Abstract
Introduction:
Long-term growth outcomes and the prevalence of obesity among older single ventricle (SV) patients have not been well characterized. We investigated these parameters, as well as the impact of obesity on survival, in an older cohort of SV patients presenting for Fontan conversion.
Methods:
We analyzed preoperative height, weight, and body mass index (BMI) of patients who underwent Fontan conversion. Overweight and obese were defined as BMI ≥85 percentile and ≥95 percentile for patients <20 years and BMI 25 to 30 kg/m2 and ≥30 kg/m2 for patients ≥20 years, respectively. Postoperative transplant-free survival was assessed among obese, overweight, and normal weight patients.
Results:
We evaluated 139 patients presenting for Fontan conversion at a median age of 23.2 years. Patients had shorter stature compared to the normal population (mean Z score −0.6, P < .001). Younger patients had lower BMI compared to the normal population (<20 years: mean Z score −0.5, P = .02), while older patients had elevated BMI (≥20 years: mean Z score +0.4, P < .001). The mean BMI among older patients approached overweight at 24.6 kg/m2. The prevalence of obesity increased with advancing age, with 36% overweight and 14% obese at >30 years. At a median of 8.2 years following Fontan conversion, obesity and overweight status were not associated with transplant-free survival.
Conclusion:
Older SV patients presenting for Fontan conversion had shorter stature compared to the normal population as well as a high prevalence of overweight and obesity. Although there was no relationship between weight status and early postoperative survival, further investigation of long-term outcomes is warranted.
Keywords: CHD, univentricular heart, Fontan, adult congenital heart disease, obesity
Introduction
Growth of single ventricle (SV) patients has mostly been studied in the interstage period and at short- to intermediate-term intervals following Fontan completion.1–8 These studies have demonstrated that SV patients experience growth restriction early in life1–4 and remain of shorter stature into the late childhood and early adolescent years.5–8 Data are conflicting as to whether patients remain underweight5,6 or achieve normal weight8,9 by adolescence or adulthood.
Recent literature regarding obesity in the congenital heart disease population has suggested that the prevalence is lower among SV patients.10,11 However, these studies focused on children through 19 years of age. The prevalence of obesity among adult SV patients, as well as its potential impact on outcomes, is unknown. In addition to the well-known negative cardiovascular effects of obesity on adults with structurally normal hearts,12–16 less well-recognized effects such as decreased lung compliance, increased ventricular mass, and diastolic dysfunction17–19 may pose unique challenges for patients with SV physiology.
Since patients presenting for Fontan conversion surgery represent a discrete, well-defined cohort of older SV patients, we aimed to investigate long-term growth and the prevalence of obesity in this population. Moreover, we sought to assess the impact of obesity on early transplant-free survival following Fontan conversion.
Methods
Patient Population
In this retrospective, single-center study, we included consecutive patients who underwent Fontan conversion surgery to total extracardiac cavopulmonary connections at our institution, the Ann & Robert H. Lurie Children’s Hospital of Chicago (formerly Children’s Memorial Hospital), from 1994 to 2012. One patient underwent a repeat Fontan conversion surgery during this time period, and data were included from the first operation only. Approval from our institutional review board was obtained, and the need for written informed consent was waived.
Our indications for Fontan conversion and surgical techniques have been previously described.20–23 Refractory arrhythmias were the most common primary indication for surgery. Pathway obstruction, residual shunting, atrioventricular valve dysfunction, and/or decreased functional status contributed to the decision to proceed with surgery. In general, the surgery consisted of takedown of the original anastomoses with the creation of a total extracardiac cavopulmonary connection, arrhythmia surgery, and epicardial pacemaker placement.
Data Collection and Definitions
Height and weight data were collected from comprehensive preoperative evaluations performed at our institution. Body mass index (BMI) was calculated using the weight in kilograms (kg) divided by the height in meters square (m2). Height, weight, and BMI for patients <20 years of age were converted to gender-specific percentiles and Z scores using the Centers for Disease Control and Prevention (CDC) growth charts and the lambda–mu–sigma (LMS) method.24 This method creates smoothing of growth percentile curves for a given age and gender and allows for efficient calculation of Z scores.25 The CDC growth charts are published through 20 years of age for pediatric patients. Since adult growth charts are not available, the percentiles and Z scores for older patients were calculated using reference values for 20-year-old subjects.
Overweight and obese patients were categorized according to standard pediatric and adult definitions. For patients <20 years of age, overweight was defined as BMI ≥85th percentile and <95th percentile and obesity as BMI ≥95th percentile. For patients ≥20 years, overweight was defined as BMI ≥25 kg/m2 and <30 kg/m2 and obesity as BMI ≥30 kg/m2. Normal weight refers to BMI <85th percentile for patients <20 years and <25 kg/m2 for patients ≥20 years.
Data were collected regarding demographic characteristics; ventricular morphology, categorized as left ventricle (LV) dominant or non-LV dominant (ie, right ventricle [RV] dominant or indeterminate); presence of heterotaxy; New York Heart Association (NYHA) classification; presence of protein-losing enteropathy (PLE), defined as a serum albumin level <3.5 mg/dL; ascites based on physical examination; and thyroid disease, defined as either a history of thyroid medications or an abnormal thyroid function test. Ventricular dysfunction and atrioventricular valve regurgitation on preoperative echocardiogram were qualitatively categorized as at least moderate or mild or less. A limited number of patients had preoperative exercise stress testing available for review, and the maximal oxygen consumption (VO2 max) was noted and is expressed in milliliters/kilogram/minute (mL/kg/min).
Postoperative outcomes following Fontan conversion, including length of postoperative hospital stay and time to all-cause mortality or heart transplant, were also collected. For patients lost to follow-up after discharge, information regarding vital status was obtained from the Social Security Administration’s Death Master File through September 2013.
Statistical Analysis
Data are represented as frequency (percentage), median (range), or mean (standard deviation [SD]) where appropriate. Since anthropometric parameters are normally distributed, we utilized parametric testing for the growth analyses. We performed subgroup analyses for patients <20 years and for patients ≥20 years compared to the normal population (Z score 0, SD ± 1) using one-sample t tests. Continuous parametric variables were otherwise analyzed with two-sample t tests and analyses of variance, assuming unequal variances. Associations among nonparametric variables were analyzed with the Mann-Whitney U or Kruskal-Wallis tests, and associations between categorical variables were tested with chi-square analyses or Fisher’s exact tests where appropriate. The association of obesity and overweight status with transplant-free survival following Fontan conversion was explored with Kaplan-Meier analyses, with the log-rank test used to compare survival between groups (obese vs normal weight and overweight vs normal weight). A P value <.05 was considered statistically significant for all analyses.
Results
Fontan conversion surgery was performed in 139 patients at a median age of 23.2 years (2.6–47.3). All cases had complete preoperative anthropometric data available for review. Table 1 displays the demographic and preoperative characteristics of the patient population.
Table 1.
Demographic and Preoperative Characteristics of Patient Population.a
| Age at primary Fontan surgery, years | 5.6 (1.1–34.9) |
| Type of primary Fontan | |
| Atriopulmonary | 109 (78) |
| Conduit (valved or nonvalved/Björk modification) | 18 (13) |
| Lateral tunnel | 12 (9) |
| Time since primary Fontan surgery, years | 16.9 (6.3–30.7) |
| Age at Fontan conversion surgery, years | 23.2 (2.6–47.3) |
| Male | 79 (57) |
| Left ventricular morphology | 119 (86) |
| Heterotaxy syndrome | 5 (4) |
| NYHA classification | |
| I | 1 (<1) |
| II | 42 (30) |
| III | 73 (53) |
| IV | 23 (17) |
| Protein-losing enteropathy | 4 (3) |
| Ascites | 26 (22) |
| Thyroid disease | 21 (15) |
| At least moderate ventricular dysfunction | 20 (14) |
| At least moderate atrioventricular valve regurgitation | 17 (12) |
Abbreviation: NYHA, New York Heart Association.
Data are reported as median (range) or frequency (percentage).
Stature
With regard to stature, 18% of the cohort was shorter than the 5th percentile (9% had Z score ≤−2), while 5% was taller than the 95th percentile (4% had Z score ≥+2). The mean height Z score was −0.6 (SD ± 1.4), which was significantly lower than the mean height Z score of the normal population (P < .001). There was a trend toward association between shorter stature and non-LV morphology (P = .07). Patients with non-LV morphology had a mean height Z score of −1.3 (SD ± 2.2), while patients with LV morphology had a mean height Z score of −0.5 (SD ± 1.2). Among patients with non-LV morphology, 15% had Z scores ≤−2, as compared to 8% of patients with LV morphology. This difference, however, was not statistically significant. NYHA classification, ventricular dysfunction, and atrioventricular valve regurgitation were not associated with stature at the time of Fontan conversion.
Weight, BMI, and Prevalence of Obesity
Fifteen percent of the cohort weighed less than the 5th percentile (10% had Z score ≤−2), while 7% weighed greater than the 95th percentile (4% had Z score ≥+2). The mean Z score for weight was −0.2 (± 1.7), which was not significantly different from the normal population (P = .12). For BMI, 10% of the cohort was lower than the 5th percentile (8% had Z score ≤−2), and 7% exceeded the 95th percentile (5% had Z score ≥+2). The mean BMI Z score was +0.09 (± 1.2), which was also not significantly different from the normal population (P = .36).
Similar to stature, NYHA classification, ventricular dysfunction, and atrioventricular valve regurgitation were not associated with weight or BMI at the time of Fontan conversion. In addition, there was no statistically significant association between PLE, ascites, or thyroid disease and weight or BMI. Preoperative exercise stress testing was available for a limited number of patients (n = 66). The median VO2 max was 20.7 mL/kg/min (7.4–37.4). There was no statistically significant difference in VO2 max among patients classified as obese (18.8 mL/kg/min), overweight (20.4 mL/kg/min), or normal weight (21.0 mL/kg/min).
The combined prevalence of overweight and obese patients was 33%: 33 patients (24%) were overweight and 13 patients (9%) were obese. The prevalence increased with advancing age at the time of presentation for Fontan conversion surgery (Figure 1). Specifically, the prevalence of both overweight and obesity was more than twofold higher in patients presenting at >30 years of age when compared to patients presenting at <20 years.
Figure 1.
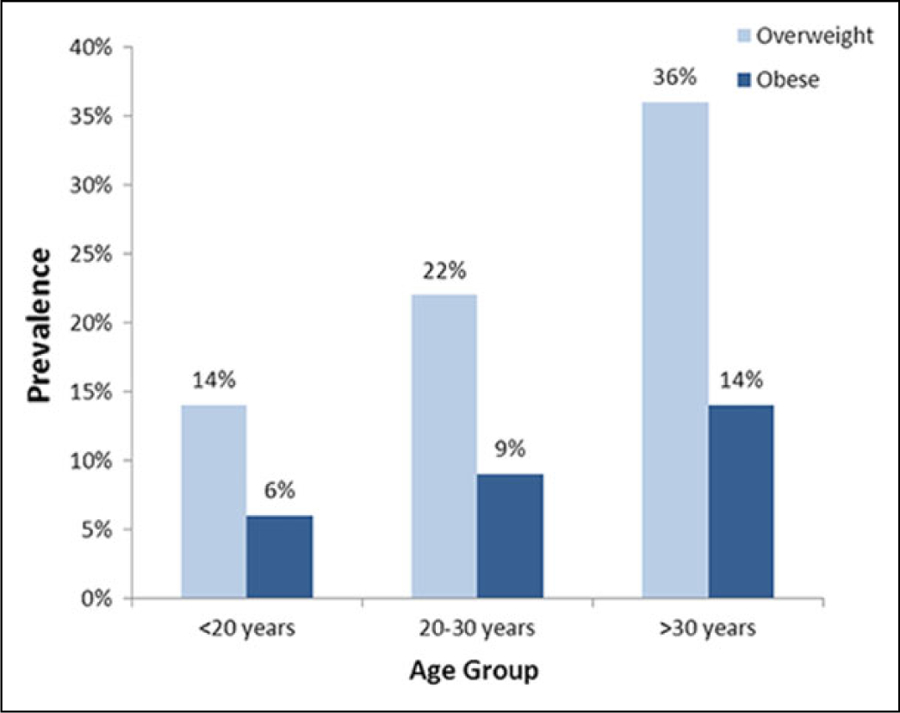
Increasing prevalence of overweight and obese single ventricle patients with advancing age.
Subgroup Analyses by Age
The growth parameters of patients <20 years of age differed from those of patients ≥20 years when compared to the normal population (Table 2). In the younger subgroup, patients had significantly shorter stature, lower weight, and lower BMI at the time of Fontan conversion when compared to the normal CDC values for age. In the older subgroup, patients were shorter than normal CDC adult stature, however, weight and BMI were significantly elevated compared to the normal CDC adult values (P = .04 and <.001, respectively; see Figure 2 for absolute values). The mean BMI among patients ≥20 years was 24.6 (±3.0) kg/m2, with males having a higher BMI, 25.4 (± 3.3) kg/m2, compared to females, 23.6 (± 2.5) kg/m2; P = .04.
Table 2.
Growth Parameters by Younger (Age <20 years) and Older (Age ≥20 years) Subgroups.a
| Height Z Score | P Value | Weight Z Score | P Value | BMI Z Score | P Value | |
|---|---|---|---|---|---|---|
| <20 Years (n = 49) | −1.0 (± 1.7) | <.001 | −1.1 (± 2.2) | .001 | −0.5 (± 1.4) | .02 |
| ≥20 Years (n = 90) | −0.3 (± 1.0) | .002 | +0.2 (± 1.0) | .04 | +0.4 (± 1.0) | <.001 |
Abbreviation: BMI, body mass index.
Z scores are expressed as mean (standard deviation). P values represent comparisons to the normal population.
Figure 2.
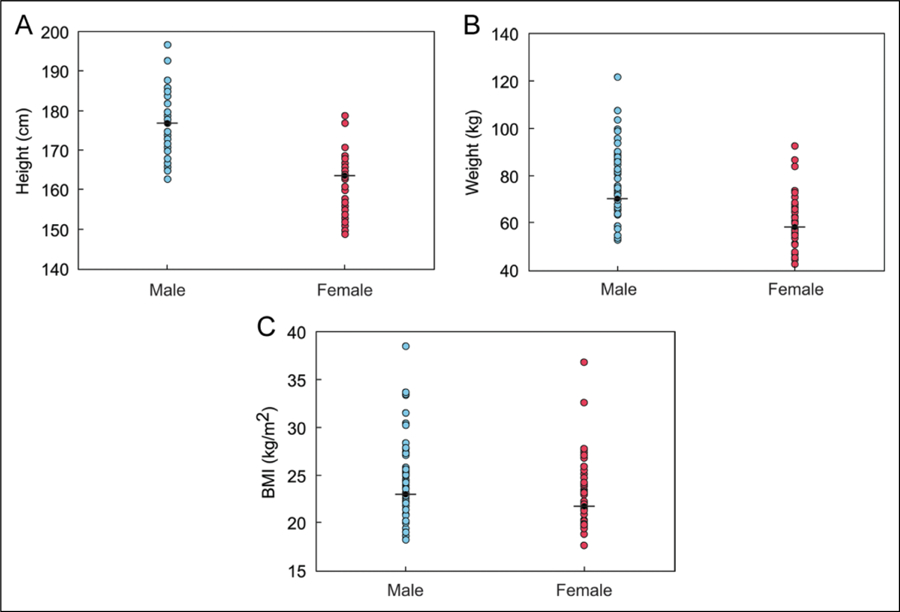
Absolute values of (A) height, (B) weight, and (C) BMI of the cohort ≥20 years. The black line represents the mean value of the normal population at 20 years of age per the CDC.24 BMI indicates body mass index; CDC, Centers for Disease Control and Prevention.
Postoperative Length of Stay and Transplant-Free Survival
The median postoperative length of hospital stay was 11 days (6–58, with one outlier at 111 days). There was no statistically significant difference in median length of stay by obesity or overweight status (12 days for both obese and overweight patients vs 11 days for normal weight patients).
The median age at most recent follow-up was 32.3 years (14.3–61.3), which was a median of 8.2 years (1.2 months-18.5 years) following Fontan conversion surgery. Thirty-two (23%) of 139 patients died and/or underwent heart transplant. Ten (7%) patients were transplanted at a median postoperative interval of 10.2 months (<1 month-9.4 years), four of whom subsequently died. All-cause mortality was 19% (26 of 139), and death occurred at a median of 4.1 years (<1 month-14.1 years) following surgery. Transplant-free survival was not associated with obesity at the time of Fontan conversion (Figure 3), nor with overweight status (log-rank P = .20).
Figure 3.
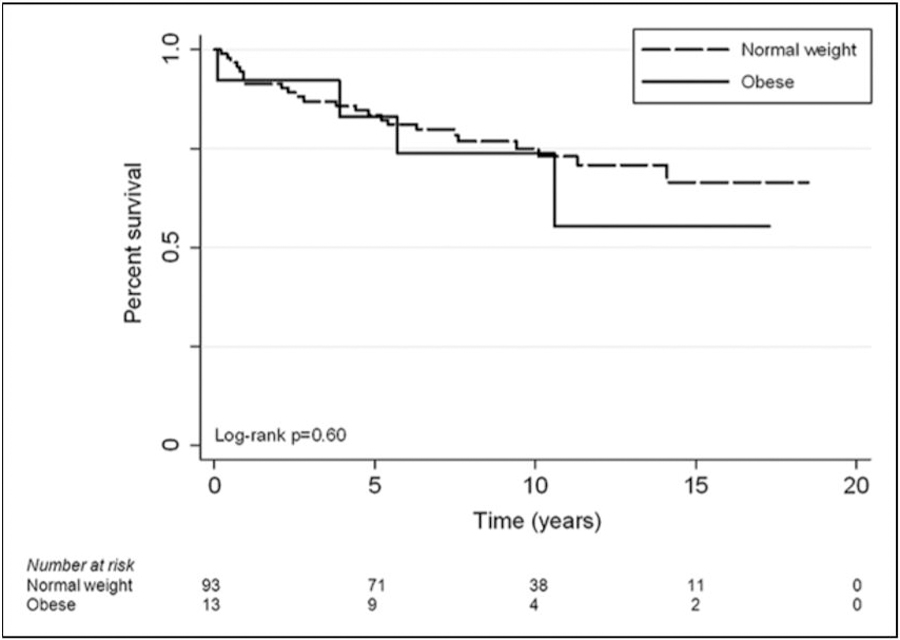
Kaplan-Meier curve depicting transplant-free survival following Fontan conversion by obesity status.
Comment
In this series of older SV patients presenting for Fontan conversion surgery, we report growth outcomes and the prevalence of obesity. While prior studies have described short- to intermediate-term growth outcomes following Fontan completion,4–9 our study investigated long-term outcomes at a median of 17 years following primary Fontan surgery. We found that this cohort of SV patients remained of shorter stature compared to the normal population. Furthermore, there was a greater prevalence of overweight and obese patients with advancing age at the time of presentation. Obesity was not, however, associated with lower transplant-free survival in the early postoperative period.
Conflicting associations between ventricular morphology and somatic growth among SV patients have been reported in the literature.4,5,8,9 François et al reported that older children and adolescents with a dominant LV were shorter than patients with a dominant RV.4 A recent study by Hessel and colleagues investigating somatic growth in 94 SV patients up to 11 years of age demonstrated that patients with a dominant RV had lower weight for age.26 Our data were not conclusive but tended to support the notion that SV patients with non-LV dominance, that is, RV dominance or indeterminate ventricular morphology, had shorter stature at the time of Fontan conversion.
Previous studies in younger populations demonstrated that SV patients either remained underweight or eventually experienced normalization of weight after the Fontan operation.5,6,9 We found that although patients <20 years of age had lower BMI compared to the normal population, the mean BMI of patients ≥20 years was elevated and approached the threshold for overweight. Males, in particular, were more likely to be overweight or obese, which mirrors national trends.27 Of note, elevated weight and BMI were not associated with markers of fluid retention, such as PLE or ascites. There was also no association between weight or BMI and thyroid disease, despite the fact that a substantial proportion of patients may have taken antiarrhythmic agents known to affect thyroid function, such as amiodarone.
Most importantly, our study showed that the prevalence of overweight and obesity among older SV patients increased with advancing age. In two large, contemporary series of younger SV patients through 19 years of age, the combined prevalence of overweight and obesity ranged from 6% to 16%.10,11 In our subgroup <20 years of age, we found the prevalence to be similar (20%). However, in the third decade of life, the prevalence of overweight and obesity increased to 31% and by the fourth decade reached 50% of patients. These findings should be substantiated in larger series of SV and adult congenital heart disease populations, in general, but raise significant concern about the susceptibility of this vulnerable patient population to national obesity trends.27
While the well-known health impacts of obesity, including myocardial infarction,12 stroke,13 hypertension,14 diabetes mellitus,15 and chronic kidney disease,16 are important with increasing age, several of the less well-known adverse consequences of obesity may be particularly deleterious in patients with SV physiology. Obesity is associated with reduced lung compliance and increased pulmonary vascular resistance,18 which may augment progressive hypoxemia in SV patients who rely on passive pulmonary blood flow. Obesity-related increases in ventricular mass and systemic vascular resistance may contribute to diastolic dysfunction and exercise intolerance.17,19 The adverse effects of obesity on ventricular mass, size, and function have already been demonstrated in patients with other forms of congenital heart disease, including transposition of the great arteries28 and tetralogy of Fallot.29 Finally, autonomic imbalance from obesity may potentiate arrhythmias by increasing sympathetic tone,30 which can rapidly destabilize an already tenuous SV circulation.
Although obesity was not associated with longer length of hospital stay or lower transplant-free survival in the current study, it may be an important modifiable risk factor for functional outcome and quality of life, which were not investigated in this study. In addition, obesity may impact late mortality in this population. While it is possible that the ‘‘obesity paradox’’ may play a role, wherein adult patients with higher BMI have reduced mortality following acute coronary syndromes and cardiac surgery,31,32 this finding has not been consistently demonstrated in the literature, particularly at the extremes of weight and with longer duration of follow-up.33,34 This phenomenon also may not apply to high-risk SV patients in whom the pathophysiologic consequences of obesity are unique.
Interventions targeting obesity may be important for this patient population; however, further investigation is warranted. SV patients tend to lead relatively sedentary lives, whether by choice, functional limitation, or physician restriction.35–38 The adverse cardiorespiratory consequences of obesity should at least be considered when discussing exercise restrictions with patients and families. Exercise programs for adults with congenital heart disease are emerging and may prove beneficial for Fontan patients.39,40 In general, education regarding cardiovascular risk factors, along with serial risk assessment and therapeutic life style management, should be considered as part of routine, long-term Fontan care.
Limitations
The study was limited by its retrospective, single-center design. Since our subjects were exclusively drawn from patients undergoing Fontan conversion, the findings may not be generalizable to all older SV patients. Importantly, we may have been underpowered to detect a survival difference between the weight groups due to our limited sample size and duration of follow-up, which may have been too short for patients to accrue mortality. Patients were referred from multiple different institutions for Fontan conversion and most returned to those institutions, thus, serial anthropometric and other data prior to and following the surgery were not readily available. Associated morbidities, indices of functional outcome, including postoperative exercise capacity, and quality of life, were not examined. Finally, obesity-related risk factors, such as fasting glucose and lipid levels were not available either preoperatively or postoperatively. Further surveillance with ongoing investigation and risk stratification of this population, as well as other SV patients, is warranted in the future.
Conclusions
Consistent with trends in childhood, older SV patients presenting for Fontan conversion remained of shorter stature compared to the normal population. However, adult patients demonstrated elevated weight and BMI, with the prevalence of obesity increasing with advancing age. Although there was no relationship between obesity and early postoperative transplant-free survival in the current study, obesity may be an important modifiable risk factor for functional outcome, quality of life, and/or late mortality among the SV population. The effects of obesity on SV physiology should be explored further, along with targeted measures to reduce the overall cardiovascular morbidity in this patient population.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was partly supported by grants from the Children’s Heart Foundation (Lincolnshire, IL) and the Saving tiny Hearts Society (Deerfield, IL) as well as by an endowment to the Ann & Robert H. Lurie Children’s Hospital of Chicago, Division of Pediatric Cardiology by Mr. Warren Batts. Dr. Freud is supported by the National Institutes of Health (T32-HL007572).
Abbreviations and Acronyms
- BMI
body mass index
- CDC
Centers for Disease Control and Prevention
- LV
left ventricle
- NYHA
New York Heart Association
- PLE
protein-losing enteropathy
- RV
right ventricle
- SD
standard deviation
- SV
single ventricle
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Srinivasan C, Jaquiss RD, Morrow WR, et al. Impact of staged palliation on somatic growth in patients with hypoplastic left heart syndrome. Congenit Heart Dis. 2010;5(6): 546–551. [DOI] [PubMed] [Google Scholar]
- 2.Williams RV, Zak V, Ravishankar C, et al. Factors affecting growth in infants with single ventricle physiology: a report from the Pediatric Heart Network Infant Single Ventricle Trial. J Pediatr. 2011;159(6): 1017–1022. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daymont C, Neal A, Prosnitz A, Cohen MS. Growth in children with congenital heart disease. Pediatrics. 2013;131(1): e236–e242. [DOI] [PubMed] [Google Scholar]
- 4.François K, Bove T, Panzer J, et al. Univentricular heart and Fontan staging: analysis of factors impacting on body growth. Eur J Cardiothorac Surg. 2012;41(6): e139–e145. [DOI] [PubMed] [Google Scholar]
- 5.Cohen MI, Bush DM, Ferry RJ Jr, et al. Somatic growth failure after the Fontan operation. Cardiol Young. 2000;10(5): 447–457. [DOI] [PubMed] [Google Scholar]
- 6.Day RW, Denton DM, Jackson WD. Growth of children with a functionally single ventricle following palliation at moderately increased altitude. Cardiol Young. 2000;10(3): 193–200. [DOI] [PubMed] [Google Scholar]
- 7.Vogt KN, Manlhiot C, Van Arsdell G, Russell JL, Mital S, McCrindle BW. Somatic growth in children with single ventricle physiology impact of physiologic state. J Am Coll Cardiol. 2007; 50(19): 1876–1883. [DOI] [PubMed] [Google Scholar]
- 8.Ono M, Boethig D, Goerler H, Lange M, Westhoff-Bleck M, Breymann T. Somatic development long after the Fontan operation: factors influencing catch-up growth. J Thorac Cardiovasc Surg. 2007;134(5): 1199–1206. [DOI] [PubMed] [Google Scholar]
- 9.Hasan BS, Bendaly EA, Alexy RD, Ebenroth ES, Hurwitz RA, Batra AS. Somatic growth after fontan and mustard palliation. Congenit Heart Dis. 2008;3(5): 330–335. [DOI] [PubMed] [Google Scholar]
- 10.Shustak RJ, McGuire SB, October TW, Phoon CK, Chun AJ. Prevalence of obesity among patients with congenital and acquired heart disease. Pediatr Cardiol. 2012;33(1): 8–14. [DOI] [PubMed] [Google Scholar]
- 11.Pinto NM, Marino BS, Wernovsky G, et al. Obesity is a common comorbidity in children with congenital and acquired heart disease. Pediatrics. 2007;120(5): e1157–e1164. [DOI] [PubMed] [Google Scholar]
- 12.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67(5): 968–977. [DOI] [PubMed] [Google Scholar]
- 13.Wilson PW, Bozeman SR, Burton TM, Hoaglin DC, Ben-Joseph R, Pashos CL. Prediction of first events of coronary heart disease and stroke with consideration of adiposity. Circulation. 2008; 118(2): 124–130. [DOI] [PubMed] [Google Scholar]
- 14.Mendizabal Y, Llorens S, Nava E. Hypertension in metabolic syndrome: vascular pathophysiology. Int J Hypertens. 2013;2013: 230868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schienkiewitz A, Schulze MB, Hoffmann K, Kroke A, Boeing H. Body mass index history and risk of type 2 diabetes: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Am J Clin Nutr. 2006;84(2): 427–433. [DOI] [PubMed] [Google Scholar]
- 16.Silverwood RJ, Pierce M, Hardy R, et al. Early-life overweight trajectory and CKD in the 1946 British birth cohort study. Am J Kidney Dis. 2013;62(2): 276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kossaify A, Nicolas N. Impact of overweight and obesity on left ventricular diastolic function and value of tissue Doppler echocardiography. Clin Med Insights Cardiol. 2013;7: 43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parameswaran K, Todd DC, Soth M. Altered respiratory physiology in obesity. Can Respir J 2006;13(4): 203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen MS, Zak V, Atz AM, et al. Anthropometric measures after Fontan procedure: Implications for suboptimal functional outcome. Am Heart J. 2010;160(6): 1092–1098.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mavroudis C, Deal BJ, Backer CL, et al. J. Maxwell Chamberlain Memorial Paper for congenital heart surgery 111 Fontan conversions with arrhythmia surgery: surgical lessons and outcomes. Ann Thorac Surg. 2007;84: 1457–65; discussion 1465–1466. [DOI] [PubMed] [Google Scholar]
- 21.Mavroudis C, Backer CL, Deal BJ, Johnsrude CL. Fontan conversion to cavopulmonary connection and arrhythmia circuit cryoblation. J Thorac Cardiovasc Surg. 1998;115(3): 547–556. [DOI] [PubMed] [Google Scholar]
- 22.Backer CL, Tsao S, Deal BJ, Mavroudis C. Maze procedure in single ventricle patients. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2008:44–48. [DOI] [PubMed]
- 23.Backer CL, Deal BJ, Mavroudis C, Franklin WH, Stewart RD. Conversion of the failed Fontan circulation. Cardiol Young. 2006;16(suppl 1): 85–91. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Growth charts: Percentile data files with LMS values. Hyattsville, MD: National Center for Health Statistics; Web site. http://www.cdc.gov/growthcharts/clinical_charts.htm; last reviewed August 4, 2009, last updated August 4, 2009; Accessed December 1, 2012. [Google Scholar]
- 25.Flegal KM, Cole TJ. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Natl Health Stat Rep. 2013;(63):1–3. [PubMed] [Google Scholar]
- 26.Hessel TW, Greisen G, Idorn L, Reimers JI. Somatic growth in 94 single ventricle children – comparing systemic right and left ventricle patients. Acta Paediatr. 2013;102(1): 35–39. [DOI] [PubMed] [Google Scholar]
- 27.Ogden CL CM, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010 NCHS Data Brief, no 82. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 28.Pasquali SK, Marino BS, Powell DJ, et al. Following the arterial switch operation, obese children have risk factors for early cardiovascular disease. Congenit Heart Dis. 2010;5(1): 16–24. [DOI] [PubMed] [Google Scholar]
- 29.Maskatia SA, Spinner JA, Nutting AC, Slesnick TC, Krishnamurthy R, Morris SA. Impact of obesity on ventricular size and function in children, adolescents and adults with Tetralogy of Fallot after initial repair. Am J Cardiol. 2013;112(4): 594–598. [DOI] [PubMed] [Google Scholar]
- 30.McCully BH, Hasan W, Streiff CT, et al. Sympathetic cardiac hyperinnervation and atrial autonomic imbalance in diet-induced obesity promote cardiac arrhythmias. Am J Physiol Heart Circ Physiol. 2013;305(10): H1530–H1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gruberg L, Weissman NJ, Waksman R, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39(4): 578–584. [DOI] [PubMed] [Google Scholar]
- 32.Stamou SC, Nussbaum M, Stiegel RM, et al. Effect of body mass index on outcomes after cardiac surgery: is there an obesity paradox? Ann Thorac Surg. 2011;91(1): 42–47. [DOI] [PubMed] [Google Scholar]
- 33.Kadakia MB, Fox CS, Scirica BM, Murphy SA, Bonaca MP, Morrow DA. Central obesity and cardiovascular outcomes in patients with acute coronary syndrome: observations from the MERLIN-TIMI 36 trial. Heart. 2011;97(21): 1782–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benedetto U, Danese C, Codispoti M. Obesity paradox in coronary artery bypass grafting: myth or reality? J Thorac Cardiovasc Surg. 2014;147(5): 1517–1523. [DOI] [PubMed] [Google Scholar]
- 35.Lunt D, Briffa T, Briffa NK, Ramsay J. Physical activity levels of adolescents with congenital heart disease. Aust J Physiother. 2003;49(1): 43–50. [DOI] [PubMed] [Google Scholar]
- 36.Stefan MA, Hopman WM, Smythe JF. Effect of activity restriction owing to heart disease on obesity. Arch Pediatr Adolesc Med. 2005;159(5): 477–481. [DOI] [PubMed] [Google Scholar]
- 37.Moons P, Van Deyk K, Dedroog D, Troost E, Budts W. Prevalence of cardiovascular risk factors in adults with congenital heart disease. Eur J Cardiovasc Prev Rehabil. 2006;13(4): 612–616. [DOI] [PubMed] [Google Scholar]
- 38.Dua JS, Cooper AR, Fox KR, Graham Stuart A. Physical activity levels in adults with congenital heart disease. Eur J Cardiovasc Prev Rehabil. 2007;14(2): 287–293. [DOI] [PubMed] [Google Scholar]
- 39.Dua JS, Cooper AR, Fox KR, Graham Stuart A. Exercise training in adults with congenital heart disease: feasibility and benefits. Int J Cardiol. 2010;138(2): 196–205. [DOI] [PubMed] [Google Scholar]
- 40.Ubeda Tikkanen A, Opotowsky AR, Bhatt AB, Landzberg MJ, Rhodes J. Physical activity is associated with improved aerobic exercise capacity over time in adults with congenital heart disease. Int J Cardiol. 2013;168(5): 4685–4691. [DOI] [PMC free article] [PubMed] [Google Scholar]


