Abstract
To achieve universal health coverage, the scale-up of high impact public health interventions is essential. However, scale-up is challenging and often not successful. Therefore, a systematic review was conducted to provide insights into the factors influencing the scale-up of public health interventions in low- and middle-income countries (LMICs). Two databases were searched for studies with a qualitative research component. The GRADE-CERQual approach was applied to assess the confidence in the evidence for each key review finding. A multi-level perspective on transition was applied to ensure a focus on vertical scale-up for sustainability. According to this theory, changes in the way of organizing (structure), doing (practice) and thinking (culture) need to take place to ensure the scale-up of an intervention. Among the most prominent factors influencing scale-up through changes in structure was the availability of financial, human and material resources. Inadequate supply chains were often barriers to scale-up. Advocacy activities positively influenced scale-up, and changes in the policy environment hindered or facilitated scale-up. The most outstanding factors influencing scale-up through changes in practice were the availability of a strategic plan for scale-up and the way in which training and supervision was conducted. Furthermore, collaborations such as community participation and partnerships facilitated scale-up, as well as the availability of research and monitoring and evaluation data. Factors influencing scale-up through a change in culture were less prominent in the literature. While some studies articulated the acceptability of the intervention in a given sociocultural environment, more emphasis was placed on the importance of stakeholders feeling a need for a specific intervention to facilitate its scale-up. All identified factors should be taken into account when scaling up public health interventions in LMICs. The different factors are strongly interlinked, and most of them are related to one crucial first step: the development of a scale-up strategy before scaling up.
Keywords: Scale-up, public health interventions, barriers and facilitators, LMICs, systematic review
Key Messages
Scale-up is a complex process. Applying the multi-level perspective on transition to scale-up provides a useful framework with a specific focus on how public health interventions in low- and middle-income countries (LMICs) could be embedded in a certain landscape, through changes in the way of organizing (structure), doing (practice) and thinking (culture).
A systematic review of the literature found that resources, advocacy, the supply chain and policies and guidelines were the main factors influencing scale-up related to structure, while training and supervision, scale-up strategy, collaborations, and research and monitoring and evaluation and the social–cultural environment were factors influencing scale-up related to practice and culture, respectively. The interlinkages of the different factors influencing scale-up highlight the importance of a holistic approach to scale-up.
For the scale-up of public health interventions in LMICs, an a priori development of a scale-up strategy is an essential step for success. This scale-up strategy provides a base for policymakers and programme managers on how changes in structure, practice and culture could be facilitated and how to manage and adapt the scale-up process within the existing landscape to ensure sustainable scale-up.
Introduction
Worldwide, a multitude of public health interventions have been implemented mostly at small scale (WHO/ExpandNet, 2011). However, the impact of these small-scale interventions often remains limited to the implementation area and outcomes of these interventions are generally not sustainable (WHO/ExpandNet, 2011); especially, delivering proven health interventions to the poorest and most remote communities in low- and middle-income countries (LMICs) remains a serious problem (Yamey, 2012). To achieve universal health coverage, successful small-scale interventions need to cover broader populations in various settings, especially in LMICs. Therefore, the scale-up of public health interventions is essential (Milat et al., 2015). Nevertheless, ‘scale-up is challenging and not always successful’ (Smith et al., 2015). Interventions that have shown to be successful at small scale cannot simply be expanded to cover a broader population (Smith et al., 2015).
Multiple definitions of scale-up are identified in the literature, and generally, there is no commonly agreed definition (Yamey, 2012). A distinction can be made between scale-up as an objective such as ‘an intervention at scale’ and scale-up as a process where scale-up will lead to a certain outcome such as universal health coverage (Mangham and Hanson, 2010). According to the WHO/ExpandNet (2010), scale-up is: ‘deliberate efforts to increase the impact of successfully tested pilot, demonstration or experimental projects to benefit more people and to foster policy and programme development on a lasting basis’. There is a distinction between vertical scale-up and horizontal scale-up. Horizontal scale-up refers to the expansion or replication of an intervention, whereas vertical scale-up refers ‘to the policy, political, legal, regulatory, budgetary or other health systems changes needed to institutionalize the innovation at the national or sub-national level’ (WHO/ExpandNet, 2010). To ensure that scale-up is sustainable and that the upgraded changes will remain after the scale-up process has ended, vertical scale-up is crucial (WHO/ExpandNet, 2009; Yamey, 2012; Ghiron et al., 2014). This means that fundamental changes in the existing system are needed, which can be seen as a transition (Grin et al., 2010). One of the frameworks used to understand transitions is the ‘multi-level perspective on transition’. This framework views transitions as non-linear processes and describes the interaction of processes at the following three analytical levels: niches, regimes and landscape (Van der Ham et al., 2013). A niche is ‘a specific type of societal subsystem’ (Van den Bosch and Rotmans, 2008, p. 31), which can be seen as the pilot intervention in the case of scale-up. The regime entails ‘the dominant structure, culture and practices through which actors interact’ (Van der Ham et al., 2013; Table 1).
Table 1.
Definitions of structure, practice and culture
| Structure | ‘Physical infrastructure, economic infrastructure and institutions’ (Grin et al., 2010, p. 109). |
| Practice | ‘What people actually do, how they actually work and behave’ (Van der Ham et al., 2013, p. 127). |
| Culture | ‘The set of shared values, perceptions and interpretative frames of the involved actors’ (Essink, 2012, p. 15). |
The landscape entails ‘the broader societal trends and contexts of transitions, such as demographics, culture, and values’ (Van der Ham et al., 2013). Scaling up public health interventions at niche level implies that these interventions will be transformed into mainstream practice at regime level (i.e. integrated into the existing health system), and this transformation is influenced by the landscape (i.e. contextual factors such as the existing norms and values; Van den Bosch and Rotmans, 2008). To move from a practice at niche level to a mainstream practice at regime level, changes in or new constellations of the structure (way of organizing), practice (way of doing) and culture (way of thinking) need to take place (Van den Bosch and Rotmans, 2008). In this article, we define scale-up according to the definition provided by the WHO/ExpandNet and we apply the multi-level perspective on transition to understand how various factors influence scale-up, and in particular vertical scale-up for sustainability.
Over the past years, the concept of scaling up has become increasingly popular (WHO/ExpandNet, 2010) and multiple initiatives in LMICs have explored how successful small-scale interventions can be scaled up (Yamey, 2012). To increase the success rate of these initiatives, ‘understanding the factors influencing scale-up is clearly important’ (Spicer et al., 2014, p. 30). Over the past 10 years, the number of publications on the scale-up of health interventions has increased significantly (Mangham and Hanson, 2010). In addition, the number of studies describing frameworks for scaling up health interventions has increased (Milat et al., 2015) and, recently, some studies have been published on the costs of scale-up (Tromp et al., 2013; Ying et al., 2014; Kripke et al., 2016). Two reviews have listed barriers and facilitators to scale-up (Pérez-Escamilla et al., 2012; Milat et al., 2015). However, these reviews provide limited information explaining ‘how’ factors influence scale-up, while understanding this is important to inform future scale-up of public health interventions. Building on the results of the existing reviews, this review aims to contribute to filling the knowledge gap on why certain public health interventions are successfully scaled up and others not in LMICs. It uses a multi-level perspective on transitions to ensure a focus on vertical scale-up and therefore sustainability.
Methodology
A qualitative systematic literature review was conducted to allow gaining in-depth understanding of the factors influencing scale-up.
Criteria for considering studies for this review
The review included primary studies with a qualitative research component. The included studies needed to have a focus on the scale-up of public health interventions in LMICs and describe facilitators and/or barriers to scale-up as (part of the) results and/or discussion section. We defined public health interventions as ‘interventions that are intended to promote or protect health or prevent ill health in communities or a population. These are distinguished from clinical interventions, which are intended to prevent or treat illness in individuals’ (Milat et al., 2015).
Search methods for the identification of studies
The following two databases were used: PubMed and POPLINE. English studies from 2010 to August 2019 were included. Year 2010 was chosen as the cut-off point as described by Milat et al. (2015), and our own first scanning of the literature showed that literature on scaling up has significantly expanded over the past years. The search comprised three different phases. In the first phase, for the PubMed search, we used the existing search strategy of a narrative review by Milat et al. (2015) as this was the most recent review on scale-up. We slightly adapted the strategy because of our focus on LMICs. For the POPLINE search, the PubMed search strategy was simplified and used only two search terms. This was done to identify as many studies as possible. In the second phase, to assure that no studies were missed, a second search included specific disease/health areas addressed by public health interventions receiving global attention: tuberculosis, malaria, human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS), sexual and reproductive health and rights and water, hygiene and sanitation. These terms were selected based on the search of phase 1, which showed that literature on scaling up public health interventions mostly focused on these areas. The search strategy is shown in Supplementary File S1. In the third phase, a hand search of references of selected full-text articles took place.
Selection of studies
One researcher assessed the titles of the studies, and if the title seemed relevant to the objective of this review, the abstract was retrieved. Two researchers independently assessed these abstracts to evaluate their potential eligibility, and those that were clearly irrelevant were discarded at this stage. The full texts of all studies identified as potentially relevant by both researchers were retrieved. These studies were then assessed independently by three researchers, based on the review’s inclusion criteria and delimiters (Table 2). At all stages, disagreements between the researchers were resolved via discussion.
Table 2.
Overview of inclusion criteria and delimiters
| Primary studies with a qualitative research component |
| Studies focusing on scale-up of a public health intervention |
| Studies describing barriers and facilitators of scale-up |
| Studies conducted in LMICs |
| English language studies |
| Full-text available studies |
| Studies published between 2010 and August 2019 |
Data management
A data extraction form in Excel facilitated the collection of information about the characteristics of the study (authors, methods, etc.), the characteristics of the intervention and the scale-up, and the barriers and facilitators to scale-up. The data extraction form was filled for each included study by one researcher. Thereafter, a second researcher read the same studies and added to and adjusted the filled data extraction form.
Assessment of confidence and quality
To assess the confidence of evidence of the key qualitative review findings, the GRADE-CERQual approach was applied (Lewin et al., 2018b). The GRADE-CERQual approach entails an assessment of the following four different components for each individual review finding: (1) methodological limitations, (2) coherence, (3) adequacy and (4) relevance (Table 3).
Table 3.
Components of GRADE-CERQual approach (Lewin et al., 2018b, p. 5)
| 1. Methodological limitations | ‘The extent to which there are concerns about the design or conduct of the primary studies that contributed evidence to an individual review finding’ (Lewin et al., 2018a, p. 1) |
| 2. Coherence | ‘An assessment of how clear and cogent the fit is between the data from the primary studies and a review finding that synthesizes that data’ (Lewin et al., 2018a, p. 1) |
| 3. Adequacy | ‘An overall determination of the degree of richness and quantity of data supporting a review finding’ (Lewin et al., 2018a, p. 1) |
| 4. Relevance | ‘The extent to which the body of data from the primary studies supporting a review finding is applicable to the context specified in the review question’ (Lewin et al., 2018a, p. 1) |
To assess the first component of the GRADE-CERQual approach, the methodological limitations, the Critical Appraisal Skills Programme method was used (CASP, 2017). Two researchers independently assessed the methodological quality of each included study, and during this assessment, there was a specific focus on whether the data analysis was sufficiently rigorous. The other three components of the GRADE-CERQual components were jointly assessed by two researchers. Based on the four components, an overall assessment of the confidence of the evidence of each of the key review findings was made (Lewin et al., 2018a). In general, downgrading took place during the assessment of the overall confidence of the key review findings, especially when there were strong concerns regarding methodological limitations.
Data extraction and synthesis
Extracted data on factors influencing the scale-up of public health interventions in LMICs were categorized in common themes through an inductive approach. Data were coded according to these themes in NVivo 11 and categorized in overarching themes following the multi-level perspective on transition: factors influencing a change in structure, practice or culture. When factors were related to more than one theme, it was assigned to the theme where most of the studies focused on. After data extraction, narratives for each theme were developed and discussed within the team.
Results
In this section, first an overview of the search approach and the included articles is provided, followed by the findings describing different factors influencing scale-up.
A total of 5019 articles were identified, of which 1207 articles were duplicates and, therefore, excluded. A total of 3812 articles were reviewed, of which 295 articles were included for abstract reading. Based on the abstracts, 68 full-text studies were reviewed, of which 26 studies met the inclusion criteria. One study was identified through hand-searching reference lists, and therefore, 27 studies were included for data extraction (Figure 1). Supplementary File S2 provides an overview of the reasons for excluded studies.
Figure 1.
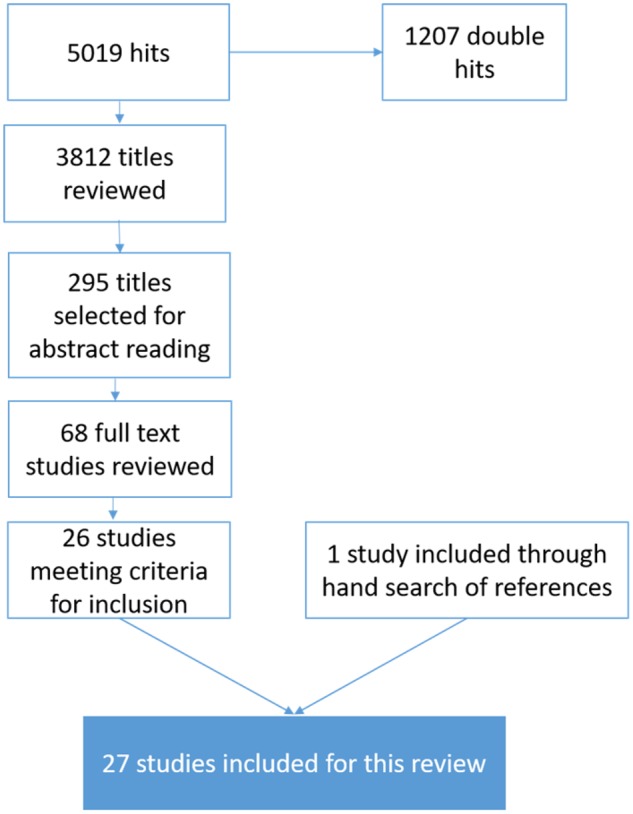
Flowchart of search results.
Of the 27 studies included, five studies reported about two programme scale-ups.1 The studies were conducted in a variety of geographical areas: 14 studies focused on Africa, 3 studies focused on Asia and 1 study focused on South America. Furthermore, six studies concentrated on multiple countries in Africa and Asia, one study included Africa, Asia and South America and two studies were more generic and included LMICs in general. The studies included a variety of public health interventions that were scaled up: 17 studies reported data on scaled up interventions related to sexual and reproductive health and rights including HIV and AIDS; 6 studies concerned the scale-up of community health interventions, such as the management of childhood illness; 1 study presented data on a scaled intervention on depression; 1 study presented intervention on the treatment and safe storage of household water; and 2 studies reported public health interventions in general. Eleven studies provided a definition of scale-up and four of the described project or programme scale-ups used a framework to guide their scale-up approach: three used ExpandNet and one used the Comprehensive Care Management and Treatment Plan. Seven studies applied the ExpandNet framework retrospectively to analyse how scale-up had taken place. Seven of the 11 studies providing definitions of scale-up highlighted sustainability. Table 4 provides an overview of included studies.
Table 4.
Overview of included studies
| Author (year) | Intervention | Country | Definition of scale-up | Use of framework to inform scale-up |
|---|---|---|---|---|
| Ansbro et al. (2015) | Point-of-care rapid syphilis tests | Zambia | No | No |
| Araya et al. (2012) | National Depression Detection and Treatment Programme | Chile | Yes: ‘an increased supply of services, which ideally should be built on a scientific evidence-base and be sustainable over time’ | No |
| Bellows et al. (2016) | Family planning through supply and demand strengthening | Zambia | No | No |
| Blauvelt et al. (2018) | Free health and nutrition hotline | Malawi | No | No |
| Fitzgerald et al. (2016) | Early Infant Male Circumcision | Kingdom of Swaziland | No | No |
| Gergen et al. (2018) | Performance-based financing programme on HIV and maternal–child health services | Mozambique | Yes: ‘the benefit of more people through increased service and population coverage and the cultivation of policy and sustainable programme development’ | No |
| Ghiron et al. (2014) | Community-based efforts to simultaneously address population issues, public health concerns, environmental conservation and sustainable livelihoods | Kenya and Uganda | No | Yes, ExpandNet |
| Goga and Muhe (2011) | The Integrated Management of Childhood Illness Strategy | 27 countries of all 6 WHO regions | No | No |
| Hainsworth et al. (2014) | Adolescent contraceptive services | Ethiopia, Mozambique, Ghana, Tanzania and Vietnam | No | No |
| Igras et al. (2014) | Standard days method (family planning method) | Rwanda | No | Yes, ExpandNet |
| Jordan et al. (2016) | A first-aid device for obstetric haemorrhage | Ethiopia, India, Nigeria and Zimbabwe | No | No |
| Keyonzo et al. (2015) | Package of family planning interventions | Kenya | No | Yes, ExpandNet |
| Krumholz et al. (2015) | Evidence-based strategy of community-based primary care (including community-based nurses and volunteers) | Ghana | No | No |
| MacGregor et al. (2018) | Antiretroviral treatment adherence clubs | South Africa | Yes: ‘an extension of the geographic reach and/or scope and coverage of an intervention, as well as to the processes and capacities and resources required to achieve such expansion’ | No |
| Ojomo et al. (2015) | Household water treatment and safe storage | Tanzania and Ghana | Yes: ‘scale-up refers to the extent to which household water treatment and safe storage can be made available to the target population as well as the extent to which it is adopted by that population and used correctly and consistently’ | No |
| Omimo et al. (2018) | Community-based efforts to simultaneously address population issues, public health concerns, environmental conservation and sustainable livelihoods | Kenya and Uganda | Yes: ‘Deliberate efforts to increase the impact of successfully tested pilot, demonstration or experimental projects to benefit more people and to foster policy and programme development on a lasting basis’ | Yes, ExpandNet |
| Pappa et al. (2015) | Gender-integrated programmes | India | No | No |
| Pérez-Escamilla et al. (2018) | Integrated early childhood development programmes | Bangladesh, Chile, India and South Africa | Yes: ‘a process aimed at maximizing the reach and effectiveness of a range of actions, leading to sustained impact on outcomes’ | No |
| Schneider et al. (2010) | Antiretroviral therapy | South Africa | No | Yes, scale-up was guided by the Comprehensive Care Management and Treatment Plan |
| Somassè et al. (2013) | Community-based management of acute malnutrition approach | Burkina Faso | No | No |
| Spicer et al. (2014) | Maternal and newborn health interventions | Ethiopia, India and Nigeria | Yes: ‘an increase in the coverage of health interventions that have been tested in pilot and experimental projects in order to benefit more people’ | No |
| Spicer et al. (2016) | Maternal and newborn health interventions | Ethiopia, India and Nigeria | Yes: ‘an increase in the coverage of health interventions that have been tested in pilot and experimental projects in order to benefit more people’ | No |
| Spicer et al. (2018) | Maternal and newborn health interventions | Ethiopia, India and Nigeria | Yes: ‘the adoption and implementation of donor-funded maternal and new-born health innovations, thereby increasing their geographical reach to benefit a greater number of people beyond donor-funded implementers’ project districts or in the longer term beyond donor-funded project periods’ | No |
| Svanemyr et al. (2015) | Life Skills Based Education (including sexuality education) | Pakistan | No | No |
| Wickremasinghe et al. (2018) | Maternal and newborn health interventions | Ethiopia, India and Nigeria | Yes: ‘government adoption and implementation of health innovations, increasing geographical reach to benefit a greater number of people beyond externally funded implementers’ programme districts’ | No |
| Yamey (2012) | Health interventions in general | LMICs | Yes: ‘the ambition or process of expanding the coverage of health interventions’ | No |
| Yothasamut et al. (2010) | Pap smear and VIA services (methods for cervical cancer screening) | Thailand | No | No |
WHO, World Health Organization; VIA, Visual inspection of cervix with acetic acid.
Factors influencing scale-up
The included studies described a wide range of factors influencing a change in the structure, culture or practice, thereby facilitating or hindering scale-up. A summary of these factors (the key review findings) and the confidence attached to them based on the GRADE-CERQual assessment are presented in Table 5. The order of the factors presented in the table and in the text is based on their overall confidence. When factors had the same confidence, the order was based on the number of studies supporting them. Details of the GRADE-CERQual assessment are provided in Supplementary File S3.
Table 5.
Summary of key review findings on factors influencing scale-up of public health interventions in LMICs and their confidence
| Summary key review finding | Number of studies | Studies contributing | Overall confidence |
|---|---|---|---|
| Factors influencing a change in structure | |||
| Advocacy: Involvement of champions at local and national levels is a facilitator of the scale-up of public health interventions. Advocacy is necessary to raise attention for the problem that will be addressed by the intervention, to facilitate policy changes in favour of the intervention, to acquire financial support for scale-up, to address health systems’ gaps that could hinder scale-up and to facilitate political will. | 19 | Das et al. (2018), Araya et al. (2012), Ghiron et al. (2014), Gergen et al. (2018), Goga and Muhe (2011), Hainsworth et al. (2014), Igras et al. (2014), Jordan et al. (2016), Krumholz et al. (2015), MacGregor et al. (2018), Omimo et al. (2018), Pérez-Escamilla et al. (2018), Schneider et al. (2010), Somassè et al. (2013), Spicer et al. (2016, 2018), Svanemyr et al. (2015), Wickremasinghe et al. (2018), Yothasamut et al. (2010), Yamey (2012) | High confidence: Minor concerns regarding methodological limitations. No or very minor concerns about coherence and adequacy. Minor concerns regarding relevance. |
| Resources: Financial, human and material resources and time are factors influencing the scale-up of public health interventions. Inadequate estimating and securing of financial resources (from governments of donors) are main factors hindering scale-up, leading to limited funding available for training, supervision and human resources and limited ability to react to unforeseen costs. Implementation capacity can hinder scale-up, especially in contexts in which other factors make scale-up more difficult. | 22 | Araya et al. (2012), Bellows et al. (2016), Blauvelt et al. (2018), Fitzgerald et al. (2016), Gergen et al. (2018), Ghiron et al. (2014), Goga and Muhe (2011), Hainsworth et al. (2014), Krumholz et al. (2015), MacGregor et al. (2018), Ojomo et al. (2015), Omimo et al. (2018), Pérez-Escamilla et al. (2018), Schneider et al. (2010), Somassè et al. (2013), Spicer et al. (2016), Svanemyr et al. (2015), Wickremasinghe et al. (2018), Yamey (2012), Yothasamut et al. (2010), Spicer et al. (2014) and Spicer et al. (2018) | Moderate confidence: Minor concerns regarding methodological limitations. Minor concerns about coherence, relevance and adequacy. |
| Political will: Political will at national, regional and district government levels is a facilitator for the scale-up of public health interventions. Political will could be enhanced through alignment of the intervention with priority policies, advocacy, sharing of evidence and collaboration/involvement of the government from the start. | 12 | Bellows et al. (2016), Fitzgerald et al. (2016), Gergen et al. (2018), Hainsworth et al. (2014), Jordan et al. (2016), Krumholz et al. (2015), MacGregor et al. (2018), Schneider et al. (2010), Spicer et al. (2016), Spicer et al. (2018), Svanemyr et al. (2015) and Yamey (2012) | Moderate confidence: Minor concerns regarding methodological limitations and relevance. Moderate concerns about relevance. Data not sufficiently rich (adequacy). |
| Supply chain: Inadequate supply chains form barriers to the scale-up of public health interventions, because of the unavailability of products necessary for the intervention to be scaled | 9 | Ansbro et al. (2015), Bellows et al. (2016), Ghiron et al. (2014), Jordan et al. (2016), Krumholz et al. (2015), MacGregor et al. (2018), Ojomo et al. (2015), Schneider et al. (2010) and Spicer et al. (2016) | Moderate confidence: Minor concerns regarding methodological limitations. No or minor concerns about relevance and coherence. Data not sufficiently rich (adequacy). |
| Policies/guidelines: Alignment of public health interventions with existing policies or guidelines can facilitate scale-up. (Changes in) policies or guidelines on health financing and human resources can hinder or facilitate the scale-up of a public health intervention. | 7 | Fitzgerald et al. (2016), Igras et al. (2014), MacGregor et al. (2018), Somassè et al. (2013), Spicer et al. (2016), Spicer et al. (2018) and Wickremasinghe et al. (2018) | Moderate confidence: Minor concerns about methodological limitations. No or very minor concerns regarding coherence and relevance. Moderate concerns regarding relevance. |
| Characteristics of the intervention: In many cases, the simplicity of a public health intervention facilitates scale-up. In addition, the relevance and importance, (cost)-effectiveness, acceptability, alignment with existing systems, sustainability and adaptability of a public health intervention can facilitate its scale-up. | 22 | Araya et al. (2012), Bellows et al. (2016), Fitzgerald et al. (2016), Ghiron et al. (2014), Goga and Muhe (2011), Hainsworth et al. (2014), Igras et al. (2014), Jordan et al. (2016), Keyonzo et al. (2015), Krumholz et al. (2015), MacGregor et al. (2018), Ojomo et al. (2015), Omimo et al. (2018), Pappa et al. (2015), Pérez-Escamilla et al. (2018), Schneider et al. (2010), Somassè et al. (2013), Spicer et al. (2014), Spicer et al. (2018), Svanemyr et al. (2015), Yamey (2012) and Yothasamut et al. (2010) | Low confidence: Moderate concerns regarding methodological limitations and coherence. Minor concerns about relevance. Data not sufficiently rich (adequacy). |
| Health systems and governance: Weak health systems and governance are barriers to the scale-up of public health interventions, due to delays, corruption, limited infrastructure and resources. However, embedment of interventions within the existing health system can enhance scale-up. | 9 | Keyonzo et al. (2015), Omimo et al. (2018), Pérez-Escamilla et al. (2018), Spicer et al. (2016), Spicer et al. (2014), Svanemyr et al. (2015), Wickremasinghe et al. (2018), Yamey (2012) and Jordan et al. (2016) | Low confidence: Minor concerns regarding methodological limitations. No or very minor concerns about relevance. Serious concerns regarding coherence and adequacy: data are not rich and finding is identified by a limited number of articles. |
| Factors influencing a change in practice | |||
| Strategy: The availability of a strategic plan for scale-up, which is to be monitored and adapted over time, can facilitate the scale-up of public health interventions, as it enables strategic choices regarding training, supervision, political timing, implementation areas, targets for expansion and the allocation of resources for scale-up. | 9 | Gergen et al. (2018), Hainsworth et al. (2014), Jordan et al. (2016), Keyonzo et al. (2015), MacGregor et al. (2018), Omimo et al. (2018), Spicer et al. (2014), Spicer et al. (2018) and Yamey (2012) | High confidence: Minor concerns regarding methodological limitations and adequacy. No or very minor concerns regarding coherence and relevance. |
| Training and supervision: Insufficient or intermittent or ad hoc training and supervision forms a barrier to the scale-up of public health interventions and is related to inadequate funding and planning, high-staff turnover, lack of local expertise regarding supervision and lack of involvement of government representatives in curricula development. | 15 | Bellows et al. (2016), Ghiron et al. (2014), Goga and Muhe (2011), Hainsworth et al. (2014), Jordan et al. (2016), Keyonzo et al. (2015), Krumholz et al. (2015), MacGregor et al. (2018), Ojomo et al. (2015), Omimo et al. (2018), Schneider et al. (2010), Spicer et al. (2014), Spicer et al. (2018), Yothasamut et al. (2010) and Somassè et al. (2013) | Moderate confidence: Moderate concerns regarding methodological limitations. No or very minor concerns about coherence and adequacy. Minor concerns regarding relevance. |
| Collaborations: Different types of collaborations facilitate the scale-up of public health interventions, such as community participation, partnerships with actors that have access to specific groups and intra- and cross-sectoral collaboration at national level. A lack of these collaborations can hinder scale-up, partly through limited ownership. | 22 | Araya et al. (2012), Bellows et al. (2016), Blauvelt et al. (2018), Gergen et al. (2018), Ghiron et al. (2014), Hainsworth et al. (2014), Igras et al. (2014), Jordan et al. (2016), Keyonzo et al. (2015), MacGregor et al. (2018), Ojomo et al. (2015), Omimo et al. (2018), Pappa et al. (2015), Schneider et al. (2010), Somassè et al. (2013), Spicer et al. (2016), Spicer et al. (2014), Spicer et al. (2018), Svanemyr et al. (2015), Yamey (2012), Yothasamut et al. (2010) and Wickremasinghe et al. (2018) | Moderate confidence: Moderate concerns about methodological limitations. No or very minor concerns regarding coherence and adequacy. Minor concerns about relevance. |
| Research and Monitoring and Evaluation: The availability of research and monitoring and evaluation data facilitates the scale-up of public health interventions. Research data provide insight into the problem addressed by the intervention, which is useful for advocacy, and into the context in which scale-up takes place (before and during scale-up). Monitoring and evaluation also provides insight into context and possible implementation challenges. A lack of research can hinder scale-up, except in cases where political considerations play a major role. | 18 | Araya et al. (2012), Blauvelt et al. (2018), Fitzgerald et al. (2016), Gergen et al. (2018), Ghiron et al. (2014), Hainsworth et al. (2014), Igras et al. (2014), Jordan et al. (2016), Keyonzo et al. (2015), MacGregor et al. (2018), Schneider et al. (2010), Spicer et al. (2016), Spicer et al. (2014), Spicer et al. (2018), Wickremasinghe et al. (2018), Yamey (2012), Yothasamut et al. (2010) and Omimo et al. (2018) | Moderate confidence: Moderate concerns regarding methodological limitations. No or very minor concerns about coherence and adequacy. Minor concerns regarding relevance. |
| Politics: Politics influence the scale-up of public health interventions and can be both a barrier and a facilitator. Changes within ministries or political unrest could form a barrier to decision-making related to scale-up. However, political changes may also create a window of opportunity for scale-up, as there is a room for new directions/decisions. | 10 | Araya et al. (2012), Goga and Muhe (2011), Jordan et al. (2016), MacGregor et al. (2018), Spicer et al. (2016), Spicer et al. (2018), Yamey (2012), Yothasamut et al. (2010), Pérez-Escamilla et al. (2018) and Wickremasinghe et al. (2018) | Moderate confidence: Minor concerns regarding methodological limitations and coherence. Moderate concerns regarding adequacy and no or very minor concerns regarding relevance. |
| Leadership: Political and programme leadership can influence the scale-up of public health interventions. Political leadership depends on political will or buy-in and is, therefore, not always present, which hinders scale-up. Programme leadership, when present at different levels, facilitates scale-up. | 4 | Araya et al. (2012), Bellows et al. (2016), MacGregor et al. (2018) and Yamey (2012) | Moderate confidence: Minor concerns regarding methodological limitations. No or very minor concerns about relevance. Identified by a very limited number of articles (adequacy). |
| Factors influencing a change in culture | |||
| Sociocultural environment: The sociocultural environment can hinder the scale-up of public health interventions, as social and cultural norms, and preferences may influence the acceptance and support of the intervention when this intervention does not take the sociocultural environment enough into account. | 7 | Macgregor et al. (2018), Ojomo et al. (2015), Spicer et al. (2016), Spicer et al. (2014), Spicer et al. (2018), Svanemyr et al. (2015) and Yamey (2012) | Moderate confidence: Minor concerns regarding methodological limitations and coherence. No or very minor concerns about relevance. Data are not sufficiently rich, and finding is identified by a limited number of articles (adequacy). |
| Need/demand for intervention: When stakeholders at different levels feel that there is a need for the intervention based on available local data, this will facilitate the scale-up of public health intervention. When this need if not felt by (one of) the stakeholders, scale-up is constrained. | 7 | Araya et al. (2012), Ghiron et al. (2014), Jordan et al. (2016), Ojomo et al. (2015), Pérez-Escamilla et al. (2018), Somassè et al. (2013) and Spicer et al. (2018) | Low confidence: Minor concerns regarding methodological limitations. Moderate concerns regarding coherence and minor concerns about relevance. Data are not sufficiently rich, and finding is identified by a limited number of articles (adequacy). |
Factors influencing a change in structure
Many studies identified factors that have a substantial influence on a change in the physical and/or economic infrastructure and institutions, thereby influencing scale-up.
Advocacy
In 19 studies, advocacy was identified as an important factor influencing scale-up. First, advocacy can be used to prioritize the problem that is addressed by the intervention. For example, Araya et al. (2012) described that depression became a health priority for the Ministry of Health through lobbying activities using evidence from available studies. Second, advocacy can be used to convince decision-makers to change policies and/or guidelines, or third, to lobby for financial support for scale-up (Somassè et al., 2013; Spicer et al., 2014). Fourth, Igras et al. (2014) described advocacy being used to facilitate integration of a family planning method in an already existing performance-based financing programme. Fifth, advocacy can be useful to address health systems’ gaps that might influence the scale-up of the intervention, such as the supply chain and availability of human resources (Hainsworth et al., 2014). Sixth, advocacy activities were found to be important to ensure that interventions will be included in budgets at district, regional or national level (Goga and Muhe, 2011; Hainsworth et al., 2014). Having insights into the costs associated with the implementation and scale-up of an intervention is crucial for these advocacy activities.
Some studies highlighted the importance of planning advocacy activities, which includes methods, timing, the target(s) and plans for communicating evidence (Ghiron et al., 2014; Spicer et al., 2014; Omimo et al., 2018). In the study of Spicer et al. (2014), respondents identified several methods for advocacy namely: ‘panel discussions with officials; presenting at public meetings or conferences; promoting their work at development partners' fora; inviting government to project review meetings; presenting evidence in reports and journals; producing brochures and newsletters; and project websites and social media’. The involvement of both local and national level champions in advocacy activities was discussed as a facilitator for scale-up in several articles. Advocacy can also deliver new champions, which further facilitates scale-up (Omimo et al., 2018). For example, Krumholz et al. (2015) described that the scale-up will lose direction if local/grass-root champions are not involved. Spicer et al. (2014, 2018) described that champions from the government are crucial because policy changes will be easier when they happen from within instead of outside the government. Personal connections with government decision-makers were found to be as important, if not more, than formally engaging government during the scale-up of ‘maternal and new-born health interventions’ in Ethiopia, India and Nigeria (Spicer et al., 2018). Ghiron et al. (2014) described that during the scale-up of ‘Community based efforts to simultaneously address population issues, public health concerns, environmental conservation and sustainable livelihoods’ in Uganda and Kenya, it was good to formally identify champions who can advocate for scale-up and to train them in advocacy.
Resources
Twenty-two studies identified the availability of ‘resources’ as an important factor influencing scale-up. Most of these articles described that inadequate financial resources or funding was perceived as a challenge to the scale-up of an intervention. There were no sufficient financial resources available for training, supervision, transportation and staffing, and this limited the possibility to scale-up. Several reasons for insufficient financial resources emerged. First, during implementation of the scale-up of the intervention, unforeseen costs arose such as training costs for supervisors (Hainsworth et al., 2014). Second, there were often no estimates of costs available for the implementation and scale-up of a certain intervention, which made it difficult to develop suitable budget allocations (Araya et al., 2012). Hainsworth et al. (2014) explained that for the scale-up of ‘adolescent contraceptive services’ in five countries, only Mozambique had cost estimates available. These cost estimates, in combination with estimates of needed donor contributions, were provided to the districts, and this transparency led to the inclusion of adolescent contraceptive services in district budgets. Third, governments’ dependence on vertical, relatively short-term donor funding was mentioned as a contributor to limited financial resources for scale-up in three studies (Gergen et al., 2018; Omimo et al., 2018; Wickremasinghe et al., 2018). Some studies reported that additional financial resources for scale-up were not made available at all (Somassè et al., 2013; Gergen et al., 2018). Spicer et al. (2014) described, therefore, the importance of having a clear budget target and plan of activities related to scale-up to ensure that resources will be made available. This is closely related to having a scale-up strategy. Building the technical and management capacity of local government could facilitate the inclusion of interventions in budgets and work plans, which can improve sustainability of an intervention once external funding stops (Hainsworth et al., 2014).
Not only financial resources but also human resources, material resources (including infrastructure) and time were described as factors influencing scale-up. Besides a general lack of human resources, which constrained scale-up in many studies, four studies identified the capacity of programme implementers as a factor influencing scale-up. One of these studies referred to the management capacity of implementers, which is crucial in contexts where implementation is challenging due to the lack of political will and limited financial resources (Schneider et al., 2010). Three studies referred to implementation capacity (Spicer et al., 2014; Svanemyr et al., 2015; Gergen et al., 2018). As the capacity of programme implementers to scale up an intervention varies, capacity building activities targeting them may enable scale-up (Spicer et al., 2014, 2018; Macgregor et al., 2018; Omimo et al., 2018). However, in resource-constrained settings, the introduction and scale-up of new interventions might be perceived as extra workload by implementers (Spicer et al., 2016; Wickremasinghe et al., 2018). Capacity building is further discussed in the Training and supervision section.
Political will
Twelve studies described political will, or used other terms such as political acceptance, political buy-in and political support, as being a factor influencing the scale-up of public health interventions. The central government is generally the ‘owner’ of an intervention at scale, and therefore, their political will is very important—and this is often depending on the alignment of the intervention with priority policies (Spicer et al., 2014, 2016; 2018). For example, in South Africa, the scale-up of antiretroviral treatment adherence clubs was facilitated because of political will. This political will was based on the wish to spending on HIV programmes and the belief that the intervention would reduce congestion in clinics, rather than evidence of the intervention’s effectiveness (Macgregor et al., 2018). After a comparison of the scale-up of a ‘first-aid device for obstetric haemorrhage’ in four countries, Jordan et al. (2016) concluded that in India and Zimbabwe, scale-up was most challenging because creating government support for the scale-up of this intervention was difficult and took time. Several activities facilitating political will were described. A key activity was strategic advocacy through policy champions (Hainsworth et al., 2014; Spicer et al., 2014). Communication of evidence and involvement of the government from the beginning were also activities enabling political will (Spicer et al., 2014). Hainsworth et al. (2014) described that during the scale-up of ‘adolescent contraceptive services’, the involvement of adolescents and youth helped to keep the government accountable, especially during changes in leadership and times of reduced political support.
Political will at district and provincial/regional levels was also referred to as highly important (Schneider et al., 2010; Hainsworth et al., 2014; Gergen et al., 2018; Macgregor et al., 2018). For example, Schneider et al. (2010) compared scale-up outcomes: a comparison of the scale-up of ‘an antiretroviral programme’ in three different provinces in South Africa showed that, in the provinces where there was strong political support, the results of the scale-up were better. MacGregor et al. (2018) reported that despite the political will at provincial level, national scale-up of a ‘performance-based financing programme on HIV and maternal-child health services’ failed because of the lack of political will at national level.
Supply chain
Nine studies identified the supply chain—the process of bringing the product to the consumer—as a factor influencing the scale-up of public health interventions. Four articles reported that commodities, products and equipment were not or limited available for the interventions to be scaled. Schneider et al. (2010) described that during the scale-up of ‘antiretroviral therapy’ in South Africa, the provision of antiretroviral therapy supplies was interrupted because of the withdrawal of certain drugs from international markets. This interruption had impact on the legitimacy of the intervention experienced by the managers, providers and patients (Schneider et al., 2010). Oftentimes, it is difficult to change the inadequate (government) systems responsible for supply chain problems. Therefore, Ghiron et al. (2014) described that when there were challenges in the contraceptive supply chain, ways of contraceptive provision were developed outside the routine system. At the same time, advocacy activities took place at the Ministry of Health level to improve the commodity supply and distributions’ mechanisms.
Policies and guidelines
Seven studies described the importance of alignment of the intervention with specific policies/guidelines to facilitate scale-up. When to be scaled interventions align with governments’ health priorities, policy frameworks and targets, this can result in increased government ownership, political will and ability to implement (Spicer et al., 2016; Wickremasinghe et al., 2018; Macgregor et al., 2018). For example, Spicer et al. (2016) reported that the high priority given to maternal and newborn health in Uttar Pradesh, India, and Ethiopia was enshrined in policy frameworks, which study participants described as enabling the scale-up of interventions in this field. Changes in policies, such as health finance policies, can also influence scale-up. For example, during the scale-up of the ‘Standard Day Methods’ (family planning method), the Rwandan government initiated the implementation of a performance-based financing system, where incentives were provided based on the quantity and quality of specific services delivered. In the beginning of the scale-up, the standard day method was a part of these services, but later, it was excluded from the performance-based financing guidelines, resulting in providers receiving fewer incentives for providing the standard day method. This negatively influenced the sustainability of the scale-up (Igras et al., 2014). Fitzgerald et al. (2016) mentioned that, for the scale-up of ‘Early Infant Male Circumcision’, a policy environment, i.e. in favour of task shifting, would be important as this might help to address personnel shortages by nurses being allowed to perform minor surgical procedures.
Characteristics of the intervention
In 22 studies, specific characteristics of an intervention were identified that influence its scale-up. Most of these characteristics were only applicable for that specific type of intervention, such as the complex consent process for Early Infant Male Circumcision (Fitzgerald et al., 2016) or the technological design of a household water treatment and safe storage product (Ojomo et al., 2015). However, more general characteristics were also identified to influence the scalability of an intervention. For example, in Spicer et al. (2014), several characteristics of scalable health innovations were highlighted: relevance and importance, effectiveness, observable benefits, acceptability to health workers and communities, being simple and having low costs, alignment with existing systems, adaptability (to different contexts) and sustainability. Spicer et al. (2014) described that, to impress donors, an abundance of financial and other resources is invested in (complex) pilot interventions. However, government decision-makers’ interest is more in simple and low-cost interventions for scale-up, which could lead to compromises in quality. If an intervention has been successful during the pilot, it needs to be simplified as the same time and effort attention cannot be given during the scale-up process (Igras et al., 2014; Keyonzo et al., 2015; Jordan et al., 2016). Omimo et al. (2018) described that the package of population, health and environment interventions was too complex. This made it difficult to identify one sector and funder to lead the scale-up.
Health systems and governance
In nine studies, factors related to health systems and governance were identified as influencing scale-up. Five articles described weak health systems as a barrier for scale-up (Yamey, 2012; Spicer et al., 2014, 2016; Jordan et al., 2016; Pérez-Escamilla et al., 2018). Spicer et al. (2014) discussed that it remains a dilemma whether you should work within or outside existing health systems when scaling up. Respondents of the research of Spicer et al. (2014, 2016) stated that working within broken systems makes scale-up difficult to succeed because of delays, limited progress, corruption, bureaucracy, poor infrastructure and information systems, weak human resources or limited confidence of end-users. On the other hand, embedment of interventions within the existing health system was found to have enhanced their scale-up in two studies (Keyonzo et al., 2015; Omimo et al., 2018). Study participants of Wickremasinghe et al. (2018) indicated that if the intervention is not embedded in the health system, prospects of scale-up are low because of limited government ownership.
Yamey (2012) described that, especially at local level, governance, leadership and management capacity were weak. Svanemyr et al. (2015) described that when scaling up ‘Life Skills Based Education’ in Pakistan, institutionalization of the intervention at local level was needed because of devolution. However, the limited capacity and competencies of the local government hindered scale-up.
Factors influencing a change in practice
The included studies identified several factors having a substantial influence on a change in practice (way of doing), thereby influencing scale-up.
Strategy
Nine articles identified that an important factor influencing scale-up is the use of a strategic plan. Jordan et al. (2016) described the importance of a strategic plan for the scale-up of ‘a first-aid device for obstetric haemorrhage’, based on the facilitators identified during interviews with key informants. The scale-up plan can be used to make strategic choices regarding financial, human and technical resources, including training and supervision, and timing of different steps in the scale-up (Spicer et al., 2014; Jordan et al., 2016). Spicer et al. (2016, 2018) reported the importance of including scale-up when designing a pilot programme instead of starting to plan for scale-up during implementation, as this is often when donors pull out of the programme. One study reported that scale-up strategies need to be monitored and continuously adjusted over time (Omimo et al., 2018). Spicer et al. (2018) stressed the importance of a gradual (not abrupt) phasing-out of externally funded implementers to facilitate scale-up.
Three scale-ups that used the ExpandNet framework to inform the scale-up process (Table 4; these three scale-ups are covered in four studies) described that a scale-up strategy was developed based on the framework (Ghiron et al., 2014; Igras et al., 2014; Keyonzo et al., 2015; Omimo et al., 2018). Others also reported to have had a scale-up plan. For example, Hainsworth et al. (2014) described that the scale-up of ‘adolescent contraceptive services’ was systematically executed: there were clearly planned annual targets for expansion, selection criteria for implementation sites and strategic choices; this facilitated scale-up.
Training and supervision
Fifteen studies identified the importance of training and supervision to develop the capacity of the actors to implement the scale-up of a public health intervention, which is especially important for the sustainability of the scale-up. Several causes for ineffective training were identified: inadequate funding (Goga and Muhe, 2011; Somassè et al., 2013) and high-staff turnover, causing limited sustainability of the capacity developed (Hainsworth et al., 2014; Bellows et al., 2016). This high-staff turnover is often related to: ‘illness, position transfers, retirement, death or termination of positions due to lack of compensation’ (Bellows et al., 2016). Ansbro et al. (2015) compared the experiences of a pilot study of ‘point-of-care rapid syphilis tests (RST)’ with a national RST. During the pilot phase, training was executed at central level by the implementing organization and supervision was executed monthly by the implementing organization. During scale-up, training was executed at district level by the Ministry of Health and the implementing organization and supervision was executed only quarterly during visits made by the Ministry of Health and the implementing organization. These changes in training and supervision were experienced as negative by the respondents, and this caused a weak understanding of the different steps involved in RST, which had a negative influence on the end-user experience and, therefore, the feasibility of the scale-up. Furthermore, Ansbro et al. (2015) described that challenges regarding supervision may have been related to ineffective planning and communication, lack of dedicated budget, logistics and local expertise regarding supervision.
Other studies also described supervision as being less intensive when scaling up an intervention (Somassè et al., 2013; Krumholz et al., 2015; Macgregor et al., 2018). Krumholz et al. (2015) described that during a community-based health and family planning project, supervision structures were more extensive than during the national scale-up, where there was a reliance on the existing (weaker) country supervision system.
Several stakeholders (government, implementers and civil society) identified that for scaling up maternal and newborn interventions, the involvement of government representatives in the development of training curricula and trainings is important, as this may contribute to the institutionalization of the intervention as well to the capacity building of government representatives (Spicer et al., 2014, 2018). Indeed, Keyonzo et al. (2015) and Omimo et al. (2018) described that the involvement of trainers from the government facilitated scale-up. In addition, follow-up training was identified as a factor that might facilitate scale-up as this may address the challenges related to staff turnover (Hainsworth et al., 2014; Ojomo et al., 2015).
Collaborations
Twenty-two articles identified that collaborations between stakeholders—during all stages from pilot to scale-up—are important for scale-up. Several ways of collaborating at and between different levels were discussed. For example, Ojomo et al. (2015) described that participants identified that collaborations between different organizations were crucial for the scale-up of household water treatment and safe storage practices. Several forms of collaborations were discussed in the included studies, such as community participation, cross-sectoral collaborations, integration in other projects and partnerships with, among others, the government to increase ownership.
First, regarding community participation, participants described that the involvement of community chiefs is important as they are well respected and will facilitate behaviour change. Collaborations with community members will contribute to sustain the desired behaviour change when implementing partners leave (Ojomo et al., 2015). Spicer et al. (2014) identified the importance of understanding the attitudes, priorities and motivations of communities, which can inform the intervention to be scaled up instead of imposing an intervention on people without asking them what they want and need. Participants of the study of Yamey (2012) discussed that scale-up often fails because there is not enough engagement of key community stakeholders, resulting in the targeted community feeling not ready for the intervention. Yothasamut et al. (2010) described that the top-down approach of the cervical cancer screening scale-up did not work: collaboration and involvement of key stakeholders in decision-making did not take place. As a result, there was a low awareness of the actual needs of the target population.
Second, many articles described partnerships with different types of actors. This was seen as important for scale-up because different actors bring in different expertise. For example, respondents of the study of Ojomo et al. (2015) described that a partnership with local charity organizations contributed to positive scale-up outcomes as they had greater access to rural populations and that partnerships with private sector organizations helped as they are able to make investments.
When discussing partnerships, many studies highlighted the importance of partnership at the national government level. Fitzgerald et al. (2016) stated that to create national ownership and avoid donor-driven programmes, collaborations between different stakeholders, such as actors from the sexual and reproductive health unit at national level, were important. Araya et al. (2012) described that, for the scale-up of a ‘Depression Detection and Treatment Programme’, alliances were formed between different divisions of the Ministry of Health: the mental health unit and the primary care division. This strategic alliance was useful as the mental health unit had the technical capacity but the primary care division had the resources available.
Third, closely related to partnerships, the importance of cross-sectoral collaborations was stressed in several studies. Bellows et al. (2016) described that the complexity of a family planning intervention made it important to work together with stakeholders working in nutrition, gender and education. This facilitated the development of a good policy environment for scale-up. Araya et al. (2012) stated that cross-sectoral collaboration with universities was important during the scale-up of ‘the depression detection and treatment programme’ as the academics were able to provide relevant information for the introduction and scale-up of the national programme. Blauvelt et al. (2018) described that in the scale-up of a ‘free health and nutrition hotline’ in Malawi, multi-sectoral collaboration contributed to success among others because of collective resourcing of the intervention.
Fourth, integration of the intervention in other health-related programmes was described as a success factor, as it helps in optimizing the resources available, which increases sustainability (Ojomo et al., 2015).
One study reported that competition between different development agencies and different implementers can pose a challenge to collaboration (Spicer et al., 2014, 2016; Wickremasinghe et al., 2018). These organizations often have different interests and priorities and might be competing for funding. Some governments did co-ordinate and facilitate collaborations, e.g. through technical working groups in Ethiopia, but other governments did not, because sometimes they were more donor dependent and, therefore, felt that they could not say no to any funding.
Research and monitoring and evaluation
Eighteen studies described that research and/or monitoring and evaluation (data) are important factors influencing scale-up. Several types of research with different objectives were described. Research can be used during lobbying and advocacy activities, as research can assist to provide insights into the magnitude of the problem that will be addressed by the intervention. For example, Araya et al. (2012) discussed that national disease burden studies were crucial for informing the scale-up of the ‘National Depression Detection and Treatment Programme’ in Chile, as they showed a high disease burden caused by depression. Specific research evidence about the (pilot) intervention is important to show the effectiveness of the intervention. Yothasamut et al. (2010) described that providing evidence about the cost-effectiveness of ‘cervical cancer screening and Human Papilloma Virus vaccination’ was an important facilitator for the scale-up of this intervention in Thailand. Research on effectiveness needs to be based on local data, and providing insights into the costs associated with the intervention and scale-up is crucial (Araya et al., 2012; Jordan et al., 2016). It is important that evidence is simplified and actively brought to policymakers, as oftentimes policymakers do not have sufficient time and/or knowledge to understand complex data (Araya et al., 2012). In addition, research is crucial because it can be used to assess the environment/context in which scale-up is taking place (Igras et al., 2014; Spicer et al., 2014, 2018). Hainsworth et al. (2014) described that examining the strengths and weaknesses of the health system is important. Spicer et al. (2014) stated that exploring the political climate, policy priorities, governments systems, institutions and procedures is critical. This analysis can inform the scale-up strategy and might help to align country priorities and systems with the innovations to be scaled.
Monitoring and evaluation can facilitate scale-up, as data can be used to understand what is working and what is working less well in certain contexts, and this enables managers to make changes in the scale-up process and address implementation issues to improve outcomes. Because of the complexity of scale-up, strategic use of data is important to make corrections on time (Hainsworth et al., 2014; Jordan et al., 2016). Igras et al. (2014) described that regularly scanning the environment and identifying contextual changes are important throughout the scale-up. This will help to systematically address political issues in scale-up, such as changes in leadership. During the scale-up of a family planning package in Kenya, the government’s health information system was used for monitoring and evaluation, which enhance ownership (Keyonzo et al., 2015).
Several challenges were identified regarding the use of research and monitoring and evaluation during scale-up. For example, the research capacity in LMICs is generally restricted. Furthermore, there is generally a low interest in implementation science and, therefore, robust research methods and innovate research designs are limited (Yamey, 2012). Lastly, the information acquired from research is not always used, as often decisions are not based on evidence but on politics or ‘emotional buy in’ based on experiences with or assumptions about the outcomes of the intervention (Spicer et al., 2014, 2016; 2018; Macgregor et al., 2018).
Politics
Politics was identified as a factor influencing scale-up by 10 studies. The uncertain political climate of Zimbabwe was described as a barrier to the scale-up of ‘a first-aid device for obstetric haemorrhage’ (Jordan et al., 2016). Goga and Muhe (2011) described that frequent changes within ministries were a barrier for scale-up as it hindered the continuation of work. As stated earlier, decisions on scale-up are often based on politics instead of information about effectiveness and costs. Depending on the situation, this could hinder or facilitate scale-up.
Political changes could also facilitate scale-up. For example, Araya et al. (2012), describing the scale-up of a ‘Depression Detection and Treatment Programme’ in Chile, reported that, during the military regime, mental health problems were generally ignored. When democracy returned, mental health became one of the key priorities and this facilitated scale-up. Although Yothasamut et al. (2010) described that political instability was a challenge for the scale-up of ‘Human Papilloma Virus vaccination’ in Thailand, the political crisis also resulted in national health authorities acknowledging the problems related to cervical cancers. For the Cabinet members, it was important to show their successful policies to the population to protect their government’s position. Araya et al. (2012) described that it is better to start scale-up at the beginning of electoral cycles than at the end. This was confirmed by Spicer et al. (2016), indicating that new officials were often unwilling to accept their predecessors’ decisions to scale-up innovations.
Leadership
Strong leadership was identified as a facilitator to scale-up in four studies. The following two types of leadership were described: political leadership and programme leadership. Bellows et al. (2016) described that leadership at national level will occur if there is political will or political buy-in. Yamey (2012) discussed that creating political leadership is challenging because leadership in the Ministry of Health is often politicized. Regarding programme leadership (which is more related to the implementation of scale-up), Araya et al. (2012) found that strong and effective leadership is crucial, but it should not be borne by the capacity of one leader but by an informal team or several leaders acting at different levels who have a shared vison. Several characteristics for these leaders were identified: ‘politically friendly and trustworthy; good at forming alliances; able to understand and apply technical information; and good communicators who could adapt their terminology to fit different situations’ (Araya et al., 2012).
Factors related to or influencing a change in culture
Some studies identified factors that were related to or influence a change in culture or the way of thinking, thereby influencing scale-up.
The sociocultural environment
The sociocultural environment was described as a factor influencing scale-up. In general, Yamey (2012) described that one of the key barriers to scale-up is that interventions that were successful during pilot testing are not transferable or scalable in other settings. Different cultural environments will have different preferences, and this will influence their acceptance of an intervention (Ojomo et al., 2015; Spicer et al., 2016, 2018). Svanemyr et al. (2015) described that for the scale-up of ‘Life Skills Based Education’ (including sexuality education), the conservative environment of some Pakistani provinces made scale-up challenging, as the community support of the programme was limited. Spicer et al. (2014) also described that, during the scale-up of ‘maternal and new-born health interventions’, it was difficult to address sociocultural norms related to gender and castes in India.
The context of the pilot intervention is different from the context of the areas where the scale-up will take place (Yamey, 2012). Therefore, Schneider et al. (2010) and Spicer et al. (2016) stated that you have to find a balance between core characteristics of the intervention to be scaled and some flexibility to adapt the intervention to the different local contexts. Pappa et al. (2015) stated that it is important to ensure that the intervention is adaptable when scaling up ‘gender-integrated programs’ as the gender-related barriers vary in different contexts.
Perceived need for the intervention to be scaled
Seven studies identified the perceived need or demand for the specific intervention—from the intended beneficiaries as well as the Ministry of Health—as a factor that may influence scale-up. When the intervention addresses the needs of stakeholders, the willingness to scale it up can increase, even before evidence on effectiveness of the intervention is available (Ghiron et al., 2014). Jordan et al. (2016) reported that a recognized unmet need of the adopting community was a facilitator to the scale-up of ‘a first-aid device for obstetric haemorrhage’; although the device does not address the social, economic and gender barriers, it addresses the community need to reduce maternal mortality. Somassè et al. (2013) described a challenge during the scale-up of ‘community-based management of acute malnutrition’ that although the community was supporting the intervention, the Ministry of Health did not feel the need for this intervention as the management of the intervention was done by a team external to the health system. Araya et al. (2012) discussed that the scale-up of treatment of depression was accepted by the Ministry of Health when a study, using local data, showed the high prevalence and burden associated with depressions.
Discussion
The aim of this review was to identify how different factors influence the scale-up of public health interventions in LMICs. The studies assessed focused on the scale-up of different types of public health interventions taking place in different countries. Following a multi-level perspective on transition, changes in structure, practice and culture are necessary to ensure the scale-up of an intervention, in other words, to move from an intervention at niche level to a mainstream intervention at regime level. The factors were, therefore, categorized according to identified (failures to establish) changes in structure, practice and culture. In this section, we first provide a short overview of the findings. This is followed by three important learning points drawn from the findings of the review. Finally, the methodological limitations are discussed.
Overview of findings
One of the most prominent factors influencing a change in structure was the availability of financial, human and material resources. Inadequate supply chains were often barriers to scale-up. Design characteristics, such as the simplicity of the intervention, may influence scale-up, as well as advocacy activities, preferably with the involvement of champions at local and national levels. These advocacy initiatives can trigger a change in structure needed for scale-up, e.g. in the physical or economic infrastructure. Weak health systems and governance may form barriers to scale-up; however, the level of confidence regarding this finding was low. Changes in the policy environment, which is also related to structure, may hinder or facilitate scale-up.
The most outstanding factors influencing practice were the availability of a strategic plan for scale-up and the way training and supervision was conducted. While a scale-up strategy facilitates scale-up through planned and joint actions of all stakeholders involved, insufficient or non-continuous training forms a barrier to scale-up as found in many studies. Furthermore, collaborations such as community participation and partnerships facilitate scale-up, as well as programme and political ownership and leadership. The availability of research and monitoring and evaluation data is valuable during advocacy activities, and data can be used to adapt the intervention or scale-up strategy to be responsive towards contextual changes (in other words, changes in the landscape).
Factors influencing change in culture were less prominently described in the literature. While some studies articulated the acceptability of the intervention in a given sociocultural environment (which is related to the characteristics of the intervention), more emphasis was placed on the importance of stakeholders feeling a need for a specific intervention to facilitate its scale-up.
When all factors will be taken into account during scale-up, changes in structure, practice and culture will most likely take place, which will contribute to higher probability of sustainability of the scale-up.
The importance of vertical scale-up
Scale-up can be defined in multiple ways. According to the multi-level perspective on transition, scale-up can be defined as ‘embedding a (transition) intervention in new dominant ways of thinking (culture), doing (practice) and organizing (structure)’ (Van den Bosch and Rotmans, 2008). From this perspective, there is a strong assumption that changes in the system and, thus, institutionalization are necessary for the sustainability of the scale-up, which is also highlighted in several other publications and guidance documents (Simmons et al., 2007; WHO/ExpandNet, 2009, 2010, 2011). When scale-up is only focusing on the expansion of an intervention (horizontal), sustainability is compromised. Sustainability is also compromised when interventions are not aligned with existing policies and systems, and when principle of aid effectiveness are not respected (Spicer et al., 2018; Wickremasinghe et al., 2018). For Universal Health Coverage, sustainable scale-up of public health interventions is crucial and, therefore, a focus on vertical scale-up is highly important: the multi-level perspective can be used to guide this thinking.
Holistic approach to scale-up
The multi-level perspective on transition describes that structure, practice and culture are not mutually exclusive and influence each other: how people behave is influenced by culture and the existing structures in place and perceptions (part of culture) are influenced by the practice and structure (Essink, 2012). Creating evidence on how interlinkages may trigger change is important in understanding scale-up. This review identified many interlinkages that were important to scale-up. For example, advocacy can influence a change in the way of doing (practice), resulting in different priority setting, which could ultimately contribute to a policy change and, therefore, a change in structure. Available evidence collected through research, monitoring and evaluation is often crucial for effective advocacy and (local) research data can assist in creating a shared perception among different stakeholders on the need for a specific intervention to be scaled. Due to challenges related to human resources, specifically high-staff turnover, training and supervision needs to be frequent and continuous, for which financial resources are necessary. The interlinkages of the different factors influencing scale-up highlight the importance of a holistic approach to scale-up where all different factors influencing scale-up are taken into account and all relevant stakeholders are meaningfully involved. This is in line with the views on the scale-up of WHO/ExpandNet, which describes that expansion and institutionalization take place in a complex network of interactions. Therefore, systems thinking is seen as one of the core principles guiding scale-up (Simmons et al., 2007; Bradley et al., 2012; Paina and Peters, 2012; Barker et al., 2015).
The development of a scale-up strategy
For the scale-up of public health interventions in LMICs, policymakers and programme managers can take the various factors influencing scale-up as identified in this review into account. The development of a scale-up strategy before scaling up is a first step where ways of addressing these factors, throughout the process of scale-up, could be described. In this scale-up strategy, it is important to ensure a focus on how to manage the scale-up process through facilitating changes in structure, practice and culture, within the existing landscape. WHO/ExpandNet (2010) developed a practical guidance document that describes nine steps for developing a scale-up strategy. They focus on strategic choices regarding the innovation itself, the capacity of the user organization, the environment and the vertical and horizontal scale-up. Continuous monitoring and evaluation of the scale-up process and its outcomes is important, as this will provide insights in how to continuously change and strengthen the scale-up strategy (WHO/ExpandNet, 2009; 2010).
In this literature review, most of the identified factors influencing scale-up did so through changes in structure and practice, fewer factors that influenced scale-up through changes in culture were identified. Factors that influence a change in culture seem to be related to the type and complexity of the intervention that is being scaled. For example, the scale-up of an intervention on sexual education could be challenging in a certain culture because of the sensitivity of the intervention. In this case, it can be argued that scale-up can be facilitated if people’s perceptions on this sensitivity are influenced, e.g. through raising community awareness or behaviour change interventions. Acceptance of an intervention might also depend on the institutional culture of the service delivery system (Simmons et al., 2007). The landscape is an important component of the multi-level perspective on transition: it influences the transition from niche to regime levels, and the required changes in structure, practice and culture. Most of the included articles made general references to the landscape but did not provide deeper analyses on how it set the boundaries for scale-up. However, specific approaches to working within the landscape—including the cultural context, security, political ideologies and governance systems, which cannot be controlled—will need to be considered when scaling up public health interventions (Spicer et al., 2016, 2018). This is also why Aichatou et al. (2016) highlighted the importance of a proof of implementation besides a proof of concept before scaling up. While our review did not focus on landscape factors, it is important to continuously assess the landscape, to adapt the scale-up strategy when needed.
Setting the delimiter at year 2010 might have resulted in the exclusion of more in-depth information of factors influencing scale-up from earlier studies. One of the challenges of this literature review was to identify whether studies were focusing on scale-up or on a pilot intervention. Given the great interest in scale-up (Mangham and Hanson, 2010), the term scale-up is often used in titles, abstracts or full articles; however, these articles are often not focusing on scale-up. It is possible that studies were excluded because of the diffuse distinction between a pilot intervention to be scaled (later) and an intervention that is or has been scaled up, especially as there is no common definition of scale-up. Furthermore, because of the interlinkages between the factors influencing scale-up, their categorization was not a straightforward exercise. The categorization exercise was, therefore, done by two researchers where discussions took place until consensus was reached.
The selection of the studies and data analysis were performed by a team of three researchers, decreasing the chances of (interpretation) bias through joint discussion. The GRADE-CERQual approach was used to assess the confidence of each key review finding. The focus of the literature review was clearly delineated, and therefore, there were little concerns regarding relevance. The methodological quality of the included studies, and therefore, the methodological limitations related to the review findings, varied. For some studies, there were concerns regarding the depth of data, which influenced the adequacy as well as the coherence of the review findings. Having used the GRADE-CERQual approach, we can conclude with moderate confidence that the majority of the key review findings is reasonable representations of barriers and facilitators of the scale-up of public health interventions in LMICs (Lewin et al., 2018a). While our review findings resonate with factors influencing scale-up as presented in other sources (WHO/ExpandNet, 2009; 2011; Paina and Peters, 2012; Milat et al., 2015), the low and moderate confidence of some of the review findings indicate that there is a room for improved reporting on scale-up processes and implementation research.
Conclusion
To enhance global health, scale-up of successful tested public health interventions in LMICs is crucial. Scale-up is a complex process and influenced by multiple factors. Applying the multi-level perspective on transition to scale-up provides a useful framework with a specific focus on how interventions could be embedded in a certain landscape, through changes in the structure, practice and culture. This literature review identified several factors that have the potential to make a change in structure, practice and culture. These factors should be taken into account when scaling up public health interventions in LMICs. Different factors strongly influence each other, and most of them are related to one crucial step: the development of a scale-up strategy before scaling up after which continuous revision of the strategy needs to take place based on the actual scale-up process and outcomes.
Supplementary Material
Acknowledgements
The systematic literature review presented in this article is performed as part of the Perform2Scale project. Perform2Scale is a 5-year international research consortium aiming to develop and evaluate a sustainable approach to scaling up a district-level management strengthening intervention in different and changing contexts. The project is part of the European Union’s Horizon 2020 research and innovation programme. This work was supported by the European Union’s Horizon 2020 research and innovation programme (grant number 733360).
Conflict of interest statement. None declared.
Ethical approval. No ethical approval was required for this study.
Footnotes
Ghiron et al. (2014) and Omimo et al. (2018) report about the scale-up of an integrated population, health and environment project in East Africa. The scale-up of this project was guided by the ExpandNet framework. Spicer et al. (2014, 2016; 2018) and Wickremasinghe et al. (2018) report about the scale-up of maternal and newborn health interventions in Ethiopia, India and Nigeria. Spicer et al. (2014, 2016) and Wickremasinghe et al. (2018) use the same data set in their studies.
References
- Aichatou B, Seck C, Anne TSB, Deguenovo GC, Ntabona A, Simmons R.. 2016. Strengthening government leadership in family planning programming in Senegal: from proof of concept to proof of implementation in 2 districts. Global Health: Science and Practice 4: 568–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansbro E, Gill M, Rynolds J. et al. 2015. Introduction of syphilis point-of-care tests, from pilot study to national programme implementation in Zambia: a qualitative study of healthcare workers’ perspectives on testing, training and quality assurance. PLoS One 10: e0127728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araya R, Alvarado R, Sepúlveda R, Rojas G.. 2012. Lessons from scaling up a depression treatment program in primary care in Chile. Revista Panamericana de Salud Pública 32: 234–40. [DOI] [PubMed] [Google Scholar]
- Barker PM, Reid A, Schall MW.. 2015. A framework for scaling up health interventions: lessons from large-scale improvement initiatives in Africa. Implementation Science 11: 12.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellows B, Nambao M, Jaramillo L, Fanaiayan R, Dennie M, Hardee K.. 2016. Scaling up Family Planning in Zambia. Part 1: Assessment and Feasibility of Maintaining an Innovative Program. Washington, DC: Population Council, The Evidence Project. [Google Scholar]
- Blauvelt C, West M, Maxim L. et al. 2018. Scaling up a health and nutrition hotline in Malawi: the benefits of multisectoral collaboration. BMJ 363: k4590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley EH, Curry LA, Taylor LA. et al. 2012. A model for scale up of family health innovations in low-income and middle-income settings: a mixed methods study. BMJ Open 2: e000987.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASP. 2017. CASP Checklist: 10 Questions to Help You Make Sense of a Qualitative Research. Oxford: https://casp-uk.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf, accessed 10 October 2017. [Google Scholar]
- Das JK, Akseer N, Mirzazada S. et al. 2018. Scaling up primary health services for improving reproductive, maternal, and child health: a multisectoral collaboration in the conflict setting of Afghanistan. BMJ 363: k4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essink D. 2012. Sustainable Health Systems: The Role of Change Agents in Health System Innovation. Hertogenbosch, The Netherlands: BoxPress. [Google Scholar]
- Fitzgerald L, Benzerga W, Mirira M. et al. 2016. Scaling up Early Infant Male Circumcision: lessons from the Kingdom of Swaziland. Global Health: Science and Practice 4: S76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gergen J, Falcao J, Rajkotia Y.. 2018. Stunted scale-up of a performance-based financing program on HIV and maternal–child health services in Mozambique—a policy analysis. African Journal of AIDS Research 17: 353–61. [DOI] [PubMed] [Google Scholar]
- Ghiron L, Shillingi L, Kabiswa C. et al. 2014. Beginning with sustainable scale up in mind: initial results from a population, health and environment project in East Africa. Reproductive Health Matters 22: 84–92. [DOI] [PubMed] [Google Scholar]
- Goga A, Muhe L.. 2011. Global challenges with scale-up of the integrated management of childhood illness strategy: results of a multi-country survey. BMC Public Health 11: 503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grin J, Rotmans J, Schot J.. 2010. Transitions to Sustainable Development: New Directions in the Study of Long Term Transformative Change. New York: Routledge. [Google Scholar]
- Hainsworth G, Engel D, Simon C, Rahimtoola M, Ghiron L.. 2014. Scale-up of adolescent contraceptive services: lessons from a 5-country comparative analysis. Journal of Acquired Immune Deficiency Syndromes 66: S2. [DOI] [PubMed] [Google Scholar]
- Igras S, Sinai I, Mukabatsinda M, Ngabo F, Jennings V, Lundgren R.. 2014. Systems approach to monitoring and evaluation guides scale up of the Standard Days Method of family planning in Rwanda. Global Health: Science and Practice 2: 234–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan K, Butrick E, Yamey G, Miller S.. 2016. Barriers and facilitators to scaling up the non-pneumatic anti-shock garment for treating obstetric hemorrhage: a qualitative study. PLoS One 11: e0150739.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyonzo N, Nyachae P, Kagwe P. et al. 2015. From project to program: Tupange’s experience with scaling up family planning interventions in urban Kenya. Reproductive Health Matters 23: 103–13. [DOI] [PubMed] [Google Scholar]
- Kripke K, Reed J, Hankins C. et al. 2016. Impact and cost of scaling up voluntary medical male circumcision for HIV prevention in the context of the new 90-90-90 HIV treatment targets. PloS one 11: e0155734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumholz AR, Stone AE, Dalaba MA, Phillips JF, Adongo PB.. 2015. Factors facilitating and constraining the scaling up of an evidence-based strategy of community-based primary care: management perspectives from northern Ghana. Global Public Health 10: 366–78. [DOI] [PubMed] [Google Scholar]
- Lewin S, Bohren M, Rashidian A. et al. 2018a. Applying GRADE-CERQual to qualitative evidence synthesis findings—paper 2: how to make an overall CERQual assessment of confidence and create a Summary of Qualitative Findings table. Implementation Science 13: 10.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin S, Booth A, Glenton C. et al. 2018b. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. BioMed Central 13: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macgregor H, Mckenzie A, Jacobs T, Ullauri A.. 2018. Scaling up ART adherence clubs in the public sector health system in the Western Cape, South Africa: a study of the institutionalisation of a pilot innovation. Globalization and Health 14: 40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangham L, Hanson K.. 2010. Scaling up in international health: what are the key issues. Health Policy and Planning 24: 85–96. [DOI] [PubMed] [Google Scholar]
- Milat A, Bauman A, Redman S.. 2015. Narrative review of models and success factors for scaling up public health interventions. Implementation Science 10: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojomo E, Elliott M, Goodyear L, Forson M, Bartram J.. 2015. Sustainability and scale-up of household water treatment and safe storage practices: enablers and barriers to effective implementation. International Journal of Hygiene and Environmental Health 218: 704–13. [DOI] [PubMed] [Google Scholar]
- Omimo A, Taranta D, Ghiron L. et al. 2018. Applying ExpandNet’s systematic approach to scaling up in an integrated population, health and environment project in East Africa. Social Sciences 7: 8. [Google Scholar]
- Paina L, Peters DH.. 2012. Understanding pathways for scaling up health services through the lens of complex adaptive systems. Health Policy and Planning 27: 365–73. [DOI] [PubMed] [Google Scholar]
- Pappa S, Muralidharan A, Dayal R, Das M.. 2015. Promoting Gender Equality in India: three Approaches to Scale-up. Washington, DC: Futures Group, Health Policy Project. [Google Scholar]
- Pérez-Escamilla R, Cavallera V, Tomlinson M, Dua T.. 2018. Scaling up Integrated Early Childhood Development programs: lessons from four countries. Child: Care, Health and Development 44: 50–61. [DOI] [PubMed] [Google Scholar]
- Pérez-Escamilla R, Curry L, Minhas D, Taylor L, Bradley E.. 2012. Scaling up of breastfeeding promotion programs in low- and middle-income countries: the “breastfeeding gear” model. Advances in Nutrition 3: 790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider H, Coetzee D, Van Rensburg D, Gilson L.. 2010. Differences in antiretroviral scale up in three South African provinces: the role of implementation management. BMC Health Services Research 10 (Suppl. 1): S4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons R, Fajans P, Ghiron L.. 2007. Scaling up Health Service Delivery: From Pilot Innovations to Policies and Programmes. Geneve, Switserland: World Health Organization. [Google Scholar]
- Smith J, DE Graft-Johnson J, Zyaee P, Ricca J, Fullerton J.. 2015. Scaling up high-impact interventions: how is it done? International Journal of Gynaecology and Obstetrics 130: S4. [DOI] [PubMed] [Google Scholar]
- Somassè YE, Bahwere P, Laokri S, Elmoussaoui N, Donnen P.. 2013. Sustainability and scaling-up analysis of community-based management of acute malnutrition: lessons learned from Burkina Faso. Food and Nutrition Bulletin 34: 338–48. [DOI] [PubMed] [Google Scholar]
- Spicer N, Berhanu D, Bhattacharya D. et al. 2016. ‘The stars seem aligned’: a qualitative study to understand the effects of context on scale-up of maternal and newborn health innovations in Ethiopia, India and Nigeria. Globalization and Health 12: 75.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spicer N, Bhattacharya D, Dimka R. et al. 2014. ‘Scaling-up is a craft not a science’: catalysing scale-up of health innovations in Ethiopia, India and Nigeria. Social Science & Medicine 121: 30–8. [DOI] [PubMed] [Google Scholar]
- Spicer N, Hamza YA, Berhanu D. et al. 2018. ‘The development sector is a graveyard of pilot projects!’ Six critical actions for externally funded implementers to foster scale-up of maternal and newborn health innovations in low and middle-income countries. Globalization and Health 14: 74.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svanemyr J, Baig Q, Chandra-Mouli V.. 2015. Scaling up of life skills based education in Pakistan: a case study. Sex Education 15: 249–62. [Google Scholar]
- Tromp N, Siregar A, Leuwol B. et al. 2013. Cost-effectiveness of scaling up voluntary counselling and testing in West-Java, Indonesia. Acta Medica Indonesiana 45: 17–25. [PubMed] [Google Scholar]
- Van den Bosch S, Rotmans J.. 2008. Deepening, Broadening and Scaling Up: A Framework for Steering Transition Experiments. Delft and Rotterdam, The Netherlands: Knowledge Centre for Sustainable System Innovations and Transitions (KCT).
- Van der Ham AJ, Shields LS, Broerse JE.. 2013. Towards integration of service user knowledge in mental healthcare in low and middle-income countries: insights from Transition Theory. Knowledge Management for Development Journal 9: 125–39. [Google Scholar]
- WHO/EXPANDNET. 2009. Practical Guidance for Scaling Up Health Service Innovations. Geneva, Switzerland: World Health Organization.
- WHO/EXPANDNET. 2010. Nine Steps for Developing a ScalingUp Strategy. Geneva, Switzerland: World Health Organization.
- WHO/EXPANDNET. 2011. Beginning with the End in Mind: Planning Pilot Projects and Other Programmatic Research for Successful Scaling Up. Geneva, Switzerland: World Health Organization.
- Wickremasinghe D, Gautham M, Umar N, Berhanu D, Schellenberg J, Spicer N.. 2018. “It’s about the idea hitting the bull’s eye”: how aid effectiveness can catalyse the scale-up of health innovations. International Journal of Health Policy and Management 7: 718.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamey G. 2012. What are the barriers to scaling up health interventions in low and middle income countries? A qualitative study of academic leaders in implementation science. Globalization and Health 8: 11.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying R, Barnabas RV, Williams BG. 2014. Modeling the implementation of universal coverage for HIV treatment as prevention and its impact on the HIV epidemic. Current HIV/AIDS Reports 11: 459–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yothasamut J, Putchong C, Sirisamutr T, Teerawattananon Y, Tantivess S.. 2010. Scaling up cervical cancer screening in the midst of human papillomavirus vaccination advocacy in Thailand. BMC Health Services Research 10: S5.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


