Abstract
Introduction:
Healthier school environments can benefit students, and school wellness policies may result in meaningful enhancements. Schools participating in federal child nutrition programs must implement wellness policies as mandated by law. The primary study objective is to assess effectiveness of implementing school-based nutrition and physical activity policies on student BMI trajectories.
Study design:
Cluster randomized trial using 2 × 2 factorial design.
Setting/participants:
Twelve randomly selected schools in an urban district. Students were followed for 3 years through middle school, fifth to eighth grades (2011–2015, n=595 students, 92.3% participation, 85.2% retention).
Intervention:
Specific to randomized condition, support was provided for implementation of nutrition policies (e.g., alternatives to food-based rewards/celebrations) and physical activity policies (e.g., opportunities for physical activity during/after school).
Main outcome measures:
Sex-/age-adjusted BMI percentile and BMI z-score; behavioral indicators. Data collected via standardized protocols.
Results:
Analyses followed intention-to-treat principles, with planned secondary analyses (conducted 2016–2018). Students at schools randomized to receive support for nutrition policy implementation had healthier BMI trajectories over time (F=3.20, p=0.02), with a greater magnitude over time and cumulatively significant effects 3 years post-intervention (β= −2.40, p=0.04). Overall, students at schools randomized to receive the nutrition intervention had an increase in BMI percentile of <1%, compared with students in other conditions, whereas BMI percentile increased 3%–4%. There was no difference in student BMI between those in schools with and without physical activity policy implementation. Examining behavioral correlates in eighth grade, students at schools randomized to the nutrition condition consumed fewer unhealthy foods and sugar-sweetened beverages, and ate less frequently at fast-food restaurants (all p<0.03).
Conclusions:
This cluster randomized trial demonstrated effectiveness of providing support for implementation of school-based nutrition policies, but not physical activity policies, to limit BMI increases among middle school students. Results can guide future school interventions.
Trial registration:
This study is registered at www.clinicaltrials.gov .
INTRODUCTION
Schools have figured prominently in national discourse about policy approaches to prevent childhood obesity because they afford concentrated contact, teach health education, provide meals, and can model health-promoting environments.1–3 In 2004, all school districts participating in the U.S.’s federal meal programs were required to create a committee of stake-holders and write a school wellness policy.4 School wellness policies required schools to set goals for physical education and nutrition education, as well as set nutrition standards for meals and snacks served. Several years later (in 2010, and prior to this study), the scope of school wellness policies was expanded by The Healthy, Hunger-Free Kids Act to include policies on physical activity and food marketing in schools; in addition, school districts must measure policy implementation and share findings publicly.5
There is a robust body of empirical literature that documents that healthier school environments benefit students. For example, quality physical education predicts higher levels of physical activity in school.6 School wellness policies that promote increased access to healthier foods and limit access to unhealthy foods have been linked to lower caloric intake7 and improved student dietary quality8,9 at school. There is emerging evidence that stronger state-level competitive food policies are associated with a healthier weight trajectory among middle school students.10
The rationale behind requiring school wellness policies is that, when implemented, they will lead to meaningful improvements in the school environment. Although nearly every school district in the country has a written policy, several studies have found that strong written policies do not necessarily predict thorough implementation.11–13 School districts face multiple demands and have been expected to implement new policies with little to no additional financial support. One strategy has been to collaborate with local organizations, such as universities, health systems, and community-based organizations, to assist in implementation and evaluation of school wellness policies after they have been written and approved.14,15 The objective of this cluster randomized trial is to assess whether implementation of specific nutrition and physical activity components of the written school wellness policies lead to healthier student outcomes, including BMI trajectories and behavioral correlates. In addition, the study seeks to determine whether these policy interventions are more or less effective for girls or boys and for differences on baseline BMI (i.e., prevention/treatment) based on prior research that has demonstrated these subgroup effects.16,17
METHODS
This study was conducted in New Haven, Connecticut, an urban district with >21,000 students. Using a quantitative coding system to evaluate written school wellness policies in all Connecticut districts, New Haven’s policy scored higher than any other district.18,19 Therefore, it was an ideal setting to assess implementation of a strongly written school wellness policy.
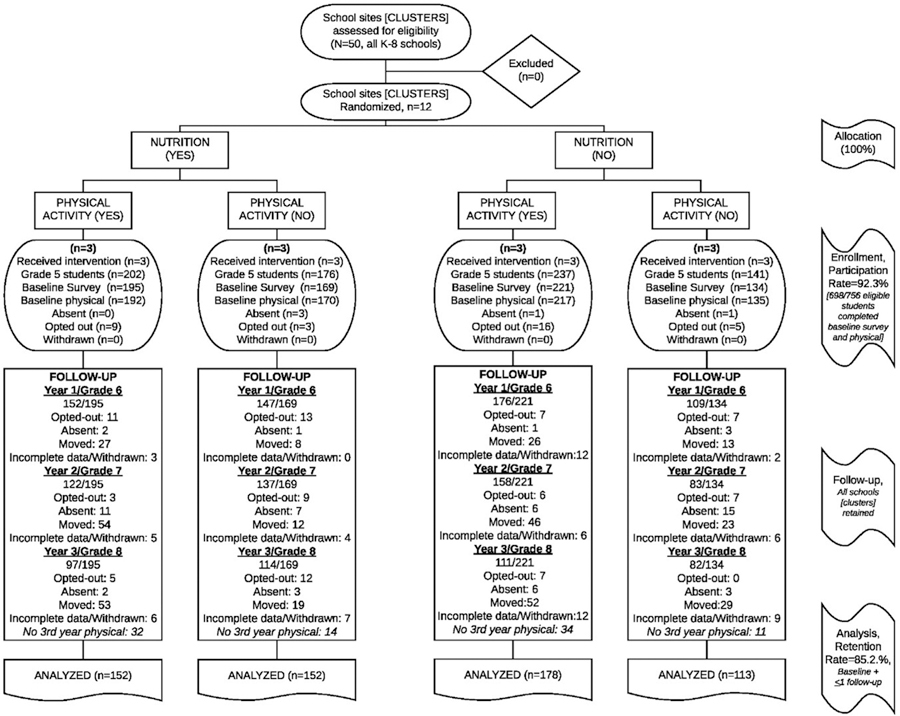
Twelve schools (kindergarten through eighth grade [K–8]) were randomly selected from among the 50 K–8 district schools. All agreed to participate. Schools served as clusters, and were randomized to receive support for school wellness policy implementation via standard 2 × 2 factorial design (Figure 1), such that policy interventions related to nutrition and physical activity were implemented and evaluated, leading to four conditions: nutrition only, physical activity only, nutrition and physical activity (dual), or delayed. Schools randomized to the delayed condition received other health-relevant training (e.g., oral health, cold/influenza prevention) during the study period, with obesity-related materials delivered after data collection was completed. To minimize selection bias, all schools were recruited before randomization. Randomization was achieved using a computer-generated sequence. Enrollment was conducted in 2011, with annual data collection and implementation through 2015.
Figure 1.
CONSORT diagram.
All procedures were approved by Yale University IRB, the New Haven Board of Education, and participating schools, including permission to collect identifying information and track the same students over time. Regulations as established by the Family Educational Rights and Privacy Act20 and the Health Insurance Portability and Accountability Act21 were followed. Parental consent and student assent were obtained, and participation was entirely voluntary and noncoercive. Throughout the entire trial, there were no adverse effects to report. CONSORT with extension to cluster randomized trials guide this report.22
Study Population
Because randomization was conducted by school, all students in these school enrolled in the requisite grades were invited to participate. Of 756 students enrolled in study schools, 698 completed baseline surveys and physical assessments (92.3% participation rate). This high participation rate was achieved working in close partnership with the school district. To minimize participant burden and maximize participation, all data were collected during school. There were no differences in sociodemographic or health indicators between students who completed baseline assessments and those who did not. To be included in the final analytic sample, students were enrolled in fifth grade when the study began (n=533) or began attending a target school in sixth grade (n=62). All had one or more follow-up sessions over the study period (through eighth grade, 2014–2015 academic year), resulting in a final sample of 595 students (85.2% retention; CONSORT diagram in Figure 1). The majority of loss to follow-up was due to movement out of study schools or the district as a whole. Sample size was based on the primary study endpoint: student BMI. With power at 0.80, α set to 0.05, and interclass correlation assumed at 0.001, a total of 12 schools and 588 students were needed to detect small/medium effect (Δ=0.30; software Optimal Design, version 3.0).23
Measures
Research staff provided technical assistance and support to schools to implement components of the district’s written school wellness policy (Table 1), as well as basic and advanced workshops on building a school culture of health for administrators, teachers, and parents twice annually. All schools received $500/year to support a member of the school community (most often teachers) to establish and lead a School Wellness Team. The focus was on different elements of written policy implementation depending on the schools’ randomized study condition. Each school was assigned one research staff member who visited the school one to two times per month. Visits typically included meeting with the School Wellness Team, principal, all teachers for the target grade, school cafeteria manager (nutrition condition), and physical education teachers (physical activity condition). Newsletters were distributed triennially to reinforce targeted health messages (e.g., Rethink Your Drink campaign). Additionally, nutrition interventions included cafeteria-based nutrition promotion to encourage healthy food choices, taste-testing new foods, and providing alternatives for use of food during celebrations. Physical activity interventions included promotion of active transport (walk/bike) to school, integrating physical activity into classroom lessons, and fitness challenges. Table 1 provides a list of interventions to support school wellness policy implementation.
Table 1.
Policies and Study Interventions to Support School Wellness Policy Implementation
| Intervention group | Policies | Implementation support by research staff |
|---|---|---|
| District-wide in all schools | ● Meals served through the National School Breakfast Program and National School Lunch Program will be appealing and attractive to students; will be served in clean and pleasant settings; will include no fried vegetables at K-8 schools; will offer a variety of fruits and vegetables; and will offer only low-fat milk (no flavored milk). All cereals are whole grain. ● Competitive foods will not be sold. ● Students will have physical education class at least 90 minutes per week |
● Create School Wellness Teams each year at each school. Recruit an in-school team leader and pay a stipend to the leader of $500 per year. Attend School Wellness Team meetings and assist in setting annual goals to support the implementation of wellness policies. ● Meet annually with teachers and principals to support the implementation of wellness policies. Provide gift cards for principals to use to incentivize teachers to implement policies in the classroom. |
| Nutrition intervention schools | ● Schools will not use food or beverages as rewards for academic performance or good behavior. Schools will not withhold food or beverages as punishment. ● Schools should limit celebrations that involve food during the school day to no more than one party per class per month. Each party should include no more than one food or beverage that does not meet nutrition standards for food and beverages sold individually. The district will disseminate a list of healthy party ideas to parents and teachers. ● Schools will provide nutrition education to foster lifelong habits of healthy eating. Nutrition education will also extend to the students’ homes via workshops for parents, materials given to students and directly sent to parent/guardians such a school menus and other bulletins. ● Schools should engage students and parents, through taste tests of new entrées and surveys, in selecting foods sold through the school meal programs in order to identify new, healthful, and appealing food choices. |
● Meet with teachers each year and provide materials to support the nutrition education curriculum in the classroom. Provide school with materials that contain messages about healthy beverage choices. ● Meet with food service director and staff regularly to support professional development and ensure that all meals meet federal nutritional criteria, specifically increasing whole grain products and lowering sodium. Ensure all competitive foods meet state standards. ● Meet with principals and teachers each year to ensure that food is not used for celebrations or as a reward in class. Provide alternative strategies to the principals and teachers to reward students. ● Work with cafeteria staff to provide nutrition education activities in the cafeteria, including taste-testing. ● Work with School Wellness Teams to conduct school-wide campaigns to limit sugary drinks and promote water. ● Provide newsletters to be sent home with students with nutrition tips and ideas for healthy snacking. |
| Physical activity intervention schools | ● Schools will provide a quality physical education program that will foster a life-long appreciation for physical fitness through participation in fitness activities. Students will acquire the knowledge to lead a healthy and productive lifestyle. ●Teachers and other school and community personnel will not use physical activity (e.g., running laps, pushups) or withhold opportunities for physical activity (e.g., recess, physical education) as punishment. |
● Support physical education curriculum; provide resources for equipment; focus on exposing students to a variety of activities to enhance lifetime fitness. ● Work with teachers to support the integration of physical activity into the classroom. ● Work with principals and teachers to ensure that there are no punitive uses of physical activity and promote positive physical activity-focused fundraising and celebrations. ● Provide support for physical activity outside of school, including walking/running clubs, use of school building for physical activity after school hours, and participation in community physical activity events. ● Promote school-wide campaigns to increase physical activity, including distribution of individual activity monitors and online tracking program. ● Provide newsletters to be sent home with students with fun family physical activity ideas and information about community physical activity resources |
K–8, kindergarten through eighth grade.
To control for time and attention, time with schools receiving support for both nutrition and physical activity policies was adjusted to be equivalent to the other conditions. As described, for delayed-intervention schools, health-focused messages not related to obesity prevention were implemented, with obesity prevention delivered at the end of the trial.
Data were collected from multiple sources each fall (September–November) and linked via school-assigned identification numbers to protect privacy.24 Student-level demographic data were obtained from the school district administrative database: birthdate, sex, race/ethnicity. Student surveys (English or Spanish) were administered in school computer labs (Surveymonkey.com). To address literacy concerns, all questions and responses were read aloud while students completed surveys online. Research assistants helped students with technical or content-related questions. Surveys took ≅30 minutes, and participants received small gifts after each survey.
Physical measurements were obtained by trained research assistants according to WHO Expanded STEPS protocol.25 Height was measured to nearest half-centimeter using a stadiometer. Weight was measured to nearest 0.10 pound using an electronic flat scale. Primary outcome was BMI, measured annually, from baseline through end of study (fifth to eighth grades). BMI percentile was calculated based on Centers for Disease Control and Prevention age-adjusted and sex-adjusted growth charts.26 Age- and sex-specific BMI percentile is the most commonly used indicator to measure growth and chart overweight/obesity among adolescents.27 Moreover, many students are overweight and obese, and BMI percentile is a better indicator of adiposity, particularly for children with high BMI.28 Outcomes were specified a priori during clinical trial registration (www.ClinicalTrials.gov, ).
An additional focus was concurrent changes of obesogenic behaviors. Nutritional habits were obtained from self-reported student surveys based on nutrition items from the Youth Risk Behavior Survey29 and School-Based Nutrition Monitoring Questionnare.30 Students were asked about foods and drinks consumed yesterday in school, at home, or elsewhere. Surveys were only administered on days when students had school the prior day. Indices were created for consumption of healthy foods (fruit, vegetables, green salad, potatoes-not fried), unhealthy foods (french fries, chips, candy, ice cream, other sweets), healthy drinks (water, milk, 100% juice), and unhealthy drinks (flavored milk; soda; sweetened coffee; and sport, energy, and flavored drinks). Participants also were asked about number of days within past 7 days that they ate at fast-food restaurants and drank sugar-sweetened beverages. Physical activity behaviors were measured based on U.S. Centers for Disease Control and Prevention physical activity recommendations for children (≥60 minutes/day).31
Statistical Analysis
Data analyses were conducted using prespecified hypotheses and intention-to-treat principles, whereby students were assigned to an intervention group based on school of enrollment in fifth grade. Students who transferred from a nonstudy school to a study schools in sixth grade (n=62) were assigned to an intervention group based on sixth grade school. Maximum likelihood approach was used to handle missing observations, with the assumption that any data missing were missing completely at random or missing at random.32 Basic statistics describe students by intervention condition. Differences in categorical variables were compared using the Rao–Scott chi-square test.
Hierarchical linear modeling was conducted to test effects of study condition on outcomes over time. For continuous outcomes —including primary outcomes models using BMI percentile— hierarchical linear mixed models were used; for categorical variables, hierarchical generalized linear mixed models were used33; for count outcomes, generalized linear mixed models Poisson regression was used.34 Models include baseline BMI, sex, nutrition intervention, physical activity intervention, time, and two- and three- way interactions between the intervention conditions X time. In longitudinal data, change in response depends on baseline values (e.g., individuals with high baseline BMI might still have higher BMI at the end of the study simply because of higher starting values).
Because the goal is to understand whether there is differential change to BMI in response to interventions, and whether there is an interaction with time, the authors accounted for baseline BMI using the constrained longitudinal data analysis full likelihood approach35 in which the baseline values, as well as post-randomization values, are modeled as dependent variables. In these models and because of randomization, baseline mean responses for treatment groups were assumed equal following standard methodologic approaches.36,37
Multivariable analyses accounted for multilevel nature of data, adjusting for intra-cluster correlation (ICC) among repeated measures within students and schools, and allowed use of all study timepoints. A random intercept model with no predictors was fit to calculate ICC. A three-level hierarchical model was initially tested; however, the ICC for students within schools was 0 (exactly 0), and ICC for time within students was 0.917. Therefore, the two-level hierarchical model (Time=level 1, Students=level 2) was more parsimonious, producing a better model fit. Models with the lowest Akaike Information Criteria were deemed to have best fit. Compound symmetry covariance structures were best fit for between-individual random effect and within-individuals random error. Time and intercept were included as random effects in the statistical models.
All statistical analyses were conducted using SAS, version 9.4. Final analyses for this paper were conducted upon completion of the trial, with details of student behavior at final year and post-hoc analyses more recently (2016–2018).
RESULTS
Mean age of students at study entry was 10.9 years (SD=0.6). Racial/ethnic categorization generally reflected distribution of students in the district: 47.2% Hispanic, 35.0% black, and 17.8% white/other. Students in study conditions did not differ by age or race. Girls accounted for 54% of participants. The physical activity–only condition had significantly more girls; the largest study school, randomized to this condition, was a school where two thirds of students were female. Mean age- and sex- adjusted BMI percentile did not differ at study entry by intervention (mean=73.1, SD=29.5). Although average BMI could be categorized as healthy weight, more than one half of students were overweight (85th to <95th percentile) or obese (≥95th percentile): 22.5% and 29.2%, respectively (Table 2).
Table 2.
Baseline Characteristics by Intervention Condition (n=595)
| Nutrition (yes) |
Nutrition (no) |
|||||
|---|---|---|---|---|---|---|
| Characteristics | n | Overall (n=595) | PA+ Dual (n=152) | PA− Nutrition only (n=152) | PA+ PA only (n=178) | PA− Delayed (n=113) |
| Age, years, M ± SD | 595 | 10.9 ± 0.62 | 10.9 ± 0.70 | 10.7 ± 0.55 | 10.9 ± 0.62 | 10.9 ± 0.59 |
| Race/ethnicity, % | ||||||
| Hispanic | 281 | 47.2 | 49.3 | 66.5 | 42.1 | 26.6 |
| Non-Hispanic black | 208 | 35.0 | 42.1 | 11.2 | 33.7 | 59.3 |
| Non-Hispanic white | 106 | 17.8 | 8.6 | 22.4 | 24.2 | 14.2 |
| Sex, % | ||||||
| Male | 275 | 46.2 | 50.0 | 50.0 | 37.6 | 49.6 |
| Female | 320 | 53.8 | 50.0 | 50.0 | 62.4 | 50.4 |
| BMI percentile, M ± SD | 595 | 73.1 ± 29.5 | 73.8 ± 27.9 | 73.8 ± 28.1 | 73.0 ± 31.5 | 71.4 ± 30.3 |
| BMI z-score, M ± SD | 595 | 0.89 ± 1.15 | 0.89 ± 1.10 | 0.90 ± 1.06 | 0.90 ± 1.24 | 0.86 ± 1.19 |
| BMI category, % | ||||||
| Underweight | 13 | 2.2 | 2.0 | 0.7 | 3.4 | 2.7 |
| Normal | 270 | 45.4 | 48.0 | 48.0 | 39.3 | 47.8 |
| Overweight | 134 | 22.5 | 24.3 | 23.0 | 23.6 | 17.7 |
| Obese | 178 | 29.9 | 25.7 | 28.3 | 33.7 | 31.9 |
| Nutrition behaviors | ||||||
| Healthy food total/day, M ± SD | 554 | 2.20 ± 1.3 | 2.5 ± 1.3 | 2.1 ± 1.4 | 2.1 ± 1.2 | 2.2 ± 1.3 |
| Unhealthy food total/day, M ± SD | 553 | 2.38 ± 1.7 | 2.5 ± 1.9 | 2.4 ± 1.6 | 2.3 ± 1.7 | 2.2 ± 1.4 |
| Healthy drink total/day, M ± SD | 556 | 2.67 ± 1.3 | 3.0 ± 1.5 | 2.6 ± 1.3 | 2.6 ± 1.3 | 2.6 ± 1.1 |
| Unhealthy drink total/day, M ± SD | 540 | 2.3 ± 2.1 | 2.6 ± 2.2 | 2.4 ± 2.2 | 2.1 ± 1.9 | 2.1 ± 1.9 |
| Ate fast food last week, % | — | 69.1 | 73.0 | 73.0 | 66.3 | 62.8 |
| PA behavior | ||||||
| Meets PA guideline (≥60 minutes/7 days per week), % | — | 20.8 | 22.4 | 19.1 | 24.2 | 15.9 |
| Days/week ≥60 minutes of PA, M ± SD | 505 | 4.0 ± 2.3 | 4.1 ± 2.2 | 3.8 ± 2.3 | 4.2 ± 2.3 | 3.5 ± 2.4 |
PA, physical activity.
There were no notable school-level differences in size or relevant socioeconomic characteristics. Specifically, school size ranged from 465 to 580 students (mean=492), with mean class size constant (20–23 students). Free lunch is available to all students in the district because eligibility is high overall, exceeding 60% in all schools (mean=71.4%).
There was a significant interaction between the nutrition intervention X time (F=3.20, p=0.02): students in schools randomized to receive support for nutrition policies had healthier BMI percentile trajectories (Figure 2A, described in more detail below). There was no significant interaction between the physical activity intervention X time (p=0.94; Figure 2B). Further, there was no significant interaction between the two interventions (p=0.33), and no three-way interaction between nutrition intervention X physical activity intervention X time (p=0.35).
Figure 2.
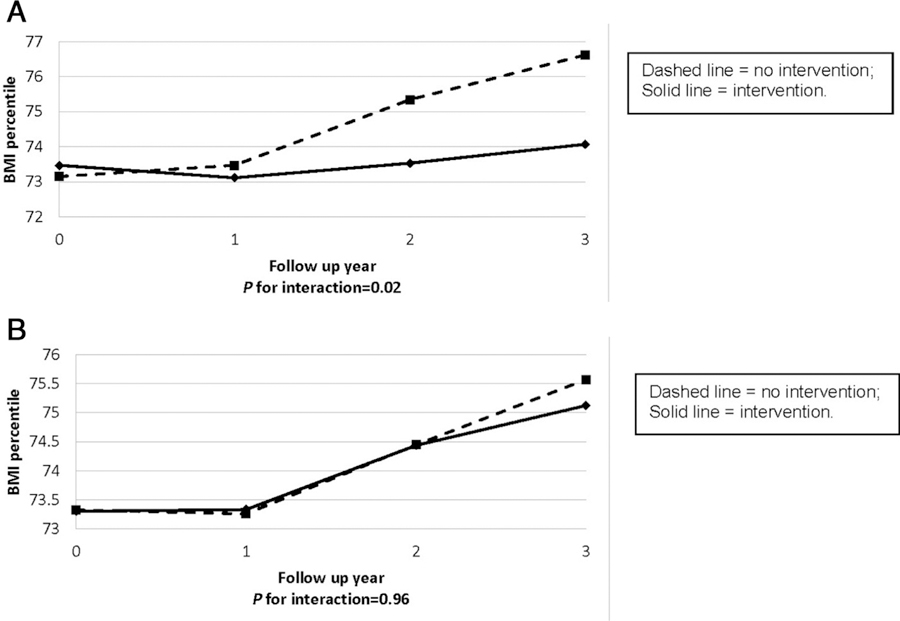
(A) BMI percentile over time by nutrition intervention status. (B) BMI percentile over time by physical activity intervention status. Note: (A) BMI percentile M±SE differences: at baseline (0.32±0.77, p=0.68), 1-year post-intervention (−0.35±0.29, p=0.65), 2 years post-intervention (−1.81±0.85, p=0.034), and 3 years post-intervention (−2.55±0.90, p=0.005). (B) BMI percentile M±SE differences: at baseline (−0.02±0.77, p=0.98), 1-year post-intervention (0.07±0.79, p=0.93), 2 years post-intervention (−0.012±0.85, p=0.99), and 3 years post-intervention (−0.45±0.90, p=0.62).
Examining effects of the interaction between the nutrition intervention X time, there was no significant difference between BMI percentile of students in schools randomized to receive the nutrition intervention versus those who were not at baseline (β=0.65, p=0.55), Year 1 (β=0.01, p=0.99), and Year 2 post-intervention (β=−1.23, p=0.28). However, significant differences emerged during Year 3 post-intervention (β= −2.40, p=0.04). Notably, the magnitude of intervention effects increased over time (Figure 2A). Overall, students at schools randomized to the nutrition-only and dual study conditions had an increase in BMI percentile of less than 1 percentile (0.68 and 0.55, respectively), compared with students at schools randomized to physical activity–only and delayed intervention conditions, where increase in BMI percentile was 2.98 and 3.86, respectively.
Post-hoc analyses were conducted to assure that any skewness in BMI percentile did not impact model specification. Although there was some skewness (−1.09), the plot of residuals of the predicted values did not show any systemic trends and residuals were relatively symmetrical (mean=0.0, variance=0.009).
Additional analyses were conducted to determine whether effects are stable using BMI z-score as the outcome. Students in schools randomized to the nutrition condition were less likely to have an increase in BMI z-score, with stronger cumulative effects over time (Year 2: β= −0.01, Year 3: β= −0.03); however, the primary interaction of nutrition intervention X time was not statistically significant (p=0.16). Consistent with BMI percentile, there was no significant difference by BMI z-score between students in schools randomized to physical activity versus those who were not (Year 2: β=0.09, Year 3: β=0.08).
Given significant effects for students in schools randomized to the nutrition intervention, changes in dietary behaviors over time were examined. Specifically, at the end of the study (eighth grade), students in schools randomized to nutrition interventions reported consuming fewer unhealthy foods (mean=1.83 [SD=0.11] vs mean=2.23 [SD=0.12], β= −0.19, p=0.02), and less frequent consumption of sugar-sweetened beverages (37.95% vs 27.18% drank sugar-sweetened beverages on 2 or fewer days in the past 7 days; OR=1.36, p=0.025) compared with those in schools with no targeted nutrition intervention. These students also were less likely to have had any meals at fast-food restaurants in the past 7 days (26.34% vs 35.20%, OR=0.58, p=0.02). There was no difference in healthy foods or healthy beverage consumption. There was no significant improvement in days per week of ≥60 minutes of physical activity or among the proportion of students who meet physical activity guidelines (≥60 minutes, 7 days/week) among students in schools randomized to the physical activity intervention compared with students in schools not randomized to receive physical activity intervention.
To test for interactions between the interventions with sex, based on an a priori analytic plan, a fully saturated model was run. This included all baseline study indicators (BMI, age, sex, race/ethnicity, nutrition intervention, physical activity intervention, time), as well as the two interaction terms (nutrition X sex, physical activity X sex) and interactions between intervention conditions X by time (nutrition X physical activity, nutrition X time, physical activity X time, nutrition X physical activity X time). There were no statistically significant interactions.
Finally, there was interest in determining whether the nutrition intervention was effective for all students across baseline BMI. There was a significant interaction between time X intervention among students in the BMI healthy weight group (fifth to 84.9th percentile, p=0.04), but not among students underweight, overweight, or obese. Similar to results for the entire study sample, the magnitude of effects increased over time.
DISCUSSION
Students who attended schools that were randomized to receive support to implement nutrition-focused school wellness policies were significantly less likely to experience an increase in BMI across middle school (from fifth through eighth grades) than students in comparison schools. At the end of the study, these students reported lower consumption of unhealthy foods and sugar-sweetened beverages, although there was no effect on consumption of healthy foods and beverages. The magnitude of effects of the nutrition intervention was stronger over time, which is likely a result of increased dose or cumulative impact. This is consistent with two meta-analyses of school-based randomized trials to prevent obesity that indicate that interventions implemented for more than 1 year are more effective.16,38 Recent guidelines to advance implementation of the U.S. Preventive Services Task Force recommendations for childhood obesity treatment recommend behavioral interventions of longer duration.39
By contrast, BMI percentile did not differ among students in schools randomized to support implementation of physical activity policies versus those that did not. There is evidence that nearly all U.S. school districts are adherent to requirements to have a school wellness policy; however, language used to describe physical activity policies tends to be weaker than those used to describe nutrition policies.40 One reason may be that only federal meal programs are subject to state government oversight. Related, a recent study in Washington, DC, documented better implementation of nutrition-related school policies than those for physical education.41
The subgroup of adolescents in the healthy weight range were significantly more likely than other students to experience weight stability, suggesting that “prevention may be better than cure.”17,42 Prevention trials—focused on preventing healthy-weight children from becoming overweight—have documented moderate-to-strong support for school-based interventions that focus on the kinds of nutrition and physical activity initiatives implemented. Reviews indicate that childhood obesity prevention interventions can be effective in reducing adiposity, especially in the most methodologically rigorous studies.16,43 Although nutrition-promoting school environments may be one element of a comprehensive strategy to address childhood obesity, students who are already overweight or obese likely need more tailored, intensive interventions.44 Obese children are at greatest risk for becoming obese adults; clinical management of obesity and its concurrent comorbid conditions is difficult, and it is even more challenging for adults to lose excess weight.
Slowing weight gain in adolescence is clinically important to prevent adult obesity.45 Clinical Practice Guidelines from the Endocrine Society indicate that simply maintaining weight has long-term health benefits for overweight and minimally obese adolescents as they mature.46 Furthermore, elevated BMI among adolescents, even within healthy range, is a significant risk factor for chronic disease in adulthood. For example, for every 1-unit increase in adolescent BMI, Tirosh and colleagues47 reported a 12% increase in expected hazard of coronary heart disease. For a hypothetical student, the observed 3%–4% difference in mean BMI percentile is equivalent to a difference of about 2 pounds; if this trajectory is sustained over time, weight gain would substantially increase risk for severe comorbid conditions associated with overweight and obesity, such as metabolic and cardiovascular risks, as well as musculoskeletal disorders, depression, and more.46
This study was conducted when substantial attention was given to school nutrition environment nationally. The Healthy, Hunger-Free Kids Act required the U.S. Department of Agriculture to update nutrition standards for school meals and competitive foods, as well as provide guidance for school wellness policies.5 New school meal regulations were implemented in the third and fourth years of this study, but the initiation of Smart Snacks did not require any changes because no competitive foods were sold in the district. New regulations for school wellness policies, released after the conclusion of this study, require districts to update, strengthen, and evaluate their own policy compliance. Specifically, districts are required to review and consider evidence-based strategies in determining their goals, and describe public involvement, policy leadership, and an evaluation plan. This increased transparency and community involvement provides an opportunity for parents, educators, and administrators to work together to implement and evaluate improvements to the school environment.
Limitations
There are several limitations to this study. First, neither schools nor researchers could be blinded to study condition. However, bias was minimized by post-recruitment randomization at the school level. Although statistical significance was modest, the effect size was in line with other interventions that have been effective in preventing BMI increase among adolescents.16,38,48 Students were socioeconomically disadvantaged and predominantly Latina and black; therefore, results may not be generalizable to others. Nonetheless, results could inform future interventions aimed at reducing persistent racial and ethnic disparities in obesity. As with any longitudinal study, clinical, behavioral, and psychosocial factors could confound results. School environment, parent involvement, and other external factors are difficult to control. Also, there is no assessment of how effectively each component of school wellness policies was being implemented prior to study participation. And, as always, there are limitations to self-report measures for both nutrition and physical activity behaviors (e.g., lack of accelerometry). BMI itself may be a poor outcome measure of the impact of physical activity interventions: with increased exercise BMI may increase despite decreasing adiposity. Despite these challenges, implementation of nutrition-based school wellness policies reduced obesity-related risk.
There also were notable strengths. Children were followed across the middle school years, when health habits are formed and can be sustained. Outcomes included both biological and behavioral measures. The cluster randomized design brings numerous strengths, evaluating effectiveness under conditions of actual use and generalizability to similar schools. This design maintains rigor and internal validity of a randomized trial, while enhancing external validity through methodologic features identified by Glasgow49: (1) representative patients (i.e., urban settings, not homogenous or least medically complex), (2) diverse ambulatory clinical practice settings (i.e., not just those with greatest expertise, most resources), (3) comparison condition represents standard of care rather than no treatment, and (4) use of multiple outcomes.
CONCLUSIONS
Implementation of school-based nutrition policies should be an important component of multisector interventions to prevent an adverse trajectory of weight gain. This trial—focused on school wellness policy support and implementation—had a larger effect than previous studies, indicating that school-based structural interventions may be particularly promising. School systems should consider earlier interventions; in this study, more than one half of students were already overweight or obese by fifth grade. Adolescents who are obese are significantly more likely than those who are healthy weight to have prediabetes, hypertension, or hypercholesterolemia; and they are at greater risk for bone and joint problems, sleep apnea, and social and psychological problems related to stigmatization and poor self-esteem. Future research must replicate effects and identify potential mechanisms; that is, identify how implementing better nutrition policies improves outcomes. Furthermore, it would be useful to identify factors that influence uptake, fidelity, sustainability, cost, and scale-up of policies and other innovations that improve health outcomes for children and adolescents. Dietz et al.2 suggest that limitations of clinical approaches to obesity prevention and the capacity of the medical system to address social and environmental risk factors re-emphasize the need for school-based and other public health approaches.50 This study provides important evidence to guide future interventions and policy implementation in schools—translating science to improved health of the public.
ACKNOWLEDGMENTS
This study was funded by the National Institute of Child Health and Human Development, NIH (1R01 HD070740, JR Ickovics and MB Schwartz, Multiple PIs), with additional support from the U.S. Centers for Disease Control and Prevention and Yale-Griffin Prevention Research Center (5U48DP000053, JR Ickovics, PI). The funders had no role in the design, implementation, evaluation, or interpretation of this study. More information on the protocol is available at ClinicalTrials.gov .
Footnotes
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Office of Disease Prevention and Health Promotion. Healthy People 2020. www.healthypeople.gov Accessed October 4, 2017.
- 2.Dietz WH, Douglas CE, Browson RC. Vital directions from the National Academy of Medicine. Chronic disease prevention: tobacco avoidance, physical activity and nutrition for a healthy start. JAMA. 2016;316(16):1645–1646. 10.1001/jama.2016.14370. [DOI] [PubMed] [Google Scholar]
- 3.Roberto CA, Swinburn B, Hawkes C, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers and new thinking. Lancet. 2015;385(9985):2400–2409. 10.1016/S0140-6736(14)61744-X. [DOI] [PubMed] [Google Scholar]
- 4.Child Nutrition and WIC Reauthorization Act of 2004. PL 108–265; 118 Stat 729. 108th Congress Sec. 204. www.govtrack.us/congress/bills/108/s2507/text Published 2004 Accessed October 4, 2017.
- 5.Healthy, Hunger-Free Kids Act of 2010. PL 111–296; 124 Stat 3183. 2010 (111th Congress). www.gpo.gov/fdsys/pkg/PLAW-111publ296/pdf/PLAW-111publ296.pdf Accessed October 4, 2017.
- 6.Castillo JC, Clark BR, Butler CE, Racette SB. Support for physical education as a core subject in urban elementary schools. Am J Prev Med. 2015;49(5):753–756. 10.1016/j.amepre.2015.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taber DR, Chriqui JF, Chaloupka FJ. Differences in nutrient intake associated with state laws regarding fat, sugar, and caloric content of competitive foods. Arch Pediatr Adolesc Med. 2012;166(5):452–458. 10.1001/archpediatrics.2011.1839. [DOI] [PubMed] [Google Scholar]
- 8.Chriqui J, Pickel M, Story M. Influence of school competitive food and beverage policies on obesity, consumption, and availability: a systematic review. JAMA Pediatr. 2014;168(3):279–286. 10.1001/jamapediatrics.2013.4457. [DOI] [PubMed] [Google Scholar]
- 9.Hoelscher DM, Moag-Stahlberg A, Ellis K, Vandewater EA, Malkani R. Evaluation of a student participatory, low-intensity program to improve school wellness environment and students’ eating and activity behaviors. Int J Behav Nutr Phys Act. 2016;13:59 10.1186/s12966-016-0379-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taber DR, Chriqui JF, Perna FM, Powell LM, Chaloupka FJ. Weight status among adolescents in states that govern competitive food nutrition content. Pediatrics. 2012;130(3):437–444. 10.1542/peds.2011-3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Budd EL, Schwarz C, Yount BW, Haire-Joshu D. Factors influencing the implementation of school wellness policies in the United States, 2009. Prev Chronic Dis. 2012;9:E118 10.5888/pcd9.110296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sánchez V, Hale R, Andrews M, et al. School wellness policy implementation: insights and recommendations from two rural school districts. Health Promot Pract. 2014;15(3):340–348. 10.1177/1524839912450878. [DOI] [PubMed] [Google Scholar]
- 13.Lucarelli JF, Alaimo K, Belansky ES, et al. Little association between wellness policies and school-reported nutrition practices. Health Promot Pract. 2015;16(2):193–201. 10.1177/1524839914550245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Department of Agriculture Food and Nutrition Service. Team nutrition: local school wellness policies. www.fns.usda.gov/tn/local-school-wellness-policy Published 2017 Accessed October 4, 2017.
- 15.NIH. School nutrition and physical activity policies, obesogenic behaviors and weight outcomes. https://grants.nih.gov/grants/guide/pa-files/PA-13-100.html Published 2013 Accessed October 4, 2017.
- 16.Da Silveira JA, Taddei JA, Guerra PH, Nobre MR. The effect of participation in school-based nutrition education interventions on body mass index: a meta-analysis of randomized controlled community trials. Prev Med. 2013;56(3–4):237–243. 10.1016/j.ypmed.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Karp SM, Gesell SB. Obesity prevention and treatment in school-age children, adolescents and young adults—where do we go from here? Prim Prev Insights. 2015;5:1–4. 10.4137/PPRI.S12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwartz M, Lund A, Grow HM, et al. A comprehensive coding system to measure the quality of school wellness policies. J Am Diet Assoc. 2009;109(7):1256–1262. 10.1016/j.jada.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz M, Henderson K, Falbe J, et al. Strength and comprehensiveness of district school wellness policies predict policy implementation at the school level. J Sch Health. 2012;82(6):262–267. 10.1111/j.1746-1561.2012.00696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Family Educational Rights and Privacy Act. 20 U.S.C. § 1232g; 34 CFR Part 99.
- 21.Health Insurance Portability and Accountability Act. PL 104–191.
- 22.Campbell MK, Piaggio G, Elbourne DR, Altman DG, Consort Group. Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345:e5661 10.1136/bmj.e5661. [DOI] [PubMed] [Google Scholar]
- 23.Raudenbush SW, Spybrook J, Congdon R, et al. Optimal Design Plus Empirical Evidence Software for Multi-level and Longitudinal Research, version 3.0. http://wtgrantfoundation.org/resource/optimal-design-with-empirical-information-od Published 2011 Accessed October 4, 2017.
- 24.Ickovics J, Carroll-Scott A, Peters SM, et al. Health and academic achievement: cumulative effects of health assets on standardized test scores among urban youth in the United States. J Sch Health. 2014;84 (1):40–48. 10.1111/josh.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO. STEPS Surveillance Manual, The WHO STEPwise approach to chronic disease risk factor surveillance. Geneva: WHO; http://apps.who.int/iris/bitstream/10665/43376/1/9241593830_eng.pdf Published 2005 Accessed October 4, 2017. [Google Scholar]
- 26.CDC. About Child and Teen BMI. Atlanta, GA: CDC; www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html Accessed October 4, 2017. [Google Scholar]
- 27.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000. CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002(246):1–190. [PubMed] [Google Scholar]
- 28.Freedman DS, Butte NF, Taveras EM, et al. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–14. Obesity (Silver Spring). 2017;25 (4):739–746. 10.1002/oby.21782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brener ND, Kann L, Shanklin S, et al. Methodology of the youth risk behavior surveillance system–2013. MMWR Recomm Rep. 2013;62 (1):1–20. [PubMed] [Google Scholar]
- 30.Hoelscher DM, Day RS, Kelder SH, Ward JL. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. J Am Diet Assoc. 2003;103(2):186–194. 10.1053/jada.2003.50031. [DOI] [PubMed] [Google Scholar]
- 31.CDC. Physical Activity Basics. Atlanta, GA: CDC; www.cdc.gov/physicalactivity/everyone/guidelines/children.html Accessed October 4, 2017. [Google Scholar]
- 32.Little TD, Jorgensen TD, Lang MK, Whitney E, Moore G. On the joys of missing data. J Pediatr Psychol. 2013;39(2):151–162. 10.1093/jpepsy/jst048. [DOI] [PubMed] [Google Scholar]
- 33.Raudenbush SW, Bryk AS, eds. Hierarchical Linear Models Applications and Data Analysis Methods. 2nd ed Thousand Oaks, CA: Sage Publications, 2002. [Google Scholar]
- 34.Atkins DC, Baldwin SA, Zheng C, Gallop RJ, Neighbors C. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychol Addict Behav. 2013;27(1):166–177. 10.1037/a0029508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liang KY, Zeger S. Longitudinal data analysis of continuous and discrete responses for pre–post designs. SankhyaSer B. 2000;62:134–148. [Google Scholar]
- 36.Vickers AJ, Altman DG. Analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–1124. 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. Hoboken, NJ: Wiley, 2004. [Google Scholar]
- 38.Sbruzzi G, Eibel B, Barbiero SM, et al. Educational interventions in childhood obesity: a systematic review with meta-analysis of randomized clinical trials. Prev Med. 2013;56(5):254–264. 10.1016/j.ypmed.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 39.Wilfley DE, Staiano AE, Altman M, et al. Improving access and systems of care for evidence-based childhood obesity treatment: conference key findings and next steps. Obesity. 2017;25(1):16–29. 10.1002/oby.21712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Piekarz-Porter E, Schermbeck RM, Leider J, Young SK, Chriqui JF. Working on Wellness: How Aligned are District Wellness Policies with the Soon-To-Be Implemented Federal Wellness Policy Requirements? Chicago, IL: National Wellness Policy Study, Institute for Health Research and Policy, University of Illinois at Chicago; 2017. www.go.uic.edu/NWPSproducts. [Google Scholar]
- 41.Snelling A, Belson SI, Watts E, et al. Measuring the implementation of a school wellness policy. J Sch Health. 2017;87(10):760–768. 10.1111/josh.12548. [DOI] [PubMed] [Google Scholar]
- 42.Pandita A, Sharma D, Pandita D, Pawar S, Tarig M, Kaul A. Childhood obesity: prevention is better than cure. Diabetes Metab Syndr Obes. 2016;9:83–89. 10.2147/DMSO.S90783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y, Wu Y, Wilson RF, et al. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis. Rockville, MD: Agency for Healthcare Research and Quality, 2014. Report No.: 13-EHC081-EF. [PubMed] [Google Scholar]
- 44.Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med. 2009;37(5):418–427. 10.1016/j.amepre.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 45.Goldschmidt AB, Wilfley DE, Paluch RA, Roemmich JN, Epstein LH. Indicated prevention of adult obesity: how much weight change is necessary for normalization of weight status in children? JAMA Pediatr. 2013;167(1):21–26. 10.1001/jamapediatrics.2013.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.August GP, Caprio S, Fennoy I, et al. Prevention and treatment of pediatric obesity: an Endocrine Society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab. 2008;93(12):4576–4599. 10.1210/jc.2007-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tirosh A, Shah I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Eng J Med. 2011;364(14):1315–1325. 10.1056/NEJMoa1006992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev. 2009;10(1):110–141. 10.1111/j.1467-789X.2008.00515.x. [DOI] [PubMed] [Google Scholar]
- 49.Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health. 2012;102(7):1274–1281. 10.2105/AJPH.2012.300755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lewallen TC, Hunt H, Potts-Datema W, Zaza S, Giles W. The Whole School, Whole Community, Whole Child Model: a new approach for improving educational attainment and healthy development for students. J Sch Health. 2015;85(11):729–739. 10.1111/josh.12310. [DOI] [PMC free article] [PubMed] [Google Scholar]