Abstract
Background
7.0-T T2-weighted MRI offers excellent visibility of the subthalamic nucleus (STN), which is used as a target for deep brain stimulation (DBS) in Parkinson's disease (PD). A comparison of 7.0-T MRI to microelectrode recordings (MER) for STN border identification has not been performed.
Objective
To compare representation of STN borders on 7.0-T T2 MRI with the borders identified during MER in patients undergoing DBS for PD and to evaluate whether STN identification on 7.0-T T2 MRI leads to alterations in stereotactic target planning.
Design/Methods
STN border identification was done using volumetric 7.0-T T2 MRI acquisitions. This was compared to the STN borders identified by MER. STN target planning was independently performed by 3 DBS surgeons on T2 imaging using 1.5-, 3.0-, and 7.0-T MRI.
Results
A total of 102 microelectrode tracks were evaluated in 19 patients. Identification of the dorsal STN border was well feasible on 7-T T2, whereas the ventral STN was undistinguishable from the substantia nigra. The dorsal STN border on MRI was located more dorsal than MER in 73% of trajectories. The average distance from MRI to MER border was 0.9 mm (range −4.4 to +3.5 mm). STN target planning showed high correspondence between the 3 field strengths.
Conclusion
7.0-T T2 MRI offers the possibility of easy identification of the dorsal border of the STN. However, higher field strength MRI does not change the planning of the target. Compared to MER, the dorsal border on MRI was located more dorsal in the majority of cases, situating MER activity within STN representation.
Keywords: Deep brain stimulation, Subthalamic nucleus, Microelectrode recordings, 7-T MRI
Introduction
Deep brain stimulation (DBS) of the subthalamic nucleus (STN) is an effective surgical treatment for patients with advanced Parkinson's disease (PD) [1]. The dorsolateral part of the STN is considered the optimal location for DBS in PD and was traditionally identified by intraoperative electrophysiological microelectrode recordings (MER) [2].
In recent years, T2-weighted MRI has been applied for STN identification, and some centers now omit MER and rely solely on MRI [3]. Magnetic field strengths have increased, leading to improved STN delineation, and 7.0-T T2 MRI potentially provides superior visualization of the STN (Fig. 1) [4]. However, it is not clear whether this leads to exact representation of the dorsolateral sensorimotor area of the STN as the location determined by MER has not been compared with STN representation on 7.0-T MRI [5, 6].
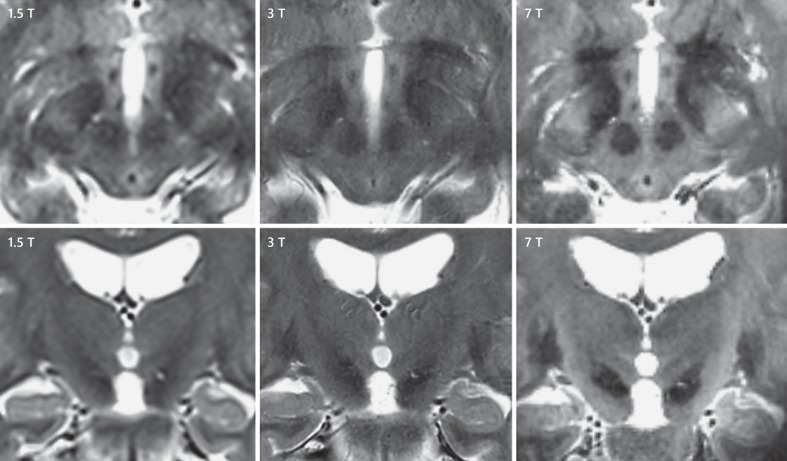
Fig. 1.
Axial and coronal midbrain sections showing the dorsolateral subthalamic nucleus (STN) on 3 different MRI field strengths. Left upper and lower panel, a 1.5-T T2 sequence; middle upper and lower panel, a 3.0-T T2 sequence; and right upper and lower panel, a 7.0-T T2 sequence. All upper panels are axially oriented, and all lower panels are coronally oriented sections. The hypointense STN signal is situated anterolateral to the red nucleus on axially orientated sections - visible as hypointense almond shaped above the substantia nigra on coronally orientated sections. Every increase in field strength results in clearer STN delineation, and the dorsolateral area can best be evaluated on 7.0-T T2 MRI.
We compared STN borders seen on 7.0-T T2-weighted MRI with the borders obtained during MER in patients undergoing DBS for PD. In addition, we evaluated if the superior STN visualization on 7.0-T T2 MRI leads to significant alterations in stereotactic target planning compared to 1.5- and 3.0-T T2 MRI acquisitions.
Methods
Patients
In our DBS center, 1.5-T T2-weighted MRI acquisition is used for STN identification since 2003, whereas 3.0- and 7.0-T T2 MRI were added in 2012 and 2015, respectively, to further optimize STN delineation. For the current retrospective study, data were collected from all patients who underwent awake MER-guided DBS implantation for PD between January 2015 and June 2016 for whom a complete set of 1.5-, 3.0-, and 7.0-T T2-weighted MRI was available.
Surgical Procedure
The surgical procedure of DBS placement was described in detail elsewhere [7]. On the day of surgery, the Leksell stereotactic G frame (Elekta AB, Stockholm, Sweden) was placed, and patients underwent a frame-based 1.5-T stereotactic MRI. Preoperative 3.0- and 7.0-T MRI sequences were coregistered with stereotactic volumetric T1-weighted sequences using SurgiPlan software (Elekta). STN target planning was started with standard stereotactic coordinates relative to the midcommissural point: 11.5 mm in the lateral direction, 2 mm in the posterior direction, and 4 mm in the ventral direction. Target planning was subsequently individually adjusted to the position of the red nucleus and STN representation on 1.5-, 3.0-, and 7.0-T axial and coronal T2 acquisitions. Trajectories were planned entering on top of a frontal gyrus while avoiding ventricle and blood vessel penetration. All patients were operated under local anesthesia, and MER was performed. It was noted when adjustments in ring and arc were needed after burr hole placement for optimizing microelectrode entrance. After the optimal MER trajectory had been determined, the DBS electrode (Cartesia; Boston Scientific, Marlborough, MA, USA, or model 3389, Medtronic Inc., Minneapolis, MN, USA) was implanted. Adequate placement was evaluated with fluoroscopy. Subsequent implantation of the pulse generator in the infraclavicular region was performed under general anesthesia. On the postoperative day, a computed tomography (CT) scan was made to evaluate electrode position, to assess the postoperative pneumocephalus, and to rule out asymptomatic hemorrhage.
Electrophysiologically Defined STN
MER was started 5 or 6 mm above the intended target and advanced with 0.5-mm steps to approximately 2 or 3 mm below the target until the electrophysiological STN signal was lost or the substantia nigra pars reticulata signal was encountered. In most cases, we used 3-track recordings (all concurrent) with the planned trajectory as the central channel and additional lateral and anterior channels at a 2-mm distance from the central channel. Electrophysiological STN activity was recognized as a typical broadening of background noise with tonic and irregular discharge pattern and occasional burst. During surgery, electrophysiological recordings were reviewed and interpreted by the neurophysiologist (Y.D. or W.V.P.), neurologist (R.M.A.B., J.M.D., or V.J.J.O.), and DBS surgeon (P.R.S. or P.M.). For this analysis, electrophysiological recordings were reviewed offline and double checked for the presence of typical STN activity. The dorsal and ventral electrophysiological STN border was determined for each microelectrode track and expressed in millimeter distance to the intended target depth.
7.0-T T2-Weighted MRI- versus MER-Defined STN
Each microelectrode trajectory was projected on volumetric sagittal 7.0-T T2-weighted MRI using SurgiPlan (Elekta). Dorsal and ventral STN borders were identified using axial-, coronal-, and oblique-oriented (trajectory view) imaging and expressed as their respective distance in millimeter to the intended target depth along the MER trajectory. We then compared STN borders as seen on 7.0-T T2-weighted MRI with the borders obtained during MER.
Comparing STN Target Planning on Different T2 Acquisitions of Different MRI Field Strengths
STN target planning was repeated postoperatively for this analysis and independently performed by 3 DBS surgeons (P.R.S., P.M., and M.B.) on axial- and coronal-orientated T2-weigthed MRI using 1.5-, 3.0-, and 7.0-T acquisitions. Different field strengths and cases were offered in random order to prevent possible influence of sequential target determination. STN target planning was started with standard stereotactic coordinates relative to the midcommissural point: 11.5 mm lateral, 2 mm posterior, and 4 mm ventral. Target planning was subsequently optimized based on the red nucleus (Bejjani line [8]) and STN visualization (Fig. 2). The STN contour representation was considered to be lateral to the anterior border of the red nucleus with hypointense head and thinning posterior tail. For comparison of target planning, x, yand z coordinates were compared between the 3 field strengths (intrarater) and between surgeons (interrater) using independent t tests.
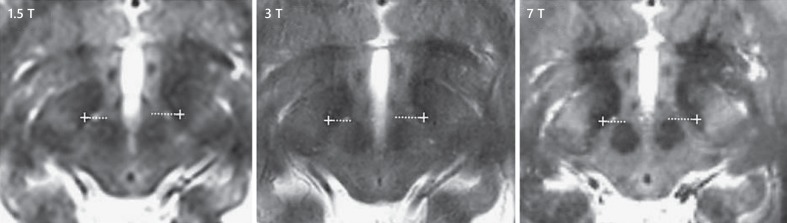
Fig. 2.
Axial midbrain sections showing the subthalamic nucleus (STN) at maximal diameter of the red nucleus on 1.5-, 3-, and 7.0-T T2 MRI sequences. The horizontal white dotted line coincides with the Bejjani line; a white cross indicates the STN target point. A comparison showed high correspondence for x, y, and z STN coordinates between the 3 field strengths (Table 2). This is expected to result from high resemblance of the reference points used: the anterior red nucleus and medial STN border.
MRI Parameters for Each Sequence
T2-weighted MRI was performed for all field strengths.
For 1.5 T (Siemens, Malvern, Pennsylvania), the parameters included the following: repetition time, 5,750 ms; echo time, 99 ms; field of view, 256 × 256 mm; voxel size, 1 × 1 × 2 mm; slice thickness, 2.0 mm; and acquisition time, 4.43 min.
For 3.0 T (Siemens, Malvern, Pennsylvania), the parameters included the following: repetition time, 4,625 ms; echo time, 80 ms; field of view, 230 × 200 mm; voxel size, 0.5 × 0.5 × 2 mm; slice thickness, 2.0 mm; and acquisition time, 4.46 min.
For 7.0 T (Phillips, Healthcare, Cleveland, OH, USA), the parameters included the following: a 3D turbo spin echo (TSE) sequence with TSE factor 182, repetition time, 3,000 ms, TE 296 ms, voxel size, 0.7 × 0.7 × 0.7 mm; slice thickness 0.7 mm, and acquisition time 7.33 min.
Results
From January 2015 until June 2016, 78 PD patients underwent STN DBS in our center. For 19 patients, representing 36 DBS electrodes and 102 microelectrode tracks, a complete set of 1.5-, 3.0-, and 7.0-T T2-weighted MRI was available. There were 13 male patients; average age at surgery of 62 ± 7 years. Two patients underwent unilateral surgery. In 30 hemispheres, 3 microelectrode tracks were conducted and in 6 hemispheres 2.
STN Border Identification on 7.0-T MRI versus MER
Identification of the dorsal STN border was feasible in all patients, whereas the ventral STN could not sufficiently be distinguished from the substantia nigra. In some cases, an estimation could be obtained of the ventral STN border using the coronal orientation. However, this could not be further clarified using the axial and oblique orientations. We therefore limited the comparison between MRI and MER to the dorsal border (Table 1; Fig. 3, 4). In 75 trajectories, typical electrophysiological STN activity was observed. In 55 (73%), the dorsal STN border on 7-T T2-weighted MRI was located more dorsal than on MER, in 18 (24%) the dorsal STN border on 7-T T2-weighted MRI was located more ventral than on MER, and in 2 (3%) both borders coincided (Table 1; Fig. 4). Mean difference between the 7.0-T dorsal STN border was 0.9 mm compared to MER (range −4.4 to +3.5 mm). For the central and anterior microelectrode channel, representing 92% of definite electrode placement, the dorsal STN border on MRI was located more superior in 78% of trajectories compared to MER with an average distance of 1.2 mm (range −1.9 to +3.5 mm). Average distance for the central channels used for implantation was −1.6 mm (range −3.3 to +1.5 mm).
Table 1.
Dorsal STN border comparison between 7-T T2 MRI and MER
| Channels | Trajectories traversing STN on 7.0-T MRI | Trajectories showing typical electrophysiological STN activity | 7.0-T dorsal STN border = MER dorsal STN border | 7.0-T dorsal STN border more dorsal than MER dorsal STN border | 7.0-T dorsal STN border more ventral than MER dorsal STN border | Difference between 7.0-T and MER dorsal STN border, mm | Trajectory used for final electrode placement | Difference between 7.0-T and MER used for dorsal STN border placement, mm |
|---|---|---|---|---|---|---|---|---|
| Central (n = 36) | 35 | 29 (83) | 0 (0) | 25 (86) | 4 (14) | −1.9±1.4 (−4.4 to +1.5)* | 21 (58) | −2.0±1.1 (−3.2 to +1.4) |
| Anterior (n = 36) | 34 | 26 (76) | 1 (4) | 18 (69) | 7 (27) | −0.5±1.7 (−3.2 to +3.5)* | 12 (33) | +0.1±2.1 (−2.8 to + 3.5) |
| Lateral (n = 30) | 20 | 20 (100) | 1 (5) | 12 (60) | 7 (35) | +0.0±1.7 (−2.1 to +2.9) | 3 (8) | −0.5±0.0 (−0.5 to +0.5) |
| All (n = 102) | 89 | 75 (84) | 2 (3) | 55 (73) | 18 (24) | −0.9±1.7 (−4.4 to +3.5)* | 36 (100) | −1.3±1.8 (−3.2 to +3.5) |
For the trajectory distance between dorsolateral STN border, minus indicates MRI border to be located dorsal relative to the electrophysiological border and plus indicates MRI border to be located ventral relative to the electrophysiological border. In columns 3–6, the numbers (%) of trajectories are given. In column 7, differences ± standard deviations (range) are stated.
p < 0.05.
Fig. 3.
Comparison of the dorsal STN border on 7.0-T T2-weighted MRI with its electrophysiologically determined border (MER). a Coronally orientated image of left and right mesencephalic and diencephalic areas: the STN (almond shaped) is situated above the substantia nigra. b The microelectrode trajectory (white dotted line) is superimposed on MRI; the bottom part penetrates the STN. The white box is drawn around this bottom part and enlarged in b′. b′ MER results at 3 stereotactic depths (−3.5, −2.0, and −0.5 mm compared to the planned target depth) along the microelectrode trajectory. The electrophysiological STN at −0.5 mm relative to the planned target depth (green dot) corresponded with the STN representation on 7.0-T MRI. However, at −3.5 and −2.0 mm relative to the planned target depth, the microelectrode trajectory was situated within STN representation on 7.0-T MRI without showing electrophysiological STN activity (red dots). Thus, the dorsal STN border on 7.0-T MRI was located more dorsal than the dorsal STN border on MER.
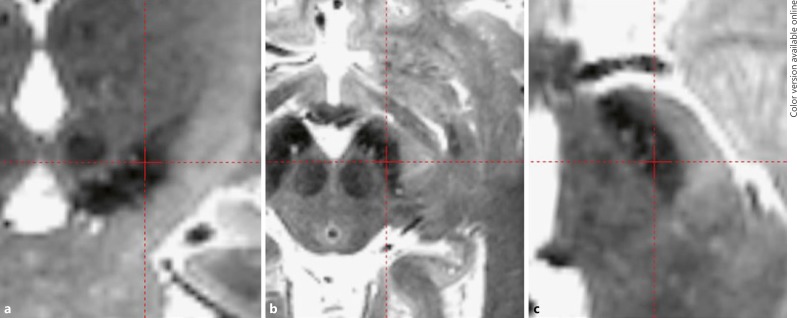
Fig. 4.
Depiction of the ventral STN border on 7.0-T T2-weighted MRI. a Coronal-orientated view of the STN. An estimation could be obtained of the ventral STN border using this orientation. The red cross approximately coincides with the ventral border. However, this could not be further clarified using the corresponding axial (b) and oblique orientations (c). STN could not sufficiently be distinguished from the substantia nigra. We therefore limited the comparison between MRI and MER to the dorsal border.
Comparison of Field Strengths in T2 STN Target Planning
Mean STN target point coordinates relative to the midcommissural point for the 3 DBS surgeons are presented in Table 2. Comparison of 1.5-, 3.0-, and 7.0-T MRI, stereotactic coordinates showed high correspondence between the 3 field strengths (intrarater reliability) and between surgeons (interrater reliability) (Table 2).
Table 2.
Mean STN target point coordinates of 3 DBS surgeons relative to the midcommissural point on 1.5-, 3.0-, and 7.0-T T2-weighted MRI
| Field strength | Lateral, mm |
Posterior, mm |
Inferior, mm |
||||||
| S1 | S2 | S3 | S1 | S2 | S3 | S1 | S2 | S3 | |
|---|---|---|---|---|---|---|---|---|---|
| 1.5 T | 11.0 (0.7) | 10.8 (0.7) | 11.0 (0.5) | 2.7 (0.8) | 2.6 (0.8) | 3.0 (1.0) | 4.6 (0.7) | 4.3 (0.6) | 5.1 (0.7) |
| 3.0 T | 11.0 (0.6) | 10.8 (0.6) | 11.0 (0.7) | 2.8 (0.9) | 2.4 (0.7) | 2.9 (1.0) | 5.0 (0.9) | 4.4 (0.6) | 5.3 (0.7) |
| 7.0 T | 10.7 (0.8) | 10.8 (0.8) | 10.7 (0.9) | 2.6 (0.9) | 2.6 (1.0) | 2.8 (0.9) | 4.9 (0.8) | 4.5 (0.8) | 5.1 (0.8) |
Absolute distances are stated (standard deviations).
Discussion
Dorsal Border of the STN on 7-T MRI
We compared the position of the dorsal STN border on 7.0-T T2 MRI with MER and found the dorsal electrophysiological STN border is situated lower than the STN border seen on 7.0-T MRI in the majority of patients. The difference between MRI and MER dorsal border averaged 0.9 mm but varied from 4.4 mm more dorsal to 3.5 mm more ventral. The STN representation on 7.0-T provides an indication but not an exact representation of the MER activity location in the dorsal STN. To our knowledge, this is the first study comparing dorsal MRI STN on 7.0-T T2 with MER.
STN Targeting: MER or MRI?
Insight into the location of typical electrophysiological STN activity projected on the STN representation on MRI provides a step towards defining a DBS hot spot. As response rate to DBS is correlated to electrode location [9], optimal and thus less variable motor improvement for individual patients may be obtained when the position of the dorsal STN border can be identified more accurately. The dorsolateral electrophysiological STN represents the motor area and contains the optimal location for DBS [10]. Thus far, this part can only be identified directly by intraoperative electrophysiological findings showing increased β-oscillatory activity [2]. When the preoperatively identifiable optimal DBS location on MRI matches the MER findings consistently, MER and test stimulation in awake patients become redundant.
The current analysis indicates that correspondence between MRI and MER can be variable and stresses the necessitation of sequence evaluation before definite implementation in DBS targeting.
STN Targeting using 7.0-T MRI
Our stereotactic STN target point localization comparing 1.5-, 3.0-, and 7.0-T MRI showed high correspondence for x, yand z coordinates. The differences in y and z reached statistical significance, but they are small enough (y < 0.5 mm and z < 0.7 mm) not be considered clinically relevant.
The high correspondence may have resulted from using conventional targeting of reference structures as the red nucleus (Bejjani line) and medial STN border (Fig. 2). Although delineation of these structures is enhanced by 7.0 T, localization does not differ such compared to 1.5-T and 3.0-T field strengths that alterations in planned stereotactic coordinates occur. The added value of 7.0 T over lower field strengths for STN targeting is possibly limited [4]. However, as recently more insight has been obtained regarding the optimal area of stimulation within the 3D STN representation [9], 7.0 T could offer an advantage in the preoperative identification of a theoretical individual DBS hot spot [9, 11, 12]. In the future, tractography and functional connectivity are other possible techniques that could aid in DBS hot spot identification [13]. Its anatomical location could be clearly shown using the image superiority of 7.0 T over lower field strengths [11]. Implementing this hot spot would transform targeting as conventional reference structures possibly become redundant.
Future Perspectives and Study Limitations
Future studies incorporating the dorsal STN on 7.0 T during preoperative stereotactic planning in de novo patients are needed to evaluate the value of its implementation in a prospective manner. In addition to field strength, tractography and quantitative susceptibility mapping could possibly also provide more insight into the stimulation of STN subregions and improve STN substantia nigra discrimination [13, 14].
The current study has several limitations. First, MER trajectories were evaluated using planned trajectories (although intraoperative adjustments in ring and arc were incorporated in the analysis), and MER evaluation was preferably done using intraoperative CT, which directly locates microelectrodes in the stereotactic space. Second, the found range of border differences between MRI and MER in our study could possibly be due to small image fusion errors after coregistration. These errors may be difficult to detect. To optimize registration accuracy between different sequences, all coregistrations were visually inspected by 2 members of the surgical team, one of whom was always a DBS surgeon (P.R.S. or P.M.). Structures used for verification included the anterior and posterior commissure, course of blood vessels, ventricles, outlines of the mesencephalon, and gyri and sulci. We found comparable high visual accuracy of coregistration for all T2-weighted imaging. Third, we cannot exclude that the (small) inaccuracy and imprecision of our stereotactic methods have contributed to the observed difference between 7.0-T MRI- and MER dorsal STN borders: since the STN is convex-shaped and located in oblique fashion, with the dorsal STN located lateral and posterior relative to the ventral STN, an error in mediolateral (x) or anteroposterior (y) direction may have altered the dorsal entry point in the STN of the intraoperative trajectory compared to the planned trajectory.
Conclusion
7.0-T T2-weighted MRI offers the possibility of easy identification of the dorsal border of the STN. However, higher field strength MRI does not change the planning of the target. Compared to MER, the dorsal border was located more dorsal on MRI in the majority of cases, situating MER activity within STN representation.
Disclosures Statement
The DBS team of the Academic Medical Center received financial compensation for teaching courses for the European Continuing Medical Training program. P.R. Schuurman acts as independent advisor for Medtronic, Elekta, and Boston Scientific. M. Caan, W.V. Potters, Y. Dilai, V.J.J. Odekerken, J.M. Dijk. R.M.A. de Bie, M. Bot, and P. van den Munckhof have no disclosures.
References
- 1.Odekerken VJ, van Laar T, Staal MJ, Mosch A, Hoffmann CF, Nijssen PC, et al. Subthalamic nucleus versus globus pallidus bilateral deep brain stimulation for advanced Parkinson's disease (NSTAPS study): a randomised controlled trial. Lancet Neurol. 2013 Jan;12((1)):37–44. doi: 10.1016/S1474-4422(12)70264-8. [DOI] [PubMed] [Google Scholar]
- 2.Gross RE, Krack P, Rodriguez-Oroz MC, Rezai AR, Benabid AL. Electrophysiological mapping for the implantation of deep brain stimulators for Parkinson's disease and tremor. Mov Disord. 2006 Jun;21((S14 Suppl 14)):S259–83. doi: 10.1002/mds.20960. [DOI] [PubMed] [Google Scholar]
- 3.Aviles-Olmos I, Kefalopoulou Z, Tripoliti E, Candelario J, Akram H, Martinez-Torres I, et al. Long-term outcome of subthalamic nucleus deep brain stimulation for Parkinson's disease using an MRI-guided and MRI-verified approach. J Neurol Neurosurg Psychiatry. 2014 Dec;85((12)):1419–25. doi: 10.1136/jnnp-2013-306907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Laar PJ, Oterdoom DL, Ter Horst GJ, van Hulzen AL, de Graaf EK, Hoogduin H, et al. Surgical accuracy of 3-tesla versus 7-tesla magnetic resonance imaging in deep brain stimulation for parkinson disease. World Neurosurg. 2016 Sep;93:410–2. doi: 10.1016/j.wneu.2016.06.084. [DOI] [PubMed] [Google Scholar]
- 5.Verhagen R, Schuurman PR, van den Munckhof P, Contarino MF, de Bie RM, Bour LJ. Comparative study of microelectrode recording-based STN location and MRI-based STN location in low to ultra-high field (7.0 T) T2-weighted MRI images. J Neural Eng. 2016 Dec;13((6)):066009. doi: 10.1088/1741-2560/13/6/066009. [DOI] [PubMed] [Google Scholar]
- 6.Hamani C, Richter EO, Andrade-Souza Y, Hutchison W, Saint-Cyr JA, Lozano AM. Correspondence of microelectrode mapping with magnetic resonance imaging for subthalamic nucleus procedures. Surg Neurol. 2005 Mar;63((3)):249–53. doi: 10.1016/j.surneu.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 7.Bot M, Bour L, de Bie R, Contarino MF, Schuurman R, van den Munckhof P. Can we rely on susceptibility-weighted imaging (swi) for subthalamic nucleus identification in deep brain stimulation surgery? Neurosurgery. 2015 doi: 10.1227/NEU.0000000000001130. [DOI] [PubMed] [Google Scholar]
- 8.Bejjani BP, Dormont D, Pidoux B, Yelnik J, Damier P, Arnulf I, et al. Bilateral subthalamic stimulation for Parkinson's disease by using three-dimensional stereotactic magnetic resonance imaging and electrophysiological guidance. J Neurosurg. 2000 Apr;92((4)):615–25. doi: 10.3171/jns.2000.92.4.0615. [DOI] [PubMed] [Google Scholar]
- 9.Bot M, Schuurman PR, Odekerken VJ, Verhagen R, Contarino FM, De Bie RM, et al. Deep brain stimulation for Parkinson's disease: defining the optimal location within the subthalamic nucleus. J Neurol Neurosurg Psychiatry. 2018 May;89((5)):493–8. doi: 10.1136/jnnp-2017-316907. [DOI] [PubMed] [Google Scholar]
- 10.Zaidel A, Spivak A, Grieb B, Bergman H, Israel Z. Subthalamic span of beta oscillations predicts deep brain stimulation efficacy for patients with Parkinson's disease. Brain. 2010 Jul;133((Pt 7)):2007–21. doi: 10.1093/brain/awq144. [DOI] [PubMed] [Google Scholar]
- 11.Plantinga BR, Temel Y, Duchin Y, Uludag K, Patriat R, Roebroeck A, et al. Individualized parcellation of the subthalamic nucleus in patients with parkinson's disease with 7t mri. Neuroimage. 2016 doi: 10.1016/j.neuroimage.2016.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akram H, Sotiropoulos SN, Jbabdi S, Georgiev D, Mahlknecht P, Hyam J, et al. Subthalamic deep brain stimulation sweet spots and hyperdirect cortical connectivity in Parkinson's disease. Neuroimage. 2017 Sep;158:332–45. doi: 10.1016/j.neuroimage.2017.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lambert C, Zrinzo L, Nagy Z, Lutti A, Hariz M, Foltynie T, et al. Confirmation of functional zones within the human subthalamic nucleus: patterns of connectivity and sub-parcellation using diffusion weighted imaging. Neuroimage. 2012 Mar;60((1)):83–94. doi: 10.1016/j.neuroimage.2011.11.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu T, Eskreis-Winkler S, Schweitzer AD, Chen W, Kaplitt MG, Tsiouris AJ, et al. Improved subthalamic nucleus depiction with quantitative susceptibility mapping. Radiology. 2013 Oct;269((1)):216–23. doi: 10.1148/radiol.13121991. [DOI] [PMC free article] [PubMed] [Google Scholar]