83] |
Comparison 6. Foot massage versus routine care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptoms associated with oedema (lower leg circumference (right ankle)) | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐1.02, 0.80] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bergstein 1975.
| Methods | Randomised controlled trial comparing O ‐ (B‐hydroxyethyl) rutoside (HR) with matching placebo. | |
| Participants | Inclusion criteria: 28 weeks' gestation with visible varicose veins on legs and vulva and subjective complaints, no sign of internal disease or arterial or orthopaedic abnormality of the legs. Exclusion criteria: women on salt‐free diet or taking diuretics or wearing bandages or supportive stockings. |
|
| Interventions | A double‐blind trial that used 300 mg rutoside (O‐Beta‐hydroxylethyl rutoside) 3 times daily in capsule form, for 8 weeks versus placebo from 28 weeks of gestation. Women were assessed by interview at 28 weeks, 32 weeks and 36 weeks' gestation. Leg circumference also taken at these times. Participants were asked to take no other drugs, particularly analgesics. |
|
| Outcomes | Subjective response to treatment judged by reduction in pains and paraesthesiae and reduction in ankle circumference. Neonatal outcomes: live birth, Apgar scores. |
|
| Notes | Women were asked to take the bottles back so that the remaining capsules could be counted and a check made that the dosage had been taken correctly. All women gave birth to healthy babies with good Apgar scores, no further information provided. Sample size: 69 women. Country: The Netherlands. Study years: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation sequence generation not fully described: "two groups randomly allocated". |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study described as double blind. Active drug (rutoside) and placebo capsules were identical in appearance, scent or taste. There was blinding of participants and personnel. Bottles were labelled with randomly‐selected numbers not revealed to the investigator until the end of the trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | There was blinding of participants and personnel/investigator. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 69 women randomised. 3 women lost to follow‐up. 1 woman in the intervention group moved, and 2 women in the placebo group developed deep vein thrombosis. |
| Selective reporting (reporting bias) | Low risk | Outcomes stated of interest have been reported. |
| Other bias | Low risk | None noted. |
Coban 2010.
| Methods | Randomised controlled trial evaluating foot massage for decreasing lower leg oedema, | |
| Participants | Inclusion criteria: healthy pregnant women > 30 weeks' gestation, irrespective of parity, with visible oedema of the ankles and feet, attending Manisa Central Primary Health Care Clinic for antenatal care visits. Exclusion criteria: psychiatric problems, pre‐eclampsia, eclampsia and systemic co‐existing disease. |
|
| Interventions | 20 minutes daily foot massage using baby oil by a professional masseur for 5 consecutive days and usual prenatal care versus usual prenatal care. Survey given to all women on first day. | |
| Outcomes | Lower leg and foot circumference. Demographic characteristics, eating habits and weight gain during pregnancy were also collected. Circumference measurements taken on days 1 and 5 in controls and on days 1, 5 and 7 in the intervention group. | |
| Notes | Study received ethics approval from Ege University Nursing School Ethics Committee. Same paper published in the Midwifery digest 21:1, 2011. Sample size: 80 women. Country: Manisa, Western Turkey. Study years: March 2007 ‐ August 2007. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described. Women matched for age, number of pregnancies and gestational week before randomisation. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described. Personnel and women would have been aware of group assignment due to the need to arrange extra foot massage visits. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding of outcome assessor not described. Women would have been aware of assignment and this may have affected self‐reported data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 80 women randomised, data for all women reported. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Low risk | None noted. |
Irion 2011.
| Methods | Randomised controlled trial comparing standing water immersion for 20 minutes with sitting upright in a chair with legs elevated for 20 minutes. | |
| Participants | Inclusion criteria: healthy pregnant women(at least 34 weeks) with functionally significant lower extremity oedema that limited activity during the last 6 weeks of pregnancy and were cleared medically by their obstetrician. Functionally significant was defined as "visually evident ankle/foot swelling, inability to wear shoes worn prior to pregnancy, and obvious indentation following removal of socks" Exclusion criteria: none stated. |
|
| Interventions | Standing in water immersion for 20 minutes compared with sitting upright in a chair with legs elevated for 20 minutes. Women standing in water were allowed to stand or walk in place. Water temperature was between 29 and 33 degrees celsius. | |
| Outcomes | Measured foot volume. | |
| Notes | Sample size: 32 women. Country: Alabama, USA. Study years: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding of outcome assessor not described/possible due to the nature of the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 32 women randomised, and data for all women reported. |
| Selective reporting (reporting bias) | Low risk | Only 1 outcome, foot volume, appears to have been collected and reported. |
| Other bias | Low risk | None noted. |
Jacobs 1986.
| Methods | Randomised controlled trial comparing external pneumatic intermittent compression with no compression. | |
| Participants | Inclusion criteria: healthy women with normal pregnancies with ankle oedema. Exclusion criteria : chronic illness, varicose veins or leg lesions, who took medications not routinely prescribed in pregnancy or taking oral contraceptives during the year preceding the study. Intervention n = 17 and control n = 18. |
|
| Interventions | External pneumatic intermittent compression for 30 minutes while resting in the left lateral position versus 30 minutes resting in the left lateral position. | |
| Outcomes | Volume changes in the lower leg measured after the 30‐minute treatment and again after a 10‐minute walk. | |
| Notes | The pump unit was approximately 6 x 6 x 3 inches and weighed 1.5 kg. The unit had variable pressure controls over a range of 20 to 60 torr. Total cycling time is 3.2 minutes ‐ 48 seconds to attain pressure, 48 seconds to maintain pressure, and 96 seconds for pressure release. Sample size: 35 women. Country: Utah, USA. Study years: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence from a random numbers table. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. Women were similar, except women in experimental group were closer to their delivery date. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described. Personnel would have been aware of group assignment due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding of outcomes assessors not described, but staff would have been aware of group assignment due to the nature of the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all women presented. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Low risk | None noted. |
Katz 1990.
| Methods | Randomised controlled trial comparing bed rest and immersion in water for treating leg oedema in pregnancy. | |
| Participants | Inclusion criteria: healthy pregnant women aged 26‐35 with singleton pregnancies between 34‐38 weeks' gestation. Total number of recruited participants was not mentioned in the paper. The authors stated that 11 women completed the study, of whom 6 were primigravida, numbers not split per randomised group. Exclusion criteria: none stated. |
|
| Interventions | Group 1: lateral supine bed rest at room temperature. Group 2: sitting in a bathtub of waist‐deep water at 32 ± 0.5 C with leg horizontal. Group3: sitting immersed in shoulder‐deep water at 32 ± 0.5 C with leg extended downward. |
|
| Outcomes | Outcomes reported: maternal heart rate, mean arterial pressure, urine output, haemoglobin, haematocrit, plasma volume, sodium clearance and adverse events. Infant outcomes: live birth, gestation at birth. Although, data not split per randomised group. | |
| Notes | The authors stated that 50 minutes of shoulder immersion in water resulted in more diuresis and mean arterial blood pressure compared to bed rest. It was not possible to trace the authors. "All pregnancies ended with deliveries of infants between 38‐41 weeks gestation". "No women developed complications after the study was finished". Sample size: 11 women, numbers not split per randomised group. Country: North Carolina, USA. Study years: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were 'assigned randomly', sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding of outcomes assessors not described, but staff would have been aware of group assignment due to the nature of the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Total number of recruited participants was not mentioned in the paper. The authors stated that 11 women completed the study. |
| Selective reporting (reporting bias) | Low risk | Selective reporting not apparent. |
| Other bias | Low risk | None noted. |
Marhic 1991.
| Methods | Randomised controlled trial comparing 4 g of troxerutin (Hydroxyethylrutoside) in 2 doses with a placebo. | |
| Participants | Inclusion criteria: pregnant women in their second trimester with symptomatic vulvar varicosities and venous insufficiency in their lower extremities. Exclusion criteria: none stated. |
|
| Interventions | intervention group: 4 g of troxerutin (Hydroxyethylrutoside) in 2 doses. Comparision group: placebo. Study duration: 4 months. |
|
| Outcomes | Pain and discomfort from vulvar varicosities. Pain due to limb venous insufficiency. Heaveness in the legs. |
|
| Notes | The trial examined the efficacy of troxerutin in gynaecology and obstetric. In this review, only information about obstetric populations was included. Data not in useable format. Not able to trace the authors. Sample size: 30 women. Country: France. Study years: not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study described as double blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessor not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 30 women randomised. Data for all women presented. |
| Selective reporting (reporting bias) | Low risk | Selective reporting not apparent. |
| Other bias | Low risk | None noted. |
Mollart 2003.
| Methods | Randomised controlled trial comparing 2 types of reflexology (relaxing foot and lymphatic foot) with no reflexology (control). | |
| Participants | Inclusion criteria: greater than 30 weeks' gestation with visible oedema of ankles and feet, able to speak, read and write English. Exclusion criteria: none stated. |
|
| Interventions | Random allocation of women into either: (i) relaxing foot reflexology technique to the reflex zones of the chest, abdomen, spine, pelvis and head (20 participants); (ii) lymphatic foot reflexology using grapeseed oil to reflex zones of the lymphatic system, liver, gastrointestinal tract and kidneys (25 participants); (iii) control group rested on a couch for equal time duration but received no reflexology (10 participants). Each session lasted 15 minutes approximately. |
|
| Outcomes | Objective ankle and foot circumference measurements, mean scores on stress, tension, anxiety, discomfort, irritability, pain and tiredness levels. Mean well being scores among the 3 groups were also assessed. | |
| Notes | 55 women finished session 1 with complete data, 39 completed session 2 and 20 participants completing session 3. As a result of the dwindling sample size only session 1 has been analysed and presented in the paper 3. Sample size: sample size calculation performed to identify moderate and severe ankle oedema and set at 120 women (40 per randomised group). However, due to limited sample at study hospital this was reset at 60 participants in total. Within the study 69 women were randomised, 7 withdrew after randomisation. Country: Australia. Study years: September 1999 ‐ August 2001. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study described as randomised but sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study described as single‐blind; however, women randomised to either of the 2 groups of reflexology or control (no reflexology) would have been aware of treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Personnel were not blind to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 69 women were randomised. 7 withdrew after randomisation; 1 woman gave birth before the session, and 6 women had incomplete data. Data for 55 women who received at least 1 treatment session. 21% missing data. |
| Selective reporting (reporting bias) | Low risk | Selective reporting not apparent. |
| Other bias | Unclear risk | 1. Authors state "circumference measurements were not able to record the decrease in skin tension and swelling as experienced by the participants". 2. Up to 4 reflexology sessions were planned, but by the third session only 20/69 women remained. Analysis was done on the results of the first session only. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adamczyk 2013 | Study aim was to determine whether prophylactic use of compression stockings would prevent varicose veins. |
| Coughlin 2001 | Eligibility criteria were pregnant women with superficial venous reflux and normal deep veins diagnosed by duplex scan, therefore study not eligible for inclusion in review. |
| Heynen 1972 | Not a randomised controlled trial. |
| Mauss 1969 | Not a randomised controlled trial. |
| Sohn 1995 | Not a randomised controlled trial. |
| Steiner 1990 | Cross‐over study. |
| Steiner 1991 | Cross‐over study. |
| Thaler 2001 | Study aim was to determine whether prophylactic use of compression stockings would prevent varicose veins. |
| Tsouderos 1989 | This was a single administration of Daflon 500 mg on venous haemodynamics in a clinical pharmacological trial. The trial included 3 groups of 10 women; (i) women without varicose; (ii) pregnant women; (iii) post thrombotic syndrome. Data not provided in useable format, result showed a decrease in mean venous capacitance in the pregnancy group. |
Characteristics of ongoing studies [ordered by study ID]
Heller 2013.
| Trial name or title | Preventing the development of venous insufficiency in pregnant women through use of compression stockings. |
| Methods | Randomised controlled trial. |
| Participants | 80 pregnant women without and with varicose veins. |
| Interventions | Compression stockings as a prevention and treatment. |
| Outcomes | Incidence of varicose veins. |
| Starting date | February 2012. |
| Contact information | Jennifer Heller. |
| Notes | No evidence of study completion/publication. |
Differences between protocol and review
Methods have been updated to the current standard text used by Cochrane Pregnancy and Childbirth. 'Summary of findings' tables have been included in this 2015 update.
An outcome previously included, stopping of intervention early, has been removed for this 2015 update. We have added the following outcomes to the review:
Preterm birth (as defined by authors) (not prespecified)
Death (perinatal/neonatal death) (not prespecified)
Congenital malformations (not prespecified)
"Reduction in symptoms associated with varicose veins and oedema" was changed to "Symptoms associated with varicose veins and oedema" in this update.
Contributions of authors
R Smyth (RS) and N Aflaifel (NA) independently identified studies for inclusion and exclusion. RS reviewed the study selection and resolved disagreements on whether the studies had to be included or excluded. RS undertook the data extraction and entered the data into RevMan with NA checking the data entry. RS and NA wrote the results and discussion. NA assessed the quality of the evidence and produced the 'Summary of findings' tables using the GRADE approach. AA Bamigboye commented on the final draft and approved its content.
Sources of support
Internal sources
Effective Care Research Unit, East London, South Africa.
The University of Liverpool, UK.
External sources
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Bergstein 1975 {published data only}
- Bergstein NAM. Clinical study on the efficacy of O‐(Beta‐Hydroxyethyl) Rutoside (HR) in varicosis of pregnancy. Journal of International Medical Research 1975;3:189‐93. [DOI] [PubMed] [Google Scholar]
Coban 2010 {published data only}
- Coban A, Sirin A. Effect of foot massage to decrease physiological lower leg oedema in late pregnancy: a randomized controlled trial in Turkey. International Journal of Nursing Practice 2010;16(5):454‐60. [DOI] [PubMed] [Google Scholar]
- Coban A, Sirin A. Effect of foot massage to decrease physiological lower leg oedema in late pregnancy: a randomized controlled trial in Turkey. MIDIRS Midwifery Digest 2011;21(1):52‐6. [DOI] [PubMed] [Google Scholar]
Irion 2011 {published data only}
- Irion JM, Irion GL. Water immersion to reduce peripheral edema pregnancy. Journal of Women's Health Physical Therapy 2011;35(2):46‐9. [Google Scholar]
Jacobs 1986 {published data only}
- Jacobs MK, McCance KL, Stewart ML. Leg volume changes with EPIC and posturing in dependent pregnancy edema. Nursing Research 1986;35:86‐9. [PubMed] [Google Scholar]
Katz 1990 {published data only}
- Katz VL, Ryder RM, Cefalo RC, Carmichael SC, Goolsby R. A comparison of bed rest and immersion for treating the edema of pregnancy. Obstetrics & Gynecology 1990;75:147‐51. [PubMed] [Google Scholar]
Marhic 1991 {published data only}
- Marhic C. Clinical and rheological efficacy of troxerutine in gynecology and obstetrics. Revue Francaise de Gynecologie et d Obstetrique 1991;86:209‐12. [PubMed] [Google Scholar]
Mollart 2003 {published data only}
- Mollart L. Single‐blind trial addressing the differential effects of two reflexology techniques versus rest, on ankle and foot oedema in late pregnancy. Complementary Therapies in Nursing and Midwifery 2003;9:203‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adamczyk 2013 {published data only}
- Adamczyk A, Krug M, Schnabl S, Hafner H‐M. Compression therapy during pregnancy: boon or bane?. Phlebologie 2013;42(6):301‐7. [Google Scholar]
Coughlin 2001 {published data only}
- Coughlin LB, Gandy R, Rosser S, Cossart L. Pregnancy and compression tights for varicose veins: a randomised trial. Phlebology 2001;16:47. [Google Scholar]
Heynen 1972 {published data only}
- Heynen U. Glyvenol‐‐an integral venodynamic drug. Zeitschrift fur Allgemeinmedizin 1972;48:193‐5. [PubMed] [Google Scholar]
Mauss 1969 {published data only}
- Mauss HJ. Essaven treatment of varicose veins in pregnancy. Medizinische Welt 1969;41:2270‐3. [PubMed] [Google Scholar]
Sohn 1995 {published data only}
- Sohn C, Jahnichen C, Bastert G. Effectiveness of beta‐hydroxyethylrutoside in patients with varicose veins in pregnancy. Zentralblatt fur Gynakologie 1995;117:190‐7. [PubMed] [Google Scholar]
Steiner 1990 {published data only}
- Steiner M, Hillemanns HG. Venostasin retard in the management of venous problems during pregnancy. Phlebology 1990;5:41‐4. [Google Scholar]
Steiner 1991 {published data only}
- Steiner M. Conservative therapy of chronic venous insufficiency. The extent of the edema‐preventive effect of horse chestnut seed extract. Vasa Supplementum 1991;33:217. [PubMed] [Google Scholar]
Thaler 2001 {published data only}
- Thaler E, Huch R, Huch A, Zimmermann R. Compression stockings prophylaxis of emergent varicose veins in pregnancy: a prospective randomised controlled study. Swiss Medical Weekly 2001;131:659‐62. [DOI] [PubMed] [Google Scholar]
Tsouderos 1989 {published data only}
- Tsoderous Y. Are the phlebotonic properties shown in clinical pharmacology predictive of a therapeutic benefit in chronic venous insufficiency? Our experience with Daflon 500mg. International Angiology 1989;8:53‐9. [PubMed] [Google Scholar]
References to ongoing studies
Heller 2013 {published data only}
- Heller J. Preventing the development of venous insufficiency in pregnant women through use of compression stockings: a randomized pilot study. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 21 May 2013] 2013.
Additional references
Bartholomew 2005
- Bartholomew JR, King T, Sahgal A, Vidimos AT. Varicose veins: newer, better treatments available. Cleveland Clinic Journal of Medicine 2005;72(4):312–4, 319–21, 325–8. [DOI] [PubMed] [Google Scholar]
Beebe‐Dimmer 2005
- Beebe‐Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Annals of Epidemiology 2005;15(3):175‐84. [DOI] [PubMed] [Google Scholar]
Campbell 2006
- Campbell B. Varicose veins and their management. BMJ 2006;333(7562):287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carr 2006
- Carr S. Current management of varicose veins. Clinical Obstetrics and Gynecology 2006;49(2):414‐26. [DOI] [PubMed] [Google Scholar]
Criquiui 2003
- Criqui MH, Jamosmos M, Fronek A, Denenberg JO, Langer RD, Bergan J, et al. Chronic venous disease in an ethnically diverse population. American Journal of Epidemiology 2003;158:448‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Enkin 2000
- Enkin M, Keirse MJNC, Neilson J, Crowther C, Duley L, Hodnett E, et al. Unpleasant symptoms in pregnancy. A Guide to Effective Care in Pregnancy and Childbirth. 3rd Edition. Oxford: Oxford University Press, 2000. [Google Scholar]
Feied 2004
- Feied C. Varicose veins. eMedicine World Medical Library. http://www.emedicine.com/ (accessed July 2006).
Hayes 1999
- Hayes J, Cox C. Immediate effects of a five‐minute foot massage on patients in critical care. Complementary Therapies in Nursing and Midwifery 1999;6:9‐13. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Lund 1970
- Lund F, Fagrell B, Kunicki J, Glenne PO. The effect of rutoside in post‐ischaemic and stasis oedema of the rat tail. Progress Cliniques et Therapeutiques dans le Domain de la Phlebology. Apeldoorn, Holland: Stenvert & Son, 1986.
Mashiah 1999
- Mashiah A, Berman V, Thole HH, Rose SS, Pasik S, Schwarz H, et al. Estrogen and progesterone receptors in normal and varicose saphenous veins. Cardiovascular Surgery 1999;7(3):327‐31. [DOI] [PubMed] [Google Scholar]
Pernoll 1991
- Pernoll ML. Current Obstetric & Gynecologic Diagnosis & Treatment. 7th Edition. Appleton and Lange, 1991. [Google Scholar]
Rabhi 2000
- Rhabi Y, Charras‐Arthapignetic C, Gris JC, Ayoub J, Brun JF, Lopez FM, et al. Lower limb vein enlargement and spontaneous blood flow echogenicity are normal sonographic findings during pregnancy. Journal of Clinical Ultrasound 2000;28(8):407‐13. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rigby 2004
- Rigby KA, Palfreyman SJ, Beverley C, Michaels JA. Surgery versus sclerotherapy for the treatment of varicose veins. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD004980] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rigby 2013
- Rigby KA, Palfreyman SJ, Beverley C, Michaels JA. Surgery for varicose veins: use of tourniquet. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD001486.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Risch 1978
- Risch WD, Koubenec HJ, Beckmann U, Lange S, Gauer OH. The effect of graded immersion on heart volume, central venous pressure, pulmonary blood distribution, and heart rate in man. Pflugers Archiv : European Journal of Physiology 1978;374:115–8. [DOI] [PubMed] [Google Scholar]
Shingler 2013
- Shingler S, Robertson L, Boghossian S, Stewart M. Compression stockings for the initial treatment of varicose veins in patients without venous ulceration. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD008819.pub3] [DOI] [PubMed] [Google Scholar]
Stansby 2000
- Stansby G. Women, pregnancy, and varicose veins. Lancet 2000;355:1117‐8. [DOI] [PubMed] [Google Scholar]
Tisi 2006
- Tisi PV, Beverley C, Rees A. Injection sclerotherapy for varicose veins. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD001732.pub2] [DOI] [PubMed] [Google Scholar]
Tschopp 1970
- Tschopp M, Pometta D, Babel J. Diabetic retinopathy . Study of the action of O‐Beta‐hydroxyethyl‐rutosides by retinal fluoresceinography. Diabetologia 1970;6:475‐81. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Bamigboye 2007
- Bamigboye AA, Smyth RMD. Interventions for varicose veins and leg oedema in pregnancy. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD001066.pub2] [DOI] [PubMed] [Google Scholar]
Young 1998
- Young GL, Jewell D. Interventions for varicosities and leg oedema in pregnancy. Cochrane Database of Systematic Reviews 1998, Issue 2. [DOI: 10.1002/14651858.CD001066] [DOI] [PubMed] [Google Scholar]


